Abstract
The L-type calcium channel (LCC) plays a regulatory role in various physical and pathological processes. In the vasculature, LCCs mediate agonist-induced vascular smooth muscle contraction. However, whether LCC-mediated vessel responses to certain vasoconstrictors vary among species remains unclear. The coronary arteries were dissected from the hearts of rats and mice. Coronary arterial ring contraction was measured using the Multi Myograph system. High K+ (60 mM)-induced coronary artery contractions were stronger in rats than in mice, whereas CaCl2-induced contraction curves did not differ significantly between the two groups. Endothelin-1, U46619 (thromboxane A2 receptor agonist), and 5-hydroxytryptamine (5-HT) induced concentration-dependent vasoconstriction of coronary arterial rings in rats and mice. The vessel rings of mice were more sensitive to ET-1 and U46619 and less sensitive to 5-HT than those of rats. The LCC blocker nifedipine significantly inhibited coronary artery contractions induced by ET-1, U46619, and 5-HT. The inhibitory effect of 1 μM nifedipine on ET-1- and 5-HT-induced coronary artery contractions was stronger in mice than in rats, whereas its effect on U46619-induced vessel contractions was weaker in mice than in rats. The 5-HT2A receptor and LCC mRNA levels were higher in the coronary arteries of rats than in those of mice, whereas the expressions of the ETA and TXA2 receptors and Orai1 mRNA levels were comparable between the two groups. LCC plays an important role in coronary arterial contraction. Rats and mice show different responses to vasoconstrictors and LCC blockers, suggesting that the coronary arteries of rats and mice have different biological characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery spasm (CAS) is the main cause of vasospastic angina and is involved in the development of coronary arterial disease. CAS is characterized by increased contractility of vascular smooth muscle. Several endogenous vasoconstrictors, such as ET-1, 5-HT, and TXA2, are spasmogenic agents in coronary arteries. L-type calcium channels (LCCs) contribute to the pathogenesis of coronary artery spasm (Ito et al., 1994, Kruse et al., 1994, Kuga et al., 2000). The LCC blocker nifedipine is used to antagonize the effects of vasoconstrictor-induced vasospasm (Higashino et al., 1997). Because obtaining coronary artery segments from patients is difficult, the effect of cardiovascular drugs is normally investigated using animal models. However, differences in the vascular responses of coronary arteries to vasodilator drugs between different experimental animals have not been investigated to date. The aim of the present study was to compare the effect of nifedipine on coronary arterial contractions induced by endogenous vasoconstrictors between rats and mice.
Materials and methods
The study protocol was approved by the Experimental Animal Ethics Committee of Guangdong General Hospital (Guangzhou, People’s Republic of China).
Vessel preparation and force measurement
Male Sprague–Dawley rats (220–280 g; 8–10 weeks) or male Kunming (KM) mice (20 ± 2 g, 8–10 weeks) were housed under 12-h light–dark conditions with ad libitum access to water and food. Rats or mice were asphyxiated with CO2 and decapitated. Hearts were removed immediately and chilled in ice-cold bicarbonate buffer solution containing (in mM) NaCl (119), KCl (4.7), CaCl2 (2.5), MgCl2 (1), NaHCO3 (25), KH2PO4 (1.2), and d-glucose (11.1). The left anterior descending coronary artery was excised from the myocardium. Adherent connective tissues were removed. The endothelium was also removed and cut into two ringed segments (approximately 2 mm in length).
Each segment was mounted in a Multi Myograph system (Danish Myo Technology, Aarhus, Denmark), and changes in arterial tone were recorded. Briefly, two tungsten wires (each with a diameter of 40 μm) were inserted through the lumen of the segment, and each wire fixed to the jaws of a myograph. The organ chamber was filled with 5 mL Krebs solution, which was bubbled constantly with a mixture of 95 % O2 and 5 % CO2 and maintained at 37 °C. Each ring was stretched initially to 1.5 mN (optimal tension) and then allowed to stabilize at this baseline tone for 90 min before the start of each experiment. Each experiment was performed using rings from different rats or mice. The endothelium was removed mechanically by rubbing the luminal surface of the ring with a small stainless-steel wire. Functional removal of the endothelium was verified by the absence of the relaxant effect of acetylcholine. In experiments using a high-K+ solution, an equimolar amount of K+ replaced Na+ to retain constant ionic strength.
