Abstract
Cannabinoids have potent vasodilatory actions in a variety of vascular preparations. Their mechanism of action, however, is complex. Apart from acting on vascular smooth muscle or endothelial cannabinoid receptors, several studies point to the activation of type 1 vanilloid (TRPV1) receptors on primary afferent perivascular nerves, stimulating the release of calcitonin gene-related peptide (CGRP). In the present study, the direct influence of the cannabinoid methanandamide and the neuropeptide CGRP on the membrane potassium ion (K+) currents of rat mesenteric myocytes was explored. Methanandamide (10 μM) decreased outward K+ currents, an effect similar to that observed in smooth muscle cells from the rat aorta. Conversely, CGRP (10 nM) significantly increased whole-cell K+ currents and this effect was abolished by preexposure to tetraethylammonium chloride (1 mM) or iberiotoxin (100 nM), inhibitors of large-conductance calcium-dependent K (BKCa) channels but not by glibenclamide (10 μM), an inhibitor of ATP-dependent K channels. In the presence of the CGRP receptor antagonist CGRP8-37 (100 nM), the adenylyl cyclase inhibitor SQ22536 (100 μM), or the protein kinase A inhibitor Rp-cAMPS (10 μM), CGRP had no effect. These findings show that methanandamide does not increase membrane K+ currents in smooth muscle cells of small mesenteric arteries, supporting an indirect mechanism for the reported hyperpolarizing influence in this vessel. Moreover, CGRP acts directly on these smooth muscle cells by increasing BKCa channel activity in a CGRP receptor and cyclic adenosine monophosphate-dependent way. Collectively, these data indicate that methanandamide relaxes and hyperpolarizes intact mesenteric vessels by releasing CGRP from perivascular nerves.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anandamide has been identified as an endogenous counterpart of Δ9-tetrahydrocannabinol, the psychoactive component of marijuana. The endocannabinoid is synthesized by cleavage of the lipid precursor arachidonyl phosphatidylethanolamine and is metabolized relatively quickly to arachidonic acid and ethanolamine. The potent vasodilatory influence of anandamide has been shown in a variety of isolated vascular preparations. Its mechanism of action, however, is complex and seems to vary with species, vessel type, and even vessel size [19, 33]. In rabbit pial arterioles and mesenteric arteries, the anandamide-induced vasodilatation is mediated by the generation of vasodilator eicosanoids, since it is blocked by indomethacin and diclofenac [4, 6]. Similarly, in isolated bovine coronary arteries, the vasorelaxant effect of anandamide has been suggested to be due to its hydrolysis to arachidonic acid and further conversion to vasodilatory eicosanoids [21]. In rat mesenteric arteries, however, the vasorelaxing influence of anandamide is unaffected by cyclooxygenase inhibition [36]. Moreover, also the stable analogue of anandamide, methanadamide, is a powerful vasodilator of these vessels [24].
Endogenous, plant-derived and synthetic cannabinoids have been reported to target receptors different from the classical CB1 and CB2 receptors. In the rat mesenteric and coronary circulation, a novel non-CB1/non-CB2 receptor present on endothelial cells has been shown to be involved in vasorelaxation [19]. Furthermore, an action on other receptors and membrane proteins was described. Cannabinoids have been shown to activate endothelial TRPV4 receptors [34] and endothelial peroxisome proliferator-activated receptor gamma [20], and anandamide has been demonstrated to bind to serotonin (5-HT)-3 receptors [5] and modulate the activity of the NMDA receptor [10]. Furthermore, stimulation of TRPV1 receptors on perivascular sensory nerves accounts for the vasorelaxing influence of anandamide [40]. Other studies showed that cannabinoids directly inhibit calcium channels [2, 8] and activate various K+ channels [25, 26, 37]—an influence which might also account for its vasorelaxant action. By contrast, cannabinoids have direct inhibitory effects on delayed rectifier K+ currents in freshly isolated rat aortic smooth muscle cells [3].
Calcitonin gene-related peptide (CGRP) is a 37-amino acid peptide that is generated by alternative splicing of the calcitonin gene transcripts. As a neurotransmitter, it is localized predominantly in sensory nerves, innervating various tissues and blood vessels. In rat hepatic and small mesenteric arteries, the vasorelaxant influence of anandamide was antagonized by the TRPV1 receptor antagonist capsazepine and the CGRP receptor antagonist CGRP(8-37) but not by the classical CB1 receptor antagonist SR141716A [40]. It was proposed, therefore, that cannabinoids exert their relaxing influence by stimulating the release of CGRP from perivascular nerves [40].
