Abstract
Background
The aim of this study was to evaluate the cardiovascular effects of N-phenyl-itaconimide (Imide-1), N-4-methyl-phenyl-itaconimide (Imide-2), N-4-methoxy-phenyl-itaconimide (Imide-3) and N-4-chloro-phenyl-itaconimide (Imide-4), and investigate the mechanisms of action involved in the observed responses.
Methods
The relaxant effect was investigated in rat superior mesenteric arteries by using isometric tension measurements. Additionally, in isolated atria were evaluated the heart rate and force of cardiac contraction and in vivo experiments was evaluated blood pressure and heart rate.
Results
Cumulative administration of itaconimides (3 × 10−8 to 3 × 10−4 M) in pre-contracted mesenteric artery rings with phenylephrine, 1 μM, induced endothelium-independent vasorelaxation. The itaconimides showed similar maximum efficacies. Additionally, Imide-3 induced vasorelaxation in rings exposed to a depolarizing-tyrode solution containing 60 mM KCl or 20 mM KCl similar to the control, suggesting the non-participation of K+ channels. Imide-3 attenuated Ca2+ influx in a concentration-dependent manner. As well, imide-3 reduced CaCl2-induced contraction in nominally calcium-free medium, in the presence of cyclopiazonic acid (20 μM), phenylephrine (1 μM) and nifedipine (1 μM), indicating a reduction of Ca2+ influx by receptor-operated channels (ROC) and store-operated channels (SOC). The presence of SKF 96365 (10−5 M), SOC blocker, did not significantly alter the vasorelaxant effect induced by imide-3. Moreover, imide-3 induced a negative inotropic effect. In vivo studies, in non-anesthetized normotensive rats, imide-3 lowered blood pressure and induced bradycardia.
Conclusions
These results suggest that itaconimides have concentration-dependent vascular effects and the vasorelaxation seems to be endothelium-independent. The vasodilatory effect induced by imide-3 may be due to a possible influence on the CaV and ROC. In addition, imide-3 is able to reduce force of cardiac contraction, blood pressure and promote bradycardia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertension is an important public health problem and has been associated with the development of cardiovascular and renal diseases. Moreover, hypertension is a major preventable risk factor for early death and disability. In this way, controlling blood pressure is significantly related with reduction of cardiovascular morbidity and mortality [1]. Hypertension causes a substantial impact to cardiovascular disease worldwide. In 2011 to 2014, 103.3 million adults in the United States met the definition for hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline, which represents approximately 45.6% of the adult population [2]. Hypertension is a treatable condition, as management includes healthy lifestyle modifications and anti-hypertensive therapy [3]. Although a wide range of treatment options are available for blood pressure control, many hypertensive individuals remain with uncontrolled hypertension [4].
Additionally, resistant hypertension is defined as persistent increase in blood pressure that remains above goal despite use of three or more antihypertensive agents of different classes, one of them being a diuretic, at the best tolerated doses [5, 6]. Several studies demonstrate that the prevalence of resistant hypertension can be predicted at ranges between 10 and 15% of treated hypertensive patients [7]. Therefore, novel drugs are needed that display multiple therapeutic effects due to the fact that the majority of current antihypertensive drugs require combination therapy based on their limited efficacy and side effects. Thus, the study of natural products, which are an important source of compounds with antihypertensive activity, can be used as a prototype to design more potent and safer drugs for the treatment of hypertension [8].
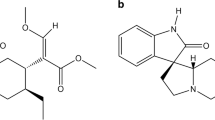
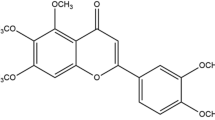
Phyllanthimide is an alkaloid isolated from Phyllanthus sellowianus (Euphorbiaceae) [9], which presents antispasmodic activity [10, 11]. This alkaloid was used as a prototype for the development of analog compounds belonging to the chemical class of cyclic imides [12, 13], which contain the group –CO–N(R)–CO–, are electrically neutral and hydrophobic molecules [14]. In addition, studies have demonstrated that cyclic imides are biologically active molecules in the cardiovascular system, promoting vasorelaxant [15, 16] and hypotensive effects [15].
In this way, cyclic imides are compounds with potential biological activities on the cardiovascular system, however to date, these molecules have been poorly studied in this system. It’s important to evaluate the potential of these substances on cardiovascular system, thus a variety of cyclic imides were synthesized, in order to investigate their effects on the cardiovascular system. Specifically, N-phenyl-itaconimide (Imide-1), N-4-methyl-phenyl-itaconimide (Imide-2), N-4-methoxy-phenyl-itaconimide (Imide-3) and N-4-chloro-phenyl-itaconimide (Imide-4), were synthesized to test their properties on the cardiovascular system, which has yet to be investigated (Fig. 1). Therefore, in this study, we aimed to investigate, for the first time, the cardiovascular activities of these itaconimides in the vascular and cardiac tissues, with propose of describing the mechanisms of action involved in the observed responses.
Material and methods
Animals
Male Wistar rats weighing 200–300 g were used in all experiments. The animals were supplied by the animal facility of the Neuroscience Laboratory, at the Institute of Health Sciences at the Federal University of Bahia and kept under controlled temperature (21 ± 1 °C) a light–dark cycle of 12 h (6 a.m. to 6 p.m.) and free access to food and water. The study was conducted in accordance with the guide of care and use of laboratory rats, adopted by the National Council for Animal Experiments Control (CONCEA—BRAZIL) and National Institutes of Health guide for the care and use of Laboratory animals (NIH Publications No. 8023, revised 1978). It was approved by the Ethics Committee on Animal Use from the Institute of Health Sciences, Federal University of Bahia (CEUA/UFBA nº120/2017).
