Abstract
Strong, K+-induced contractions of rat aorta in Ca-free, Mg-free media were not accompanied by increased intracellular calcium concentration, [Ca2+]i, whereas such contractions in the presence of the divalent cations were correlated with rising [Ca2+]i as assessed by fura-2. At the same time, calcium channel blockers, a modulator of Ca2+-binding proteins, and a modulator of actin polymerization, inhibited all types of K+-induced contractions. Increasing the K+ in isotonic medium evoked a rise of 45Ca2+ binding to the plasma membrane of freshly isolated aortic cells. Although Ca2+-dependent events underlie the mechanism of K+-induced vascular contractions in both the presence and absence of Ca2+, in contrast to the view that [Ca2+]i is a key regulator of excitation-contraction coupling in smooth muscle, we suggest that the modulation of Mg2+-dependent Ca2+ binding, probably within/at the L-type calcium channel by K+, is a trigger for aortic contraction. This Ca2+ binding may then activate actin-myosin interaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is now widely accepted that K+ induces smooth muscle contractions by increasing the intracellular calcium concentration, [Ca2+]i. A key role for [Ca2+]i in this process is based on three sets of evidence: (1) both organic and inorganic Ca2+ channel blockers inhibit contractile responses to K+ [9, 41]; (2) K+ stimulates the influx of Ca2+ into smooth muscle cells [10, 18, 20, 42]; and (3) a K+-induced rise in [Ca2+]i is measurable with fluorescent probes [4, 7, 13, 18, 37].
However, recently it has been found that in Ca2+-free physiological salt solution (pCa>9) containing endothelin, depolarization by high K+ increases the force of contraction in canine coronary artery without any changes in [Ca2+]i [33]. More recently, we demonstrated that K+ evokes reversible and reproducible contractions in endothelium-denuded rat aorta bathed in Ca-free, K-rich isotonic salt solution containing EDTA [23]. The aforementioned K+-induced contraction in Ca-free solution was observed in different strains of rats [22], and it had a strict Mg2+ dependence: physiological concentrations of Mg2+ completely suppressed contractile responses; in contrast, removal of Mg2+ from Ca-free, K-rich, isotonic salt solution followed by stripping off the membrane-bound Mg2+ with EDTA produced K+ responses with amplitudes comparable to K+-induced contraction in normal Ca solution. Modulators of intracellular Ca2+ pools had no effect on K+-induced contraction in Ca-free, Mg-free medium, suggesting that this type of response is unlikely to be a function of increasing [Ca2+]i [23]. On the other hand, blockage of protein kinase C [23, 24] and tyrosine kinase (our unpublished data) did not affect this contraction, also suggesting that the K+-induced contractile response potentiated by EDTA in rat aorta is not due to altered sensitivity of the contractile apparatus to [Ca2+]i. The existence of two types of K+-induced contractions with almost the same amplitudes [23], but with different requirements for Ca2+, indicates that either a rise in [Ca2+]i is not essential for the development of contractions, or there are two mechanisms of action for contractile responses initiated by K+.
The purpose of the present study was therefore to delineate the mechanisms of K+-induced contraction in the rat aorta. The data provide evidence that the mechanisms of aortic contractions in normal Ca, K-rich medium (pCa=2.6) and in Ca-free, Mg-free, K-rich medium containing EDTA (pCa>8) are similar in nature. The K+-induced contractile responses under either condition remain Ca2+ dependent. Ca2+ may come from outside or inside smooth muscle cells; therefore, altered Ca2+ binding to subunits of the Ca2+ channels, rather than a rise in [Ca2+]i, is likely to be the trigger for vascular contractions in the rat aorta.
Materials and methods
Isometric force measurement in vascular preparations
Adult male Sprague-Dawley (SD) rats (in some experiments adult male normotensive Wistar Kyoto rats) (220–350 g) anesthetized by160 mg kg−1 pentobarbitone were killed by decapitation following the guidelines of Government and University regulations on the use of experimental animals. The thoracic aorta was isolated, trimmed and placed in isotonic salt solution (ISS; Table 1). Each aortic ring was placed in a tissue bath containing ISS bubbled with 95% O2 and 5% CO2 and mounted isometrically under a previously determined optimum resting tension (1.8–2.0 g). Isometric recording of contractile force was monitored using a force displacement transducer (Grass F-10) coupled to a Grass model 7H polygraph recorder. Only endothelium-denuded aortic rings (see below) were used in our experiments.
Fura-2 loading of vascular preparations
Aortic rings were obtained by the methods described above, turned inside out, and the luminal surface was rubbed gently with a cotton swab to remove endothelium. When pre-contracted by phenylephrine, this endothelium-denuded aorta failed to exhibit acetylcholine-evoked relaxation. Rings were then incubated either at room temperature for 2.5–3 h, or at 37°C for 1.5–2 h in a solution with the following composition (mM): NaCl 138, KCl 4.6, CaCl2 2.5, MgSO4 1.2, glucose 11, Hepes-TRIS 20 (pH 7.4), which contained 7–25 μM fura-2AM and 0.01% pluronic M-127 (final volume of solution was 3–5 ml). Loading was carried out in the dark. After loading, the rings were washed five times with 10 ml of solution (without fura-2AM and pluronic M-127) to remove the extracellular dye.
Measurement of contractility and [Ca2+]i
Each fura-2-loaded rat aortic ring was mounted vertically in a perfusion chamber with one side attached to a fixed wire and the other to a force transducer (BG10 g; Kulite Semiconductor Products). Resting tension was adjusted to 1.0–1.3 g. Tension and fluorescence ratio were displayed simultaneously in real time. The value of the first contraction in aortic rings stimulated by isotonic K-rich solution (ISS in which 80 mM NaCl was substituted by 80 mM KCl, K80 ISS; see Table 1) was taken to be 100%. The experiments were performed with a fluorimeter specially designed to measure the surface fluorescence of living tissues (Deltascan 4000 microscope system, Photon Technology International). The aortic ring was illuminated by alternating excitation wavelengths of 340 and 380 nm, and the emitted light was collected to a photo-multiplier through a 500-nm band-pass filter. The ratio of the fluorescence due to excitation at 340 nm (F 340) to that at 380 nm (F 380) was calculated from successive illumination periods and referred to as R 340/380, which reflected the relative level of [Ca2+]i. The basal levels of both R 340 and R 380 in fura-2-loaded aortic rings showed a gradual decrease with time (no more than 10%; data not shown), but this had no significant effect on the R 340/380 ratio, and was probably due to the slow loss of fura-2 or to photo-bleaching. Despite the uncertainly of the cytosolic conditions for calibration of [Ca2+]i in living tissues [37], the absolute value of basal levels of the [Ca2+]i in ISS, in Ca0Mg0 ISS, (Table 1) and in Ca0Mg0 ISS containing 0.1 mM EGTA were estimated using the formula of Grynkiewicz et al. [11] as modified by Himpens et al. [13]. The basal levels of [Ca2+]i in aortic cells bathed in these solutions were 218.3±5.4 nM (pCa=6.7), n=8; 125.4±3.3 nM (pCa=6.90), n=8 and 88.3±6.3 nM (pCa=7.1), n=12, respectively.