The mechanism involved in vasorelaxation to CGRP seems to vary among species and vessel types. In the rat aorta [9] and pulmonary arteries [38] and human omental and bovine retinal arteries [1], CGRP interacts with endothelial receptors stimulating the release of endothelium-derived relaxing factors, as both endothelium removal and blocking NO synthesis significantly reduced vasorelaxation. By contrast, in cat cerebral, pig coronary, and rat mesenteric vessels, CGRP acts directly on the smooth muscle cells. A number of studies have shown that CGRP relaxes tension by increasing the cyclic AMP content in vascular smooth muscle [13, 14, 39]. The resultant activation of protein kinase A (PKA) and PKA-dependent phosphorylation has been shown to open ATP-dependent K+ (KATP) channels [18, 23] hyperpolarizing and relaxing the tissue [35]. In line with this view, we have shown that the hyperpolarization of isolated rat gastric and small mesenteric arteries evoked by methanadamide was abolished by capsazepine [3]. Exogenous CGRP produced a hyperpolarization of the smooth muscle cells of comparable time course and magnitude, and both methanandamide- and CGRP-induced membrane potential changes were sensitive to the KATP channel inhibitor glibenclamide. However, two studies on isolated rat and porcine coronary arteries have failed to demonstrate KATP channel opening in CGRP-induced vasorelaxation [14, 22]. CGRP might also mediate relaxation by activation of large-conductance calcium-dependent K (BKCa) channels, by inhibition of voltage-gated calcium channels [2] or by decreasing the Ca2+ sensitivity of the contractile apparatus [30]. In rat gastric arteries, we found the vasorelaxation to CGRP to be partly sensitive to low concentrations of tetraethylammonium chloride (TEA), suggesting involvement of BKCa channel activation [2]. In a number of vascular preparations, PKA-dependent vasodilators have been shown to activate smooth muscle BKCa channels [28].
In the present experiments, we explored possible direct actions of methanandamide and of CGRP on rat small mesenteric artery smooth muscle cells by comparing their effects on whole-cell K+ currents in freshly isolated myocytes. We specifically addressed the question whether CGRP might activate BKCa currents in these cells.
Materials and methods
Cell isolation
Smooth muscle cells from rat small mesenteric arteries were dissociated on the day of the experiments. The animals were treated in accordance with the Guiding Principles for the Care and Use of Animals (published by National Academy Press, 2101 Constitution Ave, NW, Washington, DC 20055, USA, 1996) and the experiments were approved by the ethical committee on animal research of Ghent University. The animals were anesthetized by a lethal dose (200 mg kg−1) of pentobarbitone and killed by cervical dislocation. Third-order branches of the superior mesenteric artery from 2–3-month-old female Wistar rats were excised and placed in a chilled solution containing (in millimolars): NaCl, 135; KCl, 5; NaHCO3, 20; CaCl2, 2.5; MgSO4·7H2O, 1.3; KH2PO4, 1.2; EDTA, 0.026; glucose, 10, which was continuously bubbled with 95% O2/5% CO2. The vessels were carefully cleared of adherent fat and connective tissue and cut into small pieces. The artery segments were subsequently transferred to cold (4°C) low calcium dissociation medium (DM) containing (in millimolars): NaCl, 110; KCl, 5; CaCl2, 0.16; MgCl2, 2; KH2PO4, 0.5; EDTA, 0.49; NaH2PO4, 0.5; taurine, 10; HEPES, 10; glucose, 10, titrated to pH 7.0. The small pieces were allowed to rest in this medium for 30 min. The tissue was then transferred to fresh DM supplemented with papain (17 U/ml) and bovine serum albumin (2 mg/ml) for 20 min, after which dithiothreitol was added from a concentrated stock solution to a final concentration of 6.7 mM, and the mixture was warmed to 37°C for 20 min. The partially digested tissue was subsequently washed twice in cold DM. After this, collagenase (410 U/ml) and hyaluronidase (330 U/ml) were added, and the mixture was warmed to 37°C for 20 min. The digested tissue was washed three times in cold DM. After this, gentle trituration with a wide-bore Pasteur pipette yielded a suspension of single cells, which was kept at 4°C in the low-Ca2+ medium.
Electrophysiological recordings
Electrophysiological recordings were performed as previously described [32]. Briefly, part of the cell suspension was pipetted into a perfusion chamber fixed to the stage of an inverted microscope (Nikon, Diaphot). After 10 min, allowing the cells to adhere to the glass bottom of the chamber, the cells were superfused with a normal calcium-containing solution containing (in millimolars): NaCl, 140; KCl, 5.4; CaCl2, 1.8; MgCl, 1; HEPES, 10; glucose, 10, pH = 7.4.