Drugs
The drugs used in this study were: (−)-phenylephrine hydrochloride, acetylcholine chloride, cremophor, nifedipine, sodium nitroprusside, SKF 96365, cyclopiazonic acid, dimethyl sulfoxide (DMSO), ketamine, xylazine, heparine, all acquired from Sigma-Aldrich (Sigma Chemical Co., Saint Louis, MO, USA). The cyclic imides were obtained from the itaconic anhydride with different aromatic amines [17]. For the preparation of the itaconimides solutions, drugs were solubilized in cremophor and diluted to the desired concentrations with distilled water (in vitro assay) or NaCl 0.9% (in vivo assay) just before use. The final concentration of cremophor in the organ bath never exceeded 0.003% and had no effect when tested in control preparations. Nifedipine, SKF 96365 and cyclopiazonic acid was dissolved in DMSO 100%. The other compounds were freely dissolved in distilled water. Tyrode’s physiological solution was used throughout all arterial experiments with the following compositions (mM): NaCl, 158.3; KCl, 4.0; CaCl2, 2.0; MgCl2, 1.05; NaH2PO4, 0.42; NaHCO3, 10.0, and glucose, 5.6. All reagents were purchased from Sigma (Sigma-Aldrich, St. Louis, USA).
Vascular studies using superior mesenteric artery
Wistar rats were euthanized in a CO2 chamber. The superior mesenteric arteries were quickly removed as described by Silva and colleagues [18], and cleaned from connective tissue and fat, and segmentally cut into rings (2 mm), which were suspended in organ baths containing Tyrode’s solution, bubbled with 95% O2/5% CO2, and maintained at 37 º C and pH 7.4. Tissues were stabilized with an optimal resting tension of 7.5 mN for 60 min. Isometric tension of the superior mesenteric arterial ring was recorded by a force transducer (Insight, Ribeirão Preto, SP, Brazil) coupled to an amplifier-recorder (Insight, Ribeirão Preto, SP, Brazil) and to a computer equipped with a data acquisition software. An intact endothelium was assessed by the ability of Ach (1 μM) to induce 90% or more of relaxation of rings pre-contracted with Phe (1 μM). In the endothelium denuded rings, the relaxation to Ach was less than 10%. When necessary, the endothelium was mechanically removed by gentle rubbing the vessel with a thin wire.
Effect of itaconimides on the vasculature
After the stabilization period, two successive contractions of similar magnitude were produced by Phe, 1 μM, (alpha1-adrenergic agonist) in endothelium-intact and -denuded rings. In the tonic phase of the second contraction, different concentrations of itaconimides (Imide-1, 2, 3 and 4; 3 × 10−8 to 3 × 10−4 M) were cumulatively added to the organ bath and the effects were compared. Additionally, these itaconimides were also added when an endothelium-intact vessel was at basal tone in order to examine the effect of itaconimides on spontaneous muscle tone.
Evaluation of the K+-channels activity in the vasorelaxant response induced by Imide-3
Different concentrations of Imide-3 (3 × 10−8 to 3 × 10−4 M) were added cumulatively to the organ bath to evaluate if Imide-3 can attenuate the relaxation of vessels pre-contracted with 60 mM KCl or phenylephrine in Tyrode’s solution with 20 mM KCl in endothelium–denuded rings.
Investigation of the effects induced by Imide-3 in Ca2+ influx
To investigate the effects of imide-3 on Ca2+ influx in endothelium denuded rings, cumulative concentrations of CaCl2 (10−6–10−2 M) were added in Tyrode’s solution (60 mM KCl) nominally without Ca2+ (15 min), depolarization medium, in the absence (control) or presence of different itaconimide concentrations (10−6, 10−5, 3 × 10−5 and 10−4 M).
In another set of experiments, the effects induced by imide-3 on Ca2+ influx through other channels instead of voltage-sensitive Ca2+ channels (Cav), such as, receptor-operated channels (ROC) and store-operated channels (SOC), was also investigated. First, rings were maintained in a Tyrode’s solution nominally without Ca2+ and incubated with cyclopiazonic acid (20 μM; 20 min), inhibitor of the sarco/endoplasmic reticulum Ca2+-ATPase (SERCA), Phe (1 μM; 5 min) and nifedipine (1 μM; a Cav blocker; 20 min), which was then followed by a single application of CaCl2 (10−2 M) to induce contraction. In the same vessel, this experimental protocol was repeated by pre-incubation with cyclopiazonic acid, Phe and nifedipine following incubation of imide-3 at different concentrations (10−5, 3 × 10−5 and 10−4 M) for 10 min, which was followed by a single application of CaCl2. The role of imide-3 on Ca2+ influx, most likely through SOC and ROC was assessed by comparing CaCl2 mediated contraction in the absence or presence of different concentrations of imide-3 with nifedipine/Phe/cyclopiazonic acid. Another experiment was performed to investigate the role of SOC, where endothelium-denuded rings were pre-incubated with SKF 96365 (10−5 M, a SOC blocker), for a period of 30 min, before adding Phe (1 μM), and then concentration–response to imide-3 (3 × 10−8 to 3 × 10−4 M) was initiated.
