Abstract
Purpose
The da Vinci surgical robot system was developed to overcome the weaknesses of endoscopic surgery. However, whether robotic surgery is superior to endoscopic surgery remains uncertain. Therefore, the purpose of this study was to compare the surgical and oncologic outcomes between endoscopic and robotic thyroidectomy using bilateral axillo-breast approach (BABA).
Methods
Between January 2008 and June 2015, papillary thyroid carcinoma patients who underwent thyroidectomy with central neck dissection using endoscopic (n = 480) or robotic (n = 705) BABA were primarily reviewed. We performed 1:1 propensity score matching and 289 matched pairs were yielded.
Results
Operation time was significantly longer in the robotic thyroidectomy than in the endoscopic thyroidectomy (184.9 vs. 128.9 min, P < 0.001). A significantly higher number of central lymph nodes (CLNs) were resected in the robotic thyroidectomy than in the endoscopic thyroidectomy (5.3 vs. 4.4, P = 0.003). However, the incidence of other outcomes including hospital stay, postoperative duration, thyroglobulin level, radioactive iodine ablation, hemorrhage, chyle leakage, wound infection, recurrent laryngeal nerve injury, and loco-regional recurrence did not significantly differ between the endoscopic thyroidectomy and the robotic thyroidectomy.
Conclusions
Endoscopic thyroidectomy is comparable with robotic thyroidectomy in view of surgical complications and LRR. Because robotic thyroidectomy resected a larger number of CLNs than did endoscopic thyroidectomy, further long-term follow-up studies will be required to clarify the possible prognostic benefits of robotic thyroidectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among the various endoscopic methods, endoscopic thyroidectomy using a bilateral axillo-breast approach (BABA) offers an optimal symmetric surgical view of important anatomical landmarks, including recurrent laryngeal nerves (RLNs), thyroidal vessels, parathyroid glands, and the trachea. Additionally, the cosmetic results of BABA procedures are excellent, with no long axillary or anterior chest scars [1]. Based on these findings, we began employing endoscopic thyroidectomy with BABA in 2008.
Although the endoscopic approach has improved cosmetic outcomes, there are several limitations, including the disability to obtain adequate surgical viewing angles, precisely manipulate endoscopic instruments, and meticulously dissect thyroid tissues, due to its accompanying two-dimensional visual representation and non-flexible endoscopic instruments [2–4]. Because the previous studies have suggested benefits of robotic thyroidectomy [5], such as improved dexterity and visualization [6, 7], we adopted the use of the da Vinci surgical robot system (Intuitive Surgical, Sunnyvale, CA, USA) to overcome the weaknesses of endoscopic thyroidectomy [8].
Nonetheless, the benefits of robotic thyroidectomy in terms of learning curve, cost-effectiveness, and oncologic outcomes still remain controversial [9]. Most of the previous studies comparing endoscopic thyroidectomy and robotic thyroidectomy have been based on a transaxillary approach [6, 7, 10–14]. Only one previous study compared endoscopic thyroidectomy with robotic thyroidectomy based on BABA [15]. Furthermore, no study has investigated prognostic impact, such as the rate of loco-regional recurrence (LRR), between endoscopic thyroidectomy and robotic thyroidectomy in papillary thyroid carcinoma (PTC) patients.
The purpose of this study was to compare the surgical and oncologic outcomes between endoscopic thyroidectomy and robotic thyroidectomy using BABA. Previous comparison studies were performed using only simple univariate analyses [6, 7, 10–15]. However, we used propensity score matching to compare both oncologic and surgical outcomes under a matched condition.
Patients and methods
Patient selection
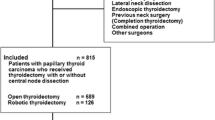
Between January 2008 and June 2015, a total of 2030 patients who underwent thyroidectomy with or without central neck dissection (CND) using endoscopic or robotic BABA at the Thyroid Cancer Center of Samsung Medical Center were primarily reviewed (Fig. 1). A total of 845 patients were excluded based on the following criteria: age less than 18 years, benign diseases, non-PTC carcinomas, PTC combined with other histologic type of thyroid cancers, presence of distant metastasis, cases of no CND, cases of lateral neck dissection, or follow-up duration less than 6 months (including residual tumor or suspicious lymph node [LN] detected within 6 months after initial surgery, reoperation within 6 months of the initial surgery, or loss to follow-up within 6 months). Ultimately, 1185 PTC patients were included for analysis.
