Abstract
Introduction
Fibrin sealants and topical hemostatic agents have been used extensively in hepatobiliary and pancreatic (HPB) surgery to promote coagulation and clot formation decreasing the need for allogeneic blood transfusion and to act as tissue sealants, ideally preventing biliary, enteric, and pancreatic leaks.
Results
Current literature has demonstrated some favorable outcomes using many different products for application in the field of HPB surgery. However, critical findings exist demonstrating lack of reproducible efficacy or benefit. In all, many clinical trials have demonstrated effectiveness of fibrin sealants and other agents at reducing the need for intraoperative and postoperative blood transfusion. Ability to effectively seal tissues providing biliostatic effect or preventing postoperative fistula formation remains debated as definitive evidence is lacking.
Conclusions
In the following invited review, we discuss current literature describing the use of topical agents and fibrin sealants in liver and pancreas surgery. We summarize major contemporary clinical trials and their findings regarding the use of these agents in HPB surgery and provide evidence from the preclinical literature as to the translation of these products into the clinical arena.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbidity and mortality in hepatobiliary and pancreas (HPB) surgery have increasingly improved over the past two decades, particularly in high volume centers [1]. Better operative techniques, including the widespread application of minimally invasive HPB surgery, enhanced critical care in the postoperative period, and new technologically advanced materials designed to aid and improve hemostasis both in and out of the operating room continue to change this field. Specific challenges associated with HPB surgery include both intraoperative and postoperative include bleeding from raw liver and pancreas resection surfaces, bile leak, and pancreatic duct leak leading to pancreatic fistula [2]. An increasing application of topical agents and fibrin sealants for use in HPB surgery have been previously described and requires critical appraisal of the literature pertaining to these agents and their efficacy in this unique operative setting [3, 4, 2].
In the following invited review article, we discuss the use of topical hemostatic agents and fibrin sealants in hepatobiliary and pancreas surgery. We describe agents currently available on the market and the current body of literature describing the use of these products in the HPB surgery field. We include evidence from the preclinical literature regarding the efficacy of these products and their translation to the clinical application.
Types of fibrin sealants and topical agents
Fibrin sealants and topical hemostatic agents have been shown to be effective for many different applications. While primarily helping to control perioperative blood loss, they may also control blood loss in areas that are difficult to suture or provide support for sutures in friable, bleeding tissues [5, 6]. Additional evidence supports the use of these agents for sealing cut surfaces preventing tissue leaks and as an adjunct to promote wound healing [7, 8]. In a Cochrane-based meta-analysis of the use of fibrin sealants across many different surgical subspecialties, 18 different trials have found a significant reduction in allogenic blood transfusion with the use of fibrin sealants [9].
Available types of fibrin sealants and topical hemostatic agents have evolved through the years to complex drug delivery systems and varying application systems (Table 1). Most commercially available fibrin sealants contain two components: human fibrinogen and human- or bovine-derived thrombin. The mixture of the two components forms a cross-linked insoluble fibrin clot at the site of application [10]. Some products include the addition of an anti-fibrinolytic agent such as aprotinin or tranexamic acid to prevent enzymatic degradation of the clot formed or special filtration techniques to reduce plasminogen concentration [10]. Newer formulations include carrier-bound fibrin sealants, which have provided new application methods for effective hemostasis. These methods provide drug delivery systems often in the form of a patch or solid application material to cover large surface areas. TachoSil is one such product and consists of an equine collagen fleece patch carrying human fibrinogen and thrombin [11].
Other topical hemostatic agents contain different biological and synthetic materials used alone or in combination to promote intraoperative hemostasis (Table 2). Oxidized cellulose-based products (Surgicel, Fibrillar etc.) have been on the market in the USA for over 40 years and are commonly used for intraoperative hemostatic control. This was followed by a series of bovine collage and porcine-derived gelatin-based products introduced in the 1980s and 1990s. Newer formulations of hemostatic agents are derived from polyethylene glycol, cyanoacrylate, or polysaccharides. Thrombin is also available in human-derived, bovine, and recombinant forms for direct application in the setting of diffuse oozing or bleeding [12]. When combined with bovine- or porcine-derived gelatin (FloSeal, Surgiflo, Costasis), the flowable matrix-based application can be used in both laparoscopic and open surgery to provide hemostatic control. We have found that many of these topical hemostatic agents provide better intraoperative blood loss control for active bleeding as compared to topical fibrin sealants that may be better in situations in which minimal oozing is observed.
