Abstract
Changes in pH modulate the responsiveness of vascular smooth muscle cells to vasoconstrictor stimuli, but their effect on endothelium-dependent responses is unknown. Therefore, the influence of moderate changes in pH on responses to endothelium-dependent and –independent agonists was determined in aortae and carotid arteries of 15- to 26-week-old male C57BL/6N mice. Isolated rings were suspended in Halpern–Mulvany myographs for isometric tension recording. The preparations were exposed to either acidic (pH 7), control (pH 7.4) or alkaline (pH 7.8) modified Krebs–Ringer bicarbonate buffer solutions and their contractions and relaxations compared. Endothelium-dependent relaxations to acetylcholine (in the presence of meclofenamate or of the thromboxane-prostanoid (TP) receptor antagonist S18886) were comparable at the three pH values tested in contracted aortic or carotid arterial rings. Endothelium-dependent contractions of quiescent carotid arteries were reduced in acidosis and potentiated in alkalosis compared to control; these effects were reversible. The carotid arteries produced equal amounts of 6-keto prostaglandin F1α and thromboxane B2 at the different pH values tested. Contractions to the full TP receptor agonist U46619 were similar in the three milieus, but after inducing partial TP receptor blockade (with low concentrations of the TP receptor antagonist S18886) they were depressed in acidosis compared to alkalosis. Prostacyclin as a partial TP receptor activator also induced weaker contractions at low than at high pH, whereas its vasodilator effect was not affected. These findings demonstrate that changes in pH modulate endothelium-dependent contractions in mouse arteries primarily by altering the sensitivity of TP receptors of vascular smooth muscle to endothelium-derived contracting factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endothelial cells cause relaxations of the underlying vascular smooth muscle by releasing nitric oxide (NO) [13, 18, 27] and/or causing endothelium-dependent hyperpolarizations (EDH) [6, 10, 29]. They can also favor vasoconstriction in a variety of blood vessels by liberating endothelium-derived contracting factors (EDCF), in particular vasoconstrictor prostanoids [9, 12, 20, 23]. Endothelial function is compromised by cardiovascular risk factors such as aging, obesity, diabetes and hypertension; the resulting endothelial dysfunction is characterized by a reduced production of NO and/or an augmented release of EDCF [2, 23, 40, 42, 46].
The extracellular pH is a major local regulator of the tone of vascular smooth muscle both in vivo and in vitro [4, 34, 41]. Acidosis in particular can modulate the release of norepinephrine by the adrenergic nerve endings within the vascular wall [47, 48]. To the best of the authors’ knowledge, the impact of metabolic acidosis and alkalosis on either endothelium-dependent relaxations or contractions of mouse arteries has not been reported.
The present experiments were designed to test the hypothesis that moderate changes in pH in the physiopathological range acutely modulate endothelium-dependent changes in vascular tone.
Materials and methods
The experiments were performed in accordance with the Guide for the Care and Use of Laboratory Animals issued by the U.S. Institute of Laboratory Animal Research (ILAR, eight edition, 2011) and were approved by the institutional Committee on the Use of Live Animals for Teaching and Research (CULATR) of the University of Hong Kong.
Animals
Male C57BL/6N mice (15–26 weeks old; body weight=30.7±0.5 g) were obtained from, and housed in the local laboratory animal unit at constant temperature under a 12-h light–dark cycle with ad libitum access to water and standard chow. On the day of the experiments, the mice were anaesthetized with a mixture of fentanyl citrate (0.4 mg/kg), fluanisone (12.5 mg/kg) plus midazolam (6.25 mg/kg) prior to exsanguination by cardiac puncture.
Tissue harvesting and preparation
Carotid arteries and aortae were excised and immediately placed into ice-cold modified Krebs–Ringer bicarbonate solution of the following composition (in mM): NaCl, 129; KCl, 4.7; KH2PO4, 1.18; MgSO4, 1.17; NaHCO3, 14.9; glucose, 5.5; calcium disodium EDTA, 0.026; CaCl2, 2.5 (control solution). Preliminary experiments (data not shown) confirmed that this composition permits to achieve a stable pH of 7.4 in the covered myograph chambers when aerated continuously with 95% O2 and 5% CO2 [28]. The arteries were dissected free of adherent fat and connective tissue in cold control solution, cut into rings (length: approximately 2 mm for carotid arteries and 3 mm for aortae; four rings per blood vessel type for each animal) and suspended between stainless steel wires or pins in covered aerated chambers of Halpern–Mulvany myographs (model 610M; Danish Myo Technology A/S, Aarhus, Denmark). The preparations were allowed to equilibrate at 37°C for 30 min prior to the first application of force (5 mN). For each individual ring every 3 to 5 mN increase in tension was followed by replacement of the control solution for several minutes with an iso-osmotic high potassium solution (60 mM KCl with equimolar substitution of sodium by potassium). The high potassium solution was washed out after the induced response has exceeded or was similar in amplitude to the preceding KCl contraction. Thereby, an active length–tension relationship [45] was obtained for each individual preparation, leading to an optimal resting tension of approximately 18 mN in carotid and 25 mN in aortic rings. The response to the final depolarization with 60 mM KCl was allowed to plateau, which occurred within 15 to 20 min, and this sustained increase in contractile force was used as submaximal reference contraction, averaging 5.6±0.1 mN in carotid and 15.5±0.4 mN in aortic rings. After repeated washouts, part of the preparations remained in control solution at pH 7.4. The other preparations were incubated in either acidic [in mM: NaCl, 137; NaHCO3, 7 (pH 7)] or alkaline [in mM: NaCl, 119; NaHCO3, 25 (pH 7.8)] isosmotic modified Krebs–Ringer bicarbonate buffered solution. Osmolality was measured with a Wescor Vapor Pressure osmometer 5520 (Wescor®, Logan, UT, USA). The actual pH was measured in samples of solutions pipetted out of the myograph chambers or checked directly in the myograph using a portable pH meter HI 8014 with microelectrode HI 1083B (HANNA® Instruments, Smithfield, RI, USA).