Atrial tissue preparation
Rats were euthanized in a CO2 chamber, hearts were quickly removed and the isolated left and right atria were maintained in an organ bath with krebs-bicarbonate (117.0 mM NaCl, 5.36 mM KCl, 2.5 mM CaCl2, 1.03 mM KH2PO4, 0.57 mM MgSO4, 25.0 mM NaHCO3, and 11.1 mM glucose) at a temperature of 37 °C and gassed with 95% O2 and 5% CO2. Isometric tension recordings of suspended atria were performed. The initial tension of each atrium was adjusted to 5.0 mN and the tissues were maintained during a stabilization period for 45 min before beginning the experiments. The isometric tension was recorded by a force transducer (FORT-10; WPI, Sarasota, FL, USA) connected to an amplifier-recorder (Miobath-4, WPI, Sarasota, USA). In each left atrium, used for cardiac inotropic analyses, was measured the excitation threshold, the minimum voltage of electrical stimulation required to elicit sustained synchronous contractions of the whole atrium. During the experiment, the left atrium was continuously electrically stimulated by square voltage pulses with a frequency of 3 Hz for 3 ms to 1.5 times the excitation threshold voltage of each heart tissue, in order to ensure that all cardiomyocytes were excited, as previously described [19], with an AVS stimulator (AVS, Brazil). Right atrium were measured for rhythmic and spontaneous organic contractions and imide-3 was added in 3 different concentrations (3 × 10−7, 3 × 10−6 and 3 × 10−5 M).
Influence of imide-3 on blood pressure (BP) and heart rate (HR)
On the day prior to animal experimentation where rats were anesthetized with ketamine/xylazine (75 mg/kg and 20 mg/kg ip, respectively), a polyethylene catheter (PE-10 connected to PE-50) filled with heparinized saline solution (1000 U/mL) was inserted into the abdominal aorta through the left femoral artery to measure the pulsatile arterial pressure (PAP). A second catheter was inserted into inferior vena cava through the left femoral vein for intravenous drug administration. Twenty-four hours following these surgical procedures, experiments were performed in non-anesthetized rats, under conscious and free-moving conditions. After 30 min of cardiovascular parameters stabilization, sodium nitroprusside (10 µg/kg, iv) was administered to verify the effectiveness of the venous catheter implantation and subsequently different doses of Imide-3 (0.1, 1 and 10 mg/kg randomly, iv) were administered. The PAP were continuously monitored through the arterial catheter connected to a blood pressure transducer (AD Instruments) whose signal was amplified and digitally recorded by an analog-to-digital interface (Power/Lab 8 35, application for data acquisition, LabChart, New South Wales, Austrália) and recorded (1 kHz) on a microcomputer for later analysis. The mean arterial pressure (MAP), systolic arterial pressure (SAP), diastolic arterial pressure (DAP) and heart rate (HR) were obtained from the PAP.
Data analysis
The values were expressed as means ± standard error of the mean (S.E.M.), and n represents a number of rings obtained from different rats. All calculations were performed using GraphPad Prism© software, version 5.0 (GraphPad Software Inc., La Jolla, CA, USA). The maximal effect (Emax) corresponds to maximum relaxation of the itaconimides, and pD2 to negative logarithm of the concentration of a substance that induces 50% of maximal effect (− log EC50). The pD2 was calculated using non-linear regression. For statistical analyses, Student's t test and one-way ANOVA was used to compare 2 and 3 or more groups, respectively, followed by Bonferroni's multiple comparisons post-test. Values of p < 0.05 were considered statistically significant.
Results
Itaconimides induce endothelium-independent-relaxation in mesenteric artery
As shown in Fig. 2, imides-1, 2, 3 and 4 (3 × 10−8 to 3 × 10−4 M) induced concentration-dependent relaxation in superior mesenteric artery segments with intact endothelium, pre-contracted with phe (1 μM). Imide-1 (Emax = 92.9 ± 14.1%; pD2 = 5.08 ± 0.15, n = 7), imide-2 (Emax = 93.7 ± 7.9%; pD2 = 4.63 ± 0.07, n = 7), imide-3 (Emax = 108.7 ± 3.8%; pD2 = 4.57 ± 0.04, n = 7) and imide-4 (Emax = 103.7 ± 4.2%; pD2 = 4.67 ± 0.04, n = 6). The efficacy and pharmacological potency for endothelium-denuded rings imide-1 (Emax = 103.8 ± 10.4%; pD2 = 4.72 ± 0.11, n = 7), imide-2 (Emax = 102.4 ± 4.4%; pD2 = 4.68 ± 0.07, n = 6), imide-3 (Emax = 107.5 ± 6.3%; pD2 = 4.64 ± 0.09, n = 6) and imide-4 (Emax = 100.2 ± 2.6%; pD2 = 4.69 ± 0.05, n = 7) were statistically similar to endothelium intact. Thus, there were no statistical differences among the maximum efficacy of itaconimides. In addition, imide-1 showed higher pharmacological potency than imide-2 (**p < 0.05), Imide-3 (**p < 0.01) and imide-4 (*p < 0.05). Furthermore, there was no significant change in basal tone following administration of itaconimides (data not shown). Imide-1 was the most potent drug tested, however, the substance was quite unstable. Since the other itaconimides presented similar potency, we selected the imide-3 to characterize the possible mechanisms involved in pharmacological actions.
Effects of itaconimides in superior mesenteric artery. Representative original recordings of the effects of itaconimides imide-1 (a), imide-2 (b), imide-3 (c) and imide-4 (d) on the isolated mesenteric artery rings, pre-contracted with phenylephrine. The arrows represent the time-course of the itaconimides administration (3 × 10−8 to 3 × 10−4 M). Concentration–response curves (e–h) showing the relaxant effect of itaconimides on the isolated mesenteric artery rings with endothelium-intact (E+ , ■) or endothelium-denuded (E−, ●) and bar graph showing the Emax and pD2 values in different condition. Bar graph comparing the Emax (i) and pD2 (j) of itaconimides on the isolated mesenteric artery rings with endothelium-intact. Results are expressed as mean ± S.E.M. e Imide-1, E+ (n = 7) and E− (n = 7); f Imide-2, E+ (n = 7) and E− (n = 6); g Imide-3, E+ (n = 7) and E− (n = 6) and h Imide-4, E+ (n = 6) and E− (n = 7). Statistical analysis was performed using unpaired Student’s t tests
Imide-3 inhibited contraction induced by depolarization with High K+ concentration
In endothelium-denuded rings, imide-3 (3 × 10−8 to 3 × 10−4 M) inhibited the sustained tonic contraction induced by 60 mM KCl in a concentration-dependent manner. The response of imide-3 was not significantly changed when compared to rings contracted with phe (1 μM) (Fig. 3).