Properties of fibrin sealant agents may allow for enhanced tissue adhesion and lead to better tissue sealing and potentially decreased postoperative leakage of bile or pancreatic fluid. Properties of many other hemostatic agents serve for just that purpose, providing hemostasis quickly and effectively with decreased ability for tissue sealant or adhesive effect. Choice of topical agent to be used intra-operatively should be based upon the desired effect and the unique operative situation.
Liver preclinical
To evaluate effectiveness of hemostatic agents in animal models of liver surgery, several trials have demonstrated effectiveness of topical-based fibrinogen thrombin and collagen applications in promoting hemostasis [13]. Animal models have demonstrated the effectiveness of a fibrinogen/thrombin patch in achieving hemostasis in the setting of blunt liver injury and severe coagulopathy [14]. Preclinical models have also been used to study effectiveness of bile duct sealing using liquid fibrin sealant or fibrin collagen patch with increased pressure in the common bile duct [15]. In this series, fibrin collagen patch resisted significantly higher intraductal pressures prior to evidence of bile leakage as compared to liquid fibrin sealant [15].
Liver clinical
Current attitudes regarding the use of fibrin sealants for hemostasis in liver surgery have demonstrated an increasing trend towards the use of these products by HPB surgeons for hemorrhage control. In a study published in 2013, UK hepatobiliary specialists were surveyed and asked to comment on their use of hemostatic agents during liver resection; of the respondents, 62 % routinely used these products and 33 % used them occasionally [16]. Those surveyed also felt manufactured hemostatic agents played a major role in achieving hemostasis (64 %), with preference given to fibrin-based products by 27 % of survey respondents [16]. Likely, most surgeons find these products safe and at least somewhat effective, and as long as they are not cost prohibitive and readily available, they will continue to use them in practice. These findings are echoed from a previous study in which Dutch surgeons were surveyed regarding the use of topical hemostatic agents in liver surgery [4]. Similar findings were reported in that 87 % used hemostatic agents after resection of liver parenchyma, 57 % used them routinely, and as many as 45 % of the surveyed Dutch surgeons believed fibrin sealants reduce liver surface-related complications [4].
In a meta-analysis review of the benefits of fibrin sealant after liver resection, Ding and colleagues conclude mixed results, namely, evidence exists from randomized trials that fibrin sealant is superior to other topical hemostatic agents and argon beam coagulation in controlling intraoperative hemorrhage [17]. Ultimately, there was no significant benefit to fibrin sealant use in “reducing amount of drainage, drainage duration, transfusion requirements, bile leakage, rebleeding and mortality” [17]. A similar review of fibrin sealants in liver surgery published in 2012 concludes many of the same findings [18]. Time to achieve hemostasis in liver surgery is reduced when fibrin sealants are applied, but no strong evidence exists that fibrin sealants reduce incidence of bile leakage after liver resection, and this may be due to a lytic effect of bile on the fibrin-induced clot [18]. An additional meta-analysis describes the hemostatic and biliostatic efficacy of fibrin sealants in elective liver surgery and finds that while time to hemostasis may be reduced intra-operatively, this does not translate to improved perioperative outcomes or reduced incidence of postoperative hemorrhage or bile leak with routine use of fibrin sealants [19].
Of the carrier-bound fibrin sealants, collagen sponge delivery systems have been studied extensively for application in liver-related surgery, likely because the large surface area allows for easy, even coverage on raw cut surfaces. In a randomized prospective trial comparing TachoSil® to argon beam coagulation for hemostasis during liver resection, TachoSil® was found to significantly reduce time to hemostasis [11]. As compared to oxidized cellulose matrix Surgicel®, TachoSil® was not associated with reduced overall complication rate in liver surgery, but when patients were stratified into those undergoing major hepatic resection as compared to minor hepatic resection, a reduction was seen in overall complications and liver surgery specific complications as compared to Surgicel®[20]. TachoSil has also been found to be associated with reduction of postoperative bile leak following elective liver resection and liver trauma [21].
