Abstract
Multicellular cardiac muscles are widely used to study cardiac (patho-)physiology in vitro. One of the potential pitfalls of such experiments is that muscles with a large diameter have a larger diffusion barrier for transport of oxygen and waste products and can thus potentially form a hypoxic core. Although a sufficiently small muscle size is critical for obtaining unambiguous data, the relationship between muscle diameter and contractile performance specifically under near-physiological conditions remains unknown. Small uniform trabeculae of various diameters isolated from LBNF1 rats were stimulated at different temperatures (27.5–37.5°C) and frequencies (1–8 Hz). Twitch contractions and rapid cooling contractures were used to assess contractile performance and SR Ca2+ load, respectively. We observed that at physiological frequencies and temperatures, contractile performance was clearly diminished in muscles with diameter >150 μm, likely due to the decreased rates of oxygen supply and waste removal. At room temperature slower contractions allow sufficient time for oxygen diffusion into the muscle core, and as a result the difference in contractile performance between the thin and thick muscles was less. Thus, in order to exclude adverse effects on contractile performance in multicellular myocardium under physiological conditions, it is essential that the preparations are of sufficient small diameter (<0.15 mm).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multicellular trabeculae and/or papillary muscles are widely used to study the (patho-)physiology of cardiac muscle. Though, as any experimental model, this in vitro model has certain limitations, it clearly possesses several unique advantages. Although whole heart preparations are closer to in vivo anatomical situation, the contractile performance assessed is generated by the heart as a whole, and is generally not normalized for cross-sectional area of the contractile machinery. In addition, assessment of intracellular ion-homeostasis in the whole heart is not unambiguous due to technical limitations. The isolated trabeculae also have distinct advantages over more reductionistic models such as isolated cardiomyocytes. Unlike isolated myocytes, load-dependent effects can be controlled or studied using cardiac trabeculae [6, 7, 11]. In addition, frequency-dependent activation is a prominent cardiac regulatory process, but in myocytes isolated from small rodents on which the bulk of cardiac research is done (rats and mice), the in vivo frequency range cannot be investigated due to technical limitations related to unloaded shortening dynamics. With the preservation of functional gap junctions and presence of other cell types like fibroblasts and endothelial cells, trabeculae are the smallest units of functional myocardium that reliably reciprocate the in vivo situation.
Trabeculae have been used as an experimental model to study the patho-physiology of cardiac function for more than three decades [5, 7, 9, 16, 18] and protocols have been developed to accurately assess both intracellular calcium transients [1] and SR functionality [2, 4]. These muscles can be obtained from all mammalian hearts, including human hearts, as well as from hearts with pathological phenotypes. However, a large number of these experiments are conducted at room temperature and, as a result of the slower kinetics, typically at sub-physiological frequencies. Recently, meaningful extrapolation of the results from these studies to normal cardiac function at body temperature and in vivo frequency range has been seriously questioned [8, 12].
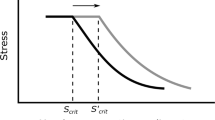
Trabecular diameter may affect its contractile properties as thicker muscles likely present a greater diffusion barrier for oxygen and nutrients. However, trabeculae of various diameters, even papillary muscles, have been used in a majority of previous studies. Schouten et al. determined that the critical diameter for cardiac muscles is ~0.2 mm in order to minimize core hypoxia-related impairment of contractile function [15]. This critical diameter was deducted from experiments at a sub-physiological temperature (26°C), and at sub-physiological frequencies (0.1–3.3 Hz). At temperatures and frequencies closer to the in vivo range, contractions are considerably faster [8, 12] allowing shorter diastolic intervals. The muscles have to spend more energy but have shorter periods of time to replenish oxygen and nutrients, as well as to wash out waste products. Thus, at physiological temperatures and frequencies, the critical diameter could very well be significantly lower than the previously determined 0.2 mm.
We thus set out to determine the diameter of trabeculae above which its dimensions can have a significant impact on their contractile parameters under physiological conditions, as well as to measure contractile parameters in muscles under and just over this critical diameter.
Materials and methods
Dissection and isolation of the trabeculae
Male LBNF1 rats (175–225 g) were anesthetized using intraperitoneal injection of sodium pentobarbital (60 mg/kg). The chest cavity was opened by bilateral thoracotomy and 1,000 U of heparin was injected into the heart at the apex. The heart was removed and immediately perfused with Krebs Henseleit (KH) solution containing (in mM) 137 NaCl, 5.0 KCl, 1.2 MgSO4, 1.2 NaH2PO4, 20 NaHCO3, 10 glucose, and 0.25 CaCl2. 2,3-butanedione monoxime (BDM; 20 mM) was added to the perfusate to minimize cutting damage, and to arrest the heart [14]. The buffer solution was oxygenated continuously by bubbling with a mixture of 95%O2/5% CO2, resulting in a constant pH of 7.4.