Whole-cell membrane currents were recorded at room temperature using the conventional patch clamp technique. Borosilicate glass capillaries were used. Pipettes were attached to the headstage of an EPC-9 patch clamp amplifier (HEKA, Lambrecht/Pfalz, Germany). Pipette resistance ranged 3–5 MΩ after fire polishing. The composition of the pipette solution for conventional whole-cell recording was (in millimolars): KCl, 102; K+ (from KOH), 38; EGTA, 10; NaCl, 10; CaCl2, 1; HEPES, 10; Na2GTP, 0.2; NaADP, 0.1; Na2ATP, 3; MgCl2, 3 (pH 7.2, free Ca2+ = 17.1 nM). Pipettes were coated with beeswax. After breaking in, the cell membrane capacitance was measured from the capacitive transient using the automatic compensation procedures of the EPC-9 amplifier. Series resistance was compensated by 2–30%. Membrane currents were evoked by stepping the membrane potential from a holding potential of −70 mV for 200 ms to various test potentials between −110 and +60 mV, in 10-mV increments at 3-s intervals. Currents were filtered at 2.3 kHz and followed on computer monitor. Membrane currents were sampled at 5 kHz, recorded on hard disk, and analyzed using the Review program of the EPC-9 system. Current values given in the “Results” represent the steady state current, measured as the average current during the terminal 50-ms portion of the voltage step. In some experiments, measurements of the myocyte membrane potential were performed with the whole-cell patch configuration in current clamp mode.
Drugs
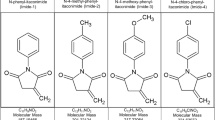
Papain, BSA, dithiothreitol, collagenase (type VIII), hyaluronidase (type I-S), glibenclamide, TEA, 4-aminopyridine (4-AP), SQ22536, and adenosine 5′-triphosphate disodium salt (ATP) were obtained from Sigma Aldrich (St. Louis, MO, USA). Calcitonin gene-related peptide (CGRP rat), iberiotoxin, CGRP8-37, Rp-cAMPS, and R-(+)-methanandamide were obtained from Tocris (Bristol, UK).
The influence of a drug was investigated by adding the appropriate amount from a stock solution to a reservoir containing equilibrated superfusion solution a few seconds before use. Preexposure times to the various blockers were at least 10 min. During superfusion, membrane potential was stepped to 60 mV at 20-s interval, in order to observe the influence on the corresponding current and to verify that a steady state effect was reached before recordings of the current family were started. The influences of methanandamide and CGRP reached steady state 4 to 7 min after adding these substances to the superfusate.
Stock solutions of methanandamide were made in anhydrous ethanol, while glibenclamide was dissolved in dimethyl sulfoxide. The final concentration of solvent never exceeded 0.1%. CGRP, iberiotoxin, TEA-Cl, and Rp-cAMPS were dissolved in water. 4-AP was added as a solid to the external medium. All concentrations are expressed as final molar concentrations in the superfusate.
Statistics
Results are presented as normalized (i.e., picoamperes per picofarad) means ± s.e. mean. Statistically significant differences are evaluated using Student’s t test for paired or unpaired observations, as appropriate. A P value <0.05 indicates a significant difference. n represents the number of cells.
Results
Freshly isolated smooth muscle cells from small mesenteric arteries were superfused at least 10 min with the control solution before measurements were started.
Influence of methanandamide and CGRP on membrane currents
Cells were clamped at a holding potential of −70 mV. Depolarizing voltage steps of increasing amplitude resulted in the activation of a family of outward currents which displayed graded voltage-dependent activation kinetics and showed little inactivation during the 200-ms test pulse (Fig. 1a).
Influence of methanandamide on I K. a Representative current traces from a small mesenteric artery myocyte in control conditions (Co) and in the presence of methanandamide (Me, 10 μM). b Mean normalized current (I)–voltage (V) plot showing the influence of methanandamide on the steady state current. Each point represents the mean ± s.e. mean from four cells. *P < 0.05, statistically significant from control value. Inset shows the difference current (Co–Me) on an extended current axis
Influence of methanandamide
The addition of methanandamide (10 μM) to the bath fluid decreased outward K+ currents of the smooth muscle cells (Fig. 1a). The current block by methanandamide reached a steady state approximately 5 min after its addition to the superfusate. As we have described for smooth muscle cells from rat aorta [32], the inhibitory influence of the cannabinoid was most pronounced on current inactivation during the 200-ms depolarizing step (Fig. 1a). In four experiments, the mean current amplitude measured at the end of the voltage step to +60 mV decreased from 19.3 ± 2.6 pA/pF in control conditions to 10.5 ± 0.5 pA/pF in the presence of methanandamide. The I–V plot (Fig. 1b) revealed a statistically significant inhibition (P < 0.05) in the potential range of −20 to +60 mV. The methanandamide-sensitive (difference) current reversed at −72 mV (Fig. 1b inset), indicative for inhibition of a K+ current.
