Abstract
Embryonic stem cells (ESCs) can uniquely proliferate indefinitely and differentiate into all cell lineages. ESCs may therefore provide an unlimited supply of cells for cell-based therapies. Previous study reported the presence of hyperpolarization-activated inward currents in undifferentiated mouse (m) ESCs, but the functional role of this hyperpolarization-activated current in mESCs is unknown. In this study, the role of this current in maintaining the proliferative capacity and the cell cycle progression of ESCs was investigated. In D3 mESCs, this hyperpolarization-activated inward current can be blocked by HCN channel blocker ZD7288. Application of the HCN channel blockers, cesium (1–10 mM) or ZD7288 (0.1–30 μM), attenuated cell proliferation in a concentration-dependent manner. Both HCN blockers were found to be non-cytotoxic to mESCs as determined by cell viability test. Interestingly, ZD7288 at 10 and 30 μM was found to decrease the proportion of cells in G0/G1 phase and increase the proportion of cells in S phase. This suggests that this hyperpolarization-activated current can affect the cell cycle progression in mESCs. In summary, the present investigation suggests that ESC proliferation and cell cycle progression can be regulated by this hyperpolarization-activated current.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Embryonic stem cells (ESCs) are derived from the inner cell mass of blastocysts. They can self-renew and are pluripotent, meaning that they can proliferate indefinitely and have the ability to differentiate into all cell lineages. Concerning the proliferative characteristic, numerous reports showed that ESCs have atypical cell cycle regulation when compared with somatic cells [10, 13, 14, 18, 36]. In somatic cells, when cells progress through the cell cycle, there are rhythmic rise and fall of the expressions of cyclin E, A, and B and also the activities of cyclin-dependent kinases (cdks). However, in ESCs, these cell cycle regulators, except cyclin B, are present at relatively stable levels throughout the cell cycle [10, 28]. In addition, the activities of various cdks are maintained at high level throughout the cell cycle in ESCs; cell cycle oscillation of the kinase activity is detected only with cyclin B/Cdc2 [28]. All these previous findings suggested that ESCs have unique cell cycle regulation. Since ESCs are pluripotent, they have been suggested to act as a potential source of differentiated cells for cell-based therapies [15, 31, 38]. However, due to the extremely active cell cycle and the unlimited proliferation ability of ESCs, potential tumor formation problem is one of many hurdles that need to be overcome. A deeper understanding of how ESCs control the cell cycle progression may help in providing insights into the possible strategies of eliminating the risk of tumor formation after transplantation.
Hyperpolarization-activated cyclic nucleotide-gated (HCN) channels are ion channels that open in response to membrane hyperpolarization; and this HCN channel opening would in turn lead to membrane depolarization due to the influx of a mixed current of Na+/K+ [4, 6, 26]. HCN channels are therefore classically known as “pacemaker channels” since they mediate the inward movement of cations which contribute to spontaneous rhythmic activity within groups of heart and brain cells [4, 6, 26]. However, function(s) of HCN channels in ESCs, a type of non-excitable cells, is largely unexplored.
Interestingly, previous study reported the presence of a cesium-sensitive hyperpolarization-activated inward current in undifferentiated mouse (m) ESCs by patch clamping [35]. However, the functional role of this current in maintaining the characteristics of mESCs has never been explored. In the present study, by employing HCN channel blockers ZD7288 and cesium, we aimed to dissect the potential roles of this current in the proliferation and cell cycle progression of mESCs.
Materials and methods
Maintenance of mESCs
The mESC line D3 (ATCC, USA) was used. It was maintained on gelatin-coated culture dishes without feeder layer and propagated in Dulbecco's modified Eagle's medium (Invitrogen) supplemented with 15% fetal bovine serum (Hyclone), 2 mM l-glutamine, 0.1 mM ß-mercaptoethanol, 0.1 mM nonessential amino acids, and 1,000 U/ml leukemia inhibitory factor (Chemicon), similar to the way we described recently [32, 35].
Whole cell patch clamp recording
Trypsinized mESCs were plated in 35 mm dish attached to the stage of an inverting microscope (Nikon) and were allowed to settle down for half an hour. Cells were continuously perfused with external solution containing (in millimolar) 145 NaCl, 5 KCl, 1.8 CaCl2, 1 MgCl2, 10 HEPES, and 10 glucose, with pH 7.4 adjusted with NaOH and 295–320 mOsm in osmolarity. The membrane currents were recorded using an Axopatch 200B patch amplifier (Axon Instruments) and digitized with a Digidata 1440 A/D converter and Clampex 10.0 software (Molecular Devices). Recording pipettes were pulled from borosilicate glass tubing with a horizontal puller (P-97, Sutter Instruments), fire polished by using a FP-830 fire polisher (Narishige), and typically had a resistance of 3.0–5.0 MΩ when filled with pipette solution containing (in millimolar) 140 KCl, 10 EGTA, 10 HEPES, and 5 MgATP, with pH 7.3 adjusted with KOH and 290–310 mOsm in osmolarity. After the establishment of whole-cell configuration, the adjustment of capacitance compensation and series resistance compensation was done before recording the membrane signals. Of the series resistance, 70–80% was compensated electronically. Signasls were filtered at 2 kHz and digitized at 10 kHz. Leak subtraction protocol was performed. ZD7288 was applied with a fast step perfusion system (SF-77B; Warner Instruments) through 3-barrel square glass tubing. The distance from the tube mouth to the cell examined was around 100 μm. The application of each drug could be driven by gravity and controlled by the corresponding valve.