Experimental protocols
The rings were allowed to equilibrate for at least 10 min in one of the solutions described above, before incubation with inhibitors. Subsets of rings were incubated for 30 min with the NO synthase inhibitor N ω-nitro-l-arginine methyl ester (l-NAME, 3×10−4 M) [3, 8, 32, 35], the cyclooxygenase inhibitor meclofenamate (10−6 M) [24, 26], or the thromboxane-prostanoid (TP) receptor antagonist, S18886 (3-[(6-amino-(4-chlorobenzensulfonyl)-2-methyl-5,6,7,8-tetrahydronapht)-1-yl]propionic acid; 10−7 M) [36, 39, 49]. Relaxations were measured in preparations contracted with phenylephrine or U46619 to the level of their individual reference contraction to 60 mM KCl solution prior to the addition of increasing cumulative concentrations of acetylcholine (10−10 to 10−4 M), sodium nitroprusside (10−11 to 10−5 M), or prostacyclin (10−8 to 10−5 M; in the presence of l-NAME, meclofenamate and S18886). Contractions were induced in quiescent carotid preparations (in the presence of l-NAME) by acetylcholine (10−10 to 10−4 M) or phenylephrine (10−10 to 3×10−5 M). After maximal relaxation to sodium nitroprusside (10−5 M) followed by repeated washouts, the rings were incubated with l-NAME and contracted with the TP receptor agonist U46619 (10−10 to 3×10−6 M). These experiments were repeated after achieving partial TP receptor blockade with 10−8 or 3×10−8 M S18886.
In a subset of quiescent carotid rings, contractions were evoked by a single concentration of acetylcholine (10−5 M). In another subset of carotid arteries contracted with acetylcholine (10−5 M), the solution was pipetted out of the myograph chamber after 10 min and stored at −80°C for further analysis by enzyme-linked immunosorbent assay (ELISA) [16, 21, 25, 30].
Prostacyclin (PGI2, final concentration 10−5 M) was added to quiescent carotid preparations (in the presence of meclofenamate and absence or presence of S18886; 10−7 M) at low and high pH in the absence or presence of the prostacyclin (IP) receptor antagonist CAY10441 (10−6 M) [37].
ELISA determination of 6-keto prostaglandin F1α and thromboxane B2
The concentrations of the stable metabolites of prostacyclin and thromboxane A2 were determined in duplicates of undiluted pipetted out solution samples and assayed using commercial EIA kits (Cayman Chemical Company, Ann Arbor, MI, USA) according to the manufacturer’s instructions.
Drugs
Acetylcholine chloride, l-NAME, meclofenamate, phenylephrine and sodium nitroprusside were purchased from Sigma-Aldrich (St. Louis, MO, USA); 9,11-dideoxy-9α,11α-methanoepoxy prostaglandin F2α (U46619) was from Enzo Life Sciences (Farmingdale, NY, USA). Prostaglandin I2 sodium salt (prostacyclin, PGI2) and 4,5-dihydro-N-[4-[[4-(1-methylethoxy)phenyl]methyl]phenyl]-1H-imadazol-2-amine (CAY10441) were obtained from Cayman Chemical Company. S18886 was a kind gift from Les Laboratoires Servier (Suresnes, France). All drugs were dissolved in distilled water except U46619, and CAY10441, which were dissolved in ethanol (10−2 M). Final concentrations did not exceed 0.1% for ethanol. Prostacyclin was dissolved in basic phosphate buffered solution (pH >10.2). Concentrations are given as final molar concentration in the myograph solution.
Statistical analysis
Contractions are expressed as percent of the reference contraction to 60 mM KCl and relaxations as percentage of contractions to phenylephrine or U46619. Student’s t-test for unpaired observations was used where appropriate to analyze statistical differences between groups. Concentrations causing half-maximal responses (EC50) were calculated and compared using nonlinear regression analysis in Prism version 5 (GraphPad Software Inc., San Diego, CA, USA). Negative logarithms of EC50 are displayed as pD 2 values and the calculated maximal responses (E max) presented as percentages of reference contractions. Two-way ANOVA for the variables pH and drug were used for multiple comparisons, followed by Bonferroni post hoc analysis. Results are shown as means ± standard error of the mean (SEM), where n indicates the number of preparations from different mice. P values less than 0.05 were considered to indicate statistically significant differences.