Surgical strategy
Following the American Thyroid Association guidelines [16], total thyroidectomy was performed when the primary tumor size was >1 cm, and when multifocality, bilaterality, extrathyroidal extension (ETE), or regional LN metastasis was detected during the preoperative or intraoperative examination. Therapeutic CND was performed when suspicious lymphadenopathy was detected during the preoperative or intraoperative examination. Prophylactic CND was performed on PTC patients with clinically uninvolved central neck, in particular, for advanced primary tumors (T3/T4) [16] or according to the surgeon’s preference at the time of the operation. In our institutions, a total of three surgeons (JH Choe, JH Kim, and JS Kim) have performed endoscopic or robotic thyroidectomy, and we used the same surgical procedures as described in our previous study [15].
Surgical outcomes
We defined “transient” as a symptom duration lasting less than 6 months after initial surgery, and “permanent” as a symptom duration lasting six or more months after initial surgery [7, 13]. RLN injuries, described as vocal cord palsy (VCP), were determined using medical records and/or laryngoscopy. Hypoparathyroidism was defined as a serum parathyroid hormone (PTH) level less than 5 pg/ml at any point during the follow-up period [17, 18]. Hypoparathyroidism was assessed only in total thyroidectomy cases. Hemorrhage, chyle leakage, and wound infection were defined as cases that were confirmed by reoperation. Total drainage was defined as the cumulative amount of drainage.
Postoperative follow-up and management
After the initial surgery, all patients underwent regular follow-up at 6–12 month intervals. Clinical evaluations included physical examinations, ultrasonography (US), iodine-131 scans, and serum thyroglobulin (Tg) tests. Losses to follow-up, withdrawals, and deaths were censored as of the last date of follow-up. LRR was defined as presence of tumor or metastatic LN on cytology from aspiration biopsy or on histopathology from reoperation, which were developed at least 6 months after the initial surgery. Although radioactive iodine (RAI) ablation was generally proposed for aggressive features, as recommended by American Thyroid Association guidelines [16], the final decision was at the discretion of the physician or patient.
Statistical analysis
Statistical analysis was performed using SPSS version 22.0 software (Chicago, IL, USA), and statistically significant differences were defined as those with P values less than 0.05. To reduce the possibility of selection bias and the impact of confounders, we stringently adjusted the clinicopathological characteristics of enrolled PTC patients (sex, age, Asia-Pacific body mass index [BMI] consensus [19], extent of thyroidectomy, laterality of CND, tumor size, multifocality, and ETE) using 1:1 propensity score matching [20]. Although we presented TNM stage in Table 1, we did not use TNM stage as a matching variable due to following reasons. First of all, we initially excluded PTC patients with distant metastasis. Secondly, the components of T-stage (tumor size and ETE) were used as matching variables. Thirdly, retrieved CLN was used as an outcome variable in this study to compare the efficacy of robotic and endoscopic BABA. The use of methods that account for the matched nature of the sample is recommended after propensity score matching [21]. Accordingly, when estimating statistical significance, unpaired methods (Student’s t test for continuous variables and Chi-square test for categorical variables) were used before propensity score matching, while paired methods (Paired t test for continuous variables and McNemar’s test for categorical variables) were used after propensity score matching. Kaplan-Meier methods and the log-rank test were adopted for analysis of time-dependent variables.
Results
Clinicopathological characteristics of PTC patients according to the type of surgical approach (Table 1)
Of the 1185 PTC patients, 480 (40.5 %) underwent endoscopic thyroidectomy and 705 (59.5 %) underwent robotic thyroidectomy. Robotic thyroidectomy was significantly associated with male gender (P < 0.001), bilateral CND (P < 0.001), large tumor size (P < 0.001), and advanced N-stage (P = 0.001). Propensity score matching was performed on 1185 PTC patients, and 289 matched pairs were yielded. After propensity score matching between endoscopic and robotic thyroidectomy, there was no significant difference in the clinicopathological characteristics.