Cell proliferation assay and viability test
Cell proliferation was determined in 24-well plates by simple cell counting techniques. mESCs were treated with different concentrations of ZD7288 [chemical name: 4-(N-ethyl-N-phenylamino)-1,2-dimethyl-6-(methylamino) pyrimidinium chloride] or Cs+ for the entire period of the experiments. Medium was changed daily. Cells were collected at different time points for cell counting. Cells treated with equal volume of water (solvent for ZD7288 and Cs+) were used as control. Numbers of viable and non-viable cells were determined by trypan blue exclusion assay.
Cell cycle analysis by flow cytometry
Cells were collected by trypsinization for subsequent cell cycle analysis. For analysis of DNA content, cells were fixed in 70% ethanol, rehydrated in PBS, treated for 30 min with RNase A (1 mg/ml) and for 5 min with propidium iodide (1 mg/ml). Fluorescence intensity was determined by flow cytometry on FACSCanto (BD Pharmingen). Data acquisition was performed with the CellQuest software (BD Pharmingen), and the percentages of G0/G1, S, and G2/M phase cells was calculated with the MODFIT software program.
Cell cycle synchronization
mESC line D3 was cultured on gelatin-coated culture dishes without feeder layer at a concentration of 5 × 104 cells/well of 6-well plates. Cell synchronization was then performed as previously described [10, 21]. For synchronization of cell at G0/G1 phase, mESCs were first treated with 2.5 mM thymidine (Sigma) for 12 h, then washed twice with prewarmed PBS and then released into prewarmed medium for 6 h. These cells were treated with 0.5 mM mimosine (Sigma) for 6 h [10, 21]. For synchronization at S phase, mESCs were first treated with 2.5 mM thymidine for 12 h and then washed twice with prewarmed PBS and released into prewarmed medium for 12 h. mESCs were blocked by 2.5 mM thymidine again for another 12 h, washed twice with prewarmed PBS, and released into prewarmed medium for 3 h [21]. For synchronization at M phase, ESCs were first treated with 2.5 mM thymidine for 12 h, then washed twice with prewarmed PBS and incubated in the presence of 150 ng/ml of TN-16 (Biomol) for 5 h [10]. Synchronized cells were collected for subsequent cell cycle analysis and protein extraction.
Plasma membrane and cytosolic fractionation
Protein was extracted using homogenizing buffer (0.32 M sucrose, 5 mM Tris at pH 7.4, phosphatase, and protease inhibitors). Lysate was centrifuged at 500×g for 10 min at 4°C. The supernatant was further centrifuged at 100,000×g for 1 h at 4°C to separate the cytosolic (supernatant) and plasma membrane (pellet) fraction. The pellet was resuspended with buffer containing 20 mM HEPES, 1 mM EDTA, 10% glycerol, 120 mM KCL, and 2% Triton X-100. Protein concentration was determined using Bradford assay.
Total protein extraction
Cell lysates were made using RIPA lysis buffer (0.5 M Tris–HCl at pH 7.4, 10% NP-40, 1.5 M NaCl, 10 mM EDTA, 2.5% deoxycholic acid, 1 mM DTT, phosphatase and protease inhibitors) and centrifuged at 2,900×g, 4°C for 20 min. Protein concentration was determined using Bradford assay.
Western blot analysis
Protein samples were first mixed with sample buffer (125 mM Tris at pH 6.8, 4% SDS, 20% glycerol, 0.06% bromophenol blue, 10% beta-mercaptoethanol). They were then separated using 6% or 10% SDS-polyacrylamide gel electrophoresis. Gels were transferred to polyvinylidene difluoride membranes and blocked with 5% non-fat dry milk in TBST for 1 h. Blots were incubated with primary antibody overnight at 4°C in 5% non-fat milk. For pre-absorption control, primary antibody was firstly incubated with antigen with ratio of 1 μg of antigen for 1 μg of antibody at room temperature for 2 h as suggested by the manufacturer. After washing with TBST, blots were incubated with horseradish peroxidase-conjugated secondary antibodies at a dilution of 1:5,000 in 5% non-fat milk for 1 h at room temperature. After washing with TBST, signals were obtained using ECL detection reagents (Perkin Elmer). Primary antibodies and dilutions used were: rabbit polyclonal anti-HCN2 1:400 (Alomone), rabbit polyclonal anti-HCN3 1:400 (Alomone), mouse monoclonal anti-cyclin B1 1:200 (Santa Cruz), mouse monoclonal anti-TATA-box binding protein (TBP) 1:1,000 (Abcam), rabbit polyclonal anti-β-tubulin 1:1,000 (Santa Cruz), mouse monoclonal anti-GAPDH 1:10,000 (Ambion), and mouse monoclonal anti-Na+/K+-ATPase 1:1,000 (Abcam). Secondary antibodies and dilutions used were: rabbit anti-mouse, goat anti-rabbit, all at 1:5,000 dilution (Dako). In case of quantitation of protein expression, the integrated density value of the protein of interest was first normalized to that of the loading control protein of the same sample; the values in each group were then normalized to the values of the S-phase synchronized cells (i.e., normalized value of S-phase synchronized cells was 1).