Some of the current literature would argue against the use of fibrin sealants in liver surgery as providing no significant efficacious benefit. The largest series comparing the use of fibrin sealant (Tissucol®) and a collagen sponge applied to the raw liver surface edge as compared to no application was reported [22]. This series found no differences in postoperative outcomes specifically including transfusion rates, drainage volumes, or evidence of biliary fistula [22]. In 2012, a randomized controlled trial was performed in 310 non-cirrhotic patients who underwent liver resection; prophylactic fibrin sealant (Crosseal®) was applied to the cut liver surface in half and no sealant in the other group [23]. There was no difference in resection surface-related complications, bile leakage, or CT scan demonstrated fluid collections between the two groups in this study [23]. However, in findings published in 2004 in which Crosseal® was administered by spray application to liver cut surface following resection, there was a significantly reduced time to achieve hemostasis [24]. So perhaps the argument can be made in favor of fibrin sealants and their ability to achieve immediate intraoperative hemostasis with some reservation on postoperative primary complications from liver-related surgery.
Specifically focusing on incidence and prevention of bile leakage after liver resection, Kobayahsi and colleagues reported a low incidence of bile leak after liver resection from cut surface (raw liver edges) when applying a polyglycolic acid felt to cover raw liver defects [25]. This was compared to raw liver surface edges covered with a conventional fibrin-coated collagen fleece [25]. In the Italian literature, retrospective analysis of 610 liver resections reported that application of fibrin glue significantly reduced postoperative bile leakage and more so found it was an independently associated protective factor for the prevention of postoperative bile leak [26]. A review article describing the use of hemostatic agents specifically for prevention of biliary leakage was published by Erdogan and colleagues [27]. They include description of a French multicenter randomized series, in which they found lower postoperative drain fluid amounts and lower concentration of bilirubin present in the fluid when fibrin glue was applied to cut surface edges, but did not show overall lower leakage rates or intra-abdominal fluid collections with fibrin sealant application [28]. Similar to the Kobayashi trial, Hayashibe and colleagues were able to significantly drop rates of bile leakage from cut resection surfaces when fibrin glue was combined with a bioabsorbable polyglycolic acid sheet to the cut resection surface [29].
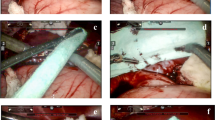
The increasing use of laparoscopic techniques for HPB surgery has also encouraged the use of laparoscopic application of fibrin sealants and hemostatic agents. This may be due to the fact that technical success in laparoscopic liver surgery requires careful intraoperative control of bleeding to avoid obscuring visualization. Even small amounts of unmanaged bleeding may provide a cause for conversion to open surgery, so topical hemostatic agents may provide a direct role in successful laparoscopic liver surgery [30]. As a result of this trend towards minimally invasive surgery, many companies have adapted applicator devices or changed product design to ease application of hemostatic agents via minimally invasive techniques. Of the published literature, a non-inferiority study regarding the use of polyglycolic acid felt in laparoscopic liver surgery was not associated with any significant differences as compared to the group identified before fibrin sealant use [31]. Despite this, we believe the predominant trend towards minimally invasive surgery will likely continue to afford adaptations in products designed to control hemostasis via minimally invasive application.
Pancreas clinical
Fibrin sealants and topical agents have gained an increasing use following pancreatectomy procedures for intraoperative hemostasis control but more so, for the prevention of postoperative pancreatic fistula (POPF). Rates of pancreatic fistula formation remain highly variable based upon the procedure type, method of pancreatic transection, and institutional clinical volume. By and large, accepted postoperative pancreatic fistula rates range between 5 and 30 % [32], and vary in severity from chemically detected but requiring no intervention, to pancreatic leaks with severe clinical sequelae requiring intervention as defined by the ISGPF guidelines [33]. Efforts to improve pancreatic fistula rates have focused on many different operative technique modifications and the increasing use of applied fibrin glue and topical sealants for prevention of postoperative pancreatic fistula. One example of a technical modification combines the use of a vascular pedicle round ligament flap from the anterior abdominal wall to reinforce the pancreaticoenteric anastomosis in pancreaticoduodenectomy or at the stump of the pancreas following distal pancreatectomy with fibrin glue sealant [34]. From our own experience, this technique yields low rates of POPF, 8.8 % following pancreaticoduodenectomy and 5.3 % for all pancreas resection procedures [34].