Isolation of single vascular muscle cells
Thoracic aortas were excised (30–40 rats per experiment) and placed in ISS1 (Table 1) bubbled with 100% O2. Each aorta was cleaned of adhering loose connective tissue and cut into rings 0.5–1 mm thick. Endothelial cells were removed by gently rubbing the internal surface with a wooden probe. The rings were washed with Ca-free K solution obtained by equimolar substitution of KCl for NaCl in Ca-free ISS1 (Ca0K130 ISS1, Table 1) and bubbled with O2. Cells were isolated at low temperature [2] using the following procedure: Rings were gently homogenized by hand in Ca0K130 ISS1 containing 20 μM EGTA at 0–2°C, first with Teflon-glass, and then with glass-glass homogenizers. The solid pellet of connective tissue was discarded and the homogenate was incubated at 0–2°C in Ca0K130 ISS1 for 2 h with 0.2% collagenase (Sigma Type 1) and 0.1% elastase (Sigma Type IV from porcine pancreas). The digested homogenate was centrifuged at 2000×g for 30 s. The pellet of packed cells was washed twice with Ca0K130 ISS1 containing 20 μM EGTA under the same conditions. The cells were re-suspended in ISS1 containing 5 μM EGTA and kept at 0–2°C. After isolation, soybean trypsin inhibitor (2 μg/ml) was added to the cell suspension. Although cells remained viable for 32 h, all experiments were performed within 3–6 h after isolation.
Cell populations were examined through an inverted microscope equipped with phase contrast optics. Cell yield was determined by counting successive fields at ×125 magnification. A specific test for cell membrane integrity with 0.1% trypan blue showed that 75–80% of our cells excluded dye. The prepared cells were long and spindle-shaped without evidence of being contracted as a result of the isolation. To assess the effect of K+ on cell length, the cell suspension was equilibrated in ISS1 at room temperature (22°C) and treated with 20 mM KCl (final concentration) (K20 ISS1, Table 1) for 2 min. Cell shortening was measured using the method described by Prichard and Ashley [35]. To ensure uniform sampling of the population, at least 35 cells per treatment were measured and a cell length histogram was constructed (see Fig. 6A).
Permeabilization of cells
To find the concentration of saponin necessary for reliable permeabilization of cells, 2×105 cells/ml were incubated with different concentrations of the detergent (2–100 μg/ml) for 10 min in Ca0K130 ISS1 containing 20 μM EGTA (pCa=7.5) and then exposed to trypan blue. The uptake of the dye was monitored to determine the proportion of permeable cells in the population. The nuclei of over 90% of the cells in suspension were stained after pre-incubation with 25 μg/ml of saponin. Consequently, 30 μg/ml saponin (97% staining) was used in our experiments.
Measurement of 45Ca2+ uptake
It has been reported that high Na+ is able to reduce Ca2+-sensitivity in skinned vascular smooth muscle cells [15]. Therefore, to further study of the influence of K+ on Ca2+ transport in permeabilized cells, we chose ISS1 containing 130 mM NaCl and 20 μM Ca2+ (pCa=4.7) (for the other components see Table 1), which, despite the relatively high Ca2+, failed to evoke any contractile responses (data not shown). Part of the cell suspension was equilibrated for 30–40 min at room temperature (22°C) in ISS1. Then aliquots (2×105 cells/ml) were pre-incubated for 10 min at room temperature with nifedipine (0.1 μM), or with saponin (30 μg/ml), or with a mixture of saponin and nifedipine. Control cells were pre-incubated under the same conditions, but with an equal quantity of distilled water instead of drugs. After treatment, aliquots of cell suspension were mixed (1:1) with aliquots of ISS1 containing CaCl2, 45CaCl2 and KCl (final concentrations: [Ca2+]ex=20 μM and [45Ca2+]ex=1.5 μCi/ml, [K+]ex=20 mM) (K20 ISS1, see Table 1). In some experiments, K20 ISS1 contained ryanodine (5 μM), the inhibitor of Ca2+ release from the sarcoplasmic reticulum [12], and oligomycin (10−6 g/ml), the metabolic inhibitor of Ca2+ transport in mitochondria [17]. To explore the influence of Mg2+ on 45Ca2+ uptake, aortic cells were treated with 20 mM K+ in medium containing 5 mM Mg2+ (K20Mg5 ISS1, Table 1). The cell suspension was incubated for 1–30 min at room temperature. The rate of Ca2+ uptake was linear for 10 min. Therefore, the incubation time taken to evaluate the rate of Ca2+ transport was limited to 5 min or less. The incubation mixture was rapidly filtered through Whatman GF/C filters, which were immediately washed five times with 6 ml ISS1 to decrease nonspecific 45Ca2+ binding to the membrane filter. After filtration of the incubation mixture, the radioactivity on the GF/C filters was determined (Universal LSC cocktail for aqueous samples, Sigma) in a scintillation counter (LS 6500, Beckman).
Measurement of 45Ca2+ efflux
To study the rate of 45Ca2+ efflux, relatively larger aortic strips weighing about 10 mg (wet weight) were used. The strips were first placed in ISS with the CaCl2 concentration reduced to 0.1 mM for 30 min before being loaded for 3 h at 22°C in an identical solution containing 5 μCi 45Ca2+/ml. After loading, tissues were washed in ISS lacking CaCl2, and containing 0.5 mM EGTA (to minimize the superficial calcium pool), and then were sequentially passed through a series of test tubes containing 1 ml of efflux medium. 45Ca2+ efflux was measured in three solutions: (3) Ca0 ISS containing 40 μM EGTA, (4) Ca0Mg0K130 ISS containing 40 μM EGTA, and (5) Ca0Mg0K130 ISS containing 0.3 mM EDTA (see Fig. 6 and figure legends). To evaluate the contributions of Ca2+ channels and Ca2+-ATPase to the mechanism of 45Ca2+ efflux from aortic cells, either 2 mM NiCl2 or 5 μM calmidazolium were added to all aforementioned solutions (3, 4 and 5) (see Fig. 7 and figure legends). The aliquots from each tube (0.8 ml) were later dissolved in 5 ml of scintillation fluid (Universal LSC cocktail for aqueous samples, Sigma). At the conclusion of each efflux experiment, the 45Ca2+ remaining in the tissue was determined. Dried tissue was dissolved in 0.5 ml of 0.1 N HCl containing 20 mM EGTA and counted for 45Ca2+ in the same scintillation fluid.
45Ca2+ efflux is expressed as nmoles g−1 min−1, as determined from the specific activity of the loading solution, and tissue wet weights.
Measurement and calculation of free concentrations of Ca2+ and Mg2+ in solutions
All solutions (Table 1) were made with de-ionized and double-distilled water. The concentrations of contaminating Ca2+ ([Ca2+]free) and Mg2+ ([Mg2+]free) in nominally ion-free solutions were measured by atomic absorption spectrophotometry (AAS-855, Nippon Jarret Ash.). [Ca2+]free and [Mg2+]free in solutions containing EGTA and EDTA were calculated using the apparent stability constants described by Martel & Smith [26, 27].