Membrane potential measurement by membrane potential-sensitive dye followed by flow cytometry
To determine the membrane potential of the whole-cell population, staining by voltage-sensitive dye followed by flow cytometry was preferred to other methods. After trypsinization, cells were divided into two groups: unstained group and DiBAC4(3)-treated group in which cells were resuspended in 500 ul HEPES solution and incubated with 500 nM DiBAC4(3) (Invitrogen) for 10 min at 37°C [19, 23]. Cells were used directly for membrane potential measurement after incubation. Fluorescence intensity was determined on FACSCanto (BD Pharmingen). Winmdi software program was used to generate picture of unstained and DiBAC4(3)-treated group overlay. Peaks of unstained populations of different groups were aligned so that the difference between stained populations could be determined.
Statistical analysis
The results were expressed as mean ± SEM. Statistical significance between two groups of means was determined using unpaired Student's t test. P < 0.05 was considered to be statistically significant.
Results
Presence of hyperpolarization-activated inward currents and HCN3 proteins in undifferentiated mESCs
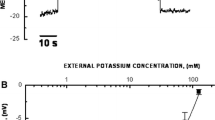
By using patch clamp techniques, a hyperpolarization-activated inward current was detected in the undifferentiated mESC line D3 (Fig. 1), similar to what has been observed for another mESC line R1 [35]. There were time-dependent and voltage-dependent components of this hyperpolarization-activated inward current (Fig. 1). In addition, this current could be blocked by specific HCN blocker ZD7288 at 30 μM (Fig. 1). Therefore, this current possesses characteristics resembling the current mediated by HCN channel proteins [26]. HCN channels can exist as homotetramer or heterotetramer of different HCN isoforms HCN1–4 [4, 6, 26]. By employing gene expression profiling techniques, PCR fragments corresponding to part of HCN2 and HCN3 transcripts, but not that of HCN1 and HCN4 transcripts, were detected in mESCs in the same previous report [35]. In the present investigation, to determine the isoform(s) of HCN channel proteins expressed in mESCs which may mediate the hyperpolarization-activated inward current observed, undifferentiated mESCs were subjected to western blot. Plasma membrane protein and cytosolic protein were isolated from mESCs. Na+/K+-ATPase and GAPDH were used as loading controls for plasma membrane protein and cytosolic protein, respectively. HCN2 protein could not be detected in both the membrane and the cytosolic fractions of mESCs (100 μg proteins per lane were used), while it was present in the plasma membrane fraction of the control mouse brain cell lysate (Fig. 2A). In contrast, HCN3 protein was found to be present in the plasma membrane fraction but not the cytosolic fraction of mESCs (Fig. 2B).
A (Left panels) HCN2 protein could not be detected in mESCs although HCN2 antibodies were shown to be working by the positive control mouse brain lysate. (Right panels) Preincubation with the antigenic peptide was performed to ensure the specificity of the bands. B (Left panels) HCN3 protein was found to be present in the plasma membrane fraction of mESC protein lysate while it could not be detected in the cytosolic fraction of mESC protein lysate. (Right panels) Preincubation with the antigenic peptide was performed to ensure the specificity of the bands
HCN channel blockers decreased mESC proliferation without affecting the survival of mESCs
Application of the HCN channel blocker Cs+ at 1–10 mM, a concentration range that is commonly used for blocking HCN channels, was found to cause a concentration-dependent decrease in proliferation of undifferentiated mESCs by simple cell counting at 72 h (Fig. 3A). To further investigate if HCN channel blockers can affect the survival of mESCs, the percentage of viable cells was studied by the trypan blue exclusion assay. Same concentration of Cs+ did not affect mESC viability (Fig. 3B). To ensure specificity of the blockade, the effect of another HCN blocker, ZD7288, was also investigated. Consistently, ZD7288 at 0.1–30 μM was also found to block mESC proliferation in a concentration-dependent manner over a period of 72 h (Fig. 3C). Similarly, it was found that ZD7288 (0.1–30 μM) treatment did not decrease mESC viability (Fig. 3D).