Surgical outcomes of 578 propensity score-matched PTC patients according to the type of surgical approach (Table 2)
Total operation time was significantly longer in the robotic thyroidectomy than in the endoscopic thyroidectomy (184.9 vs. 128.9 min, P < 0.001). Particularly, the mean docking time in the robotic thyroidectomy was 16.5 min. Significantly, more CLNs were resected in the robotic thyroidectomy than in the endoscopic thyroidectomy (5.3 vs. 4.4, P = 0.003). However, other outcomes were not significantly different between the two groups.
Prognostic impact of the type of surgical approach among PTC patients (Fig. 2)
The median follow-up time was 57.1 months (range, 6.0–98.5) and the endoscopic thyroidectomy had a significantly longer follow-up time than the robotic thyroidectomy (60.8 vs. 53.2 months, P < 0.001). LRR was observed in nine patients (1.6 %): four (1.4 %) in the endoscopic thyroidectomy and five (1.7 %) in the robotic thyroidectomy. As shown in Fig. 2, the 5-year recurrence-free survival (RFS) rates were 98.5 % in the endoscopic thyroidectomy and 98.0 % in the robotic thyroidectomy, which were not significantly different (P = 0.777).
Discussion
The purpose of this study was to compare the surgical and oncologic outcomes between endoscopic thyroidectomy and robotic thyroidectomy using BABA. In this study, we used propensity score matching to adjust baseline characteristics of PTC patients. Therefore, oncologic and surgical outcomes were compared under a matched condition. To the best of our knowledge, this study is the first to compare LRR between endoscopic thyroidectomy and robotic thyroidectomy.
As shown in Table 1, before propensity score matching, robotic thyroidectomy was significantly associated with aggressive characteristics, such as large-sized tumors. This finding is consistent with results reported in previous studies [6, 10, 12]. Male patients more frequently underwent robotic thyroidectomy than endoscopic thyroidectomy, which might be attributable to the fact that men have more prominent skeletomuscular structures that can pose greater technical challenges than do those of women. Furthermore, more extensive surgery (bilateral CND) was performed in the robotic thyroidectomy. This result might be explained by the belief of surgeons that robotic thyroidectomy has relative technical advantages over endoscopic thyroidectomy [6].
Technical advantages of robotic thyroidectomy were as follows: (1) a robotic system provides a three-dimensional view and can magnify the visualization of target structures; (2) a surgeon can easily achieve an optimal view and access deep and narrow spaces; (3) steady vision is provided by a robotic arm, which can reduce surgeon’s fatigue and filter out vibrations caused by hand tremors of the surgeon; and (4) a surgeon can use three arms during the operation, with the snake-like motion of the Maryland dissector and the availability of multi-jointed Prograsp forceps. However, in an endoscopic system, a surgeon is limited in the ability to manipulate non-articulated arms; (5) a robotic system is entirely controlled by the operator, which reduces the possibility of problems caused by inexperienced assistants that commonly occur during endoscopic thyroidectomy.
There was no significant difference in surgical complications between endoscopic and robotic thyroidectomy (Table 2), which is in line with the findings of a recently conducted meta-analysis [22]. Stimulated Tg levels and the proportion of stimulated Tg < 1.0 ng/ml could reflect surgical completeness in thyroidectomy [23]. In our study, mean stimulated Tg levels and the proportion of stimulated Tg < 1.0 ng/ml were not different between endoscopic and robotic thyroidectomy. However, as we and others have found [11, 13, 14], the total operation time was significantly longer in the robotic thyroidectomy than in the endoscopic thyroidectomy (184.9 vs. 128.9 min, P < 0.001), which could be explained by several factors: (1) a robotic system generally requires docking time; (2) although the motion of the robot arm is more delicate than that of a human arm, the robotic system does not allow the surgeon to experience tactile sensation; and (3) changing instruments, which requires repetitive connection to and disconnection from the robot arm, is a time-consuming procedure compared to endoscopic thyroidectomy in which instruments are directly gripped by a human hand.