Calcium-dependent contractions of aortic rings were examined by varying the EGTA/CaEGTA ratio in the bath, and [Ca2+]free was calculated from the equation: [Ca2+]free=Kd[CaEGTA]/[EGTA], where the dissociation constant for the Ca-EGTA complex (Kd) was 350 nM [26, 27]. [Ca2+]free in Ca-EDTA buffers was calculated using Eqcal for Windows (Biosoft 1996). The concentration of Ca2+ required to give the half-maximum response (EC50) was computed by nonlinear regression using Prism 2.01 (GraphPad Software). [Ca2+]free and [Mg2+]free were expressed as pCa (−log[Ca2+]) and pMg (−log[Mg2+]), respectively.
Statistics and drug sources
Values are presented as the mean±SEM. Statistical significance was tested using Student's unpaired t-test; P<0.05 was regarded as statistically significant.
Salts and saponin were purchased from Merck (Germany). Dihydrocytochalasin B, W-7 [N-(6-aminohexyl)-5-chloro-1-naphthalenesulfonamide,HCl], ML-9 [1-(5-chloronaphthalene-1-sulfonyl)homopiperazine,HCl], HA 1077 [(5-isoquinolinesulfonyl)homopiperazine, 2HCl], ryanodine and oligomycin were obtained from Calbiochem (USA). All other drugs were purchased from Sigma (USA).
Explanation of the solution naming system
We found that conventional language was not effective in describing the 14 basic solutions and their variants used in this study. We have therefore adopted a simple system that allows the reader to see the key features of each solution when its effects are described. Table 1 shows the composition of the basic solutions used in this study. The normal physiological medium for aortic rings/strips is ISS and for fresh isolated cells, ISS1. ISS lacking either Ca2+ or both divalent cations (Ca2+and Mg2+) are termed Ca0 ISS and Ca0Mg0 ISS. ISS1 deficient in Ca2+ is Ca0 ISS1. High-K+ solutions are obtained either by substituting equimolar amounts of Na+ with K+ in ISS (K130 ISS) or by replacing 80 mM Na+ in ISS with 80 mM K+ (K80 ISS). If Ca2+ is omitted from the K+ solutions, they are described as Ca0K130 ISS and Ca0K80 ISS. High-K+ solutions lacking both divalent cations (Ca2+ and Mg2+) are termed Ca0Mg0K130 ISS and Ca0Mg0K80 ISS. K+-rich medium for cells was prepared by adding 20 mM KCl to ISS1 (K20 ISS1). Both ISS1 and K20 ISS1 lacking Ca2+ are described as Ca0 ISS1 and Ca0K20 ISS1. Specific chelators of Ca2+ and Mg2+, EGTA and EDTA, whose concentrations are indicated in the text and figure legends, were used to further reduce the concentrations of divalent cations in solutions.
Results
Contributions of [Ca2+]i and the Ca2+/Mg2+ ratio to the development of K+-induced contractions
Relationship between K+-induced force development and [Ca2+]i in rat aorta bathed in Ca0Mg0K80 containing EGTA and EDTA
Representative traces of force development (Fig. 1A) and changes in [Ca2+]i, as evaluated by fura-2 (Fig. 1B), from aortic rings bathed in solutions with different calcium concentrations show that K+-induced depolarization evoked an increase in both tension and [Ca2+]i in K80 ISS (ISS where 80 mM NaCl was substituted by 80 mM KCl, Table 1) (control), and a prominent K+-induced tension in Ca0Mg0K80 ISS containing 0.1 mM EGTA (43% of control) was potentiated to 75% of control by 3 mM EDTA. However, both the K+ response and its potentiation by EDTA were accompanied by a decline in R 340/380. It should be noted that in contrast to the high-K solution (Ca0Mg0K80 containing 0.1 mM EGTA), the low-K medium (Ca0Mg0K5 containing 0.1 mM EGTA) produced a weak contraction (6.1±0.6%, n=15 of Ca0Mg0K80 ISS containing 0.1 mM EGTA) (data not shown). The relaxation from K+-induced potentiation by EDTA, which was produced by washing the aortic rings with Ca0 ISS containing 0.1 mM EGTA, was associated with some restitution in [Ca2+]i. The second test of K+-induced contraction in Ca2+-containing medium was also accompanied by an increase in R340/380. None of the solutions caused any change in R 340/380 in unloaded rings (data not shown). Thus, these findings clearly demonstrate a dissociation between K+-induced contractions and elevated [Ca2+]i in Ca2+-deficient solutions containing Ca2+ chelators.
Simultaneous measurement of force and fura-2 fluorescence in a rat aortic ring in different solutions. A Force development. B The 340/380 nm ratio, representative of [Ca2+]i. The application of solutions is shown by numbers under the trace: 1 ISS; 2 K80 ISS; 3 Ca0 ISS containing 0.1 mM EGTA; 4 Ca0Mg0K80 ISS containing 0.1 mM EGTA; 5 Ca0Mg0K80 ISS containing 3 mM EGTA. All solutions maintained at 30°C and pH 7.42. This tracing is typical of more than 7 independent experiments
Effects of calcium channel blockers and modulators of actin polymerization on K+-induced contraction in aortic rings bathed in Ca0Mg0K80 ISS containing EDTA
K+ strongly contracted aortic rings bathed in Ca0Mg0K80 ISS (Table 1) containing either 0.04 mM EDTA (pCa=8.4) or 0.1 mM EDTA (pCa=8.9) at 37°C (46% and 63% of control, respectively; Fig. 2). Any contamination with external Ca2+ in these experiments was excluded by multiple washing (6×15 ml) of aortic rings with Ca0 ISS (Table 1) containing 0.025 mM EGTA, followed by incubation for a few minutes in this solution (Fig. 2A). We used the low concentrations of Ca2+ chelators in the aforementioned solutions to retain sufficient membrane-bound Ca2+ for the binding of organic Ca2+ channel blockers to the receptor [34]. Figure 2 demonstrates that EGTA, Ni2+, Mg2+, nifedipine and verapamil were able to produce vasodilatation in aortic rings that had been pre-contracted in Ca0Mg0K80 ISS containing various concentrations of EDTA. However, organic Ca2+ antagonists (5 μM trifluoperazine, 50 μM verapamil and 0.1 μM nifedipine) became more effective depending, perhaps, on how much residual Ca2+ and Mg2+ remained bound to the plasma membrane. Indeed, the inhibitory efficiency of the organic compounds shifted from 30–40% to 70–80% of complete relaxation of aortic rings, if the EDTA in Ca0Mg0K80 ISS was reduced from 0.1 to 0.04 mM. On the other hand, the inorganic Ca2+ antagonists (3 mM Mg2+ and 3 mM Ni2+) and 10 mM EGTA, which mainly binds Ca2+ ions, almost completely relaxed the rings (Fig. 2). Thus, the data suggest that Ca2+ is still required for K+-induced contraction in rat aorta in Ca-free, Mg-free media containing EDTA, and that these Ca2+-dependent processes appear to be targeted by various Ca2+ antagonists.