A Effects of Cs+, a non-specific blocker of HCN channels, on mESC proliferation. Application of Cs+ decreased mESC proliferation in a concentration-dependent manner at 72 h. The viable cell numbers in each group were normalized to that of control. Values are mean ± S.E.M. of four experiments. **p < 0.01 and ***p < 0.001 vs. control group. B Effects of Cs+ on the viability of mESCs. 1–10 mM Cs+ did not decrease the viability of mESCs at 72 h when compared with that of control. Values are mean ± S.E.M. of four experiments. C Effects of ZD7288, a specific blocker of HCN channels, on mESC proliferation. Application of ZD7288 attenuated the increase in cell number of mESCs in a concentration-dependent manner. Values are mean ± S.E.M. of three to five experiments. *p < 0.05 for 10 μM ZD7288 group vs. control group while †p < 0.05 for 30 μM ZD7288 group vs. control group. D Effects of ZD7288 on the viability of mESCs. 0.1–30 μM ZD7288 did not decrease the viability of mESCs when compared with that of control. Values are mean ± S.E.M. of three to five experiments
HCN channel blockers decreased the proportion of cells in G0/G1 phase and increased the proportion of cells in S phase
The cell cycle distribution of undifferentiated mESCs after application of HCN blockers was summarized in Fig. 4. Application of ZD7288 led to a decrease in the proportion of cells in the G0/G1 phase and an increase in the proportion of cells in the S phase in a concentration-dependent manner. While the percentage of cells in G0/G1 phase in control mESCs was 29.46 ± 1.38%, 10 and 30 μM ZD7288 decreased the percentage to 23.59 ± 1.22% (p < 0.05 vs. control) and 15.45 ± 0.57% (p < 0.01 vs. control), respectively (Fig. 4). In addition, the proportion of cells in S phase increased from 56.33 ± 0.57% in control mESCs to 64.18 ± 0.16% and 68.84 ± 0.97% in 10 and 30 μM ZD7288 groups, respectively (p < 0.05 in both cases vs. control; Fig. 4).
A Effects of ZD7288 on the cell cycle distribution of mESCs. 10 and 30 μM ZD7288 treatment decreased the percentage of cells in G0/G1 phase and increased the percentage of cells in S phase in a concentration-dependent manner. Values are mean ± S.E.M. of three experiments. *p < 0.05 and **p < 0.01 vs. control group. B Representative raw traces of cell cycle analysis of different groups by the Modfit program
HCN channel blockers did not affect cyclin B expression
Since cyclin B, the cyclin that is important for the G2 to M phase transition, is the only cyclin that changes its expression when undifferentiated ESCs progress through the cell cycle [10, 28], it is possible that HCN current is involved in cell cycle progression by regulating cyclin B expression. To determine the effect of HCN channel blockers on the expression of cyclin B, western blot analysis was performed on proteins of 10 and 30 μM ZD7288-treated mESCs cell lysate. TBP was used as a loading control protein. The result showed that there was no significant difference in protein expression level of cyclin B between the ZD7288-treated mESCs groups and the control group (Fig. 5).
Expression of cyclin B upon the treatment of ZD7288. (Upper panel) Representative blots showing the expression of cyclin B in mESCs upon the treatment with different concentrations of ZD7288. TBP was used as control loading protein. (Lower panel) Bar chart showing the expression of cyclin B upon ZD7288 treatment. Cyclin B protein expression was not altered in different treatment groups. Values are mean ± S.E.M. of four experiments
No differential HCN3 isoform expression was observed in different phases of the cell cycle
Since application of HCN blockers led to decrease in mESC proliferation and change in cell cycle distribution, this raises the possibility that different phases of the cell cycle express different level of HCN proteins and therefore HCN blockers have differential effects on different cell cycle phases. To determine the expression of HCN3 protein in different cell cycle phases, mESCs were treated with different reagents to arrest them to different phases of the cell cycle. After each treatment for synchronization, flow cytometry was done to analyze the cell cycle distribution (Fig. 6A). For mESCs treated with thymidine and mimosine, 70.73 ± 0.61% of the cells were synchronized to the G0/G1 phase. For simplicity, we referred these synchronized cells as “G0/G1-phase synchronized cells”. For mESCs treated with double thymidine plus a 3-h release, all (100.00 ± 0.00%) of the cells were synchronized in the S phase (we referred this as “S-phase synchronized cells”). For mESCs treated with thymidine and TN-16, 97.09 ± 0.88% of the cells were synchronized in the G2/M phase (we referred this as “G2/M-phase synchronized cells”).