After flushing the blood out of the heart, the right ventricle was carefully opened and unbranched thin trabeculae were carefully dissected. A small portion of the tricuspid valve was left attached to one end, and a block of ventricular tissue remained attached to the other end of the trabeculae to facilitate mounting the muscle onto the experimental setup. Width (measured as the top-view dimension in the folded-open right ventricle) and thickness (width after the muscle was rotated 90° around the long axis) were measured in the isolated dissected muscle, and a width-to-thickness ratio was calculated. After mounting in the setup and stretching the trabecula to the experimental length, the length of the muscles was measured. Now, the width (that has become smaller than in the unloaded situation due to constant volume behavior) was re-measured, and thickness was calculated by multiplying the width in stretched position with the width/thickness ratio obtained prior. Each dimension was measured under 40× magnification (~10 μm resolution). Thus, the reported dimensions of the muscle reflect the dimensions when the actual force records were obtained.
Critical diameter protocol
After transferring the muscle to the custom-designed experimental chamber, the valvular end was connected to a hook while the ventricular cube rested on a basket-like extension of the force transducer (KG7, Scientific Instruments, Heidelberg, Germany). This method of mounting minimizes damage to the muscle [18]. Initially, the trabecula was bathed in a circulating KH solution (without BDM) and with 0.25 mM calcium, after which calcium was increased to 1.5 mM. We used an ultra-small chamber, ~150 μl volume that was perfused at a rate of 5 ml/min, thus, the entire bath volume was refreshed every 2 s, keeping bath oxygen completely constant during the experiment, but also between experiments, allowing a direct comparison between the muscles. The muscle was first kept completely slack and stimulated at 1 Hz and 37.5°C. Within a 10-min period, the trabeculae were stretched to its optimal length. Optimal length was defined as the length above which further lengthening resulted in a sharp increase in diastolic tension and minimal or no change in developed (=systolic minus diastolic) tension. To measure the critical diameter with a good fidelity, the pilot study included muscles (n=51) from three different protocols (including the one used in the present study). In all of these initially identical protocols, the fresh muscles were stimulated at 8 Hz, and contractions recorded, without prior intervention. In two protocols, muscles were thereafter used for other studies (mainly testing pharmacological agents). Muscles in the third group were used for the protocols in this manuscript. Muscles that were unresponsive to electrical stimuli or ones that became arrhythmic any time during this protocol or any follow-up protocol were excluded from the critical diameter assessment.
Clearly, diffusion is generally a 3-D concept. However, in our linear muscle preparations, length of the preparation is always ten times greater than the thickness, and thus this third linear dimension of diffusion does not contribute to diffusion process in any significant way. As an indicator for diffusion distance, the smaller dimension, thickness, was taken as the diffusion limitation. Width of the muscle (top view when the RV is opened) is larger than the thickness, thus contributing significantly less to perfusion. Moreover, the width-to-thickness ratio was fairly constant (thin group 0.49±0.05 and thick group 0.57±0.07), thus, for all practical purposes, thickness of the muscle is the strongest determinant of diffusion.
Thick vs thin muscle functional comparison
Muscles were stimulated initially at 1 Hz, and temperature set to 27.5°C. After stabilizing for about 20 min, the muscle was stimulated at 1, 2, and 3 Hz and a rapid cooling contracture (RCC) was recorded at each frequency. For each recorded point, muscles were allowed to stabilize for ~1–2 min. RCC was done by rapidly (<1 s) exposing the muscle to the same KH solution at 0°C while switching off the stimulation. The RCC protocol takes ~5–10 s to perform, is reproducible, reversible and can be done multiple times on the same muscle without loss of function [2, 4]. At the end of the force–frequency protocol, stimulation was returned to a baseline of 1 Hz. The same protocol was repeated at different temperatures and frequencies.
Data acquisition and analysis
Twitch contractions were continuously recorded throughout the experiment. Force development was normalized to the cross-sectional area of the trabecula to allow for comparison between muscles of different diameters, including those from previously published work. Twitches were recorded at each experimental condition upon stabilization. Data were collected and analyzed on- and offline using custom-written software (LabView, National Instruments).