Effects of dihydrocytochalasin B, EGTA, trifluoperazine and Ca2+ channel inhibitors on K+-induced contraction in EDTA-containing solutions. A Experimental protocol. Numbers under traces identify the solutions used. Aortic rings bathed in (1) isotonic salt solution (ISS) (pH 7.45, 37°C) were contracted by substitution of ISS by (2) ISS in which 80 mM NaCl was substituted by 80 mM KCl (K80 ISS). After the relaxation of these rings in (1) ISS, they were washed in (3) zero-Ca ISS (Ca0 ISS) containing 25 μM EGTA to decrease external pCa to 7.71 and removed absorbed Ca2+ from tissue surface. Further aortic rings were washed either in (4) Ca0Mg0K80 ISS containing 0.1 mM EDTA (left graph) or (5) Ca0Mg0K80 ISS containing 0.04 mM EDTA (right graph). Inhibitors were applied at the arrows: a verapamil (50 μM), b trifluoperazine (5 μM), c nifedipine (0.1 μM), d dihydrocytochalasin B (5 μM), e NiCl2 (3 mM)/MgSO4 (3 mM) and f EGTA (10 mM). These tracings are typical of 8 independent experiments. B Summary of data on the inhibitory action of different drugs obtained in experiments according to the protocol. Contraction of aortic rings in K80 ISS was defined as 100%. Data are mean±SEM of 8 independent experiments. *P<0.05 versus either solution 4 (left graph) or solution 5 (right graph). **P<0.001 versus either solution 4 (left graph) or solution 5 (right graph)
Furthermore, aortic contractions in Ca0Mg0K80 ISS containing either 0.04 mM or 0.1 mM EDTA were inhibited not only by Ca2+ channel blockers but also by a modulator of actin polymerization, dihydrocytochalasin B (65% and 56% of complete relaxation, respectively) (Fig. 2).
Relationship between force development and [Ca2+]i in rat aorta bathed in Ca0Mg0K80 ISS (nominally free of divalent cations medium): effects of calcium channel blockers and modulators of actin polymerization
The data shown in Fig. 3A demonstrate that K+ is capable of eliciting a prominent contraction in rat aorta bathed in Ca0Mg0K80 ISS. Since the Ca2+ gradient between the cytosol and this ISS (nominally free of divalent cations) was found to remain relatively high ([Ca2+]i=125.4±3.3 nM, n=8, versus [Ca2+]ex=6200±168 nM, n=8), it was possible that high K+ could provide the rise in [Ca2+]i required for force development. To determine whether [Ca2+]i can be a trigger for K+-induced responses of rat aorta in ISS nominally free of divalent cations, [Ca2+]i and force development were measured simultaneously (Fig. 3A). In fura-2-loaded aortic rings, substitution of ISS by K80 ISS rapidly increased R 340/380 (Fig. 3A, bottom trace) and this [Ca2+]i elevation accompanied the K+-induced tension (Fig. 3A, upper trace). Washing the rings with ISS evoked relaxation, which was accompanied by restoration of [Ca2+]i to the basal level. Subsequent replacement of ISS by Ca0 ISS had no effect on muscular tone, but resulted in a reduced value of R 340/380 (Fig. 3A, bottom trace). A final replacement of Ca0 ISS by Ca0Mg0K80 ISS caused a relatively strong contraction (44% of control), but this contraction either was not accompanied by a change in [Ca2+]i or by small alterations in the [Ca2+]i that remained below the baseline level (Fig. 3A). Despite the contrasting changes in [Ca2+]i observed during K+-induced responses in a Ca2+-rich medium and those in nominally Ca2+-free, Mg2+-free solutions, both types of contraction were almost completely inhibited by Ca2+ channel blockers (nifedipine, verapamil, Ni2+ and Mg2+), a Ca2+-chelator (EGTA) and an antagonist of Ca2+ binding proteins (trifluoperazine) (Fig. 3B). Furthermore, the modulator of actin, dihydrocytochalasin B, was able to inhibit the contractions by about 65% in both solutions (Fig. 3B). Thus, these findings suggest that the K+-induced aortic contraction in nominally Ca2+-free, Mg2+-free solution is somehow associated with Mg2+-sensitive, Ca2+-dependent events in smooth muscle cells and is independent of the [Ca2+]i fluctuations.
A Simultaneous measurement of force and fura-2 fluorescence of aortic rings bathed in both normal high-K medium (K80 ISS) and in ISS nominally free of divalent cations (Ca0Mg0K80 ISS). The upper trace shows force development; the lower trace shows the 340/380 ratio (R 340/380), indicating [Ca2+]i. The solutions used are identified by numbers under the traces: 1 ISS; 2 K80 ISS; 3 Ca0 ISS; 4 Ca0Mg0K80 ISS. All solutions were maintained at 37°C and pH 7.42. This tracing is typical of 6 independent experiments. B Analysis of inhibition of K+-induced responses. Effects of different Ca2+ antagonists and a modulator of actin polymerization on aortic rings precontracted by either K80 ISS (left histogram) or Ca0Mg0K80 ISS (right histogram). The maximal relaxation induced by a mixture of EGTA (10 mM) and papaverine (0.1 mM) either in K80 ISS or in Ca0Mg0K80 ISS was defined as 100%. Data are mean±SEM of 8 dependent experiments
Relationship between Ca2+/Mg2+ ratio in solutions and K+-induced contraction in rat aorta
The data shown in Fig. 4A indicate a positive correlation between K+-induced contraction and the Ca2+/Mg2+ ratio (for low and medium concentrations of Ca2+ in the medium), either in solutions with physiological concentrations of Mg2+ (Fig. 4A, right), or in nominally Mg2+-free solutions (Fig. 4A left). This further substantiates the suggestion made above.
Relationships between the Ca2+/Mg2+ ratio and A development of the K+-induced contraction, and B, C relaxation in rat aorta. A pCa/tension curves. Ca2+ was gradually added to aortic rings bathed in either Ca0K130 ISS containing 0.1 mM EGTA (right graph) or Ca0Mg0K130 ISS containing 0.1 mM EGTA (left graph). Both solutions were maintained at 22°C and pH 7.42. The contraction of aortic rings in K130 ISS was defined as 100%. The inserts show the positive correlation between Ca2+/Mg2+ ratio and tension, derived from the above curves. Data are mean±SEM of 12 independent experiments. B Effect of Ca0K130 ISS containing EGTA on a K+-pre-contracted aortic ring. Numbers under the trace identify the solutions used: 1 ISS; 2 K130 ISS; 3 Ca0K130 ISS containing 0.02 mM EGTA. All solutions were maintained at 22°C and pH 7.42. This tracing is typical of 8 independent experiments. C Simultaneous measurements of force (upper trace) and R 340/380 (lower trace) in a rat aortic ring bathed in solutions with different Ca2+/Mg2+ ratios. Solutions are identified by numbers under the bottom trace: 1 ISS; 2 K130 ISS; 4 Ca0Mg0K130 ISS containing 0.02 mM EGTA. 3 mM Mg2+ was added at the arrow. All solutions were maintained at 22°C and pH 7.42. The tracing is typical of 6 independent experiments
Contribution of [Ca2+]i and the external Ca2+/Mg2+ ratio to the relaxation of rat aorta pre-contracted by K+
A reduction of [Ca2+]i, when Ca2+ is withdrawn from the K+-containing medium, is considered to be the dominant mechanism for relaxation in smooth muscles [4, 7, 13, 18, 37]. This mechanism was operating when aortic rings contracted by K130 ISS were washed with Ca0K130 ISS containing 20 μM EGTA (pCa=7.7 and pMg=2.9), i.e., when the washing solution contained a physiological concentration of Mg2+ (Fig. 4B). However, if aortic rings were washed with Ca0Mg0K130 ISS containing 20 μM EGTA (pCa=7.7 and pMg=5.4) that caused [Ca2+]i to drop below a basal level (Fig. 4C, bottom trace), the relaxation of K+-pre-contracted rings reached only 22.7±2.1% (P<0.01, n=6) of that produced by Ca0K130 ISS. The complete effect required the addition of 3 mM Mg2+ to Ca0Mg0K130 ISS (pMg=2.5) (Fig. 4C, upper trace). Thus, increasing the external Mg2+/Ca2+ ratio from 1.52×102 to 1.20×105 produces relaxation.