Effect of Imide-3 on the contractions induced by phenylephrine, KCl 60 mM or KCl 20 mM with phenylephrine. Relaxation responses induced by Imide-3 (3 × 10−8 to 3 × 10−4 M) in denuded rat mesenteric arteries rings pre-contracted with phenylephrine (1 μM) (●, n = 6), KCl 20 mM + phenylephrine (1 μM) (■, n = 6) and KCl 60 mM (▲, n = 6). Results are expressed as mean ± S.E.M. Statistical analysis was performed using one-way ANOVA followed by the Bonferroni post-test
Effect of Imide-3 on arteries treated with 20 mM KCl
To evaluate the involvement of K+ channels in the vasorelaxant response induced by Imide-3, mesenteric rings lacking endothelium, pre-contracted with phenylephrine were pre-treated with 20 mM KCl. Imide-3 did not alter the concentration–response curve when compared to the control. This finding indicates that K+ channel activation does not play a role in the relaxant effect of Imide-3 in mesenteric arteries (Fig. 3).
Effect of Imide-3 on the CaCl2-induced concentration–response curves
As shown in Fig. 4, the concentration–response curve to CaCl2 in a depolarizing medium, while in the presence of Imide-3 (10−6 or 10−5 or 3 × 10−5 or 10−4 M) was shifted to the right when compared with the control. The maximal contraction of CaCl2 was significantly (***p < 0.001) attenuated by 10−5 M, 3 × 10−5 M and 10−4 M concentrations of imide-3 (69.5 ± 10.6%, 36.3 ± 9.0%, − 3.2 ± 3.9%, respectively). These data indicate that the mechanism of action of imide-3 involves the reduction of Ca2+ influx.
Effect of Imide-3 on Ca2+ influx. Concentration–response curve of CaCl2 on rat mesenteric artery segments without endothelium, in the absence (●, n = 28) or in the presence of Imide-3 (■, 10−6 M, n = 8), (▲, 10−5 M, n = 7), (▼, 3 × 10−5 M, n = 7) and (♦, 10−4 M, n = 6). *p < 0.05 versus control. **p < 0.01 versus control. ***p < 0.001 versus control. Results are expressed as mean ± S.E.M. Statistical analysis was performed using one-way ANOVA followed by the Bonferroni post-test
Imide-3 reduced Ca2+ influx through ROC and SOC
The influence of Imide-3 on Ca2+ influx through ROC and SOC was evaluated in experiments performed with Tyrode’s solution nominally without Ca2+ in the presence of Cyclopiazonic acid/Phe/Nifedipine. Figure 5 demonstrates that the contraction evoked by CaCl2 in Tyrode’s solution nominally without Ca2+, following intracellular Ca2+-store depletion and blocking Cav, no modification of the Emax values was observed following pretreatment using different concentrations (10−5 or 3 × 10−5 M) of Imide-3 (25.3 ± 2.2%, 22.5 ± 4.6%, respectively) compared to control (29.0 ± 2.6%). However, the concentration of 10−4 M significantly reduced the contraction (7.0 ± 1.9%).
Effect of Imide-3 on the contraction induced by CaCl2 in the presence of phenylephrine, nifedipine and cyclopiazonic acid. Influence of Imide-3 (10−5, 3 × 10−5 and 10−4 M) on CaCl2 (10−2 M) mediated contraction in Tyrode’s solution nominally without Ca2+, in the presence of phenylephrine (Phe) (1 μM), nifedipine (1 μM) and Cyclopiazonic acid (CPA) (20 μM). Imide-3 (10−5 M, n = 7), (3 × 10−5 M, n = 6) and (10−4 M, n = 7). ***p < 0.001 Phe + CPA + nifedipine versus Imide-3 (10−4 M). Results are expressed as mean ± S.E.M. Statistical analysis was performed using one-way ANOVA followed by the Bonferroni post-test
Effect of SOC inhibition on the relaxation induced by imide-3
Figure 6 shows that SOC inhibition by SKF 96365 in endothelium-denuded rings did not attenuate relaxation induced by imide-3. This result suggests that SOC do not participate in the mechanism of action of imide-3.
Vasorelaxant effect from Imide-3 in the presence of SOC-inhibition. Relaxation responses induced by Imide-3 (3 × 10−8 to 3 × 10−4 M) in denuded rat mesenteric arteries rings, pre-contracted with phenylephrine, in the presence or absence of SKF 96365 (10−5 M). Results are expressed as mean ± S.E.M. (n = 6). Statistical analysis was performed using unpaired Student’s t tests
Evaluation of the direct effect of Imide-3 on the isolated atria
The influence of imide-3 on chronotropism was analyzed based on isolated right atrium spontaneous beating frequency, quantified and defined as atrial rate. The addition of three cumulative concentrations of Imide-3 (3 × 10−7 M, 3 × 10−6 M and 3 × 10−5 M) did not result in a significant negative chronotropic effect (99.3% ± 1.63, 98.0% ± 1.33, 97.4% ± 1.22, respectively) compared to control (100 ± 0) (Fig. 7a). Moreover, with the purpose of analyzing the effect of Imide-3 on the strength of cardiac contraction (inotropic effect), these concentrations of Imide-3 were added to the isolated left atrium preparation. The concentrations of 3 × 10−7 M and 3 × 10−6 M were did not significantly reduce force of cardiac contraction (86.1% ± 14.4, 61.5% ± 15.6, respectively). However, the last tested concentration, 3 × 10−5 M, demonstrated a significant negative inotropic effect (47.0% ± 15.1) compared to control (100 ± 0) (Fig. 7b, c).
