Abstract
Backgrounds
Concomitant intact parathyroid hormone (iPTH) and serum calcium measurement is deemed to be useful in predicting hypocalcemia after total thyroidectomy. This study aimed to prospectively assess the diagnostic accuracy of combined iPTH and serum calcium measurement in predicting early postoperative hypocalcemia.
Methods
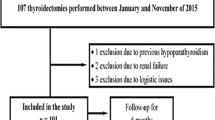
From January 2010 to January 2011, 112 patients underwent total thyroidectomy in our department. A prospective study was carried out to search for factors predicting postoperative hypocalcemia. Serum calcium, phosphorus, and iPTH levels have been measured before operation and at 6, 24, and 48 h postoperatively. Hypocalcemia was defined as a serum calcium level less than 8.0 mg/dL. Sensitivity and specificity of different serum measurements have been calculated using the receiver–operator characteristics curve.
Results
Thirty-three patients (29.5 %) had transient postoperative hypocalcemia. Serum iPTH level showed the highest sensitivity and specificity in predicting hypocalcemia after 6 h (84.8 % and 93.7 %, respectively) for a criterion value ≤12.1 pg/mL. Serum calcium level showed the highest sensitivity and specificity after 24 h (93.9 and 100.0 %, respectively) for a criterion value ≤7.97 mg/dL. Combined cutoffs of 6-h iPTH and 24-h serum calcium showed sensitivity and specificity of 100.0 %.
Conclusions
The combined measurement of 6-h iPTH and 24-h serum calcium are highly predictive of early postoperative hypocalcemia. Patients with serum iPTH and calcium level ≤ criterion value are at major risk for developing hypocalcemia. These results are important in selecting patients eligible for early discharge and those patients who need calcium and vitamin D supplementation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transient postoperative hypocalcemia is the most common complication after thyroid surgery, occurring in up to 50–68 % of patients [1, 2]. The nadir of hypocalcemia usually occurs within 48 h after thyroidectomy [3, 4]. It is usual practice to monitor patients after thyroidectomy for signs and symptoms of hypocalcemia as well as for regular measurements of serum calcium and phosphorus levels [4, 5]. The routine use of a laboratory test that could identify hypocalcemia-prone patients and/or those patients at low risk to develop hypocalcemia could be beneficial. The availability of such test could allow correct calcium and vitamin D supplementation and an early and safe discharge. The search for early risk factors predicting hypocalcemia has focused the interest on the postoperative monitoring of intact parathyroid hormone (iPTH) because of its short half-life ranging from 2 to 5 min [6, 7]. Recently, concomitant iPTH and serum calcium measurement has been considered to be useful in predicting early hypocalcemia after total thyroidectomy (TT) [3, 8, 9].
The current study aimed to prospectively assess the diagnostic accuracy of combined iPTH and serum calcium measurement in predicting early postoperative hypocalcemia and to define the most appropriate postoperative clinical pathway of patients following TT. Sensitivity, specificity, and predictive power of different postoperative serum measurements of iPTH, calcium, and phosphorus have been calculated to identify the point cutoff of minimal false-negative and false-positive results in predicting hypocalcemia.
Patients and methods
From January 2010 to January 2011, a case cohort of 112 consecutive patients (93 women and 19 men) underwent TT in our Surgical Department for a variety of thyroid disorders. These patients were enrolled in a prospective nonrandomized longitudinal study focusing on the search for those parameters predicting early postoperative hypocalcemia. Approval for this study was obtained from the Institutional Review Board of our Hospital (Ethics Committee of the Azienda Ospedaliera Universitaria of Cagliari, Italy) and written informed consent was obtained from each patient. To be enrolled in the study, patients had to meet the following inclusion criteria: undergo TT over the considered period regardless of thyroid pathology and sign a written informed consent. The exclusion criteria from the study were: undergo thyroid lobo-isthmectomy, undergo surgery for recurrent goiter, concomitant hyperparathyroidism from parathyroid adenoma or carcinoma, and concomitant treatment with oral calcium and/or vitamin D before operation. Patients submitted to central or modified radical neck dissection were not excluded from the study.
Five patients were excluded from the study because of: thyroid lobo-isthmectomy in one case, completion thyroidectomy in one case, concomitant parathyroid adenoma in one case, concomitant parathyroid carcinoma in one case, and supplementation treatment with oral calcium and vitamin D for severe osteoporosis in one case.
The current investigation aimed to assess the diagnostic accuracy of iPTH and serum calcium measurement in predicting early postoperative hypocalcemia. For this purpose, we carried out a cross-sectional study stratifying patients into two groups as normocalcemic and hypocalcemic according to their serum calcium measurements within 48 h postoperatively. All the medical records were prospectively analyzed and the comparison between groups involved evaluation of demographic data (age and sex), diagnostic results, indication for surgery, patient management, symptoms and signs of hypocalcemia, pathological diagnosis, and postoperative and follow-up results. During thyroidectomy, the main surgeon objective was to identify and dissect parathyroid glands and to maintain their blood supply. Superior parathyroid glands have been carefully dissected to preserve the origin of their blood supply from the inferior or from the superior thyroid artery. The individual branches of the arteries have been ligated distal to the given branches for superior parathyroid glands. Inferior parathyroid glands were clearly identified and preserved when orthotopic. The close association with the superior tongue of the thymus or with the remnant thymus tissue has been the landmark in the case of an ectopic inferior gland. When at least three parathyroid glands were identified, we did not perform excessive dissection to avoid any damage to potential vascularization of the remaining gland, commonly the left inferior one. In our practice, parathyroid glands are usually autotransplanted in the ipsilateral sternocleidomastoid muscle if the arterial pedicle is affected. Conversely, a decompressing incision is made on the parathyroid capsule when the gland shows signs of a venous infarction.