Results
In the equilibration period and during incubation with inhibitors or antagonists, no significant shifts in baseline tension were observed due to changes in pH in either carotid or aortic rings (data not shown).
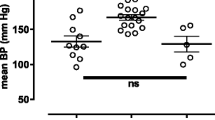
To test the responsiveness of arterial smooth muscle at different pHs, carotid rings were incubated with l-NAME (3×10−4 M). Full concentration–response curves were obtained for phenylephrine. The concentration–response curve to the α1-adrenergic agonist was shifted significantly to the left in solution with high pH compared to control, whereas at lower pH it was shifted significantly to the right; the calculated maximal response to the α1-adrenergic agonist was significantly reduced at lower pH (Fig. 1; Table 1). In further experiments comparing relaxations in phenylephrine-contracted preparations, the concentration of the α1-adrenergic agonist was adjusted to obtain a similar degree of contraction irrespective of the pH condition tested.
Endothelium-dependent responses in mouse carotid arteries
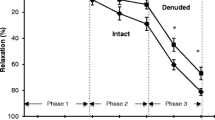
To investigate the effect of pH on endothelium-dependent responses to acetylcholine [the gold standard to evoke the release of both EDNO and EDCF [13, 23], phenylephrine-contracted preparations of carotid arteries were exposed at pH 7.0, 7.4 or 7.8, to increasing concentrations of the muscarinic agonist. The initial relaxations to 10−9 to 3×10−8 M, were not significantly different in the three pH milieus (Fig. 2a); they were followed by rebound secondary increases in tension at higher concentrations which were significantly larger in alkalosis and only marginal in amplitude at pH 7 compared to controls (Fig. 2a). Because of the similarity between the biphasic nature of the response to acetylcholine and that observed in earlier work in arteries of the spontaneously hypertensive rat and mice [8, 23, 42], these experiments were repeated in preparations treated with either the cyclooxygenase inhibitor meclofenamate (10−6 M; Fig. 2b) or the TP receptor antagonist S18886 (10−7 M; Fig. 2c); in the presence of those two agents, the response to acetylcholine was a monophasic relaxation which did not differ significantly between the three pHs (Table 1). These experiments suggested that in the range tested, pH does not affect endothelium-dependent relaxations but modulates the occurrence of endothelium-dependent contractions.
a Effect of pH on endothelium-dependent relaxations and secondary contractions to acetylcholine in control carotid artery rings contracted with phenylephrine (n=5–8), b in the presence of meclofenamate (10−6 M, n=6), and c S18886 (10−7 M, n=4–7). Data shown as means ± SEM; *P<0.05, **P<0.01 versus controls at pH 7.4
pH does not affect NO-dependent, endothelium-dependent relaxations to acetylcholine
To verify that pH does not alter the release or the action of endothelium-derived NO, similar studies were conducted in rings of mouse aorta, a preparation in which NO plays a dominant, if not exclusive role in endothelium-dependent relaxations [3, 17]. These experiments were conducted in the presence of meclofenamate (10−6 M) to prevent possible secondary endothelium-dependent contractions at higher concentrations of the muscarinic agonist [39, 42]. There were no significant differences in relaxation to acetylcholine between the three tested pH conditions (Fig. 3a). Similar results were obtained in rings contracted with 1 to 3×10−8 M U46619 (Fig. 3c; Table 1).
a Relaxations to acetylcholine in the presence of meclofenamate (10−6 M, n=6–8) and b sodium nitroprusside in the presence of the nitric oxide synthase inhibitor l-NAME (3×10−4 M, n=6) in phenylephrine contracted aortic rings. c Relaxations in the presence of meclofenamate to acetylcholine (n=6–7) and d sodium nitroprusside in the presence of l-NAME (n=6–7) in U46619 contracted aortic rings. Data shown as means ± SEM; *P<0.05, **P<0.01 versus controls at pH 7.4
The influence of pH on endothelium-independent relaxations of aortic rings was examined next in the presence of the inhibitor of NO synthases l-NAME (3×10−4 M) to prevent interference from endogenously released NO. Increasing concentrations (10−11 to 10−5 M) of the NO donor sodium nitroprusside were administered during sustained contractions to phenylephrine. Responses to lower concentrations of sodium nitroprusside were slightly but significantly altered depending on the pH milieu studied (Fig. 3b). However, there was no difference between the pH conditions in terms of maximal relaxation at the highest concentrations of this compound (Fig. 3b; Table 1). Moreover, in U46619 contracted rings, there were no significant differences in the response to sodium nitroprusside between the three pH groups (Fig. 3d). These experiments suggest that the studied changes in pH affect minimally the ability of aortic smooth muscle to relax, because they do not modify the release of endothelium-derived NO.
pH modulates EDCF-mediated, endothelium-dependent contractions
To confirm that pH changes modulate endothelium-dependent contractions, quiescent carotid rings, a blood vessel in which such responses are prominent [8, 42, 50], were incubated with l-NAME (3×10−4 M) to optimize EDCF-mediated responses [1, 39]. They were exposed to cumulatively increasing concentrations (10−10 to 10−4 M) of acetylcholine which caused concentration-dependent increases in tension, optimal at 10−5 M (Fig. 4) and prevented by either the cyclooxygenase inhibitor meclofenamate or the TP receptor antagonist S18886 (data not shown). Acetylcholine evoked significantly stronger contractions of quiescent carotid rings at the more alkaline pH, whereas the responses were significantly reduced in acidic solution (Fig. 4).