In the continuous presence of iberiotoxin (10 nM), a selective BKCa channel inhibitor, inhibition of K+ currents by methanandamide was still present (Fig. 2a). Moreover, after preexposure to both 1 mM TEA, at this concentration acting as an inhibitor of BKCa channels [15], combined with the KATP channel inhibitor glibenclamide (10 μM), methanandamide still significantly decreased K+ currents (Fig. 2b). Conversely, after preexposure to 4-AP (5 mM), the influence of methanandamide was totally abolished (Fig. 2c). These experiments, therefore, point to an inhibition of delayed rectifier K+ (Kv) currents by methanandamide. In rat aortic smooth muscle cells, indeed, anandamide and methanandamide have been shown to directly affect Kv channels [32].
Influence of methanandamide (Me, 10 μM) after blocking BKCa, KATP, and Kv. a Mean normalized current (I)–V plot showing the influence of the cannabinoid after preexposing the myocytes to iberiotoxin (Ibx, 100 nM). b Mean normalized I–V plot showing the influence of methanandamide in the combined presence of TEA (1 mM) and glibenclamide (10 μM). Mean normalized I–V plot showing the influence of methanandamide after preexposure to 4-AP (5 mM). Each point represents the mean ± s.e. mean from 7 (a) or 5 (b, c) cells. *P < 0.05 and **P < 0.01, statistically significant from control value
Influence of CGRP
Application of the neuropeptide CGRP (10 nM) significantly increased whole-cell currents in mesenteric artery smooth muscle cells. Typical traces, obtained after reaching a steady state (which lasted approximately 6 min after adding CGRP to the superfusate), are shown in Fig. 3a. In eight cells, the mean current amplitude measured at the end of the voltage step to +60 mV was increased to 220% of control levels (Fig. 3b). The I–V plot showed a statistically significant increase (P < 0.05) in the potential range from +40 to +60 mV. The CGRP-induced (difference) current appeared on depolarization beyond +10 mV and showed pronounced outward rectification. These features suggest the involvement of a voltage-dependent potassium channel such as BKCa [17].
Influence of CGRP on I K. a Representative current traces from a myocyte in control conditions (Co) and in the presence of CGRP (10 nM). b Mean normalized current (I)–V plot showing the influence of CGRP, 10 nM. Each point represents the mean ± s.e. mean from eight cells. *P < 0.05 and **P < 0.02, statistically significant from control value
In a next series of experiments, the cells were preexposed to either 1 mM TEA or to the more selective BKCa channel blocker iberiotoxin (100 nM). Both substances significantly decreased BKCa current, as also reflected by the smoother (less noisy) appearance of the current traces in the presence of the inhibitors (Fig. 4a, c). In the presence of TEA, the mean I K at +60 mV decreased from 22.6 ± 4.6 to 9.3 ± 2.0 pA/pF. Application of iberiotoxin decreased the I K at +60 mV from 31.7 ± 7.3 to 23.4 ± 8.0 pA/pF. In the continuous presence of either TEA or iberiotoxin, the additional application of CGRP had no effect (Fig. 4).
Influence of CGRP after inhibition of BKCa. channels. a Representative current traces from a myocyte in control conditions (Co), in the presence of TEA (1 mM), and after extra addition of CGRP (10 nM). b Mean normalized current (I)–V plot showing the effect of TEA and of additional exposure to CGRP. Each point represents the mean ± s.e. mean from three cells. c Representative current traces from a myocyte in control conditions (Co), in the presence of iberiotoxin (Ibx, 100 nM) and after extra addition of CGRP (10 nM). d Mean normalized current (I)–V plot showing the effect of iberiotoxin and of additional exposure to CGRP. Each point represents the mean ± s.e. mean from five cells. *P < 0.05 and **P < 0.02, statistically significant from control value
In six cells, the influence of addition of CGRP was investigated in the presence of the inhibitor of KATP channels, glibenclamide (10 μM). Preexposure to glibenclamide did not influence control currents. In the presence of glibenclamide, CGRP increased the mean current at +60 mV from 15.8 ± 3.2 to 25.3 ± 6.4 pA/pF (Fig. 5a), i.e., to 160% of the control.