From the preclinical literature, investigation was undertaken to determine the effects of biocompatibility and adhesive properties of six commercially available tissue adhesives, three cyanoacrylate derivatives, two human fibrin sealants, and one albumin glutaraldehyde [35]. While satisfactory adhesive properties were observed in animal models of pancreaticoenteric anastomosis in four of six studied tissue adhesives, all tissue adhesives studied induced histologic changes in the pancreas, which were interpreted as being potentially harmful to the pancreas [35].
In a review series of 14 articles describing the use of fibrin sealants for reduction of pancreatic fistula after distal pancreatectomy, Wilson and colleagues conclude “that the application of fibrin glue to the pancreatic stump could help to reduce the incidence of troublesome pancreatic fistulas” [10]. The largest prospective randomized controlled trial reviewed in this series was from Suzuki et al. and found a significantly lower pancreatic fistula rate after application of TISSEEL fibrin sealant (p = 0.04) [36]. Three other prospective randomized controlled trials found no significant difference in postoperative pancreatic fistula rates when fibrin sealants were applied after distal pancreatectomy [37–39] (Table 3).
A second review series published in 2014 included pooled data from 7 randomized controlled trials and 897 patients [40]. In this review, a trend was seen towards the reduction of postoperative hemorrhage and intra-abdominal fluid collection in those patients who received fibrin sealants; however, there was no significant difference in rates of POPF [40]. Fingerhut and colleagues conclude similar findings from their review of 24 studies including 6 randomized controlled trials of fibrin sealants in pancreatic surgery [39]. Of three trials which the authors assigned a level of evidence of 2 based upon good experimental trial design with randomization from the Cook definition [41], only the Suzuki trial found a reduction in POPF rates with application of fibrin sealant [36]; studies by D’Andrea and Lillemoe found no significant difference in rates of POPF with application of fibrin glue [37, 42]. Similar small case series and prospective randomized trials have also failed to demonstrate improvement in POPF rates following the application of the glutaraldehyde-based BioGlue, carrier-based fibrin patch TachoSil, fibrin glue plus falciform ligament patch, or fibrin sealant TISSEEL to pancreaticoenteric anastomoses and cut pancreatic surface margins [43–46].
Multiple small case series have been reported, however, in which the application of fibrin sealants or combination type sealants have demonstrated improved rates of postoperative pancreatic fistula following technique modification with fibrin-based sealant. Ochiai et al. describe the reduction of POPF following the application of polyethylene glycolic acid felt with fibrin glue to pancreaticojejunostomy site following pancreaticoduodenectomy and the cut stump following distal pancreatectomy [47]. Conaglen and Collier report a series of 30 patients in which none developed POPF following the application of fibrin glue to pancreaticogastrostomy anastomosis [48]. Another additional series reports successful reduction of POPF rates with application of carrier-bound fibrin adhesive to distal pancreatectomy cut surfaces [49]. Ultimately, the use of fibrin-based products or tissue sealants in pancreatic surgery likely remains a choice for surgeons based on clinical experience and individual clinical outcomes. Similar to the literature published regarding the application of fibrin sealants in liver surgery, hemostatic efficacy has been established in the realm of pancreatic surgery, but overall effectiveness in regard to tissue sealing and prevention of POPF remains debated.
Conclusions
The increasing complexity of hepatobiliary and pancreas surgery will likely continue to drive the development of biomaterials to improve outcomes and reduce both postoperative morbidity and mortality rates. Particularly with the push of minimally invasive surgical techniques gaining new ground in the realm of HPB surgery, fibrin sealants and topical agents will, in all likelihood, continue to have a place in the ease of achieving hemostasis in the operating room and potentially preventing postoperative complications. While some of the data for these agents demonstrates no significant difference to the non-use of these products and good surgical techniques, many surgeons remain comfortable with their application, and for all intents and purposes will continue to use these agents as an adjunct in their surgical practice. The effective evaluation of these products and their applicability in the realm of HPB surgery requires careful clinical trial design and thoughtful evaluation of the literature as to their effectiveness. Ultimately, in a time of exploding healthcare expenditure, the conscientious surgeon will take effectiveness, ease of use, and overall benefit to the patient when considering fibrin sealants and other topical agents in HPB surgery practice.