These results imply that the external Ca2+/Mg2+ ratio affects not only the development of contraction, but also contributes to relaxation of the rat aorta. Besides, they show that a decrease in [Ca2+]i is not essential for the relaxation of K+ pre-contracted rat aorta.
Effects of inhibitors of myosin light chain kinase, W-7 and ML-9, and Rho-associated kinase, HA 1077, on K+-induced contractile responses of aortic rings in Ca-free media
Figure 5 shows that pre-incubation of aortic rings for 20 min with 30 μM W-7, or 10 μM ML-9 or 10 μM HA 1077 failed to modify their contractile responses in Ca0Mg0K130 ISS containing 30 μM EDTA (see also [38]). Apparently, phosphorylation of myosin light chain is not associated with the K+-induced contraction in Ca-free medium.
Effects of the inhibitors of myosin light-chain kinase (MLCK) on K+-induced contractions in EDTA-containing solution. A Experimental protocol. Numbers under traces identify the solutions used. Aortic rings bathed in 1 ISS (pH 7.42, 37°C) were then contracted by substitution of (1) ISS by (2) K130 ISS. After relaxation of the rings in (1) ISS. they were washed in (3) Ca0 ISS containing 25 μM EGTA to decrease external pCa and remove absorbed Ca2+ from the tissue surface. Further aortic rings were washed in (4) Ca0Mg0K130 ISS containing 30 μM EDTA. The same protocol was used to explore the effects of MLCK inhibitors, W-7 (30 μM) and ML-9 (10 μM), and the Rho-associated kinase antagonist, HA 1077 (10 μM) which were added (separately) to solutions 1 and 3. This tracing is typical of 6 independent experiments. B Summary of data on the action of W-7, ML-9 and HA 1077 obtained in experiments according to the protocol. Contraction of aortic rings in K130 ISS was defined as 100%. Contraction of aortic rings in Ca0Mg0K130 containing 30 μM EDTA was taken as control. Data are mean±SEM of 6 independent experiments. *P<0.05 versus solution 2; **P>0.05 versus control
45Ca2+ uptake by intact and permeabilized aortic cells
To determine the mechanism underlying the K+-induced contraction, basal and K+-initiated 45Ca2+ uptakes were compared in intact and saponin-treated cells, where there is no Ca2+ gradient.
Most spindle-shaped cells were shortened by K+ in media containing Ca2+ (Fig. 6A). Figure 6B demonstrates that 20 mM KCl accelerated 45Ca2+ uptake, which remained linear for the first 10 min in both intact and saponin-treated cells incubated in ISS1 at 22°C. Longer treatment of these cells with 20 mM K+ appreciably inhibited 45Ca2+-uptake (Fig. 6B), as others have observed in smooth muscle [20]. Pre-incubation of cells with 0.1 μM nifedipine or application of 5 mM Mg2+ to aortic rings completely inhibited the Ca2+ uptake stimulated by K+ (Fig. 6B). The maximal K+-induced 45Ca2+ uptake in saponin-treated cells was a little less than that in controls (the maximal Ca2+ uptake was 0.31±0.015 nmol/105 cells and 0.25±0.008 nmol/105 cells, n=8, respectively) (Fig. 6B). The values of the nifedipine-sensitive augmentation of 45Ca2+ influx in saponin-treated and intact cells differed by <15% (Fig. 6C). Treatment of cells with 5 μM ryanodine and 10−6 g/ml oligomycin slightly modified the time-course of K+-induced Ca2+ uptake in permeabilized cells (data not shown). As a result, the difference in the nifedipine-sensitive increment of 45Ca2+ uptake between intact and saponin-treated cells vanished (Fig. 6D). These results imply that the inhibition of K+-initiated 45Ca2+ transport in aortic cells by nifedipine is not entirely due to the blockade of 45Ca2+ influx through channels. Hence, the inhibition of K+-activated contractions in smooth muscle by Ca2+ antagonists is probably not solely a result of the prevention of Ca2+ influx via channels or/and effect on intracellular compartments of Ca2+.
Effects on K+ on A length and B–D 45Ca2+ uptake by freshly isolated aortic cells. A Cell length histograms. Changes in length (thick line) were evaluated after application of 20 mM KCl to cells bathed in ISS1. B 45Ca2+ uptake by intact (left graph) and saponin-treated (right graph) aortic muscle cells in different solutions. 1 K20 ISS1; 2 ISS1; 3 K20Mg5 ISS1; 4 K20 ISS1 containing 0.1 μM nifedipine. Data are mean±SEM of 8 independent experiments. C K+-induced nifedipine-sensitive increment of 45Ca2+ uptake in intact (left) and saponin-treated (right) cells was calculated from results represented in B. 45Ca2+ uptake by freshly isolated cells bathed in K20 ISS1 with and without 0.1 μM nifedipine for 5 min was measured. Data are mean±SEM of 8 independent experiments. *P>0.05 versus intact cells. D The same as C, but nifedipine-sensitive increment of 45Ca2+ uptake was obtained in the presence of 5 μM ryanodine and 2×10−6 g/ml oligomycin (time-course of 45Ca2+ uptake for this graph not shown). Data are mean±SEM of 6 independent experiments. *P>0.05 versus intact cells
Influence of ions and drugs on 45Ca2+ efflux from rat aorta: relationship between K+-induced contraction in Ca-free, Mg-free medium and 45Ca2+ efflux
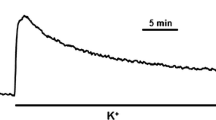
Since EDTA [10] and K+ [43] can evoke Ca2+ efflux, we correlated the Ca2+ efflux with K+-induced contraction in aortic rings in Ca-free, Mg-free solution. Fig. 7A illustrates that a prominent K+-induced contraction of aortic rings obtained after substituting Ca0 ISS containing 0.1 mM EGTA with Ca0Mg0K130 ISS containing 0.1 mM EGTA (pMg=5.47, pCa=8.15), and its potentiation by Ca0Mg0K130 ISS containing 0.3 mM EDTA, were both accompanied by accelerated 45Ca2+ efflux from aortic strips (the increments of the rate of Ca2+ efflux were 2.31±0.08 nmol g−1 min−1, n=6, and 7.77±0.41 nmol g−1 min−1, n=6, for K+ and EDTA, respectively) (Fig. 7B). The inhibitor of Ca2+-ATPase, calmidazolium (5 μM), failed to modify the Ca2+ efflux. This fact indicates that Ca2+-ATPase is unlikely to be involved in the mechanism of Ca2+ efflux in rat aorta. In contrast, the inhibitor of T- and L-type Ca2+ channels, Ni2+ (2 mM) [40], almost completely suppressed both the K+-induced contractile response and its potentiation by EDTA, associated with Ni2+-evoked reduction in K+ and EDTA effluxes by 70% and 82%, respectively (Fig. 7). This finding suggests that the K+-induced response of rat aorta in Ca-free, Mg-free medium is triggered by a Ca2+ efflux that probably takes place through Ca2+ channels.