Robotic thyroidectomy resected a significantly higher number of CLNs than endoscopic thyroidectomy (Table 2), and this result has also been found in other studies [6, 7, 10, 12]. This suggests that, given the same conditions, robotic thyroidectomy may perform more radical operations than endoscopic thyroidectomy. However, because a lot of recently conducted studies have opposed the necessity of prophylactic CND in cN0 PTC patients [24–28], this significant difference in the number of resected CLNs may be meaningful regarding PTC patients who will undergo therapeutic CND. Moreover, as shown in Fig. 2, there was no significant difference in LRR between robotic and endoscopic thyroidectomy. In our study, the follow-up period (range, 6.0–98.5 months) might have been too short to identify significant differences in prognostic impact of LN retrieval. Therefore, based on the above results, we may suggest two conclusions: (1) endoscopic thyroidectomy can be as good as robot thyroidectomy; or (2) robotic thyroidectomy may be beneficial to cN1a PTC patients who will need therapeutic CND (Fig. 3). To clarify the differences between endoscopic and robotic thyroid thyroidectomy, further long-term follow-up studies regarding advanced cases such as cN1a PTC will be required.
The mean numbers of resected CLNs were 5.3 in the robotic thyroidectomy and 4.4 in the endoscopic thyroidectomy (Table 2). A previous study based on open thyroidectomy suggested that at least five resected CLNs may be preferable for determining the quality of unilateral CND [29]. Since almost enrolled patients underwent unilateral CND (91.7 %) (Table 1), the number of resected CLNs in our study might be acceptable. Moreover, the number of resected CLNs in our study was comparable and/or superior to that of previous similar studies comparing endoscopic and robotic thyroidectomy [6, 7, 10, 12, 15, 18].
One limitation of robotic thyroidectomy compared with endoscopic thyroidectomy is cost. As shown in Table 1, operation cost was nearly three times higher in the robotic thyroidectomy than in the endoscopic thyroidectomy. Particularly in Korea, since most cancer patients are reimbursed by private medical insurance systems, the cost of robotic thyroidectomy is generally more expensive than that of endoscopic thyroidectomy. Moreover, evaluation of the requirements of robotic systems should include the large physical space needed to house the equipment, and the requisite high costs (operating room charges, anesthesia fees, consumables, equipment depreciation, and maintenance) [30].
Our study has several limitations. First, there are inevitable inherent features of a non-randomized retrospective cohort study. Therefore, the patient information in our data might not be complete and we cannot rule out the possibility of residual confounding variables of some measured or unmeasured factors. Second, most of the enrolled patients have small-sized tumor (Table 1) because we have generally recommended endoscopic or robotic thyroidectomy for early stage patients rather than advanced stage patients. Therefore, further studies using advanced stage patients will be required. Third, we did not routinely perform pre-/postoperative laryngoscopy. Therefore, despite the detailed chart review involved in this study, the incidence of transient VCP might be underestimated. However, all permanent VCP cases were confirmed by laryngoscopy. Fourth, the follow-up period (range, 6.0–85.9 months) in this study might have been too short to identify statistically significant differences in LRR. Fifth, there were few male patients in our analysis. Female patients tend to choose oncoplastic (endoscopic or robotic) techniques, i.e., those leaving no visible scar in the neck, more commonly than do male patients [23, 31–33]. Therefore, as seen in the results of this and other studies [7, 10, 13, 18], few male cases could be included in the study regarding endoscopic or robotic thyroidectomy. Sixth, although radioactive iodine (RAI) ablation was generally proposed for aggressive features, as recommended by American Thyroid Association guidelines [16], the final decision was at the discretion of the physician or patient. Therefore, there was a possible selection bias regarding RAI therapy. Finally, since we have managed patients following 2009 American Thyroid Association guidelines [16], there were some differences in the surgical strategies between the 2015 revised American Thyroid Association guidelines [34] and our study. Nonetheless, this is the first study to compare the prognostic impact of endoscopic and robotic thyroidectomy. Furthermore, since all comparisons, including surgical morbidities and oncologic outcomes, were conducted under a rigorously matched condition, our findings might have greater weight than those of other studies.
Conclusion
Endoscopic thyroidectomy is comparable with robotic thyroidectomy in view of surgical complications and LRR. Despite its longer operation time and higher operation cost, robotic thyroidectomy resected a larger number of CLNs than did endoscopic thyroidectomy. Therefore, further long-term follow-up studies will be required to clarify the prognostic benefits of robotic thyroidectomy, particularly for the treatment of advanced thyroid cancer such as cN1a PTC.