Influence of inhibition of KATP channels and the CGRP receptor. a Mean normalized current (I)–V plot showing the effect of CGRP in the presence of glibenclamide (Glib, 10 μM). b. Mean normalized current (I)–V plot showing the lack of effect of CGRP in the presence of CGRP8-37 (100 μM). Each point represents the mean ± s.e. mean from four (a) or five (b) cells. *P < 0.05, statistically significant from control value
CGRP acts by stimulating the CGRP receptor and the adenylyl cyclase pathway
In order to verify whether the effect of the neuropeptide is receptor-mediated, the CGRP receptor antagonist CGRP8-37 was applied. The mean I–V relationships obtained in five cells are shown in Fig. 5b. Preexposure to 100 nM CGRP8-37 completely prevented the current potentiation by CGRP.
In five cells, the influence of CGRP was tested after preexposure to 100 μM SQ22536, an adenylyl cyclase inhibitor. The compound significantly decreased outward K+ currents in the +40 to +60 mV range (Fig. 6a). The mean I K at +60 mV decreased from 31.5 ± 4.6 to 21.0 ± 2.9 pA/pF. A direct influence of SQ22536 on BKCa channels was excluded since preexposure to iberiotoxin did not block the effect of SQ22536 (Fig. 6b). In the continuous presence of SQ22536, CGRP had no effect (Fig. 6a). Currents in the combined presence of SQ22536 and CGRP were not significantly different from currents in the presence of SQ22536 alone.
Influence of inhibition of adenylyl cyclase or PKA. a Mean normalized current (I)–V plot showing the influence of CGRP (10 nM) after preexposure to SQ22536 (100 μM). b Mean normalized I–V plot showing the influence of SQ22536 (100 μM) after inhibition of BKCa channels with iberiotoxin (Ibx, 100 nM). c Mean normalized I–V plot showing the influence of CGRP (10 nM) after preexposure to Rp-cAMPS (10 μM). d Mean normalized I–V plot showing the influence of Rp-cAMPS (10 μM) after inhibition of BKCa channels with iberiotoxin (Ibx, 100 nM). In a–d, each point represents the mean ± s.e. mean from five cells. *P < 0.05 and **P < 0.01 denote current value statistically significant from the control value (a, c) or current in the presence of Ibx (b, d)
In five cells, the influence of the PKA inhibitor Rp-cAMPS (10 μM) was tested. The compound significantly decreased the control currents (Fig. 6c). A direct influence of Rp-cAMPS on BKCa channels was excluded since preexposure to iberiotoxin did not block the influence of Rp-cAMPS (Fig. 6d). Furthermore, after preexposure to Rp-cAMPS, CGRP failed to increase K+ currents (Fig. 6c). The currents in the combined presence of Rp-cAMPS and CGRP were not significantly different from currents in the presence of Rp-cAMPS alone.
Influence of methanandamide and CGRP on membrane potential
Some isolated resting myocytes were current clamped at 0 pA to measure membrane potential. Representative traces from two cells are shown in Fig. 7. In three cells, the application of methanandamide (10 μM) failed to alter the membrane potential (−35.5 ± 4.8 mV 5 min after addition of the cannabinoid, vs. −35.2 ± 4.3 mV in control conditions). Conversely, in three other cells, the addition of CGRP (10 nM) slowly hyperpolarized the membrane potential from −30.4 + 2.3 to −37.2 + 3.2 mV as measured 5 min after application of the neuropeptide (cf. Fig. 7).
Discussion
The present findings show that the cannabinoid methanandamide fails to increase membrane K+ currents and fails to hyperpolarize the membrane potential of isolated smooth muscle cells of small mesenteric arteries. Moreover, they reveal that the neuropeptide CGRP is acting specifically and directly on these cells by increasing the BKCa channel activity in a receptor-, cyclic adenosine monophosphate (cAMP)-, and PKA-dependent way (Fig. 8). This is consistent with earlier studies suggesting that methanandamide relaxes and hyperpolarizes intact rat mesenteric vessels by releasing the neuropeptide from perivascular nerves.
Findings of the present study as related to possible mechanisms for cannabinoid-induced vasorelaxation. Cannabinoids may activate classical CB1 or CB2 receptors of the vascular smooth muscle cells. Various cannabinoids have also been shown to activate non-CB1/non-CB2 (CBx) receptors and TRPV 4 receptors of the endothelial cells, causing the release of the endothelial relaxing factors NO and PGI 2 and activating the EDHF pathway. In addition, activation of TRPV 1 receptors on perivascular nerves has been shown, stimulating the release of vasodilator neuropeptides such as CGRP. In the present study, it is concluded that the cannabinoid methanandamide decreases delayed rectifier (K v ) currents of small mesenteric artery smooth myocytes and that CGRP causes BK Ca activation in a receptor-, cAMP-, and PKA-dependent way
In the present study, the stable cannabinoid derivative methanandamide was found to decrease K+ current in isolated smooth muscle cells from small mesenteric arteries. A similar influence has been described for smooth muscle cells isolated from the aorta of the rat [32]. In the cited study, detailed investigations using the blockers TEA and 4-aminopyridine have shown a direct influence of cannabinoids on the delayed rectifier K+ channels, independent from their possible interaction with cannabinoid receptors. In the present study, neither iberiotoxin nor the combined presence of TEA (1 mM) and glibenclamide were able to affect the influence of methanandamide, while it was completely abrogated after preexposure to 4-AP. We propose, therefore, a similar inhibition of the delayed rectifier in mesenteric artery myocytes, although this was not further investigated.