References
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236(4):397–406. doi:10.1097/01.SLA.0000029003.66466.B3, discussion 406-397
Simo KA, Hanna EM, Imagawa DK, Iannitti DA (2012) Hemostatic agents in hepatobiliary and pancreas surgery: a review of the literature and critical evaluation of a novel carrier-bound fibrin sealant (TachoSil). ISRN Surg 2012:729086. doi:10.5402/2012/729086
Kraus TW, Mehrabi A, Schemmer P, Kashfi A, Berberat P, Buchler MW (2005) Scientific evidence for application of topical hemostats, tissue glues, and sealants in hepatobiliary surgery. J Am Coll Surg 200(3):418–427. doi:10.1016/j.jamcollsurg.2004.09.047
Boonstra EA, Molenaar IQ, Porte RJ, de Boer MT (2009) Topical haemostatic agents in liver surgery: do we need them? HPB (Oxford) 11(4):306–310. doi:10.1111/j.1477-2574.2009.00065.x
Spotnitz WD, Burks S (2008) Hemostats, sealants, and adhesives: components of the surgical toolbox. Transfusion 48(7):1502–1516. doi:10.1111/j.1537-2995.2008.01703.x
Berrevoet F, de Hemptinne B (2007) Use of topical hemostatic agents during liver resection. Dig Surg 24(4):288–293. doi:10.1159/000103660
Briceno J, Naranjo A, Ciria R, Diaz-Nieto R, Sanchez-Hidalgo JM, Luque A, Rufian S, Lopez-Cillero P (2010) A prospective study of the efficacy of clinical application of a new carrier-bound fibrin sealant after liver resection. Arch Surg 145(5):482–488. doi:10.1001/archsurg.2010.62
Sarpel U, Roayaie S, Schwartz ME, Labow DM (2007) The role of fibrin sealants in hepatic surgery. Surg Technol Int 16:31–36
Carless PA, Henry DA, Anthony DM (2003) Fibrin sealant use for minimising peri-operative allogeneic blood transfusion. Cochrane Database Syst Rev 2, CD004171. doi:10.1002/14651858.cd004171
Wilson C, Robinson S, French J, White S (2014) Strategies to reduce pancreatic stump complications after open or laparoscopic distal pancreatectomy. Surg Laparosc Endosc Percutan Tech 24(2):109–117. doi:10.1097/SLE.0b013e3182a2f07a
Frilling A, Stavrou GA, Mischinger HJ, de Hemptinne B, Rokkjaer M, Klempnauer J, Thorne A, Gloor B, Beckebaum S, Ghaffar MF, Broelsch CE (2005) Effectiveness of a new carrier-bound fibrin sealant versus argon beamer as haemostatic agent during liver resection: a randomised prospective trial. Langenbecks Arch Surg 390(2):114–120. doi:10.1007/s00423-005-0543-x
Cheng CM, Meyer-Massetti C, Kayser SR (2009) A review of three stand-alone topical thrombins for surgical hemostasis. Clin Ther 31(1):32–41. doi:10.1016/j.clinthera.2009.01.005
Schelling G, Block T, Gokel M, Blanke E, Hammer C, Brendel W (1988) Application of a fibrinogen-thrombin-collagen-based hemostyptic agent in experimental injuries of liver and spleen. J Trauma 28(4):472–475
Grottke O, Braunschweig T, Daheim N, Coburn M, Grieb G, Rossaint R, Tolba R (2010) Effect of TachoSil in a coagulopathic pig model with blunt liver injuries. J Surg Res. doi:10.1016/j.jss.2010.02.002
Erdogan D, de Graaf W, van Gulik TM (2008) Adhesive strength of fibrinogen-coated collagen patch or liquid fibrin sealant in an experimental liver resection model in pigs. Eur Surg Res 41(3):298–302. doi:10.1159/000155879
Lochan R, Ansari I, Coates R, Robinson SM, White SA (2013) Methods of haemostasis during liver resection—a UK national survey. Dig Surg 30(4–6):375–382. doi:10.1159/000354036