To determine the reversibility of the effect of pH changes, carotid arterial rings were exposed three times, at 30-min intervals (after re-incubation with l-NAME), to 10−5 M acetylcholine; when a maximal response was reached, which occurred in less than 10 min, the muscarinic agonist was washed out (Fig. 5). At pH 7.4, the amplitude of the contraction decreased upon repeated exposure to the muscarinic agonist (Fig. 5a). Initial contractions obtained at pH 7 were significantly smaller, but those at pH 7.8 were significantly larger than parallel first responses obtained at pH 7.4. Incubation (prior to obtaining the second consecutive response) at pH 7.8 caused a significant and reversible potentiation (Fig. 5b), while incubation at pH 7 caused a significant and reversible depression (Fig. 5c) of the contraction to acetylcholine. These experiments demonstrate that the effects of changes in pH on endothelium-dependent contractions are reversible.
Consecutive endothelium-dependent contractions evoked by acetylcholine (10−5 M, given for 10 min or less) a at pH 7.4 throughout (n=8), b at pH 7 followed by 7.8 and again 7 (n=7), or c starting at pH 7.8 followed by 7 and again 7.8 (n=7). All experiments in the presence of l-NAME (3×10−4 M). Data shown as means ± SEM; *P<0.05, **P<0.01, ***P<0.001 compared to the preceding response, †† P<0.01, ††† P<0.001 compared to the first response at pH 7.4
To compare the effect of pH on both contractions and release of prostanoids, quiescent rings of carotid arteries were exposed to a single, optimal concentration (10−5 M) of acetylcholine in the presence of l-NAME. The contractions evoked by the muscarinic agonist again were augmented significantly at pH 7.8, and significantly weaker at pH 7 compared to those observed in control experiments performed at pH 7.4 (Fig. 6a). By contrast, the amount of 6-keto prostaglandin F1α released in the bath solution upon exposure to 10−5 M acetylcholine was not significantly different under the three experimental conditions (Fig. 6b). Low levels of thromboxane B2 were measured which were not significantly affected by pH changes (Fig. 6c).
a Effect of pH on endothelium-dependent contractions of quiescent carotid artery rings (l-NAME 3×10−4 M) to 10−5 M acetylcholine (n=7–8). b Release of 6-keto prostaglandin F1α from quiescent carotid arteries following stimulation with 10−5 M acetylcholine (n=6 [in duplicates]). c Levels of thromboxane B2 in the presence of acetylcholine (n=4 [in duplicates]). Data shown as means ± SEM; **P<0.01, ***P<0.001 versus controls at pH 7.4
These results indicate that the release of EDCF is not altered by changes in pH and thus that the observed differences in response to acetylcholine must reflect differences in responsiveness of vascular smooth muscle to the endothelium-derived vasoconstrictor prostanoids.
Prostacyclin
In aortic rings incubated with l-NAME, meclofenamate and S18886, prostacyclin caused moderate decreases in tension, which were not affected significantly by the imposed pH changes (Fig. 7a) but were prevented by the IP receptor blocker CAY10441 [37] [10−6 M; data not shown].
a Relaxations to prostacyclin in aortic rings in the presence of l-NAME (3×10−4 M), meclofenamate (10−6 M) and S18886 (10−7 M, n=6). b Effect of pH on contractions to prostacyclin in quiescent carotid artery rings in the absence (n=8) and c presence (n=8) of CAY10441 (10−6 M) in addition to l-NAME and meclofenamate. Data shown as means ± SEM, **P<0.01 between groups
Contractions to prostacyclin, the prototypical EDCF in rodent arteries [16, 31], were compared at pH 7.0 and 7.8. Indeed, besides activating prostacyclin (IP) receptors, this prostanoid acts as a partial agonist at TP receptors [16]. To exclude influences of the former and completely unmask the effect on the latter, the IP receptor antagonist CAY10441 (10−6 M) was present in some experiments, in addition to l-NAME and meclofenamate (10−6 M). In quiescent carotid arteries at the lower pH, prostacyclin (10−5 M) induced contractions, which were significantly smaller than the responses observed at pH 7.8 (Fig. 7b). The IP receptor blocker CAY10441 (10−6 M) significantly enhanced the prostacyclin-induced contractions, which remained significantly smaller at pH 7 than at pH 7.8 (Fig. 7c). The TP receptor antagonist S18886 (10−7 M) abolished all contractions to prostacyclin (data not shown).
pH modulates responsiveness to partial TP receptor activation
The concentration–response curves to the full TP receptor agonist U46619 were not significantly different at pH 7 and 7.8 (Fig. 8a). Responses to increasing concentrations of U46619 were obtained either at pH 7.0 or at pH 7.8 after achieving partial blockade of TP receptors with 10−8 M S18886; under those conditions acidosis significantly reduced contractions to U46619 (Fig. 8b). Stronger blockade of TP receptors with 3×10−8 M S18886 nearly abolished the response U46169, but revealed a significantly larger reduction of the response by acidosis (Fig. 8c).