It has been shown that the mechanism of vasorelaxation to cannabinoids differs between conduit and resistance mesenteric arteries [19]. Moreover, in a previous study, we have shown that anandamide and methanandamide did not notably alter membrane potential of the smooth muscle of the main mesenteric artery, while the cannabinoids caused a substantial and endothelium-independent hyperpolarization in small mesenteric arteries [33]. The present findings, in which a similar inhibition of K+ current was found in smooth muscle cells from resistance arteries as was described for aortic smooth muscle cells, strongly argue against a direct hyperpolarizing influence of methanandamide on the smooth muscle cells from small mesenteric arteries. In the previous microelectrode study, the anandamide-induced hyperpolarization was insensitive to the classical CB1 receptor antagonist SR141716A but fully blocked by capsazepine [33], suggesting that the substance acts indirectly by stimulation of TRPV1 receptors on perivascular sensory nerves with the subsequent release of the vasodilator neurotransmitter CGRP [24, 33, 40]. Moreover, after prolonged exposure of intact mesenteric artery strips to capsaicin, causing desensitization and/or depletion of sensory neurotransmitter, methanandamide caused a mean change in membrane potential of the smooth muscle of −0.1 ± 0.3 mV [33]. The present membrane potential measurements in isolated myocytes fully confirm such an indirect action.
The application of exogenous CGRP substantially increased mesenteric smooth muscle cell I K. Moreover, the membrane potential of isolated myocytes substantially hyperpolarized after exposure to CGRP. These findings unequivocally show that the neuropeptide is acting directly on the smooth muscle cells and that at least part of the hyperpolarization we previously found in intact small mesenteric arteries [3] is endothelium independent. This observation is also in line with literature data showing that CGRP-induced vasorelaxation of rat mesenteric arteries is endothelium independent [7, 31].
A number of studies have shown that CGRP increases cAMP content in vascular smooth muscle [14, 39]. cAMP-dependent protein kinase may activate KATP channels, as in pig coronary arteries [35] and rabbit mesenteric artery [23], or BKCa channels, as in pig coronary arteries [16] and rat aorta [27] and tail arteries [28, 29]. In some vessels, the CGRP-induced vasodilation was mediated by activation of both BKCa and KATP channels [11, 12, 14]. In preconstricted rat coronary arteries, charybdotoxin inhibited the CGRP-induced vasorelaxation, while in the resting arteries only the pretreatment with a combination of glibenclamide and charybdotoxin attenuated the CGRP-induced decrease in [Ca2+]i and tension [30]. In the present experiments, we found low concentrations of TEA and the presence of the more selective inhibitor of BKCa channels, iberiotoxin, to fully block the influence of CGRP. It was also inhibited by the CGRP receptor antagonist CGRP8-37, as well as by the adenylyl cyclase inhibitor SQ22536 and the PKA inhibitor Rp-cAMPS. Moreover, the KATP channel inhibitor glibenclamide had no effect. This shows that in the present conditions, CGRP induces BKCa channel activation of rat mesenteric artery smooth muscle cells in a receptor-, cAMP-, and PKA-dependent way.
Conclusion
In summary, we have shown that exogenous CGRP potently activates BKCa currents in small mesenteric artery smooth muscle cells and substantially hyperpolarizes the membrane potential of these cells. The influence on BKCa current is receptor-dependent and mediated by adenylyl cyclase and PKA. Moreover, methanandamide fails to hyperpolarize the membrane potential of these myocytes and decreases K+ currents in a way similar as has been described for smooth muscle cells of the aorta. The latter finding is fully consistent with studies reporting that the cannabinoid hyperpolarizes and relaxes intact mesenteric arteries indirectly, by releasing CGRP from perivascular sensory nerves.