Ding H, Yuan JQ, Zhou JH, Zheng XY, Ye P, Mao C, Chen Q (2013) Systematic review and meta-analysis of application of fibrin sealant after liver resection. Curr Med Res Opin 29(4):387–394. doi:10.1185/03007995.2013.768216
de Boer MT, Boonstra EA, Lisman T, Porte RJ (2012) Role of fibrin sealants in liver surgery. Dig Surg 29(1):54–61. doi:10.1159/000335735
Sanjay P, Watt DG, Wigmore SJ (2013) Systematic review and meta-analysis of haemostatic and biliostatic efficacy of fibrin sealants in elective liver surgery. J Gastrointest Surg 17(4):829–836. doi:10.1007/s11605-012-2055-7
Zacharias T, Ferreira N (2012) Carrier-bound fibrin sealant compared to oxidized cellulose application after liver resection. HPB (Oxford) 14(12):839–847. doi:10.1111/j.1477-2574.2012.00560.x
Frena A, Martin F (2006) How to improve bilio-stasis in liver surgery. Chir Ital 58(6):793–795
Figueras J, Llado L, Miro M, Ramos E, Torras J, Fabregat J, Serrano T (2007) Application of fibrin glue sealant after hepatectomy does not seem justified: results of a randomized study in 300 patients. Ann Surg 245(4):536–542. doi:10.1097/01.sla.0000245846.37046.57
de Boer MT, Klaase JM, Verhoef C, van Dam RM, van Gulik TM, Molenaar IQ, Bosscha K, Dejong CH, Van der Jagt EJ, Porte RJ (2012) Fibrin sealant for prevention of resection surface-related complications after liver resection: a randomized controlled trial. Ann Surg 256(2):229–234. doi:10.1097/SLA.0b013e3182602819
Schwartz M, Madariaga J, Hirose R, Shaver TR, Sher L, Chari R, Colonna JO 2nd, Heaton N, Mirza D, Adams R, Rees M, Lloyd D (2004) Comparison of a new fibrin sealant with standard topical hemostatic agents. Arch Surg 139(11):1148–1154. doi:10.1001/archsurg.139.11.1148
Kobayashi S, Nagano H, Marubashi S, Wada H, Eguchi H, Takeda Y, Tanemura M, Doki Y, Mori M (2012) Fibrin sealant with PGA felt for prevention of bile leakage after liver resection. Hepatogastroenterology 59(120):2564–2568. doi:10.5754/hge10315
Capussotti L, Ferrero A, Vigano L, Sgotto E, Muratore A, Polastri R (2006) Bile leakage and liver resection: where is the risk? Arch Surg 141(7):690–694. doi:10.1001/archsurg.141.7.690, discussion 695
Erdogan D, Busch OR, Gouma DJ, van Gulik TM (2007) Prevention of biliary leakage after partial liver resection using topical hemostatic agents. Dig Surg 24(4):294–299. doi:10.1159/000103661
Noun R, Elias D, Balladur P, Bismuth H, Parc R, Lasser P, Belghiti J (1996) Fibrin glue effectiveness and tolerance after elective liver resection: a randomized trial. Hepatogastroenterology 43(7):221–224
Hayashibe A, Sakamoto K, Shinbo M, Makimoto S, Nakamoto T (2006) New method for prevention of bile leakage after hepatic resection. J Surg Oncol 94(1):57–60. doi:10.1002/jso.20548
Saif R, Jacob M, Robinson S, Amer A, Kei-Hui D, Sen G, Manas D, White S (2011) Use of fibrin-based sealants and gelatin-matrix hemostats in laparoscopic liver surgery. Surg Laparosc Endosc Percutan Tech 21(3):131–141. doi:10.1097/SLE.0b013e31821db688
Kobayashi S, Nagano H, Marubashi S, Wada H, Eguchi H, Tanemura M, Sekimoto M, Umeshita K, Doki Y, Mori M (2011) Experience with the use of fibrin sealant plus polyglycolic acid felt at the cut surface of the liver in laparoscopic hepatectomy. Surg Endosc 25(11):3590–3596. doi:10.1007/s00464-011-1764-4