Quantitative real-time PCR (real-time PCR)
Total RNA was isolated from rats or mice coronary artery tissue using the Trizol reagent (Molecular Research Center, Cincinnati, OH, USA) according to the manufacturer’s instructions. Total RNA (1 μg) was reverse-transcribed in a total volume of 20 μL, and real-time PCR was performed using SYBR green fluorescence. Synthesis of specific primers (Online Resource 1) was performed by Invitrogen (Shanghai, People’s Republic of China). Each real-time PCR reaction comprised 1 μL RT product, 5 μL SYBR Green PCR Master Mix, and 400 nM forward and reverse primers. Reactions were performed using the ViiA™ 7 Dx Real-time PCR detection system (Applied Biosystems, Foster City, CA, USA) for 40 cycles (95 °C for 25 s, 58 °C for 25 s, 72 °C for 25 s) after an initial 2-min incubation at 95 °C. The fold change in expression of each gene was calculated using the 2−△△Ct method with β-actin as an internal control.
Chemicals
Endothelin-1, 9,11-dideoxy-11a,9a-epoxy-methanoprostaglandin F2a (U46619), 5-hydroxytryptamine (5-HT), nifedipine, and acetylcholine were purchased from Sigma (St. Louis, MO). U-46619 and nifedipine were dissolved in DMSO and the other agents in distilled water. Further dilution was made from a stock solution.
Data analysis
Data are expressed as the mean ± SEM. Increases in contractile force were expressed as a percentage of the mean value of two consecutive responses to 60 mM K+. Cumulative concentration-response curves were analyzed by nonlinear curve fitting using Sigmaplot 11.0 software. The constrictor concentration causing half (EC50) of the maximal response (E max) was calculated. For statistical analysis, a two-tailed Student’s t test was used. Individual concentration-response curves were also compared using a two-way analysis of variance followed by Bonferroni post-tests. Statistical significance was set at p < 0.05.
Results
High potassium-induced vasocontractile responses in the coronary arteries of rats and mice
High K+-induced coronary artery contractions (tension 6.3 ± 0.5 mN in rats and 3.4 ± 0.4 mN in mice, p < 0.05) were significantly stronger in rats than in mice (Fig. 1a). To determine the contractile sensitivity to Ca2+, coronary arterial rings were rinsed three times using a Ca2+-free solution containing 50 μM Na2-EGTA, then incubated in Ca2+-free and 60 mM K+ solution before cumulative addition of CaCl2. CaCl2-induceds contraction curves did not differ significantly between the two groups (E max 126.8 ± 5.9 % in rats and 124.9 ± 3.5 % in mice, p > 0.05) (Fig. 1b).
High potassium-induced vasocontractile responses in the coronary arteries of rats and mice. a High K+-induced contractions were markedly stronger in the coronary arteries of rats than in those of mice. b CaCl2-induced concentration-dependent contractions did not differ between the coronary arteries of rats (open circles) and mice (full circles). The graph shows the mean ± SEM of 8–12 experiments on samples from different rats. **p < 0.01 vs rat coronary arteries
Effect of endothelin-1 on coronary artery constriction in rats and mice
Endothelin-1 induced vasoconstriction in endothelium-denuded coronary arterial rings of rats and mice in a concentration-dependent manner (Fig. 2). Endothelin-1 at 100 nM induced maximal contraction in rats and at 30 nM induced maximal contraction in mice; the contractile response and sensitivity of coronary arteries to endothelin-1 were higher in mice than in rats (E max 152 ± 12 % in rats and 133 ± 11 % in mice, p < 0.05; EC50: 30.4 ± 1.3 nM in rats and 2.83 ± 0.11 nM in mice, p < 0.05).
Effect of nifedipine on the concentration-dependent vasoconstriction induced by endothelin-1 in endothelium-denuded coronary arterial rings of rats (a) and mice (b). ET-1 endothelin-1. Representative recording of ET-1-evoked concentration-dependent contraction in endothelium-denuded coronary arteries of rats and mice (left panel)
Endothelin-1-induced coronary artery contractions were markedly suppressed by 1 μM nifedipine (LCC blocker), which completely abolished 60 mM K+-induced contraction. The inhibition rate in rats was much lower than that in mice (67.19 ± 5.1 % in rats and 94.13 ± 7.8 % in mice, p < 0.05), suggesting that the contribution of calcium influx through LCCs to coronary artery constrictions evoked by endothelin-1 was less significant in rats than in mice.