References
Choe JH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK (2007) Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 31(3):601–606. doi:10.1007/s00268-006-0481-y
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S (2002) Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc 16(12):1741–1745. doi:10.1007/s00464-002-8830-x
Slotema ET, Sebag F, Henry J (2008) What is the evidence for endoscopic thyroidectomy in the management of benign thyroid disease? World J Surg 32(7):1325–1332
Lewis CM, Chung WY, Holsinger FC (2010) Feasibility and surgical approach of transaxillary robotic thyroidectomy without CO(2) insufflation. Head Neck 32(1):121–126. doi:10.1002/hed.21318
Chung WY (2012) Pros of robotic transaxillary thyroid surgery: its impact on cancer control and surgical quality. Thyroid: official journal of the American Thyroid Association 22(10):986–987. doi:10.1089/thy.2012.2210.com1
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2011) Excellence in robotic thyroid surgery: a comparative study of robot-assisted versus conventional endoscopic thyroidectomy in papillary thyroid microcarcinoma patients. Ann Surg 253(6):1060–1066. doi:10.1097/SLA.0b013e3182138b54
Lee J, Lee JH, Nah KY, Soh EY, Chung WY (2011) Comparison of endoscopic and robotic thyroidectomy. Ann Surg Oncol 18(5):1439–1446. doi:10.1245/s10434-010-1486-1
Kang SW, Jeong JJ, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Robot-assisted endoscopic surgery for thyroid cancer: experience with the first 100 patients. Surg Endosc 23(11):2399–2406. doi:10.1007/s00464-009-0366-x
Patel D, Kebebew E (2012) Pros and cons of robotic transaxillary thyroidectomy. Thyroid Off J Am Thyroid Association 22(10):984–985. doi:10.1089/thy.2012.2210.ed
Lee J, Yun JH, Choi UJ, Kang SW, Jeong JJ, Chung WY (2012) Robotic versus endoscopic thyroidectomy for thyroid cancers: a multi-institutional analysis of early postoperative outcomes and surgical learning curves. J Oncol:734541. doi:10.1155/2012/734541
Yoo H, Chae BJ, Park HS, Kim KH, Kim SH, Song BJ, Jung SS, Bae JS (2012) Comparison of surgical outcomes between endoscopic and robotic thyroidectomy. J Surg Oncol 105(7):705–708
Tae K, Ji YB, Jeong JH, Kim KR, Choi WH, Ahn YH (2013) Comparative study of robotic versus endoscopic thyroidectomy by a gasless unilateral axillo-breast or axillary approach. Head Neck 35(4):477–484. doi:10.1002/hed.22989
Lang BH, Chow MP (2011) A comparison of surgical outcomes between endoscopic and robotically assisted thyroidectomy: the authors’ initial experience. Surg Endosc 25(5):1617–1623. doi:10.1007/s00464-010-1450-y
Kiriakopoulos A, Linos D (2012) Gasless transaxillary robotic versus endoscopic thyroidectomy: exploring the frontiers of scarless thyroidectomy through a preliminary comparison study. Surg Endosc 26(10):2797–2801. doi:10.1007/s00464-012-2281-9
Kim WW, Kim JS, Hur SM, Kim SH, Lee SK, Choi JH, Kim S, Lee JE, Kim JH, Nam SJ, Yang JH, Choe JH (2011) Is robotic surgery superior to endoscopic and open surgeries in thyroid cancer? World J Surg 35(4):779–784. doi:10.1007/s00268-011-0960-7
Thyroid Association Guidelines Taskforce on Thyroid Nodules Differentiated Thyroid Cancer, Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid: official journal of the American Thyroid Association 19(11):1167–1214. doi:10.1089/thy.2009.0110
Lee KE, Kim E, Koo do H, Choi JY, Kim KH, Youn YK (2013) Robotic thyroidectomy by bilateral axillo-breast approach: review of 1, 026 cases and surgical completeness. Surg Endosc 27(8):2955–2962. doi:10.1007/s00464-013-2863-1
Yoo H, Chae BJ, Park HS, Kim KH, Kim SH, Song BJ, Jung SS, Bae JS (2012) Comparison of surgical outcomes between endoscopic and robotic thyroidectomy. J Surg Oncol 105(7):705–708. doi:10.1002/jso.22106
Bassett J, Organization WH (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Sydney
D'Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17(19):2265–2281
Austin PC (2011) Comparing paired vs non-paired statistical methods of analyses when making inferences about absolute risk reductions in propensity-score matched samples. Stat Med 30(11):1292–1301. doi:10.1002/sim.4200