Hackert T, Werner J, Buchler MW (2011) Postoperative pancreatic fistula. Surgeon 9(4):211–217. doi:10.1016/j.surge.2010.10.011
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13. doi:10.1016/j.surg.2005.05.001
Iannitti DA, Coburn NG, Somberg J, Ryder BA, Monchik J, Cioffi WG (2006) Use of the round ligament of the liver to decrease pancreatic fistulas: a novel technique. J Am Coll Surg 203(6):857–864. doi:10.1016/j.jamcollsurg.2006.08.021
Lamsa T, Jin HT, Sand J, Nordback I (2008) Tissue adhesives and the pancreas: biocompatibility and adhesive properties of 6 preparations. Pancreas 36(3):261–266. doi:10.1097/MPA.0b013e31816714a2
Suzuki Y, Kuroda Y, Morita A, Fujino Y, Tanioka Y, Kawamura T, Saitoh Y (1995) Fibrin glue sealing for the prevention of pancreatic fistulas following distal pancreatectomy. Arch Surg 130(9):952–955
D’Andrea AA, Costantino V, Sperti C, Pedrazzoli S (1994) Human fibrin sealant in pancreatic surgery: it is useful in preventing fistulas? A prospective randomized study. Italian J Gastroenterol 26(6):283–286
Suc B, Msika S, Fingerhut A, Fourtanier G, Hay JM, Holmieres F, Sastre B, Fagniez PL (2003) Temporary fibrin glue occlusion of the main pancreatic duct in the prevention of intra-abdominal complications after pancreatic resection: prospective randomized trial. Ann Surg 237(1):57–65. doi:10.1097/01.sla.0000041259.01594.33
Fingerhut A, Veyrie N, Ata T, Alexakis N, Leandros E (2009) Use of sealants in pancreatic surgery: critical appraisal of the literature. Dig Surg 26(1):7–14. doi:10.1159/000191284
Orci LA, Oldani G, Berney T, Andres A, Mentha G, Morel P, Toso C (2014) Systematic review and meta-analysis of fibrin sealants for patients undergoing pancreatic resection. HPB (Oxford) 16(1):3–11. doi:10.1111/hpb.12064
Cook DJ, Guyatt GH, Laupacis A, Sackett DL (1992) Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 102(4 Suppl):305S–311S
Lillemoe KD, Cameron JL, Kim MP, Campbell KA, Sauter PK, Coleman JA, Yeo CJ (2004) Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg 8(7):766–772. doi:10.1016/j.gassur.2004.06.011, discussion 772-764
Fisher WE, Chai C, Hodges SE, Wu MF, Hilsenbeck SG, Brunicardi FC (2008) Effect of BioGlue on the incidence of pancreatic fistula following pancreas resection. J Gastrointest Surg 12(5):882–890. doi:10.1007/s11605-008-0479-x
Montorsi M, Zerbi A, Bassi C, Capussotti L, Coppola R, Sacchi M (2012) Efficacy of an absorbable fibrin sealant patch (TachoSil) after distal pancreatectomy: a multicenter, randomized, controlled trial. Ann Surg 256(5):853–859. doi:10.1097/SLA.0b013e318272dec0, discussion 859-860
Carter TI, Fong ZV, Hyslop T, Lavu H, Tan WP, Hardacre J, Sauter PK, Kennedy EP, Yeo CJ, Rosato EL (2013) A dual-institution randomized controlled trial of remnant closure after distal pancreatectomy: does the addition of a falciform patch and fibrin glue improve outcomes? J Gastrointest Surg 17(1):102–109. doi:10.1007/s11605-012-1963-x
Martin I, Au K (2013) Does fibrin glue sealant decrease the rate of anastomotic leak after a pancreaticoduodenectomy? Results of a prospective randomized trial. HPB (Oxford) 15(8):561–566. doi:10.1111/hpb.12018