Effect of Imide-3 on isolated right and left rat atria. Bar graph showing the chronotropic effect of Imide-3 (3 × 10−7, 3 × 10−6 and 3 × 10−5 M) on isolated right rat atria (a). Representative tracings showing the effect of Imide-3 on left atrial contractile force (b). Bar graph showing the negative inotropic effect of Imide-3 on isolated left rat atria (c). Results are expressed as mean ± S.E.M. (n = 5). *p < 0.05 versus control. Statistical analysis was performed using one-way ANOVA followed by the Bonferroni post-test
Imide-3 induces hypotensive effects in normotensive rats
Hemodynamics changes induced by Imide-3 (0.1; 1 and 10 mg/kg, iv, administered randomly) were investigated in normotensive non-anesthetized rats. Imide-3 administration did not alter blood pressure and heart rate at the following doses: 0.1 and 1 mg/kg (− 2.06 ± 0.44; − 6.48 ± 1.89 mmHg and 0.24 ± 0.86; 4.18 ± 2.17 bpm; respectively, n = 5). However, the 10 mg/kg dose induced hypotension associated with a decrease in heart rate (− 57.3 ± 6.83 mmHg and − 78.1 ± 1.76 bpm, n = 5) (Fig. 8).
Effects of intravenous administration of Imide-3 on the mean arterial pressure and heart rate in normotensive rats. Representative tracing showed the hypotensive response and bradycardia, induced by addition of Imide-3 (10 mg/kg) in conscious normotensive rats (a). Bar graphs showing changes in mean arterial pressure (%) (b). Changes on heart rate (%) (c). Results are expressed as mean ± S.E.M. (n = 5). ***p < 0.001 versus vehicle (control). Statistical analysis was performed using one-way ANOVA followed by the Bonferroni post-test
Discussion
This study demonstrates that the itaconimides, imide-1, imide-2, imide-3 and imide-4, induce a pronounced endothelium-independent vasorelaxation in isolated rat superior mesenteric artery rings, mainly thought the inhibition of extracellular Ca2+ influx. We also demonstrated that imide-3 induced hypotensive and bradycardic effects in non-anaesthetized rats and negative inotropic action in isolated atria. Additionally, the reduction in peripheral vascular resistance and negative inotropic action could be, at least in part, responsible for the hypotensive and bradycardic effects promoted by imide-3. To the best of our knowledge, this is the first work that shows these cardiovascular effects of itaconimides.
The endothelium plays a pivotal role in regulating vascular tone by synthesizing and releasing an array of endothelium-derived relaxing factors, including nitric oxide (NO), prostacyclin (PGI2), and endothelium-dependent hyperpolarization factors (EDHF), as well as endothelium-derived contracting factors [20, 21]. To evaluate the participation of the endothelium modulating itaconimides actions, we performed experiments in the absence and presence of a functional endothelium. Our experiments demonstrated that itaconimides relaxed contractions induced by phenylephrine, in a concentration-dependent manner, with similar pharmacological potency in endothelium-denuded and in endothelium-intact artery rings. This indicates that the vasorelaxant effects of itaconimides are independent of vasoactive mediator release from endothelium and that these itaconimides may act directly on the smooth muscle cell. However, another cyclic imide, 4-Nitro-N-phenylmaleimide, has been demonstrated to produce an endothelium-dependent and -independent vasorelaxation in superior mesenteric artery rings [16].
Moreover, the four itaconimides showed similar maximal effect. However, Imide-1 demonstrated a higher pharmacological potency than the other itaconimides tested, thus the most active itaconimide was unsubstituted compound. These results suggest that there may be some unfavorable steric effects due to the substitution of the Imide-2 (–CH3), Imide-3 (–OCH3) and Imide-4 (–Cl) in the fourth position of the benzene ring because the introduction of these substituents (chloro, methyl and methoxy-substituent) decreased the pharmacological potency. As well, all itaconimides induced vasorelaxant activity, and therefore the complete structure is important for the interaction with the biological target, emphasizing the importance of the imidic ring for the biological effect. Under our experimental conditions, all vasodilator responses to itaconimides 1, 2 and 3 were reversible until the concentration of 3 × 10−5 M, therefore these vasorelaxant actions are not related to putative toxic effects (data not shown).
Furthermore, itaconimides were unable to alter the resting tone of arterial smooth muscle. Thus, these results may indicate that the itaconimides do not present vasoconstriction or vasodilation activity on basal tone, however itaconimides may possibly induce vasorelaxation only in pre-contracted mesenteric artery rings. Moreover, the most potent itaconimide was imide-1, but the substance was quite unstable. Since the other itaconimides presented similar pharmacological potency, the imide-3 was chosen to characterize the possible mechanisms involved in pharmacological actions. In the present study, imide-3 inhibited KCl (60 mM)-induced contractions, suggesting that itaconimide might interfere with electromechanical coupling, and the concentration–response curve in this condition was similar to the response obtained in the presence of Phe. It is well known that KCl solution may induce contraction of the vascular smooth muscle mainly due to depolarization and the influx of extracellular Ca2+ though Cav [22, 23] and release of calcium from the intracellular stores [24, 25]. While phenylephrine selectively activates α1-adrenergic receptors, resulting in the production of inositol trisphosphate (IP3) and diacylglycerol (DAG). IP3 increases Ca2+ by activating sarco/endoplasmic reticulum Ca2+ channels and Ca2+ release. DAG can activate protein kinase C and provoke Ca2+ entry through transient receptor protein cation channels [26]. Our current data indicate that imide-3 acts in a possible common pathway the both contractile agents, receptor independent mechanism and promote a mechanism that could be related to inhibiting calcium influx activity.