Discussion
The key finding of the present study is that the degree of endothelium-dependent contractions increases with rising pH, whereas acetylcholine-induced endothelial NO-dependent relaxations are not influenced. By contrast to the pronounced shifts to the left in alkalosis and to the right in acidosis of the concentration–response curves to phenylephrine in l-NAME treated preparations, contractions to U46619 were similar under those conditions. Partial TP receptor blockade revealed reductions in the responsiveness to the TP receptor agonist by acidosis. Likewise, the partial TP receptor activator prostacyclin caused a more pronounced contractile response at higher than at lower pH.
By contrast to the investigations in splanchnic canine veins where basal myogenic activity was modulated by alterations in pH [33, 44], in the present study resting tension was not changed after replacement of control solution either by acidic or alkaline milieus. This is explained best by the absence of myogenic tone in the murine conduit arteries studied.
The higher potency (to judge from the shift in pD 2) and efficacy (to judge from the greater maximal contraction) to the α1-adrenergic agonist phenylephrine in preparations exposed to a higher pH is in line with the initial work on pH dependency of vascular responses using the catecholamines epinephrine [4], norepinephrine [41], or adrenergic nerve stimulation [33, 43, 44, 47, 48]. Thus, the solutions used in the present study within a range of pH 7 to 7.8 have comparable effects on adrenergic activation of vascular smooth muscle as previously demonstrated — increased responses in alkalosis and decreased effects in acidosis. As in these previous studies, the current experiments represent acute effects of changes in pH on vascular reactivity ex vivo. Depending on the blood vessel studied longer term in vivo exposure to a reduced pH of the blood does not alter (mesenteric artery) or increases (pulmonary artery) adrenergic responses determined ex vivo at pH 7.4 [7]. In the pulmonary arteries, the enhanced response can be attributed to a long-term remodeling effect of acidosis [7] rather than to acute modulation of vascular tone as examined in the present study.
Endothelium-dependent effects of pH alterations were addressed in both aortae and carotid arteries focusing on NO-dependent relaxations and vasoconstrictor prostanoid-mediated endothelium-dependent contractions [8, 13, 23, 40, 42, 50], respectively. Cyclooxygenase inhibition and TP receptor antagonism rule out the contribution of EDCF to endothelium-dependent responses [23, 26, 39, 49]. In the present study, meclofenamate and S18886 facilitated endothelium-dependent relaxations to acetylcholine. In both thoracic aortae and carotid preparations, acetylcholine relaxed the tissues at similar concentrations as used in earlier work to evoke NO-dependent responses in conduit arteries of small mammals [8, 13, 23, 42]. Overall, the present findings do not indicate any direct effects of extracellular pH, in the range tested on the sensitivity of the endothelial muscarinic receptors of these arteries leading to an altered endothelial NO synthesis and release. An absence of effect of acidosis on endothelium-dependent relaxations to acetylcholine has recently been observed in small human resistance arteries [19]. The same study also found no differences in the response to the NO donor sodium nitroprusside due to changes in pH [19]. This is in keeping with the present results in the murine aorta, where pH did not affect relaxations to sodium nitroprusside during contractions to the thromboxane analog U46619 and minimal shifts in the concentration–response curves occurred only for lower concentrations of the exogenous NO donor in phenylephrine-contracted rings. Thus, the responsiveness of the vascular smooth muscle to NO is minimally affected by the changes in pH imposed in the present study, a conclusion in line with the unchanged response to endogenous NO released by acetylcholine. Likewise, the imposed changes in pH did not affect the IP receptor-mediated response to prostacyclin, confirming that they do not modify the ability to relax murine vascular smooth muscle.
The present observations in carotid arteries confirm that in the absence of cyclooxygenase inhibition or TP receptor antagonism, the response to acetylcholine of arteries with endothelium can be biphasic, whereby the initial relaxation is followed by contractions starting from 10−7 M on of the muscarinic agonist [8, 23, 40, 42, 50]. Hence, the onset and amplitude of endothelium-dependent contractions are examined best in quiescent preparations. Such experiments were performed in the presence of l-NAME to rule out the influence of NO on EDCF-mediated responses [1, 38]. The present results confirm the susceptibility of murine carotid rings to exhibit endothelium-dependent contractions upon stimulation with acetylcholine [8, 42, 50]. Meclofenamate at a final concentration of 10−6 M [26] was sufficient irrespective of pH to prevent the occurrence of endothelium-dependent contractions in both types of arteries studied. The TP receptor antagonist S18886 [36, 39, 49] had a similar abolishing effect on the contractile responses to acetylcholine in carotid arterial rings. Thus, the contractions obtained with acetylcholine in the present experiments can be attributed to the release of vasoconstrictor prostanoids (exemplified here by that of 6-keto prostaglandin F1α and thromboxane B2) and the subsequent activation of TP receptors on the vascular smooth muscle cells [1, 15, 16, 23, 26].