Ochiai T, Sonoyama T, Soga K, Inoue K, Ikoma H, Shiozaki A, Kuriu Y, Kubota T, Nakanishi M, Kikuchi S, Ichikawa D, Fujiwara H, Sakakura C, Okamoto K, Kokuba Y, Otsuji E (2010) Application of polyethylene glycolic acid felt with fibrin sealant to prevent postoperative pancreatic fistula in pancreatic surgery. J Gastrointest Surg 14(5):884–890. doi:10.1007/s11605-009-1149-3
Conaglen PJ, Collier NA (2014) Augmenting pancreatic anastomosis during whipple operation with fibrin glue: a beneficial technical modification? ANZ J Surg 84(4):266–269. doi:10.1111/ans.12072
Mita K, Ito H, Fukumoto M, Murabayashi R, Koizumi K, Hayashi T, Kikuchi H, Kagaya T (2011) A fibrin adhesive sealing method for the prevention of pancreatic fistula following distal pancreatectomy. Hepatogastroenterology 58(106):604–608
Ollinger R, Mihaljevic AL, Schuhmacher C, Bektas H, Vondran F, Kleine M, Sainz-Barriga M, Weiss S, Knebel P, Pratschke J, Troisi RI (2013) A multicentre, randomized clinical trial comparing the Veriset haemostatic patch with fibrin sealant for the management of bleeding during hepatic surgery. HPB (Oxford) 15(7):548–558. doi:10.1111/hpb.12009
Liu M, Lui WY (1993) The use of fibrin adhesive for hemostasis after liver resection. Zhonghua Yi Xue Za Zhi (Taipei) 51(1):19–22
Toti L, Attia M, Manzia TM, Lenci I, Gunson B, Buckels JA, Mirza DF, Mayer AD, Bramhall SR, Wigmore SJ (2010) Reduction in bile leaks following adult split liver transplant using a fibrin-collagen sponge: a pilot study. Dig Liver Dis 42(3):205–209. doi:10.1016/j.dld.2009.06.010
Chapman WC, Clavien PA, Fung J, Khanna A, Bonham A (2000) Effective control of hepatic bleeding with a novel collagen-based composite combined with autologous plasma: results of a randomized controlled trial. Arch Surg 135(10):1200–1204, discussion 1205
Satoi S, Toyokawa H, Yanagimoto H, Yamamoto T, Hirooka S, Yui R, Yamaki S, Matsui Y, Mergental H, Kwon AH (2011) Reinforcement of pancreaticojejunostomy using polyglycolic acid mesh and fibrin glue sealant. Pancreas 40(1):16–20. doi:10.1097/MPA.0b013e3181f82f55
Mita K, Ito H, Fukumoto M, Murabayashi R, Koizumi K, Hayashi T, Kikuchi H (2011) Pancreaticojejunostomy using a fibrin adhesive sealant (TachoComb) for the prevention of pancreatic fistula after pancreaticoduodenectomy. Hepatogastroenterology 58(105):187–191
Marczell AP, Stierer M (1992) Partial pancreaticoduodenectomy (Whipple procedure) for pancreatic malignancy: occlusion of a non-anastomosed pancreatic stump with fibrin sealant. HPB Surg 5(4):251–259, discussion 259-260
Kram HB, Clark SR, Ocampo HP, Yamaguchi MA, Shoemaker WC (1991) Fibrin glue sealing of pancreatic injuries, resections, and anastomoses. Am J Surg 161(4):479–481, discussion 482
Nanashima A, Tobinaga S, Kunizaki M, Nonaka T, Takeshita H, Hidaka S, Sawai T, Nagayasu T (2012) Does fibrin glue prevent biliary and pancreatic fistula after surgical resection? Hepatogastroenterology 59(117):1544–1547. doi:10.5754/hge10079
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hanna, E.M., Martinie, J.B., Swan, R.Z. et al. Fibrin sealants and topical agents in hepatobiliary and pancreatic surgery: a critical appraisal. Langenbecks Arch Surg 399, 825–835 (2014). https://doi.org/10.1007/s00423-014-1215-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1215-5