Another important mechanism that promotes vasorelaxation by a direct action on vascular smooth muscle cells can involve potassium channels. The opening of K+ channels causes diffusion of this cation out of the cells, resulting in membrane hyperpolarization and consequently decreases in the open probability state of Cav, ultimately leading to vasorelaxation [27,28,29]. Furthermore, elevated extracellular potassium ion concentration reduces the electrochemical gradient for K+ efflux and attenuates vasorelaxation mediated by K+ channels activation [30]. In our study, the increase in extracellular K+ concentrations (from 4 to 20 mM) did not significantly attenuate the vasorelaxation induced by imide-3, which was also observed when rings were exposed to 60 mM KCl, suggesting that K+ channel activation does not appear to be involved. Moreover, we evaluated whether vasorelaxation induced by imide-3 is associated with the inhibition of Ca2+ influx. There are different Ca2+ entry channels, such as Cav, ROC and SOC in smooth muscle cells. Cav are the major way by which Ca2+ enters vascular smooth muscle cells and their function are regulated by membrane potential, so that depolarization opens these channels, leading to vasoconstriction [31]. Imide-3 markedly reduced the Ca2+-induced vasoconstriction in mesenteric rings lacking endothelium that were pre-incubated with a high K+ solution (KCl 60 mM) nominally without Ca2+, suggesting that Ca2+-influx through Cav channels was probably inhibited. This result corroborates previous observations describing cyclic imides, phyllanthimide and 4-Nitro-N-phenylmaleimide, that decrease the influx of Ca2+ in smooth muscle cells [10, 16, 32]. However, patch clamp technique is needed to confirm a blocking effect of imide-3 on Cav in smooth muscle cells.
Next, another experimental protocol was performed to assess whether the effect of imide-3 on inhibiting Ca2+-influx could involve an additional calcium influx inhibition pathways, such as SOC and ROC. To evaluate this, arterial rings were studied in a nominally Ca2+-free Tyrode solution in the presence of cyclopiazonic acid (20 μM), used to deplete intracellular Ca2+ stores and thus activate SOC [31, 33]. Ca2+ depletion in the sarco/endoplasmic reticulum is followed by a stimulated Ca2+ entry via SOC, replenishing intracellular calcium stores. Thus, SOC are inhibited when Ca2+ stores are filled [31, 34]. Furthermore, Phe evokes contraction by activation of ROC and CaV [35]. Furthermore, ROC are activated by ligand-mediated activation of G protein coupled receptors (GPCRs) and receptor tyrosine kinase (RTK), which after ligand binding activate phospholipase C, resulting to IP3 and DAG production [36]. ROC play an important role in arterial tone regulation in response to vasoactive agonists, such as angiotensin II and α-adrenoceptor agonists [37]. Moreover, depolarization may occur after activation of ROC, leading an additional Ca2+ influx through Cav [38]. In our experiment, to exclude the participation of CaV, nifedipine (10−3 M) was used, which blocks voltage-gated L-type Ca2+ channels [39, 40], but ROC are unaffected by this blocker [41]. Under these conditions, the highest tested concentration of imide-3 significantly attenuated the CaCl2-induced contraction. These results indicate that the vasorelaxant response of imide-3 may also involve, at least in part, the inhibition of Ca2+ influx through ROC and SOC. In addition, experiments were performed to assess the involvement of SOC in relaxation induced by imide-3, using the nonspecific channel blocker, SKF 96365. The results indicate that the itaconimide-mediated relaxation was similar in the presence and absence of SKF, indicating a lack of inhibition of Ca2+ entry through SKF-sensitive channels by imide-3. Therefore, the vasodilatory effect induced by imide-3 may be due to a possible influence on the CaV and ROC.
Since the itaconimide induced a marked vasodilation by Ca2+-influx inhibition, we hypothesized that imide-3 could induce negative inotropic effect. To investigate this, experiments were carried out to evaluate the direct effect of imide-3 on the isolated atria preparations. Imide-3 induced a negative inotropic effect without a significant change in cardiac rhythmicity, but the mechanisms by which imide-3 acts in heart remain still unclear.
In vivo experiments were performed to investigate whether Imide-3 alters cardiovascular parameters in non-anesthetized normotensive rats. In these animals, we observed that intravenous administration of imide-3 induced a hypotensive response associated with bradycardia. The hypotensive effect may be due to reduced peripheral vascular resistance, and the bradycardia can be a direct or indirect action on cardiac activity.
Taken together, these results suggest that the itaconimides evaluated in this study is able to induce vasorelaxation, independent of endothelium-derived relaxing factors. In addition, imide 3 induces vasodilatation, most likely due to the inhibition of calcium influx through Cav and ROC (Fig. 9) and it also induces negative inotropic effect. These effects probably are responsible by the decreasing of blood pressure and bradycardia observed in the in vivo experiments. In this way, the results observed were promising, showing the possibility of new therapeutic option for hypertensive patients, in the future. However, further studies will be necessary to better clarify the mechanisms of action of the imide-3 on the cardiovascular system.