References
Boussery K, Delaey C, Van de Voorde J (2005) The vasorelaxing effect of CGRP and natriuretic peptides in isolated bovine retinal arteries. Invest Ophth Vis Sci 46(4):1420–1427
Breyne J, Van de Voorde J, Vanheel B (2006) Characterization of the vasorelaxation to methanandamide in rat gastric arteries. Can J Physiol Pharmacol 84(11):1121–1132
Breyne J, Vanheel B (2006) Methanandamide hyperpolarizes gastric arteries by stimulation of TRPV1 receptors on perivascular CGRP containing nerves. J Cardiovasc Pharmacol 47(2):303–309
Ellis JL, Conanan ND (1995) Modulation of relaxant responses evoked by a nitric-oxide donor and by nonadrenergic, noncholinergic stimulation by isozyme-selective phosphodiesterase inhibitors in guinea-pig trachea. J Pharmacol Exp Ther 272(3):997–1004
Fan P (1995) Cannabinoid agonists inhibit the activation of 5-HT3 receptors in rat nodose ganglion neurons. J Neurophysiol 73(2):907–910
Fleming I, Schermer B, Popp R, Busse R (1999) Inhibition of the production of endothelium-derived hyperpolarizing factor by cannabinoid receptor agonists. Br J Pharmacol 126(4):949–960
Gao YJ, Nishimura Y, Suzuki A, Nakai Y (1996) Calcitonin gene-related peptide-induced relaxation in isolated small superior mesenteric arteries from adult stroke-prone spontaneously hypertensive rats. Clin Exp Pharmacol Physiol 23:625–631
Gebremedhin D, Lange AR, Campbell WB, Hillard CJ, Harder DR (1999) Cannabinoid CB1 receptor of cat cerebral arterial muscle functions to inhibit L-type Ca2+ channel current. Am J Physiol Heart Circ Physiol 276(6):H2085–H2093
Gray DW, Marshall I (1992) Nitric-oxide synthesis inhibitors attenuate calcitonin gene-related peptide endothelium-dependent vasorelaxation in rat aorta. Eur J Pharmacol 212(1):37–42
Hampson AJ, Bornheim LM, Scanziani M, Yost CS, Gray AT, Hansen BM, Leonoudakis DJ, Bickler PE (1998) Dual effects of anandamide on NMDA receptor-mediated responses and neurotransmission. J Neurochem 70(2):671–676
Herzog M, Scherer EQ, Albrecht B, Rorabaugh B, Scofield MA, Wangemann P (2002) CGRP receptors in the gerbil spiral modiolar artery mediate a sustained vasodilation via a transient cAMP-mediated Ca2+-decrease. J Membr Biol 189(3):225–236
Hong KW, Yoo SE, Yu SS, Lee JY, Rhim BY (1996) Pharmacological coupling and functional role for CGRP receptors in the vasodilation of rat pial arterioles. Am J Physiol Heart Circ Physiol 39(1):H317–H323
Ishikawa M, Ouchi Y, Orimo H (1993) Effect of calcitonin-gene-related peptide on cytosolic-free Ca2+ level in vascular smooth-muscle. Eur J Pharmacol 246(2):121–128
Kageyama M, Yanagisawa T, Taira N (1993) Calcitonin gene-related peptide relaxes porcine coronary-arteries via cyclic AMP-dependent mechanisms, but not activation of ATP-sensitive potassium channels. J Pharmacol Exp Ther 265(2):490–497
Langton PD, Nelson MT, Huang Y, Standen NB (1991) Block of calcium-activated potassium channels in mammalian arterial myocytes by tetraethylammonium ions. Am J Physiol Heart Circ Physiol 260:H927–H934
Minami K, Fukuzawa K, Nakaya Y, Zeng XR, Inoue I (1993) Mechanism of activation of the Ca2+-activated K+ channel by cyclic AMP in cultured porcine coronary artery smooth muscle cells. Life Sci 53(14):1129–1135
Nelson MT, Quayle JM (1995) Physiological roles and properties of potassium channels on arterial smooth muscle. Am J Physiol - Cell Physiol 268:C799–C822
Nelson MT, Huang Y, Brayden JE, Hescheler J, Standen NB (1990) Arterial dilations in response to calcitonin gene-related peptide involve action of K+ channels. Nature 344:770–776
O'Sullivan SE, Kendall DA, Randall MD (2004) Heterogeneity in the mechanisms of vasorelaxation to anandamide in resistance and conduit rat mesenteric arteries. Br J Pharmacol 142(3):435–442
O'Sullivan SE, Kendall DA, Randall MD (2005) Novel time-dependent vascular actions of delta(9)-tetrahydrocannabinol (THC) mediated by peroxisome proliferator-activated receptor gamma (PPARγ). Biochem Biophys Res Commun 337(3):824–831
Pratt PF, Hillard CJ, Edgemond WS, Campbell WB (1998) N-arachidonylethanolamide relaxation of bovine coronary artery is not mediated by CB1 cannabinoid receptor. Am J Physiol Heart Circ Physiol 43(1):H375–H381