A (Upper panel) Cell cycle distribution of mESCs treated with “thymidine + mimosine”, “double thymidine”, and “thymidine + TN-16” which represented “G0/G1-phase synchronized”, “S-phase synchronized”, and “G2/M-phase synchronized” mESCs, respectively. Values are expressed as mean ± S.E.M. of three to four experiments. ***p < 0.001. (Lower panel) Representative traces showing the flow cytometry data in different synchronized groups. B Expression of HCN3 in different phases of the cell cycle. (Upper panel) Representative blots showing the expression of HCN3 in mESCs synchronized at different phases of the cell cycle. TBP was used as control loading protein. (Lower panel) Bar chart showing the expression of HCN3 at different phases. HCN3 protein expressed at a similar degree at different phases of the cell cycle. Values are mean ± S.E.M. of three experiments
To investigate the expression pattern of HCN channel protein in different phases of the cell cycle, western blot analysis was performed for HCN3 protein of the synchronized mESCs cell lysate. TBP was used as a loading control protein. The result showed that there was no significant difference in protein expression level of HCN3 between mESCs synchronized to different cell cycle phases (Fig. 6B).
mESCs at S phase had a more hyperpolarized membrane potential when compared with mESCs at G2/M phase
Figure 7 showed the representative trace of the FITC intensity between unstained group and DiBAC4(3)-treated group. DiBAC4(3) is a membrane potential sensitive dye which partitions into the cells according to membrane potential. It leads to increase in fluorescence intensity during membrane depolarization [19]. By using this dye, our group previously showed that mESCs at S phase had a more hyperpolarized membrane potential when compared with mESCs at G0/G1 phase [21]. In this study, we found that S-phase synchronized mESCs showed a relatively lower FITC intensity than that of G2/M-phase synchronized mESCs (Fig. 7), indicating that S-phase synchronized cells were more hyperpolarized than G2/M-phase synchronized cells.
Representative traces of membrane potential of “S-phase synchronized” mESCs and “G2/M-phase synchronized” mESCs as determined by voltage-sensitive dye followed by flow cytometry. The x-axis represents the fluorescence intensity while the y-axis represents the number of events. Peaks on the left correspond to unstained cells in which fluorescence intensity (the “fluorescence” was attributed to autofluorescence which was unrelated to membrane potential) was low. Peaks on the right correspond to DiBAC4(3)-stained cells in which fluorescence intensity was inversely related to the negativity of membrane potential (i.e., intensity increased with membrane depolarization). “G2/M-phase synchronized” mESCs were more depolarized when compared with “S-phase synchronized” mESCs. Similar data were obtained from three independent experiments
Discussion
In the present investigation, a hyperpolarization-activated inward current which is sensitive to ZD7288 blockade was found to be present in mESCs. Application of HCN blockers, Cs+, and ZD7288 could result in a decrease in mESC proliferation. In addition, HCN blockers decreased the proportion of mESCs in G0/G1 phase and increased the proportion of mESCs in S phase. The present results suggest that functional HCN channels may negatively regulate the progression of mESCs from G1 phase to S phase such that blockade of HCN channels would favor progression of mESCs from G1 phase to S phase. However, if HCN channel blockers only function to favor entry into S phase, one may expect that an enhanced proliferation would be observed. On the contrary, an attenuation of proliferation was observed. This phenomenon can be explained if HCN blockers also increase the time of mESCs to transit through the G2 phase and subsequently the M phase. Indeed, our present study showed that mESC proliferation decreased upon HCN channel blockade, implying an increase in the duration of one round of cell cycle. Since the proportion of cells in G2/M phase remained unchanged, this in turn suggests an increase in the time spent in G2/M phase. There are numerous previous studies showing that G2 phase to M phase transition are not of tight control when compared with other transition point [37]. In many somatic cells, G1 to S phase transition is the regulatory point [3]. However, ESC cell cycle is unique and is significantly different from the cell cycle of somatic cells [36]. The expressions of cyclin (A and E)–cdk complexes do not show periodicity and are at elevated level. Only cyclin B was shown to be regulated and has expression changes during the cell cycle progression [36]. Therefore, it is possible that the transition from G2 to M phase (or the mitotic phase) is the regulatory point and that cyclin B is being tightly regulated in the cell cycle of undifferentiated ESCs.
However, although HCN channels may regulate cell cycle progression, the present study showed that application of HCN blockers did not alter cyclin B expression. In addition, the present results hint that HCN blockade may also not favor S-phase cells to enter G2/M phase. Our previous study showed that mESCs have average membrane potentials of ~ –11 mV [21]. Since HCN blockade is predicted to cause membrane hyperpolarization, we speculate that in native mESCs, hyperpolarization is needed for mESCs to progress from G0/G1 phase to S phase while depolarization is needed for ESCs to progress from S phase to G2/M phase. Consistently, previous study by our group showed that mESCs at S phase are more hyperpolarized when compared with mESCs at G0/G1 phase [21]. In addition, our present investigation showed that mESCs at S phase are also more hyperpolarized when compared with mESCs at G2/M phase. We speculate that the more hyperpolarized membrane potential in S phase (when compared with that of G0/G1 phase or G2/M phase) would activate the HCN channels, leading to depolarization. This depolarization at the end of S phase is important for cells to transit to G2/M phase. Interestingly, the membrane potential of undifferentiated mESCs was found to be relatively positive (~ −11 mV) on average [21]. At this membrane potential, time- and voltage-dependent pacemaker current (I h) through HCN channels may not be activated [4, 6, 26], while the voltage-independent instantaneous current (I inst) through HCN channels, which is a current representing a nonzero limiting open probability at positive voltage [25], may be activated. However, I h-like current in mESCs was found to be small and technically challenging to be recorded. I inst, which is typically more than tenfold smaller in amplitude than I h [25], was even more difficult to be recorded and if any, was indistinguishable from leak current during our electrophysiological recording. Indeed, most of the previous recordings on I inst were based on heterologous expression system in which plasmid harboring the HCN cDNA was transfected into cells [8, 20, 24, 25, 34]. The amplitude of I inst recorded in these cases is expected to be larger than those I inst through endogenously expressed HCN channels. Further study can be performed to investigate the effect of overexpressing HCN channels in mESCs to elucidate the role of this I inst on the proliferation and cell cycle progression of mESCs. Nonetheless, hyperpolarization in the S phase is expected to result in one or both of the below scenarios: (1) activation of HCN channels and increase in I h which would in turn lead to depolarization and deactivation of the HCN channels, resulting in a decrease in I h at the end of S phase; (2) increase in the driving force for I inst which would in turn lead to depolarization, resulting in a decrease in driving force for I inst at the end of S phase.