Schematic representation of the possible signaling pathway of the vasorelaxant response induced by Imide-3. Imide-3 acts blocking Ca2+ influx by Cav and ROC, reducing intracellular calcium concentration and leading to vasodilation in smooth muscle cells. Additional studies will be needed to assess whether the inhibition of SOC do not participate of the mechanism of action of this itaconimide. IP3R, inositol-1,4,5-trisphosphate receptor; RyR, Ryanodine receptor; Ca2+, calcium ion; ROC, receptor-operated channels; SOC, store-operated channels; Cav, voltage-sensitive Ca2+ channels
References
Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015;28:355–61. https://doi.org/10.1093/ajh/hpu151.
Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–18. https://doi.org/10.1161/CIRCULATIONAHA.117.032582.
Cuspidi C, Tadic M, Grassi G, Mancia G. Treatment of hypertension: the ESH/ESC guidelines recommendations. Pharmacol Res. 2018;128:315–21. https://doi.org/10.1016/j.phrs.2017.10.003.
Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circ Res. 2015;116:1074–95. https://doi.org/10.1161/CIRCRESAHA.116.303603.
La SAD, Segura J, Banegas JR, Gorostidi M, La CJJD, Armario P, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902. https://doi.org/10.1161/HYPERTENSIONAHA.110.168948.
Hanselin MR, Saseen JJ, Allen RR, Marrs JC, Nair KV. Description of antihypertensive use in patients with resistant hypertension prescribed four or more agents. Hypertension. 2011;58:1008–133. https://doi.org/10.1161/HYPERTENSIONAHA.111.180497.
Siddiqui M, Dudenbostel T, Calhoun DA. Resistant and refractory hypertension: antihypertensive treatment resistance vs treatment failure. Can J Cardiol. 2016;32:603–6. https://doi.org/10.1016/j.cjca.2015.06.033.
Bai R-R, Wu X, Xu J. Current natural products with antihypertensive activity. Chin J Nat Med. 2015;13:721–9. https://doi.org/10.1016/S1875-5364(15)30072-8.
Tempesta MS, Corley DG, Beutler JA, Metral CJ, Yunes RA, Giacomozzi CA, et al. Phyllanthimide, a new alkaloid from Phyllanthus sellowianus. J Nat Prod. 1988;51:617–8. https://doi.org/10.1021/np50057a036.
Calixto JB, Yunes RA, Neto AS, Valle RM, Rae G. Antispasmodic effects of an alkaloid extracted from Phyllanthus sellowianus: a comparative study with papaverine. Braz J Med Biol Res. 1984;17:313–21.
Cechinel Filho V, Nunes RJ, Calixto JB, Yunes RA. Inhibition of guinea-pig ileum contraction by Phyllanthimide analogues: structure-activity relationships. Pharm Sci. 1995;1:399–401. https://doi.org/10.1111/j.2042-7158.1995.tb00450.x.
Pontes ZBVS, Lima EDO, Cechinel Filho V. Profile of susceptibility in vitro of Trichosporon asahii and Trichosporon inkin strains against cyclic imides. Rev Bras Ciências Farm. 2007. https://doi.org/10.1590/S1516-93322007000200014.
Cechinel Filho V, Yunes RA. Estratégias para a Obtenção de Compostos Farmacologicamente Ativos a partir de Plantas Medicinais. Conceitos sobre Modificação Estrutural para Otimização da Atividade. Quim Nova. 1998;21:99–105. https://doi.org/10.1590/S0100-40421998000100015.
Prado SRT, Cechinel-Filho V, Campos-Buzzi F, Corrêa R, Cadena SMCS, De Oliveira MBM. Biological evaluation of some selected cyclic imides: mitochondrial effects and in vitro cytotoxicity. Zeitschrift Fur Naturforsch - Sect C J Biosci. 2004;59:663–72. https://doi.org/10.1515/znc-2004-9-1010.
Seto SW, Bexis S, McCormick PA, Docherty JR. Actions of thalidomide in producing vascular relaxations. Eur J Pharmacol. 2010;644:113–9. https://doi.org/10.1016/j.ejphar.2010.06.035.
Ribeiro ÊAN, Furtado FF, Noldin VF, Corrêa R, Cechinel-Filho V, de Medeiros IA. Vasorelaxant action of N-p-nitrophenylmaleimide in the isolated rat mesenteric artery. Zeitschrift Fur Naturforsch - Sect C J Biosci. 2010;65 C:451–7. https://doi.org/10.1515/znc-2010-7-806.
Stiz D, Corrêa R, D’Auria FD, Simonetti G, Cechinel-Filho V. Synthesis of cyclic imides (methylphtalimides, carboxylic acid phtalimides and itaconimides) and evaluation of their antifungal potential. Med Chem (Los Angel). 2016;12:647–54. https://doi.org/10.2174/1573406412666160229150833.
Silva DF, Araújo IGA, Albuquerque JGF, Porto DL, Dias KLG, Cavalcante KVM, et al. Rotundifolone-induced relaxation is mediated by BKCa channel activation and Cav channel inactivation. Basic Clin Pharmacol Toxicol. 2011;109:465–75. https://doi.org/10.1111/j.1742-7843.2011.00749.x.
Dantas BPV, Alves QL, de Assis KS, Ribeiro TP, de Almeida MÔM, de Vasconcelos AP, et al. Participation of the TRP channel in the cardiovascular effects induced by carvacrol in normotensive rat. Vascu Pharmacol. 2015;67:48–58. https://doi.org/10.1016/j.vph.2015.02.016.
Godo S, Shimokawa H. Endothelial functions. Arterioscler Thromb Vasc Biol. 2017;37:e108–e114114. https://doi.org/10.1161/ATVBAHA.117.309813.
Kang KT. Endothelium-derived relaxing factors of small resistance arteries in hypertension. Toxicol Res. 2014;30:141–8. https://doi.org/10.5487/TR.2014.30.3.141.