Effect of U46619 on coronary artery constriction in rats and mice
In endothelium-denuded coronary arterial rings, U46619 (thromboxane A2 analogue) induced vasoconstriction in a concentration-dependent manner (Fig. 3). U46619 at 1 μM induced maximal contraction in rats, with an E max of 126 ± 6 % and an EC50 of 79.3 ± 1.3 nM. U46619 at 1 μM induced maximal contraction in mice, with an E max of 151 ± 6 % and an EC50 of 14.4 ± 0.11 nM. The E max was much higher in mice, but EC50 was lower. These results suggest that the contractile response and sensitivity of coronary arteries to U46619 were higher in mice than in rats.
Effect of nifedipine on concentration-dependent vasoconstriction induced by U46619 in endothelium-denuded coronary arterial rings in rats (a) and mice (b). Representative recording of U46619-evoked concentration-dependent contraction in endothelium-denuded coronary arteries of rats and mice (left panel)
Nifedipine at 1 μM could significantly inhibit U46619-induced coronary artery contractions. The inhibition rate was higher in rats than in mice (87.68 ± 9.1 % in rats and 35.26 ± 3.8 % in mice, p < 0.05), which suggested that the contribution of calcium influx through LCCs to coronary artery constrictions evoked by U46619 was greater in rats than in mice.
Effect of 5-HT on coronary artery constriction in rats and mice
The cumulative application of 5-HT could induce a concentration-dependent vasoconstriction in endothelium-denuded coronary arterial rings from rats and mice (Fig. 4). 5-HT at 10 μM induced maximal contraction in rats, with an E max of 125 ± 12 % and an EC50 of 0.81 ± 0.3 μM. 5-HT at 10 μM induced maximal contraction in mice, with an E max of 62 ± 11 % and an EC50 of 0.73 ± 0.2 μM. The E max of rats was much higher than that of mice, which indicates that the contractile response of coronary arteries to 5-HT was higher in rats than in mice.
Effect of nifedipine on concentration-dependent vasoconstriction induced by 5-HT in endothelium-denuded coronary arterial rings in rats (a) and mice (b). Representative recording of 5-HT-evoked concentration-dependent contraction in endothelium-denuded coronary arteries of rats and mice (left panel)
5-HT-induced vasocontractions were significantly suppressed by nifedipine at 1 μM. The inhibition rate was lower in rats than in mice (77.96 ± 3.8 % in rats and 94.50 ± 9.1 % in mice, p < 0.05). These results suggest that the contribution of calcium influx through LCCs to coronary artery constrictions induced by 5-HT was greater in mice than in rats.
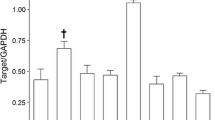
Expression of relative receptors and calcium channels in the coronary arteries of rats and mice
The 5-HT2A receptor and LCC mRNA levels were higher in the coronary arteries of rats than in those of mice, whereas the mRNA levels of the ETA receptor, TXA2 receptor, and Orai1 were comparable between the two groups (Fig. 5).
Discussion
LCCs are widely expressed in a variety of cells, especially in cardiomyocytes and SMCs (Benitah et al., 2010, Matchkov et al., 2012). The LCC is considered a main path for Ca2+ entry, which affects arterial SMC contraction. Coronary spasm is caused by endogenous vasoconstrictor-induced contraction, and LCC blockers are used to reverse vasospasm.
Rats and mice are widely used as animal models in scientific research; however, differences between species result in variation in the responses to certain stimuli. In the present study, we showed that high K+-induced vasoconstriction was stronger in rats than in mice, whereas CaCl2-induced vasoconstriction, which represents the sensitivity of vessels to Ca2+, did not differ significantly between rats and mice. High K+-induced vasoconstriction is mainly mediated by LCCs, and our results showed that LCC mRNA levels were higher in rats than in mice.