HCN channels can exist as homotetramer or heterotetramer of different HCN isoforms HCN1–4 [4, 6, 26]. By employing routine PCR, previous study showed the amplification of fragments corresponding to part of the HCN2 and HCN3 transcripts in mESCs [35]. In the present study, it was shown that only HCN3 protein, but not HCN2 protein, was present in the plasma membrane fraction of mESCs. This plasma membrane localization suggests that HCN3 protein may form functional channels which allow the conduction of HCN current. Our previous [21] and current investigation showed that membrane potential changes as mESCs progress through the cell cycle. In the present investigation, to dissect the possible role of HCN channels in maintaining the membrane potential of mESCs during cell cycle progression, the expressions of HCN3 channels at different phases of the cell cycle were probed. However, no differential expression of HCN3 channels was detected in mESCs at different phases, indicating that the membrane potential changes in different cell cycle phases are not directly attributed to the changes in HCN3 channel expression. Distinct from other three isoforms of HCN channels (HCN1, HCN2, HCN4), the gating of HCN channels formed by HCN3 subunits is found not to be positively regulated by cyclic nucleotides [20, 29]. Therefore, we speculate that, as discussed above, it is the membrane potential changes that affect the activity of the HCN channels formed by HCN3 which could in turn affect cell cycle progression.
So far, there are a number of HCN blockers, including Cs+, ZD7288, zatabradine, and ivabradine that have been discovered [4, 6, 26]. Among them, ZD7288 is the most widely used due to its high specificity and commercial availability. However, some previous studies showed that ZD7288 may possess non-specific effects. For instance, a previous study showed that ZD7288 at 100 μM facilitated voltage-gated calcium influx in pituitary lactotrophs [11]. Also, ZD7288 was found to block native T-type calcium currents in spermatogenic cells with an IC50 of about 100 μM [9]. In our present investigation, ZD7288 was used in a concentration range of 0.1 to 30 uM. This concentration range was commonly used for blocking HCN currents [1, 2, 12, 17]. Therefore, the ZD7288 concentrations that were used in the present study were not in the high concentration range that was found to affect other channels non-specifically. In addition, previous studies showed that mESCs do not posses voltage-gated calcium channels [35, 39, 40]. Due to these reasons, it is believed that ZD7288 at the concentration range that we used could exert specific HCN blocking effect.
In the heart, HCN channels are responsible for the rhythmic firing of action potentials in the pacemaker cells of the sino-atrial node [4, 6, 26]. In the brain, they are shown to be related to learning, memory, and epilepsy [4, 6, 26]. Although there were previous studies showing the molecular expression of HCN isoform transcripts [27, 33] or nicely demonstrating the functional expression of HCN currents [7] in non-excitable cells, to our best knowledge, there is no previous report on the function of HCN channels in non-excitable cells. In this study, it is clear that HCN blockers, cesium and ZD7288, decreased the proliferation and affected the cell cycle pattern of mESCs. Together with the finding that I h-like currents and HCN3 proteins are present in mESCs, it is possible that HCN channels may have a role in controlling mESC proliferation.
ESC differentiation derivatives are of great therapeutic potentials. However, there may be risk of tumor formation if undifferentiated ESCs are accidentally transplanted [5, 16, 22, 30]. In the present study, we found that blockade of HCN channels could lead to decrease in ESC proliferation, suggesting that knocking down of HCN3 subunits specifically may be a possible strategy of reducing the chance of tumor formation in future transplantation.
Conclusion
In summary, hyperpolarization-activated inward currents and HCN3 proteins are present in mESCs. In addition, putative HCN blockers cesium and ZD7288 affected ESC cell cycle progression and attenuated ESC proliferation. Therefore, our present study generates novel information on the role of this hyperpolarization-activated inward current and membrane potential in ESCs and may provide insights into the potential ways of controlling ESC growth and thereby decreasing the risk of tumor formation.