Ganitkevich VY, Isenberg G. Depolarization-mediated intracellular calcium transients in isolated smooth muscle cells of guinea-pig urinary bladder. J Physiol. 1991;435:187–205. https://doi.org/10.1113/jphysiol.1991.sp018505.
Mills RD, Mita M, Walsh MP. A role for the Ca2+-dependent tyrosine kinase Pyk2 in tonic depolarization-induced vascular smooth muscle contraction. J Muscle Res Cell Motil. 2015;36:479–89. https://doi.org/10.1007/s10974-015-9416-2.
Kobayashi S, Kanaide H, Nakamura M. Complete overlap of caffeine- and K+ depolarization-sensitive intracellular calcium storage site in cultured rat arterial smooth muscle cells. J Biol Chem. 1986;261:15709–13.
Kobayashi S, Kanaide H, Nakamura M. K+-depolarization induces a direct release of Ca2+ from intracellular storage sites in cultured vascular smooth muscle cells from rat aorta. Biochem Biophys Res Commun. 1985;129:877–84.
Ziolkowski N, Grover AK. Functional linkage as a direction for studies in oxidative stress: α-adrenergic receptors. Can J Physiol Pharmacol. 2010;88:220–32. https://doi.org/10.1139/Y10-013.
Jackson WF. Ion channels and vascular tone. Hypertension. 2000;35:173–8. https://doi.org/10.1161/01.HYP.35.1.173.
Cox RH, Rusch NJ. New expression profiles of voltage-gated ion channels in arteries exposed to high blood pressure. Microcirculation. 2002;9:243–57. https://doi.org/10.1038/sj.mn.7800140.
Joseph BK, Thakali KM, Moore CL, Rhee SW. Ion channel remodeling in vascular smooth muscle during hypertension: Implications for novel therapeutic approaches. Pharmacol Res. 2013;70:126–38. https://doi.org/10.1016/j.phrs.2013.01.008.
McCulloch AI, Bottrill FE, Randall MD, Hiley CR. Characterization and modulation of EDHF-mediated relaxations in the rat isolated superior mesenteric arterial bed. Br J Pharmacol. 1997;120:1431–8. https://doi.org/10.1038/sj.bjp.0701066.
Wynne BM, Chiao C-W, Webb RC. Vascular smooth muscle cell signaling mechanisms for contraction to angiotensin II and endothelin-1. J Am Soc Hypertens. 2009;3:84–95. https://doi.org/10.1016/j.jash.2008.09.002.
Calixto JB, Santos ARS, Cechinel Filho V, Yunes RA. A review of the plants of the genus Phyllanthus: their chemistry, pharmacology, and therapeutic potential. Med Res Rev. 1998;18:225–58. https://doi.org/10.1002/(SICI)1098-1128(199807)18:4%3c225:AID-MED2%3e3.0.CO;2-X.
Leung FP, Yung LM, Yao X, Laher I, Huang Y. Store-operated calcium entry in vascular smooth muscle. Br J Pharmacol. 2008;153:846–57. https://doi.org/10.1038/sj.bjp.0707455.
Goulopoulou S, Webb RC. Symphony of vascular contraction: how smooth muscle cells lose harmony to signal increased vascular resistance in hypertension. Hypertension. 2014;63:e33–e39. https://doi.org/10.1161/HYPERTENSIONAHA.113.02444.
Macêdo CL, Vasconcelos LHC, De C Correia AC, Martins IRR, De Lira DP, De O Santos BV, De A Cavalcante F, Da Silva BA. Mechanisms underlying vasorelaxation induced in rat aorta by galetin 3,6-dimethyl ether, a flavonoid from piptadenia stipulacea (benth.) ducke. Molecules. 2014;19:19678–95. https://doi.org/10.3390/molecules191219678.
Fernandez RA, Sundivakkam P, Smith KA, Zeifman AS, Drennan AR, Yuan JX-J. Pathogenic role of store-operated and receptor-operated channels in pulmonary arterial hypertension. J Signal Transduct. 2012;2012:1–16. https://doi.org/10.1155/2012/951497.
Earley S. Molecular diversity of receptor operated channels in vascular smooth muscle: a role for heteromultimeric TRP channels? Circ Res. 2006;98:1462–4. https://doi.org/10.1161/01.RES.0000231255.32630.df.
Yu J, Bose R. Calcium channels in smooth muscle. Gastroenterology. 1991;100:1448–600. https://doi.org/10.1016/0016-5085(91)90802-R.
Garcia DCG, Pereira AC, Gutierrez SJC, Barbosa-Filho JM, Lemos VS, Côrtes SF. Structure-related blockage of calcium channels by vasodilator alkamides in mice mesenteric artery. Vascul Pharmacol. 2016;82:60–5. https://doi.org/10.1016/j.vph.2016.05.001.
Kubo T, Taguchi K, Ueda M. L-type calcium channels in vascular smooth muscle cells from spontaneously hypertensive rats: effects of calcium agonist and antagonist. Hypertens Res Off J Jpn Soc Hypertens. 1998;21:33–7. https://doi.org/10.1291/hypres.21.33.
Hirata S, Enoki T, Kitamura R, Vinh VH, Nakamura K, Mori K. Effects of isoflurane on receptor-operated Ca2+ channels in rat aortic smooth muscle. Br J Anaesth. 1998;81:578–83. https://doi.org/10.1093/bja/81.4.578.
Acknowledgements
This work was funded by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior), FAPESB (Fundação de Amparo à pesquisa do estado da Bahia) and CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moraes, R.A., Alves, Q.L., Camargo, S.B. et al. Itaconimides derivatives induce relaxation in mesenteric artery and negative inotropism by inhibition of CA2+ influx. Pharmacol. Rep 72, 890–902 (2020). https://doi.org/10.1007/s43440-019-00051-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-019-00051-8