The present results demonstrate that, unlike endothelium-dependent relaxations, endothelium-dependent contractions to acetylcholine are pH-dependent — being stronger in alkaline than the control solution — and prevented at the lower pH studied. The effects of both acidosis and alkalosis are reversible. However, the pH changes imposed in the present study did not affect the release of EDCF. The latter conclusion is based on the observation that neither acidosis nor alkalosis caused differences in the production of vasoconstrictor prostanoids, to judge from the measured concentrations of 6-keto prostaglandin F1α — the stable metabolite of prostacyclin, a major EDCF in rodent blood vessels [16, 31] or thromboxane B2 — the stable metabolite of thromboxane A2. The low levels of the latter confirm that thromboxane A2 is not a major player in the endothelium-dependent contractions of murine arteries [22].
Taken in conjunction, the present findings make it unlikely that pH affects endothelial calcium signaling, which precedes the generation and release of both endothelium-derived relaxing and contracting factors in response to acetylcholine [46].
Prostacyclin was chosen as an endothelium-derived substance and partial TP receptor activator [15, 16, 31]. The present findings demonstrate that prostacyclin-induced contractions were weaker at lower compared to higher pH. The contractions of quiescent carotid arteries induced by the prostanoid were prevented by the TP receptor antagonist S18886 [36, 39, 49] irrespective of the experimental pH, confirming the TP receptor dependency of the response. The contractions to prostacyclin were facilitated in the presence of CAY10441 both in acidic and alkaline solution, demonstrating that IP receptors partially counteract TP receptor activation by prostacyclin. However, the relative impact of pH on the contractions to prostacyclin was comparable in the absence and presence of the IP receptor antagonist, implying that it cannot be attributed to pH dependency of the IP component of the response to the prostanoid. The latter interpretation is in line with the absence of effect of acidosis or alkalosis on the relaxations evoked by the prostanoid in the presence of S18886. Thus, the weaker response to the prototypical EDCF at lower pH must be due to an altered sensitivity to partial activation of TP receptors on vascular smooth muscle, a conclusion in line with the results obtained with the thromboxane mimetic U46619. Actually, in the absence of TP receptor blockade, the responsiveness to U46619 was comparable in the different solutions tested, which could be indicative of a pH independency of direct TP receptor activation on vascular smooth muscle. However, the full TP receptor agonist U46619 is a synthetic compound and may not completely mimic TP receptor activation by endothelium-derived partial agonists including endogenous prostaglandins, in particular, prostacyclin. In order to investigate the possible effects of pH on agonist efficacy, the contractions to U46619 were examined after a partial, progressive blockade of TP receptors with S18886. Under those conditions, the effect of pH changes on the response to the “full” agonist was comparable to that obtained on contractions to prostacyclin. The analogy with the differential impact of changes in local temperature on the response to full versus partial agonists in isolated blood vessels [11] suggests that changes in pH modulate the efficacy of vasoconstrictor agonists by altering “receptor reserve”, with alkalosis augmenting but acidosis reducing it [11], an interpretation which could also explain the observed changes in responsiveness to the α1-adrenergic agonist phenylephrine. The present findings do not permit further speculation as to the molecular changes underlying such modifications in receptor responsiveness and agonist efficacy.
In conclusion, the present study — with the limitation that it examined the impact of pH on vascular responses in conduit rather than resistance vessels — demonstrates that in murine arteries changes in pH can modulate endothelium-dependent contractions by altering the responsiveness of TP receptors on vascular smooth muscle to EDCF. In pathophysiological terms, the attenuation of endothelium-dependent vasoconstrictor responses by a lowered pH due to reduced responsiveness to EDCF resembles the blunting by acidosis of the response to sympathetic stimulation in vivo [4] and in vitro [41]. Patients with decreased blood pH are less sensitive to sympathomimetic drugs [5] and may suffer from low blood pressure. The present findings suggest that reduced or augmented responsiveness to EDCF may contribute to the hemodynamic phenotype of metabolic acidosis and alkalosis [14], respectively.