Effects of K+ and EDTA on A contractility and B 45Ca2+ efflux from aortic rings. A Numbers under traces identify the solutions used. Aortic rings bathed in (1) ISS (pH 7.4, 22°C) were contracted in (2) K130 ISS (at the same pH and temperature). After relaxation in (1) ISS, rings were washed in (3) Ca0 ISS containing 0.1 mM EGTA to remove residual Ca2+ from solution and then were placed in (4) Ca0Mg0K130 ISS containing 0.1 mM EGTA. A final response was studied in (5) Ca0Mg0K130 ISS containing 0.3 mM EDTA. To examine the effect of Ni2+, we used the same protocol; however, solutions 4 and 5 contained 2 mM NiCl2. The tracing is typical of 15 independent experiments. B Numbers above the graph identify the solutions used. Aortic rings loaded with 45Ca2+ were bathed in the following solutions: (3) Ca0 ISS containing 0.1 mM EGTA; (4) Ca0Mg0K130 ISS containing 0.1 mM EGTA; (5) Ca0Mg0K130 ISS containing 0.3 mM EDTA. To explore the effects of blocking Ca2+ channels (Ni2+) and inhibiting Ca2+-ATPase (calmidazolium), we used the same protocol; however, solutions 4 and 5 contained either 2 mM NiCl2 or 5 μM calmidazolium. Data are mean±SEM of 6 independent experiments
Discussion
It is generally accepted that the plasma membrane of the myocyte behaves like a K+-electrode, so its potential can be calculated from the Nernst equation. Elimination of the K+ diffusion potential (depolarization) across the plasma membrane by placing smooth muscle cells in high K medium leads to activation of Ca2+ channels. As a result, an increase in [Ca2+]i occurs, primarily via Ca2+-influx, which triggers contraction. However, in this study and previously [23], it has been demonstrated that K+ induces a prominent contraction of aorta not only in high-K isotonic salt solutions (K80 ISS and K130 ISS) (pCa=2.6), but also in high-K solutions deficient in Ca and Mg (Ca0Mg0K80 ISS and Ca0Mg0K130 ISS) and containing chelators of divalent ions (pCa>9). In the former case, the contraction was accompanied by a rise in [Ca2+]i (Figs. 1, 3) that is consistent with a number of other observations on this tissue [4, 7, 13, 18, 37]; whereas in the latter case there was no rise in [Ca2+]i (Fig. 1). In fact, we observed a drop in R 340/380 below the basal level (Fig. 1). This is in agreement with the previous observation that there is a gradual decrease of the basal [Ca2+]i in rat aorta bathed in solutions where external Ca2+ ([Ca2+]ex) is diminished by Ca2+ chelators [4, 37]. In addition, the development of considerable contractions in isotonic salt solution nominally free of divalent cations (Ca0Mg0K80 ISS, pCa=5.2) was also not accompanied by a rise of [Ca2+]i (Fig. 3). These data indicate that a rise in [Ca2+]i is not an obligatory factor to trigger K+ contractions in solutions lacking Ca2+.
So, we needed to reinvestigate whether Ca2+ is essential for the K+-induced contraction. In the present study, the effects of different concentrations of external Ca2+, Ca2+ channel antagonists and the Ca2+ chelator EGTA on K+-induced contraction and relaxation were determined. This revealed that contraction is directly correlated to the concentration of external Ca2+ ([Ca2+]ex) (Fig. 4A). Inhibitors of the Ca2+ channel antagonized, while EGTA, which removes all external Ca2+, abolished all the effects in both Ca-rich and Ca- free solutions (Figs. 2,3). These observations suggest that Ca2+ is essential for the K+-induced contraction. However, since contraction still took place when [Ca2+]ex was absent (Fig. 1), influx of Ca2+ via the Ca2+ channel is not required.
In support of an important role for Ca2+, we also found that Mg2+, a competitor of Ca2+ for binding sites in Ca2+ channels [25] and other organic molecules [1, 26, 27] exerted effects on K+-induced contraction that antagonized the action of Ca2+. Firstly, the development of K+-induced contraction in Ca-free solution was obvious only after removing Mg2+ from this medium. Further application of a Mg2+ chelator, EDTA [26, 27], potentiated the K+-induced contractile responses (Figs. 1, 7). Secondly, the K+-induced contraction was greater in Ca0Mg0K80 ISS containing 0.1 mM EDTA than in Ca0Mg0K80 ISS containing 0.04 mM EDTA (Fig. 2). The greater contractile response in the former case is most likely due to less Mg2+ remaining. Thirdly, the magnitude of K+-induced smooth muscle contractions in both Mg-low and Mg-normal solutions was correlated with the Ca2+/Mg2+ ratio (Fig. 4A). Fourthly, relaxation following the K+-induced contraction in K130 ISS was complete in Ca0Mg0K130 ISS containing EGTA (pCa=7.7) only after 3 mM Mg2+ was added (Fig. 4C). Note that the inhibitory action of Mg2+ in these experiments was dissociated from the drop in [Ca2+]i, as Ca0Mg0K130 ISS containing EGTA already diminished [Ca2+]i below basal levels (Fig. 4C). Thus, these results imply that the K+-induced contraction is not only Ca2+ dependent, but also Mg2+ sensitive.
To further determine the mechanism by which Ca2+ affects the K+-induced contraction in rat aorta, we measured the uptake of 45Ca2+ into the smooth muscle cells of rat aorta (Fig. 6). It has been established that uptake increases in response to high K+. The effect was attenuated by blockade of the L-type Ca2+ channel with nifedipine and Mg2+. Interestingly and more importantly, K+ ions exerted a similar effect on nifedipine-sensitive Ca2+ uptake in intact cells and in cells treated with saponin, when the influx and efflux are the same (Fig. 6C, D), as the plasmalemma is freely permeable to Ca2+ [19]. It may be suspected that the inhibitory action of nifedipine, at least in permeabilized cells, was mediated by its interaction with calmodulin. However, it has been noted that, in contrast to some other 1,4-dihydropyridines [3, 30], nifedipine neither binds to calmodulin nor alters phosphodiesterase activity in the presence or absence of calmodulin at any of the Ca2+ concentrations employed [5]. These observations suggest that K+ may increase binding of Ca2+ in the sarcolemma and that the binding site is most likely located in the L-type Ca2+ channel.