The endogenous vasoconstrictors ET-1, U46619, and 5-HT induced concentration-dependent coronary arterial contraction in rats and mice, but the responses of the vessels were different. The concentration of ET-1 producing maximal contraction, the E max, and the EC50 were higher in rats than in mice, which suggests that the coronary artery is more sensitive to ET-1 in mice than in rats. Similarly, we found that the vasoconstrictions caused by U46619 were more significant in mice than in rats. By contrast, 5-HT had a stronger effect on inducing vessel contractions in rats than in mice. Nifedipine suppressed vasoconstrictor-induced contraction, and the inhibitory effect on ET-1- and 5-HT-induced contractions was markedly stronger in mice than in rats; however, the effect of nifedipine on U46619-induced contractions was weaker in mice than in rats.
ET-1, U46619, and 5-HT are all powerful vasoconstrictors, and their effects are mediated by the ETA, TXA2R, and 5-HT2A receptors, respectively (Halcox et al., 2001, Katugampola and Davenport, 2001, Halcox et al., 2007, Nichols and Nichols, 2008). We hypothesized that the expression of these receptors may differ between rats and mice; however, our results showed that only 5-HT2A was expressed at higher levels in rats than in mice, which could explain the greater vasoconstrictions induced by 5-HT in rats than in mice. The expression of the ETA and TXA2 receptors was comparable between these two species.
These receptors belong to the G protein-coupled receptor family, and their activation upregulates the expression of inositol triphosphate (IP3) and 1,2-diacylglycerol (DAG) through the activation of phospholipase C and hydrolyzation of PIP2.
DAG can activate protein kinase C (PKC) (Somlyo and Somlyo, 2003). PKC phosphorylates CPI-17, which inhibits myosin light chain (MLC) phosphatase, promotes the phosphorylation of MLC, and enhances VSM contraction (Salamanca and Khalil, 2005). The PKC signaling pathway is involved in the vasoconstriction induced by ET-1 and U46619 (Kizub et al., 2014).
IP3 can induce an increase of intracellular Ca2+ concentration, which is mediated by the release of Ca2+ from the sarcoplasmic reticulum or Ca2+ influx through voltage-gated calcium channels. In the present study, we showed that LCC-mediated coronary artery contractility differs between rats and mice; however, the underlying mechanism is not clear. The inability of nifedipine to completely block vasoconstrictor-induced coronary contractions indicates that other ion channels may mediate Ca2+ entry. Research advances in the field of store-operated calcium entry (SOCE) have identified Orai1 and STIM1 as mediators of SOCE, and their important role in many cardiovascular diseases has been reported (Bolotina, 2012, Soboloff et al., 2012). Recently, Smani et al. (Dominguez-Rodriguez et al., 2012) showed that the store-operated calcium channel (SOCC) contributes to urotensin-II (UII)-induced rat coronary arterial contractions. In addition, SOCC has been reported to be involved in other vessel contractions (such as basilar artery, pulmonary artery) induced by endogenous vasoconstrictors ET-1, 5-HT, and U46619 (Elmoselhi and Grover, 1997, Kawanabe et al., 2006, Alapati et al., 2009). Therefore, the possible involvement of SOCC in regulating the extracellular Ca2+ influx induced by vasoconstrictors in the present study may have contributed to the differences in contractility between rats and mice. However, we found no differences in Orai1 mRNA expression levels between rats and mice.
Because both IP3 and PKC can mediate vasoconstriction, which signaling pathway plays a dominant role remains unclear. In the present study, differences in vasoconstriction between rats and mice may have been dependent on the different signal transduction pathways activated in each species.
ET-1, 5-HT, and U46619 had different effects on inducing the contraction of coronary arteries in rats and mice. This could have been partly due to differences in the expression of LCCs between these two species; however, the specific underlying mechanism remains elusive and further investigation is necessary to clarify these issues.