References
Auch-Schwelk W, Katusic ZS, Vanhoutte PM (1992) Nitric oxide inactivates endothelium-derived contracting factor in the rat aorta. Hypertension 19(5):442–445
Barton M, Baretella O, Meyer MR (2012) Obesity and risk of vascular disease: importance of endothelium-dependent vasoconstriction. Br J Pharmacol 165(3):591–602
Barton M, Haudenschild CC, d'Uscio LV, Shaw S, Münter K, Lüscher TF (1998) Endothelin ETA receptor blockade restores NO-mediated endothelial function and inhibits atherosclerosis in apolipoprotein E-deficient mice. Proc Natl Acad Sci U S A 95(24):14367–14372
Burget GE, Visscher MB (1927) Variations of the pH of the blood and the response of the vascular system to adrenalin. Am J Physiol 81(1):113–123
Campbell HDB, Crisp NW Jr, Weil MH, Brown EB Jr (1958) Depressed response to intravenous sympathicomimetic agents in humans during acidosis. Dis Chest 33(1):18–22
Chen G, Suzuki H, Weston AH (1988) Acetylcholine releases endothelium-derived hyperpolarizing factor and EDRF from rat blood vessels. Br J Pharmacol 95(4):1165–1174
Christou H, Reslan OM, Mam V, Tanbe AF, Vitali SH, Touma M, Arons E, Mitsialis SA, Kourembanas S, Khalil RA (2012) Improved pulmonary vascular reactivity and decreased hypertrophic remodeling during nonhypercapnic acidosis in experimental pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 302(9):L875–890
Crauwels HM, Van Hove CE, Herman AG, Bult H (2000) Heterogeneity in relaxation mechanisms in the carotid and the femoral artery of the mouse. Eur J Pharmacol 404(3):341–351
De Mey JG, Vanhoutte PM (1982) Heterogeneous behavior of the canine arterial and venous wall. Importance of the endothelium. Circ Res 51(4):439–447
Félétou M, Vanhoutte PM (1988) Endothelium-dependent hyperpolarization of canine coronary smooth muscle. Br J Pharmacol 93(3):515–524
Flavahan NA, Lindblad LE, Verbeuren TJ, Shepherd JT, Vanhoutte PM (1985) Cooling and alpha 1- and alpha 2-adrenergic responses in cutaneous veins: role of receptor reserve. Am J Physiol 249(5 Pt 2):H950–955
Furchgott RF, Vanhoutte PM (1989) Endothelium-derived relaxing and contracting factors. FASEB J 3(9):2007–2018
Furchgott RF, Zawadzki JV (1980) The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288(5789):373–376
Galla JH (2000) Metabolic alkalosis. J Am Soc Nephrol 11(2):369–375
Ge T, Hughes H, Junquero DC, Wu KK, Vanhoutte PM, Boulanger CM (1995) Endothelium-dependent contractions are associated with both augmented expression of prostaglandin H synthase-1 and hypersensitivity to prostaglandin H2 in the SHR aorta. Circ Res 76(6):1003–1010
Gluais P, Lonchampt M, Morrow JD, Vanhoutte PM, Félétou M (2005) Acetylcholine-induced endothelium-dependent contractions in the SHR aorta: the Janus face of prostacyclin. Br J Pharmacol 146(6):834–845
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC (1995) Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature 377(6546):239–242
Ignarro LJ, Buga GM, Wood KS, Byrns RE, Chaudhuri G (1987) Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A 84(24):9265–9269
Ives SJ, Andtbacka RH, Noyes RD, Morgan RG, Gifford JR, Park SY, Symons JD, Richardson RS (2013) α1-Adrenergic responsiveness in human skeletal muscle feed arteries: the impact of reducing extracellular pH. Exp Physiol 98(1):256–267
Katusic ZS, Shepherd JT, Vanhoutte PM (1988) Endothelium-dependent contractions to calcium ionophore A23187, arachidonic acid, and acetylcholine in canine basilar arteries. Stroke 19(4):476–479
Li Z, Wang Y, Vanhoutte PM (2011) Upregulation of heme oxygenase 1 by hemin impairs endothelium-dependent contractions in the aorta of the spontaneously hypertensive rat. Hypertension 58(5):926–934
Liu B, Luo W, Zhang Y, Li H, Zhu N, Huang D, Zhou Y (2012) Involvement of cyclo-oxygenase-1-mediated prostacyclin synthesis in the vasoconstrictor activity evoked by ACh in mouse arteries. Exp Physiol 97(2):277–289
Lüscher TF, Vanhoutte PM (1986) Endothelium-dependent contractions to acetylcholine in the aorta of the spontaneously hypertensive rat. Hypertension 8(4):344–348
Meyer MR, Baretella O, Prossnitz ER, Barton M (2010) Dilation of epicardial coronary arteries by the G protein-coupled estrogen receptor agonists G-1 and ICI 182,780. Pharmacology 86(1):58–64
Michel FS, Man RY, Vanhoutte PM (2007) Increased spontaneous tone in renal arteries of spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 293(3):H1673–1681
Miller VM, Vanhoutte PM (1985) Endothelium-dependent contractions to arachidonic acid are mediated by products of cyclooxygenase. Am J Physiol 248(4 Pt 2):H432–437
Moncada S, Palmer RM, Higgs EA (1988) The discovery of nitric oxide as the endogenous nitrovasodilator. Hypertension 12(4):365–372