After initial analysis and determination of the critical diameter, the muscles were divided into two groups, for the purpose of analysis, based on their diameter; (1) thin group with the smallest dimension ≤0.15 mm (at or below critical diameter, n=7) and (2) thick group, smallest dimension >0.15 mm (above critical diameter, n=10). Average dimensions of the two groups are given in Table 1. Data are expressed as mean±SEM unless otherwise noted. Data were statistically analyzed using Student’s t-tests (paired or unpaired) and a two-tailed value of P<0.05 was considered significant.
Results
We first identified the critical diameter in these muscle preparations for a physiological temperature and frequency. After equilibration, and sometimes a force–frequency relationship, muscles were stimulated at 8 Hz at a temperature of 37.5°C. Muscles ranged in diameter from 0.04 mm to 0.36 mm. Thus, even the thickest muscle was only about the diameter of an adult mouse papillary muscle (0.36 mm thick), and clearly smaller than a normal RV adult rat papillary muscle. All these muscles lie within the lowest range of diameters commonly used in the literature. Force per cross-sectional area was used as a measure of contractile performance. Figure 1 shows normalized force developed by 51 trabeculae, all obtained at the same preload (~ 2.2 μm), extracellular calcium concentration (1.5 mM), temperature (37°C), frequency (8 Hz), and pH (7.4). As can be clearly seen, the thinner muscles produced more force compared to their thicker counterparts. No statistically significant differences were observed in muscles in the lowest four bins (7–8 muscles/bin). Clearly, contractile function is significantly compromised in cardiac muscles of diameter >0.15 mm at 37°C and 8 Hz. We used the above-derived “critical diameter” of 0.15 mm as the cut-off diameter, and divided various sized trabeculae accordingly for the following protocols.
Muscle diameter vs force developed at 37°C and 8 Hz. Force developed by rat cardiac muscles of thickness ranging from 0.04 mm to 0.36 mm (n=51) at 8 Hz and 37°C. Data are binned according to muscle thickness into bins of n=7–8 trabeculae. Muscles <150 μm thick generally produce higher force (normalized to cross-sectional area) compared to those with thickness exceeding this critical diameter of 150 μm. No differences were observed between the four lowest bins. *Denotes P<0.05 vs the bin with the smallest diameter
We set out to evaluate the contractile function in muscles of diameter above the critical diameter at different temperature and frequencies. Based upon the critical diameter data, muscles of diameter averaging 0.11 mm (ranging 0.07–0.14 mm, n=7) are denoted as the thin group and those with diameter exceeding the critical one, were averaging 0.24 mm and are denoted as the thick group (ranging 0.17–0.46 mm, n=10). Our first observation was very obvious, force developed per cross-sectional area of the thick group was significantly lower at near-physiological temperature (32.5–37.5°C) at all frequencies (Fig. 2) compared to thinner muscles. The more demanding the experimental conditions (i.e. higher frequency and higher temperature), the more pronounced differences between thin and thick muscles become. In all of our experiments the muscles were contracting stably throughout the protocol. To ensure stability, we returned to baseline frequency of 1 Hz after completing the force–frequency relationship at every temperature. The twitch characteristics (developed force, time to peak tension, and 50% relaxation time from peak tension) before and after each force–frequency experiment were not significantly different, implying stable contractions throughout the experiment.
Fdev (active developed isometric tension) at different temperatures and frequencies in the below- vs above-critical diameter groups. It can be clearly seen that at all temperatures and frequencies the thin muscles (n=7) develop more force compared to the thick ones (n=10). *Denotes a statistically significant difference between the two groups (P<0.05)
Rapid cooling contracture revealed that amplitude of these was significantly higher for the thick group at temperature ≥30°C compared to the thin group, and this was observed across the measured range of frequencies (Fig. 3). This higher amplitude likely indicates that thicker muscles have a potentially higher SR Ca2+ load compared to the thinner group under identical experimental conditions.
Although timing parameters of the twitch contractions were not quite significantly different between the two groups (Fig. 4), this may be due to the differences in active isometric force development. Under identical loading conditions, a correlation was observed in our previous work between force of contraction and speed of relaxation [7]. Thus, the thinner group, despite having lower force does not relax faster, indicating impaired relaxation. Analysis of speed of contraction and relaxation revealed impairment of contraction and relaxation kinetics; +dF/dtmax of the thin and thick group were 1,848±450 mN/mm2/s and 887±97 mN/mm2/s, respectively, whereas the relaxation speeds (-dF/dtmax) were -1,311±356 mN/mm2/s and -681±87 mN/mm2/s in thin vs thick groups, respectively. When normalized to peak force, these parameters were similar in both groups, as expected because of the nearly identical kinetics.