Abbreviations
- ESCs:
-
Embryonic stem cells
- HCN channel:
-
Hyperpolarization-activated cyclic nucleotide-gated channel
- TBP:
-
TATA-box binding protein
References
Aponte Y, Lien CC, Reisinger E, Jonas P (2006) Hyperpolarization-activated cation channels in fast-spiking interneurons of rat hippocampus. J Physiol 574:229–243
Barrow AJ, Wu SM (2009) Low-conductance HCN1 ion channels augment the frequency response of rod and cone photoreceptors. J Neurosci 29:5841–5853
Bartek J, Lukas J (2001) Mammalian G1- and S-phase checkpoints in response to DNA damage. Curr Opin Cell Biol 13:738–747
Baruscotti M, Bucchi A, Difrancesco D (2005) Physiology and pharmacology of the cardiac pacemaker (“funny”) current. Pharmacol Ther 107:59–79
Behfar A, Perez-Terzic C, Faustino RS, Arrell DK, Hodgson DM, Yamada S, Puceat M, Niederlander N, Alekseev AE, Zingman LV, Terzic A (2007) Cardiopoietic programming of embryonic stem cells for tumor-free heart repair. J Exp Med 204:405–420
Biel M, Wahl-Schott C, Michalakis S, Zong X (2009) Hyperpolarization-activated cation channels: from genes to function. Physiol Rev 89:847–885
Bolivar JJ, Tapia D, Arenas G, Castanon-Arreola M, Torres H, Galarraga E (2008) A hyperpolarization-activated, cyclic nucleotide-gated, (Ih-like) cationic current and HCN gene expression in renal inner medullary collecting duct cells. Am J Physiol Cell Physiol 294:C893–906
Chen J, Mitcheson JS, Tristani-Firouzi M, Lin M, Sanguinetti MC (2001) The S4-S5 linker couples voltage sensing and activation of pacemaker channels. Proc Natl Acad Sci USA 98:11277–11282
Felix R, Sandoval A, Sanchez D, Gomora JC, De la Vega-Beltran JL, Trevino CL, Darszon A (2003) ZD7288 inhibits low-threshold Ca(2+) channel activity and regulates sperm function. Biochem Biophys Res Commun 311:187–192
Fujii-Yamamoto H, Kim JM, Arai K, Masai H (2005) Cell cycle and developmental regulations of replication factors in mouse embryonic stem cells. J Biol Chem 280:12976–12987
Gonzalez-Iglesias AE, Kretschmannova K, Tomic M, Stojilkovic SS (2006) ZD7288 inhibits exocytosis in an HCN-independent manner and downstream of voltage-gated calcium influx in pituitary lactotrophs. Biochem Biophys Res Commun 346:845–850
Jiang YQ, Sun Q, Tu HY, Wan Y (2008) Characteristics of HCN channels and their participation in neuropathic pain. Neurochem Res 33:1979–1989
Jirmanova L, Afanassieff M, Gobert-Gosse S, Markossian S, Savatier P (2002) Differential contributions of ERK and PI3-kinase to the regulation of cyclin D1 expression and to the control of the G1/S transition in mouse embryonic stem cells. Oncogene 21:5515–5528
Kapur N, Mignery GA, Banach K (2007) Cell cycle-dependent calcium oscillations in mouse embryonic stem cells. Am J Physiol Cell Physiol 292:C1510–1518
Kehat I, Kenyagin-Karsenti D, Snir M, Segev H, Amit M, Gepstein A, Livne E, Binah O, Itskovitz-Eldor J, Gepstein L (2001) Human embryonic stem cells can differentiate into myocytes with structural and functional properties of cardiomyocytes. J Clin Invest 108:407–414
Leor J, Gerecht S, Cohen S, Miller L, Holbova R, Ziskind A, Shachar M, Feinberg MS, Guetta E, Itskovitz-Eldor J (2007) Human embryonic stem cell transplantation to repair the infarcted myocardium. Heart 93:1278–1284
Li YL, Tran TP, Muelleman R, Schultz HD (2008) Blunted excitability of aortic baroreceptor neurons in diabetic rats: involvement of hyperpolarization-activated channel. Cardiovasc Res 79:715–721
Liu N, Lu M, Tian X, Han Z (2007) Molecular mechanisms involved in self-renewal and pluripotency of embryonic stem cells. J Cell Physiol 211:279–286
Maric D, Maric I, Barker JL (1998) Buoyant density gradient fractionation and flow cytometric analysis of embryonic rat cortical neurons and progenitor cells. Methods 16:247–259
Mistrik P, Mader R, Michalakis S, Weidinger M, Pfeifer A, Biel M (2005) The murine HCN3 gene encodes a hyperpolarization-activated cation channel with slow kinetics and unique response to cyclic nucleotides. J Biol Chem 280:27056–27061
Ng SY, Chin CH, Lau YT, Luo J, Wong CK, Bian ZX, Tsang SY (2010) Role of voltage-gated potassium channels in the fate determination of embryonic stem cells. J Cell Physiol 224:165–177