To investigate the source of Ca2+ that contributes to contraction induced by K+ ions in Ca-free, Mg-free ISS containing EDTA, we determined the efflux of 45Ca2+. Interestingly, the efflux of Ca2+ produced by high K+ and EDTA was directly correlated to force development in both Ca0Mg0K130 containing EGTA and Ca0Mg0K130 containing EDTA (Fig. 7). Therefore, with a Ca-free external medium the only source of Ca2+ is from inside the cell. These data taken together with the inhibition of Ca2+ efflux and both contractile responses by Ni2+ (Fig. 7) suggest that K+, a natural antagonist of Mg2+ [26, 27], may replace the Mg2+ bound to the external face of ion channels in smooth muscle cells. The collapse of the external Mg2+ electrostatic barrier blocking L-type Ca2+ channels [25] by K+ entails Ca2+ efflux, which can take place through the open Ca2+ channels [21] (Fig. 7B). This efflux provides a highly localized and elevated concentration of Ca2+ near the external binding sites of the Ca2+ channel. A result of the Ca2+ efflux may be a rise in Ca2+ binding to the external mouth of the L-type Ca2+ channel, and this binding appears to be a target for calcium channel blockers.
In the present study, we also found that modification of actin polymerization by dihydrocytochalasin B resulted in suppression of K+-induced contractile responses in vascular muscle in both Ca-containing and Ca-free solutions (Figs. 2, 3), suggesting that polymerization of myofilaments contributes, at least in part, to K+-induced responses of rat aorta. Results from the present study do not provide evidence that Ca2+ binding to the channel affects the conformation of thin filaments. A recent study showed direct regulation of Ca2+ channels by polymerization of actin filaments [32]. Further study is needed to determine whether changes in conformation of the pore-forming α1 subunit by Ca2+ binding shifts the conformation of thin filaments associated with these Ca2+ channels which, in turn, might initiate the formation of actin-myosin clusters resulting in the development of aortic contractions.
It is widely accepted that agonist-induced smooth muscle contraction in Ca-free medium is a result of Ca2+ sensitization of myofilaments by receptors of different agonists through mobilization of a G protein-dependent pathway and subsequent activation of various kinases (protein kinase C, tyrosine kinase, Map kinase and integrin-linked kinase) [6, 18, 39]. K+-induced contraction in Ca-free, Mg-free medium may also be due to sensitization of the contractile elements. It has been proposed that the change of membrane potential by K+ is a transducer mechanism for the alteration of myofilament Ca2+ sensitivity in smooth muscle cells [33]. However, this seems unlikely, since it was also noted that high K+ itself is unable to change the force of canine coronary artery in Ca-free, normal-Mg medium containing EGTA [33]. Possibly, sensitization of the contractile elements due to an enhancement of myosin light chain (MLC) phosphorylation at low [Ca2+]i is a more likely mechanism. We tested this hypothesis. MLC phosphorylation is determined by the balance between MLC kinase (MLCK) and MLC phosphatase (MLCP) activities [18, 39]. If [Ca2+]i remains constant in K-rich, Ca-free solution (release of Ca2+ from intracellular stores has been shown not to contribute to the K+-induced contraction; see Introduction), MLCK could only be sensitized by other kinases. However, the latter is rather unlikely because blockade of a key kinase, protein kinase C, which uses both MLC and MLCK as substrates [16, 18], did not modify the response to high K+ in rat aorta [23, 24]. In support of this, the present study has demonstrated that the response to high K+ was not altered by the inhibitors of MLCK, W-7 and ML-9 (Fig. 5). Furthermore, a lack of effect of HA 1077, an inhibitor of Rho-associated protein kinases, which inhibits MLCP activity [31], on the K+-induced contraction in Ca-free medium (Fig. 5) implies that MLCP is probably not involved in the phosphorylation of MLC upon K+ stimulation. By comparing the mechanisms of contraction in Ca-free and Ca-normal solutions, we should note that the aforementioned finding is consistent with data on ileac smooth muscle, where contraction induced by high K+ in Ca-containing medium was unaffected by the other inhibitor of Rho-associated kinase, Y-27632 [29]. However, this contradicts the data obtained very recently [28], where the inhibitory action of ML-9, Y-27632 and HA 1077 on K+-induced contraction of caudal artery in normal Ca medium was revealed. This discrepancy can be explained by the nonspecific action of these compounds. It is known that the naphthalenesulfonamide derivatives W-7 and ML-9 can interact directly with L-type Ca2+ channels [36] and inhibitors of Rho-associated protein kinases can modify the Ca2+ influx through Ca2+ channels in smooth muscles cells [14].
Thus, our experimental findings, taken together with data that K+ depolarization of smooth muscle in Ca-free medium does not induce phosphorylation significantly different from basal levels [8], indicate that the K+-induced contraction in rat aorta in Ca-free, Mg-free ISS and its potentiation by EDTA is unlikely to result from a change in the Ca2+ sensitivity of myofilaments by means of MLC phosphorylation.
In conclusion, we have provided evidence that high K+ increases the binding of Ca2+ to the external surface of the Ca2+ channel. The Ca2+ may come from both outside and inside the cell. We hypothesize that the binding of Ca2+ to the L-type Ca2+ channel may in turn trigger K+-induced contraction. Further study is, however, needed to test the hypothesis.