Discussion
We set out to experimentally derive the critical muscle diameter below which contractile function under physiologically relevant conditions is preserved and unimpaired, as well as to demonstrate differences in contractile performance in muscles below and slightly above that critical diameter. We observed that muscles exceeding a diameter of ~150 μm showed a contractile deficit. This decrease in contractile strength above this critical diameter was directly correlated with the increase in diameter.
The concepts of, the smaller the muscle the better the function is not new, as it has been investigated in the past [3, 10, 15]. However, although a robust analysis of the critical diameter of cardiac muscles had been determined previously (Schouten and co-workers) to be ~0.2 mm, this was done at 26°C (0.1–3.3 Hz). However, under more physiological conditions, contractions follow in a much more rapid succession, and diastolic time for re-oxygenation and removal of waste products is more limited. This in turn necessitates a lower value for the critical diameter to avoid contractile dysfunction due to core hypoxia. In fact, Janssen et al., showed that a linear inverse relationship exists between muscle thickness and frequency maximum at body temperature [8]. Muscles thicker than ~100–125 μm had optimal frequencies in sub-physiological range. Also, Stuyvers et al. calculated that intracellular accumulation of free inorganic phosphates increases in proportion to muscle thickness thus resulting in contractile dysfunction and blunted force–frequency response in thicker muscles [17]. Although a difference between 0.2 mm and 0.15 mm may seem not very large, the impairment of function is very significant. Muscles of twice the critical diameter (which is about the size of a small-to-normal adult mouse papillary muscle) develop less than 50% force compared to muscles with diameter at or below the critical diameter. This would imply that under physiological conditions, even smallish murine papillary muscles are already too big in diameter to unambiguously determine contractile properties. Note that even the biggest muscle we used for this study (460 μm) is still smaller than an average adult rat papillary muscle (500–800 μm), and are still at the lower end of the spectrum generally used to assess contractile function in vitro.
Throughout the protocol, muscles of the thick group developed less force despite greater apparent SR calcium load compared to those of the thin group. This difference was more pronounced and statistically significant at all temperatures above 32°C. At temperatures closer to room temperature, the slower contractions likely allow sufficient time for oxygen to diffuse into the muscle core. These data are in close agreement to the observation of a critical diameter of 0.2 mm by Schouten et al. [15]. As temperature increases, rate of contraction also increases and oxygen diffusion becomes a limiting factor. The same limitation likely holds true for diffusion of other nutrients and removal of waste products [17].
Time to peak tension and 50% relaxation time were not significantly different between the two groups, despite lower force developed by the thick muscles. At similar frequency or β-adrenergic drive, muscles that produce smaller forces tend to have faster relaxation [7], indicating a correlation between force development and relaxation properties, most likely due to the cooperative activation of the contractile apparatus. Thus, although TTP and RT50 are similar in thin vs thick muscles, absence of a decrease in these timing parameters in the larger muscles that could be expected due to a decrease in peak developed force, likely indicates an impaired relaxation in thicker muscles, which is generally observed under hypoxic conditions [13]. Moreover, impaired relaxation of the thicker muscles is further supported by reduced speeds of contraction and relaxation, and we conclude that not only the amplitude of active force development is impaired, but that diastolic performance also suffers in muscles exceeding the critical diameter.
From the RCC amplitudes experiments one would conclude that thicker muscles have apparently increased SR Ca2+ load as evidenced by the higher RCC amplitude. However, although SR load may be increased, from the current data we cannot determine whether fractional release may be altered in thick muscles. Note, however, that hypoxia causes calcium handling to become impaired, and as a result, myofilament sensitivity may be affected as a compensatory response. The rapid cooling contractions consist of two determining factors, SR calcium load as well as the myofilament response to calcium. If myofilament calcium sensitivity would be increased as a result of hypoxia, a similar SR load will give higher RCC amplitudes. Thus, although RCCs are generally used as a measure of SR calcium load, myofilament sensitivity may also be a factor in the analysis of such experiments. However, acidosis as a result of hypoxia would generally lead to a loss in myofilament calcium sensitivity, and thus may not explain the observed apparent discrepancy between SR calcium load and contractile force. In addition, myofilament calcium sensitivity is temperature sensitive, and thus it could drastically change between body temperature and when measuring an RCC at 0°C. Despite this unresolved observation, it is nonetheless clear that thick muscles give a different result and therefore is another argument as to why contractile assessment of such thick muscles should lead to ambiguous results.