Mulvany MJ, Halpern W (1977) Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41(1):19–26
Nagao T, Vanhoutte PM (1991) Hyperpolarization contributes to endothelium-dependent relaxations to acetylcholine in femoral veins of rats. Am J Physiol 261(4 Pt 2):H1034–1037
Qu C, Leung SW, Vanhoutte PM, Man RY (2010) Chronic inhibition of nitric-oxide synthase potentiates endothelium-dependent contractions in the rat aorta by augmenting the expression of cyclooxygenase-2. J Pharmacol Exp Ther 334(2):373–380
Rapoport RM, Williams SP (1996) Role of prostaglandins in acetylcholine-induced contraction of aorta from spontaneously hypertensive and Wistar–Kyoto rats. Hypertension 28(1):64–75
Rees DD, Palmer RM, Schulz R, Hodson HF, Moncada S (1990) Characterization of three inhibitors of endothelial nitric oxide synthase in vitro and in vivo. Br J Pharmacol 101(3):746–752
Shepherd JT, Vanhoutte PM (1975) Veins and their control. W.B. Saunders, Philadelphia
Shepherd JT, Vanhoutte PM (1979) The human cardiovascular system: facts and concepts. Raven Press, New York
Shi Y, Ku DD, Man RY, Vanhoutte PM (2006) Augmented endothelium-derived hyperpolarizing factor-mediated relaxations attenuate endothelial dysfunction in femoral and mesenteric, but not in carotid arteries from type I diabetic rats. J Pharmacol Exp Ther 318(1):276–281
Simonet S, Descombes JJ, Vallez MO, Dubuffet T, Lavielle G, Verbeuren TJ (1997) S 18886, a new thromboxane (TP)-receptor antagonist is the active isomer of S 18204 in all species, except in the guinea-pig. Adv Exp Med Biol 433:173–176
Sun D, Liu H, Yan C, Jacobson A, Ojaimi C, Huang A, Kaley G (2006) COX-2 contributes to the maintenance of flow-induced dilation in arterioles of eNOS-knockout mice. Am J Physiol Heart Circ Physiol 291(3):H1429–1435
Tang EH, Félétou M, Huang Y, Man RY, Vanhoutte PM (2005) Acetylcholine and sodium nitroprusside cause long-term inhibition of EDCF-mediated contractions. Am J Physiol Heart Circ Physiol 289(6):H2434–2440
Tang EH, Ku DD, Tipoe GL, Félétou M, Man RY, Vanhoutte PM (2005) Endothelium-dependent contractions occur in the aorta of wild-type and COX2−/− knockout but not COX1−/− knockout mice. J Cardiovasc Pharmacol 46(6):761–765
Tesfamariam B, Jakubowski JA, Cohen RA (1989) Contraction of diabetic rabbit aorta caused by endothelium-derived PGH2-TxA2. Am J Physiol 257(5 Pt 2):H1327–1333
Tobian L, Martin S, Eilers W (1959) Effect of pH on norepinephrine-induced contractions of isolated arterial smooth muscle. Am J Physiol 196(5):998–1002
Traupe T, Lang M, Goettsch W, Münter K, Morawietz H, Vetter W, Barton M (2002) Obesity increases prostanoid-mediated vasoconstriction and vascular thromboxane receptor gene expression. J Hypertens 20(11):2239–2245
Vanhoutte P, Clément D (1968) Effect of pH and PCO2 changes on the reactivity of isolated venous smooth muscle. Arch Int Physiol Biochim 76(1):144–146
Vanhoutte P, Leusen I (1967) Influence of variations of pH on the reactivity of isolated veins of the dog. C R Séances Soc Biol Fil 161(11):2318–2320
Vanhoutte P, Leusen I (1969) The reactivity of isolated venous preparations to electrical stimulation. Pflugers Arch 306(4):341–353
Vanhoutte PM, Shimokawa H, Tang EH, Félétou M (2009) Endothelial dysfunction and vascular disease. Acta Physiol (Oxf) 196(2):193–222
Vanhoutte PM, Verbeuren TJ, Webb RC (1981) Local modulation of adrenergic neuroeffector interaction in the blood vessel wall. Physiol Rev 61(1):151–247
Verbeuren TJ, Janssens WJ, Vanhoutte PM (1978) Effects of moderate acidosis on adrenergic neurotransmission in canine saphenous veins. J Pharmacol Exp Ther 206(1):105–114
Yang D, Levens N, Zhang JN, Vanhoutte PM, Félétou M (2003) Specific potentiation of endothelium-dependent contractions in SHR by tetrahydrobiopterin. Hypertension 41(1):136–142
Zhou Y, Varadharaj S, Zhao X, Parinandi N, Flavahan NA, Zweier JL (2005) Acetylcholine causes endothelium-dependent contraction of mouse arteries. Am J Physiol Heart Circ Physiol 289(3):H1027–1032
Acknowledgements
O.B. is grateful to Professor Matthias Barton for his long-time support and guidance. This study was supported by the Swiss National Science Foundation (grant PBZHP3-138754 to O.B.), the Hong Kong Research Grant Council (780410M), and by the World Class University program (R31-20029) funded by the Ministry of Education, Science and Technology, South Korea.
Disclosures
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baretella, O., Xu, A. & Vanhoutte, P.M. Acidosis prevents and alkalosis augments endothelium-dependent contractions in mouse arteries. Pflugers Arch - Eur J Physiol 466, 295–305 (2014). https://doi.org/10.1007/s00424-013-1323-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-013-1323-z