Jackson NR, Yao L, Tufano RP, Kandil EH (2014) Safety of robotic thyroidectomy approaches: meta-analysis and systematic review. Head Neck 36(1):137–143. doi:10.1002/hed.23223
Lee KE, Koo do H, Im HJ, Park SK, Choi JY, Paeng JC, Chung JK, Oh SK, Youn YK (2011) Surgical completeness of bilateral axillo-breast approach robotic thyroidectomy: comparison with conventional open thyroidectomy after propensity score matching. Surgery 150 (6):1266–1274. doi:10.1016/j.surg.2011.09.015
Zetoune T, Keutgen X, Buitrago D, Aldailami H, Shao H, Mazumdar M, Fahey TJ 3rd, Zarnegar R (2010) Prophylactic central neck dissection and local recurrence in papillary thyroid cancer: a meta-analysis. Ann Surg Oncol 17(12):3287–3293. doi:10.1245/s10434-010-1137-6
Zuniga S, Sanabria A (2009) Prophylactic central neck dissection in stage N0 papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 135(11):1087–1091. doi:10.1001/archoto.2009.163
Costa S, Giugliano G, Santoro L, Ywata De Carvalho A, Massaro MA, Gibelli B, De Fiori E, Grosso E, Ansarin M, Calabrese L (2009) Role of prophylactic central neck dissection in cN0 papillary thyroid cancer. Acta Otorhinolaryngol Ital 29(2):61–69
Ywata de Carvalho A, Chulam TC, Kowalski LP (2015) Long-term results of observation vs prophylactic selective level VI neck dissection for papillary thyroid carcinoma at a cancer center. JAMA Otolaryngol Head Neck Surg. doi:10.1001/jamaoto.2015.0786
Kim SK, Woo J-W, Lee JH, Park I, Choe J-H, Kim J-H, Kim JS (2016) Prophylactic central neck dissection may not be necessary in papillary thyroid carcinoma: analysis of 11,569 cases from a single institution. J Am Coll Surg 222(5):853–864
Hartl DM, Leboulleux S, Al Ghuzlan A, Baudin E, Chami L, Schlumberger M, Travagli JP (2012) Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg 255(4):777–783. doi:10.1097/SLA.0b013e31824b7b68
Cabot JC, Lee CR, Brunaud L, Kleiman DA, Chung WY, Fahey TJ 3rd, Zarnegar R (2012) Robotic and endoscopic transaxillary thyroidectomies may be cost prohibitive when compared to standard cervical thyroidectomy: a cost analysis. Surgery 152(6):1016–1024. doi:10.1016/j.surg.2012.08.029
Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS (2009) Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in papillary thyroid microcarcinoma (PTMC) patients. J Surg Oncol 100(6):477–480. doi:10.1002/jso.21367
Lee S, Ryu HR, Park JH, Kim KH, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS (2012) Early surgical outcomes comparison between robotic and conventional open thyroid surgery for papillary thyroid microcarcinoma. Surgery 151(5):724–730. doi:10.1016/j.surg.2011.12.013
Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK (2007) Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 31(12):2302–2306. doi:10.1007/s00268-007-9117-0discussion 2307-2308
Haugen BRM, Alexander EK, Bible KC, Doherty G, Mandel SJ, Nikiforov YE, Pacini F, Randolph G, Sawka A, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward D, Tuttle RMM, Wartofsky L (2015) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc. doi:10.1089/thy.2015.0020
Author’s contributions
Authorship K.S. K, J.S. K, and J.H. C participated in study conception and design, acquisition of the research data, analysis and interpretation of data, and writing of the manuscript; J.W. W, J.H. L, I. P, J.H. C, and J.H. K participated in study conception and design, analysis and interpretation of data, and critical revision of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding support
There were no relevant financial relationships or any sources of support in the form of grants, equipment, or drugs.
Disclosure statement
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Kim, S.K., Woo, JW., Park, I. et al. Propensity score-matched analysis of robotic versus endoscopic bilateral axillo-breast approach (BABA) thyroidectomy in papillary thyroid carcinoma. Langenbecks Arch Surg 402, 243–250 (2017). https://doi.org/10.1007/s00423-016-1528-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1528-7