When we further divided the obtained data (in addition to the 15 data sets, not shown), into muscles that had diameters of <100 μm and those with diameters between 100 μm and 150 μm, no difference was seen between these two groups in any of the assessed parameters. Thus we conclude that, under physiological and near physiological temperature and frequencies, the critical diameter for cardiac muscles is 150 μm in order to minimize core hypoxia-related impairment of contractile function. This implies that whenever muscle dimensions exceed this critical diameter, some degree of contractile dysfunction can be expected to occur, especially under the most demanding conditions (high frequencies at body temperature).
References
Backx PH, Ter Keurs HE (1993) Fluorescent properties of rat cardiac trabeculae microinjected with fura-2 salt. Am J Physiol Heart Circ Physiol 264:H1098–H1110
Bers DM (1987) Ryanodine and the calcium content of cardiac SR assessed by caffeine and rapid cooling contractures. Am J Physiol 253:C408–C415
Blinks JR, Koch-Weser J (1963) Physical factors in the analysis of the actions of drugs on myocardial contractility. Pharmacol Rev 15:531–599
Bridge JH (1986) Relationships between the sarcoplasmic reticulum and sarcolemmal calcium transport revealed by rapidly cooling rabbit ventricular muscle. J Gen Physiol 88:437–473
de Tombe PP, ter Keurs HE (1990) Force and velocity of sarcomere shortening in trabeculae from rat heart Effects of temperature. Circ Res 66:1239–1254
Janssen PML, Hasenfuss G, Zeitz O, Lehnart SE, Prestle J, Darmer D, Holtz J, Schumann H (2002) Load dependent induction of apoptosis in multicellular myocardial preparations. Am J Physiol Heart Circ Physiol 282:H349–H357
Janssen PML, Hunter WC (1995) Force, not sarcomere length, correlates with prolongation of isosarcometric contraction. Am J Physiol Heart Circ Physiol 269:H676–H685
Janssen PML, Stull LB, Marban E (2002) Myofilament properties comprise the rate-limiting step for cardiac relaxation at body temperature in the rat. Am J Physiol Heart Circ Physiol 282:H499–H507
Kentish JC, ter Keurs HE, Ricciardi L, Bucx JJ, Noble MI (1986) Comparison between the sarcomere length–force relations of intact and skinned trabeculae from rat right ventricle Influence of calcium concentrations on these relations. Circ Res 58:755–768
Koch-Weser J, Blinks JR (1963) The influence of the interval between beats on myocardial contractility physical factors in the analysis of the actions of drugs on myocardial contractility. Pharmacol Rev 15:601–652
Kogler H, Hartmann O, Leineweber K, Nguyen van P, Schott P, Brodde OE, Hasenfuss G (2003) Mechanical load-dependent regulation of gene expression in monocrotaline-induced right ventricular hypertrophy in the rat. Circ Res 93:230–237
Layland J, Kentish JC (1999) Positive force- and [Ca2+]i-frequency relationships in rat ventricular trabeculae at physiological frequencies. Am J Physiol Heart Circ Physiol 276:H9–H18
Lecarpentier Y, Waldenstrom A, Clergue M, Chemla D, Oliviero P, Martin JL, Swynghedauw B (1987) Major alterations in relaxation during cardiac hypertrophy induced by aortic stenosis in guinea pig. Circ Res 61:107–116
Mulieri LA, Hasenfuss G, Ittleman F, Blanchard EM, Alpert NR (1989) Protection of human left ventricular myocardium from cutting injury with 2,3-butanedione monoxime. Circ Res 65:1441–1449
Schouten VJ, ter Keurs HE (1986) The force–frequency relationship in rat myocardium The influence of muscle dimensions. Pflugers Arch 407:14–17
Stull LB, Leppo M, Marban E, Janssen PML (2002) Physiological determinants of contractile force generation and calcium handling in mouse myocardium. J Mol Cell Cardiol 34:1367–1376
Stuyvers BD, McCulloch AD, Guo J, Duff HJ, ter Keurs HE (2002) Effect of stimulation rate, sarcomere length and Ca(2+) on force generation by mouse cardiac muscle. J Physiol 544:817–830
ter Keurs HE, Rijnsburger WH, van Heuningen R, Nagelsmit MJ (1980) Tension development and sarcomere length in rat cardiac trabeculae Evidence of length-dependent activation. Circ Res 46:703–714
Acknowledgements
This study was supported by the National Institutes of Health (NIH) grant RO1 HL073816—01A1 and AHA National Center Grant SDG 0235045 N (PMLJ).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raman, S., Kelley, M.A. & Janssen, P.M.L. Effect of muscle dimensions on trabecular contractile performance under physiological conditions. Pflugers Arch - Eur J Physiol 451, 625–630 (2006). https://doi.org/10.1007/s00424-005-1500-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-005-1500-9