References
Altura BM, Altura BT (1985) New perspectives on the role of magnesium in pathophysiology in the cardiovascular system. II. Experimental aspects. Magnesium 4:245–271
Bakhramov A, Evans AM, Kozlowski RZ (1998) Differential effects of hypoxia on the intracellular Ca2+ concentration of myocytes isolated from different regions of the rat pulmonary arterial tree. Exp Physiol 83:337–347
Boström S-L, Ljung B, Mardth S, Forsen S, Thulin E (1981) Interaction of antihypertensive drug felodipine with calmodulin. Nature 292:777–778
Bruschi G, Bruschi ME, Regolisty G, Borghetti A (1988) Myoplasmic Ca2+-force relationship studied with fura-2 during stimulation of rat aortic smooth muscle. Am J Physiol 254:H840–H854
Daly MJ, Perry S, Mayer WG (1983) Calcium antagonists and calmodulin; Effect of verapamil, nifedipine and diltiazem. Eur J Pharmacol 90:103–108
Deng JT, Van Lierop JE, Sutherland C, Walsh MP (2001) Ca2+-independent smooth muscle contraction. J Biol Chem 276:16365–16373
Fay FS, Shlevin HH, Granger WC, Taylor SP (1979) Aequorin luminescence during activation of single isolated smooth muscle cells. Nature 280:506–508
Gerthoffer WT (1987) Disssociation of myosin phosphorylation and active tension during muscarinic stimulation. J Pharmacol Exp Ther 240:8–15
Godfraind T, Vanhoutte PM, Govoni S, Paoletti R (1985) Calcium entry blockers an tissue protection. Raven Press, New York
Goodman FR, Weiss GB (1971) Effect of lanthanum on45Ca movements on contractions induced by norepinephrine, histamine and potassium in vascular smooth muscle. J Pharmacol Exp Ther 177:415–425
Grynkiewicz G, Poenie M, Tsien R (1985) A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260:3440–3450
Hatem SN, Sweeten T, Vetter V, Morad M (1995) Evidence for the presence of Ca2+ channel-gated Ca2+ stores in neonatal human atrial myocytes. Am J Physiol 268:H195–H201
Himpens B, Matthijs G, Somlyo P (1989) Desensitization to cytoplasmic Ca2+ and Ca2+ sensitivities of guinea-pig ileum and rabbit pulmonary artery smooth muscle. J Physiol (Lond) 413: 489–503
Ito S, Kume H, Yamaki K, Katoh H, Honjo H, Kodama I, Hayashi H (2002) Regulation of capacitative and noncapacitative receptor-operated Ca2+ entry by rho-kinase in tracheal smooth muscle. Am J Respir 26:C491–C498
Itoh T, Suzuki H, Kuriyama H (1981) Effects of sodium depletion on contractions evoked in intact and skinned muscles of guinea-pig mesenteric artery. Jpn J Physiol 31:831–847
Kam KE, Stull J (2001) Dedicated myosin light chain kinases with diverse cellular functions. J Biol Chem 276:4527–4530
Karaki H, Weis GB (1981) Inhibitors of mitochondrial Ca2+ uptake dissociate potassium-induced tension responses from increased 45Ca retention in rabbit aortic smooth muscle. Blood Vessels 18:28–35
Karaki H, Ozaki H, Hori M, Misui-Saito M, Amano K-I, Harada K-I, Miayamoto S, Nakazawa H, Won K-J, Sato K (1997) Calcium movements, distribution, and functions in smooth muscle. Pharmacol Rev 49:157–230
Kargacin G, Fay FS (1987) Physiological and structural properties of saponin-skinned single smooth muscle cells. J Gen Physiol 90:49–73
Khoyi MA, Ishikawa T, Keef KD, Westfall DP (1996) Ca2+ induced inhibition of 45Ca2+ influx and Ca2+ current in smooth muscle of the rat vas deferens. Am J Physiol 270:C1468–C1477
Kojima Y, Tsunoda Y, Owyang C (1997) Adenosine 3′, 5′-cyclic monophosphate-stimulated Ca2+ efflux and acetylcoline release in ileal myenteric plexus are mediated by N-type Ca2+ channels: inhibition by the kappa opioid receptor agonist. J Pharmacol Exp Ther 282:403–409
Kravtsov GM, Kwan CY (1995) Regulation of vascular contraction by ionic matrix surfaces of smooth muscle cells: changes in SHR? Clin Exp Pharmacol Physiol [Suppl] 1:S237–S239
Kravtsov GM, Kwan CY (1995) A revisitation of the mechanism of action of KCl-induced vascular smooth muscle contraction: a key role of cation binding to the plasma membrane. Biol Signals 4:160–167
Kravtsov GM, Kwan CY (1996) Protein kinase plays no role in KCl-induced vascular contraction in Ca2+-free medium. Acta Pharmacol Sin 17:197–201
Kuo C-C, Hess P (1993) Block of the L-type Ca2+ channel pore by external and internal Mg2+ in rat phaechromocytoma cells. J Physiol (Lond) 466:683–706
Martell AE, Smith RM (1974) Critical stability constants, vol 1. Plenum Press, New York
Martell AE, Smith RM (1977) Critical stability constants, vol 3. Plenum Press, New York
Mita M, Yanagihara H, Hishiinuma S, Saito M and Walsh MP (2002) Membrane depolarization-induced contraction of rat caudal arterial smooth muscle involves Rho-associated kinase. Biochem J 364:431–440
Mori M, Tsushima H (2000) Activation of Rho signaling contributes to lysophosphatic acid-induced contraction of intact ileal smooth muscle of guinea-pig. Can J Physiol Pharmacol 78:729–736
Movsesian MA, Swain AL, Adelstein RS (1984) Inhibition of turkey gizzard myosin light chain kinase activity by dihydropyridine calcium antagonists. Biochem Pharmacol 35:3759–3764
Nagumo H, Sasaki Y, Ono Y, Okamoto H, Seto M, Takuwa Y (2000) Rho kinase inhibitor HA-1077 prevents Rho-mediated myosin phosphatase inhibition in smooth muscle cells. Am J Physiol 278:C57–C65
Nakamura M, Sunagawa M, Kosugi T, Serekalis N (2000) Actin filaments disruption inhibits L-type Ca2+ channels current in cultured vascular muscle cells. Am J Physiol 279:C480–C487
Okada Y, Yanagisawa T, Taira N (1992) KCl-depolarization potentiates the Ca2+ sensitization by endothelin-1 in canine coronary artery. Jpn J Pharmacol 60:403–405
Peterson BZ, Catterall WA (1995) Calcium binding in the pore of L-type calcium channels modulates high affinity dihydropyridine binding. J Biol Chem 270:18201–18204
Pritchard K, Ashley CC (1987) Evidence for Na+/Ca2+ exchange in isolated smooth muscle cells: a fura-2 study. Pflugers Arch 410:401–407
Reig JA, Viniegra S, Ballesta JJ, Palmero M, Guitierrez LM (1993) Naphthalenesulfonamide derivatives ML9 and W7 inhibit catecholamine secretion in intact and permeabilized chromaffin cells. Neurochem Res 18:317–323
Sato K, Hori M, Ozaki H, Takano-Ohmuro H, Tsuchiya T, Sugi H, Karaki H (1992) Myosin phosphorylation-independent contraction induced by phorbol ester in vascular smooth muscle. J Pharmacol Exp Ther 261:497–505
Satoh M, Ishikawa T, Matsushima S, Naka, M, Hidaka H (1987) Selective inhibition of catalytic activity of smooth muscle myosin light chain kinase. J Biol Chem 262:7796–7801
Somlyo AP, Somlyo AV (2000) Signal transduction by G-proteins, rho-kinase and protein phosphatase to smooth muscle and non-muscle myosin II. J Physiol (Lond) 522:177–185
Tang C-M, Presser F, Morad M (1989) Amiloride selectively blocks the low threshold (T) calcium channel. Science 240:213–215
Triggle CR, Triggle DJ (1975) An analysis of the action of cations of the lanthanide series on the mechanical responses of guinea-pig ileal longitudinal muscle. J Physiol (Lond) 254:39–54
Ueno H (1985) Calcium mobilization in enzymically isolated single intact and skinned muscle cells of the porcine coronary artery. J Physiol (Lond) 363:103–117
Van Bremeen C, Wuytack F, Casteels R (1975) Stimulation of45Ca efflux from smooth muscle cells by metabolic inhibition and high K depolarization. Pflugers Arch 359:183–196
Acknowledgements
We thank Dr. F. Mo (The University of Hong Kong) for help in developing the fluorescent method for evaluation of [Ca2+]i in the rat aorta.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kravtsov, G.M., Bruce, I.C., Wong, T.M. et al. A new view of K+-induced contraction in rat aorta: the role of Ca2+ binding. Pflugers Arch - Eur J Physiol 446, 529–540 (2003). https://doi.org/10.1007/s00424-003-1096-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-003-1096-x