Prieto D, Benedito S, Nyborg NCB (1991) Heterogeneous involvement of endothelium in calcitonin gene-related peptide-induced relaxation in coronary-arteries from rat. Br J Pharmacol 103(3):1764–1768
Quayle JM, BonevAD BJE, Nelson MT (1994) Calcitonin-gene-related peptide activated ATP-sensitive K+ currents in rabbit arterial smooth-muscle via protein-kinase-A. J Physiol Lond 475(1):9–13
Ralevic V, Kendall DA, Randall MD, Movahed P, Hogestatt ED (2000) Vanilloid receptors on capsaicin-sensitive sensory nerves mediate relaxation to methanandamide in the rat isolated mesenteric arterial bed and small mesenteric arteries. Br J Pharmacol 130(7):1483–1488
Randall MD, Kendall DA (1997) Involvement of a cannabinoid in endothelium-derived hyperpolarizing factor-mediated coronary vasorelaxation. Eur J Pharmacol 335:205–209
Sade H, Muraki K, Ohya S et al (2006) Activation of large-conductance, Ca2+-activated K+ channels by cannabinoids. Am J Physiol Cell Physiol 290(1):C77–C86
Sadoshima J, Akaike N, Tomoike H, Kanaide H, Nakamura M (1988) Ca-activated K-channel in cultured smooth muscle cells of rat aortic media. Am J Physiol 255(3):H410–417
Schubert R, Nelson MT (2001) Protein kinases: tuners of the BKCa channel in smooth muscle. Tr Pharmacol Sci 22(10):505–512
Schubert R, Serebryakov VN, Engel H, Hopp HH (1996) Iloprost activates K-Ca channels of vascular smooth muscle cells: Role of cAMP-dependent protein kinase. Am J Physiol Cell Physiol 40(4):C1203–C1211
Sheykhzade M, Nyborg NCB (2001) Mechanism of CGRP-induced relaxation in rat intramural coronary arteries. Br J Pharmacol 132(6):1235–1246
Takenaga M, Kawasaki H, Wada A, Eto T (1995) Calcitonin-gene-related peptide mediates acetylcholine-induced endothelium-independent vasodilation in mesenteric resistance blood-vessels of the rat. Circ Res 76(6):935–941
Van den Bossche I, Vanheel B (2000) Influence of cannabinoids on the delayed rectifier in freshly dissociated smooth muscle cells of the rat aorta. Br J Pharmacol 131(1):85–93
Vanheel B, Van de Voorde J (2001) Regional differences in anandamide- and methanandamide-induced membrane potential changes in rat mesenteric arteries. J Pharmacol Exp Ther 296(2):322–328
Watanabe H, Vriens J, Prenen J, Droogmans G, Voets T, Nilius B (2003) Anandamide and arachidonic acid use epoxyeicosatrienoic acids to activate TRPV4 channels. Nature 424:434–438
Wellman GC, Quayle JM, Standen NB (1998) ATP-sensitive K+ channel activation by calcitonin gene-related peptide and protein kinase A in pig coronary arterial smooth muscle. J Physiol Lond 507(1):117–129
White R, Hiley CR (1997) The action of the cannabinoid receptor antagonist, SR 141716A, in the rat isolated mesenteric artery. Br J Pharmacol 125(4):689–696
White R, Ho WSV, Bottrill FE, Ford WR, Hiley CR (2001) Mechanisms of anandamide-induced vasorelaxation in rat isolated coronary arteries. Br J Pharmacol 134(4):921–929
Wisskirchen FM, Burt RP, Marshall I (1998) Pharmacological characterization of CGRP receptors mediating relaxation of the rat pulmonary artery and inhibition of twitch responses of the rat vas deferens. Br J Pharmacol 123(8):1673–1683
Yoshimoto R, Mitsui-Saito M, Ozaki H, Karaki H (1998) Effects of adrenomedullin and calcitonin gene-related peptide on contractions of the rat aorta and porcine coronary artery. Br J Pharmacol 123(8):1645–1654
Zygmunt PM, Petersson J, Andersson DA, Chuang HH, Sorgard M, Di Marzo V, Julius D, Hogestatt ED (1999) Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 400:452–457
Acknowledgments
This work was supported by a BOF grant from Ghent University and by the Interuniversity Attraction Poles Program to L.L. (Belgian Science Policy, project P6/31). The authors are grateful to Julien Dupont, Tom Vanthuyne, and Cyriel Mabilde for unfailing technical assistance.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bol, M., Leybaert, L. & Vanheel, B. Influence of methanandamide and CGRP on potassium currents in smooth muscle cells of small mesenteric arteries. Pflugers Arch - Eur J Physiol 463, 669–677 (2012). https://doi.org/10.1007/s00424-012-1083-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-012-1083-1