Nussbaum J, Minami E, Laflamme MA, Virag JA, Ware CB, Masino A, Muskheli V, Pabon L, Reinecke H, Murry CE (2007) Transplantation of undifferentiated murine embryonic stem cells in the heart: teratoma formation and immune response. FASEB J 21:1345–1357
Petkova-Kirova P, Gagov H, Krien U, Duridanova D, Noack T, Schubert R (2000) 4-Aminopyridine affects rat arterial smooth muscle BK(Ca) currents by changing intracellular pH. Br J Pharmacol 131:1643–1650
Proenza C, Angoli D, Agranovich E, Macri V, Accili EA (2002) Pacemaker channels produce an instantaneous current. J Biol Chem 277:5101–5109
Proenza C, Yellen G (2006) Distinct populations of HCN pacemaker channels produce voltage-dependent and voltage-independent currents. J Gen Physiol 127:183–190
Robinson RB, Siegelbaum SA (2003) Hyperpolarization-activated cation currents: from molecules to physiological function. Annu Rev Physiol 65:453–480
Santoro B, Liu DT, Yao H, Bartsch D, Kandel ER, Siegelbaum SA, Tibbs GR (1998) Identification of a gene encoding a hyperpolarization-activated pacemaker channel of brain. Cell 93:717–729
Stead E, White J, Faast R, Conn S, Goldstone S, Rathjen J, Dhingra U, Rathjen P, Walker D, Dalton S (2002) Pluripotent cell division cycles are driven by ectopic Cdk2, cyclin A/E and E2F activities. Oncogene 21:8320–8333
Stieber J, Stockl G, Herrmann S, Hassfurth B, Hofmann F (2005) Functional expression of the human HCN3 channel. J Biol Chem 280:34635–34643
Swijnenburg RJ, Tanaka M, Vogel H, Baker J, Kofidis T, Gunawan F, Lebl DR, Caffarelli AD, de Bruin JL, Fedoseyeva EV, Robbins RC (2005) Embryonic stem cell immunogenicity increases upon differentiation after transplantation into ischemic myocardium. Circulation 112:I166–172
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM (1998) Embryonic stem cell lines derived from human blastocysts. Science 282:1145–1147
Tsang SY, Moore JC, Huizen RV, Chan CW, Li RA (2007) Ectopic expression of systemic RNA interference defective protein in embryonic stem cells. Biochem Biophys Res Commun 357:480–486
Varghese A, Tenbroek EM, Coles J Jr, Sigg DC (2006) Endogenous channels in HEK cells and potential roles in HCN ionic current measurements. Prog Biophys Mol Biol 90:26–37
Vemana S, Pandey S, Larsson HP (2008) Intracellular Mg2+ is a voltage-dependent pore blocker of HCN channels. Am J Physiol Cell Physiol 295:C557–565
Wang K, Xue T, Tsang SY, Van Huizen R, Wong CW, Lai KW, Ye Z, Cheng L, Au KW, Zhang J, Li GR, Lau CP, Tse HF, Li RA (2005) Electrophysiological properties of pluripotent human and mouse embryonic stem cells. Stem Cells 23:1526–1534
White J, Dalton S (2005) Cell cycle control of embryonic stem cells. Stem Cell Rev 1:131–138
Wong C, Stearns T (2005) Mammalian cells lack checkpoints for tetraploidy, aberrant centrosome number, and cytokinesis failure. BMC Cell Biol 6:6
Xue T, Cho HC, Akar FG, Tsang SY, Jones SP, Marban E, Tomaselli GF, Li RA (2005) Functional integration of electrically active cardiac derivatives from genetically engineered human embryonic stem cells with quiescent recipient ventricular cardiomyocytes: insights into the development of cell-based pacemakers. Circulation 111:11–20
Yanagida E, Shoji S, Hirayama Y, Yoshikawa F, Otsu K, Uematsu H, Hiraoka M, Furuichi T, Kawano S (2004) Functional expression of Ca2+ signaling pathways in mouse embryonic stem cells. Cell Calcium 36:135–146
Zhang YM, Shang L, Hartzell C, Narlow M, Cribbs L, Dudley SC Jr (2003) Characterization and regulation of T-type Ca2+ channels in embryonic stem cell-derived cardiomyocytes. Am J Physiol Heart Circ Physiol 285:H2770–2779
Acknowledgements
This study was supported by the Direct Grant for Research from the Chinese University of Hong Kong (CUHK) and the Lee Hysan Foundation Research Grant. Y.T.L. and C.K.W. were supported by postgraduate studentships from the CUHK. We would like to thank Ms Cecilia Sze-Lee Leung and Dr. Winnie Poon for their excellent technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lau, YT., Wong, CK., Luo, J. et al. Effects of hyperpolarization-activated cyclic nucleotide-gated (HCN) channel blockers on the proliferation and cell cycle progression of embryonic stem cells. Pflugers Arch - Eur J Physiol 461, 191–202 (2011). https://doi.org/10.1007/s00424-010-0899-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-010-0899-9