References
Alapati VR, McKenzie C, Blair A, Kenny D, MacDonald A, Shaw AM (2009) Mechanisms of U46619- and 5-HT-induced contraction of bovine pulmonary arteries: role of chloride ions. Br J Pharmacol 151:1224–1234
Benitah JP, Alvarez JL, Gomez AM (2010) L-type Ca2+ current in ventricular cardiomyocytes. J Mol Cell Cardiol 48:26–36
Bolotina VM (2012) Orai1, STIM1, and iPLA2 determine arterial vasoconstriction. Arterioscler Thromb Vasc Biol 32:1066–1067
Dominguez-Rodriguez A, Diaz I, Rodriguez-Moyano M, Calderon-Sanchez E, Rosado JA, Ordonez A, Smani T (2012) Urotensin-II signaling mechanism in rat coronary artery: role of STIM1 and Orai1-dependent store operated calcium influx in vasoconstriction. Arterioscler Thromb Vasc Biol 32:1325–1332
Elmoselhi AB, Grover AK (1997) Endothelin contraction in pig coronary artery: receptor types and Ca(2+)-mobilization. Mol Cell Biochem 176:29–33
Halcox JP, Nour KR, Zalos G, Quyyumi AA (2001) Coronary vasodilation and improvement in endothelial dysfunction with endothelin ET(A) receptor blockade. Circ Res 89:969–976
Halcox JP, Nour KR, Zalos G, Quyyumi AA (2007) Endogenous endothelin in human coronary vascular function: differential contribution of endothelin receptor types A and B. Hypertension 49:1134–1141
Higashino R, Sato R, Jin H, Inoue N, Fukuta Y, Kurimoto T, Tamaki H (1997) Inhibitory effects of efonidipine hydrochloride on contraction induced by several vasoconstrictors in porcine coronary artery: comparison with effects of nifedipine and nisoldipine. J Cardiovasc Pharmacol 29:624–630
Ito A, Shimokawa H, Nakaike R, Fukai T, Sakata M, Takayanagi T, Egashira K, Takeshita A (1994) Role of protein kinase C-mediated pathway in the pathogenesis of coronary artery spasm in a swine model. Circulation 90:2425–2431
Katugampola SD, Davenport AP (2001) Thromboxane receptor density is increased in human cardiovascular disease with evidence for inhibition at therapeutic concentrations by the AT(1) receptor antagonist losartan. Br J Pharmacol 134:1385–1392
Kawanabe Y, Masaki T, Hashimoto N (2006) Involvement of phospholipase C in endothelin 1-induced stimulation of Ca++ channels and basilar artery contraction in rabbits. J Neurosurg 105:288–293
Kizub IV, Klymenko KI, Soloviev AI (2014) Protein kinase C in enhanced vascular tone in diabetes mellitus. Int J Cardiol 174:230–242
Kruse HJ, Bauriedel G, Heimerl J, Hofling B, Weber PC (1994) Role of L-type calcium channels on stimulated calcium influx and on proliferative activity of human coronary smooth muscle cells. J Cardiovasc Pharmacol 24:328–335
Kuga T, Shimokawa H, Hirakawa Y, Kadokami Y, Arai Y, Fukumoto Y, Kuwata K, Kozai T, Egashira K, Takeshita A (2000) Increased expression of L-type calcium channels in vascular smooth muscle cells at spastic site in a porcine model of coronary artery spasm. J Cardiovasc Pharmacol 35:822–828
Matchkov VV, Kudryavtseva O, Aalkjaer C (2012) Intracellular Ca2+ signalling and phenotype of vascular smooth muscle cells. Basic Clin Pharmacol Toxicol 110:42–48
Nichols DE, Nichols CD (2008) Serotonin receptors. Chem Rev 108:1614–1641
Salamanca DA, Khalil RA (2005) Protein kinase C isoforms as specific targets for modulation of vascular smooth muscle function in hypertension. Biochem Pharmacol 70:1537–1547
Soboloff J, Rothberg BS, Madesh M, Gill DL (2012) STIM proteins: dynamic calcium signal transducers. Nat Rev Mol Cell Biol 13:549–565
Somlyo AP, Somlyo AV (2003) Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev 83:1325–1358
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant numbers 81273516, 81270222, 81302779, and 81470440) and by Guangdong Provincial Natural Science Foundation (S2013010014762 and S2013040014689).
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Hui Yang and Su-Juan Kuang contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 17.8 kb)
Rights and permissions
About this article
Cite this article
Yang, H., Kuang, SJ., Rao, F. et al. Species-specific differences in the role of L-type Ca2+ channels in the regulation of coronary arterial smooth muscle contraction. Naunyn-Schmiedeberg's Arch Pharmacol 389, 151–157 (2016). https://doi.org/10.1007/s00210-015-1173-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-015-1173-7