Hypocalcemia was defined as serum total calcium level less than 8.0 mg/dL (normal range 8.8–10.6 mg/dL) at one or more measurements, with or without clinical symptoms. Symptoms and signs of hypocalcemia are uncommon for serum calcium levels above this cutoff. Thus, the value of 8.0 mg/dL has been commonly used to define hypocalcemia after thyroidectomy in the published studies, although this figure is lower than the range of reference [4, 10].
Following the study protocol, concomitant serum calcium, phosphorus, and iPTH levels were measured before operation and at 6, 24, and 48 h after TT. All the blood samples were obtained from peripheral venipuncture. Serum iPTH level has been measured by the Siemens Immulite® 2500 Intact PTH and the normal range for this assay used at our institution is between 12 and 65 pg/mL. This assay uses a solid-phase two-site enzymatic chemiluminometric approach. In our laboratory, the normal low limit for iPTH is 12 pg/mL, while the low limit of detection is 3 pg/mL. Serum concentrations of calcium and phosphorus were determined by routine colorimetric assay (Olympus System Reagent®). The reference interval for serum calcium in our laboratory is 8.8–10.6 mg/dL, while the normal phosphorus range is 2.5–4.5 mg/dL.
When patients had a calcium level less than 8.0 mg/dL and developed symptoms of hypocalcemia, they were started on oral calcium supplements (calcium carbonate 2–3 g daily) and/or vitamin D (1,25-dihydroxycholecalciferol 0.25–0.50 μg daily) with dose adjusted to achieve a normal serum calcium level. Intravenous calcium gluconate (10 %) was administered for severe hypocalcemia with clinically significant symptoms. All patients who developed hypocalcemia entered a scheduled follow-up program for at least 6 months from the discharge.
Serum calcium and phosphorus levels were measured weekly during the first month and then on a monthly basis for 5 months. Serum level of iPTH was measured 2 weeks after discharge and then on a monthly basis for 6 months. Vitamin D and oral calcium supplementation was discontinued when iPTH, serum calcium, and phosphorus level reverted to normal. Patients were considered as having permanent hypoparathyroidism if oral calcium and/or vitamin D administration was required 6 months after thyroidectomy, as reported elsewhere [11].
Data collection and statistical analysis
Data were prospectively collected in a planned relational computer database (Microsoft Office Access). Patients’ characteristics, pathological findings, operative and postoperative results as well as all serum measurements were recorded. After data inputting, specific queries were devised and data analyzed. All statistical analyses were carried out using the MedCalc® 2011 statistical software (version 11.5.1). Data for age, postoperative hospital stay, preoperative and postoperative iPTH, and serum calcium and phosphorus levels were presented as the mean ± standard error of the mean (SEM) and as the median value. Data were compared for statistical analysis using the Chi-square test to evaluate differences between qualitative variables, and using the Student’s t test to compare quantitative variables. Data regarding iPTH and calcium slope were evaluated by the analysis of variance for repeated measures (ANOVA). Sensitivity, specificity, and predictive power (positive predictive value: PPV; negative predictive value: NPV) of different serum measurements of iPTH, serum calcium and phosphorus were calculated and summarized using the receiver–operator characteristics (ROC) curve. The area under the curve (AUC) was calculated. The diagnostic accuracy of a test is assessed by the area under ROC curve as follows: 0.90–1.00, excellent; 0.80–0.90, good; 0.70–0.80, fair; 0.60–0.70, poor; and 0.50–0.60, fail [12, 13]. Then, the criterion value was obtained as the point cutoff of minimal false-negative and false-positive results of serum measurements in predicting hypocalcemia. The p values were checked and reported as calculated by the statistical software. Differences were considered significant when p < 0.05.
Results
The prevalence of transient postoperative hypocalcemia was 29.5 % (33 out of 112 patients). Hypocalcemia group included 30 women and 3 men (at a ratio of 15.5:1.0) with a mean age of 53 years (range 16–73 years). Patients with normal postoperative calcemia consisted of 63 women and 16 men (at a ratio of 3.6:1.0) with a mean age of 52.1 years (range 19–80 years). There was no significant difference between groups for age and gender (Table 1).
Cross-sectional study revealed that there was no significant difference between groups for surgical indication and surgical treatment (p > 0.50 by Student’s t test). Among 33 patients with hypocalcemia, 31 had TT because of papillary thyroid carcinoma in 14 cases, follicular thyroid carcinoma in 1 case, follicular thyroid adenoma associated with multinodular goiter in 4 cases, multinodular goiter in 6 cases, toxic multinodular goiter in 2 cases, nodular variant of Hashimoto’s thyroiditis in 2 cases, and Graves’ disease in other 2 cases. One patient had TT and central neck dissection because of papillary thyroid carcinoma with central lymph node metastasis; another patient had TT associated with central and bilateral modified radical neck dissection for a medullary thyroid carcinoma. In the latter patient, an accidentally removed parathyroid gland was found in the surgical specimen of the central neck dissection. In the hypocalcemia group, no patient underwent parathyroid autotransplantation and no parathyroid glands were found into the thyroid parenchyma. A decompressing incision on one parathyroid gland was made in two cases of venous infarction. Overall, four parathyroid glands were identified in 26 patients of this group, and three glands in other 7 patients.
Of 79 patients without hypocalcemia, 76 had TT because of papillary thyroid carcinoma in 25 cases, follicular thyroid carcinoma in 6 cases, follicular thyroid adenoma associated with multinodular goiter in 5 cases, multinodular goiter in 26 cases, toxic multinodular goiter in 5 cases, nodular variant of Hashimoto’s thyroiditis in 6 cases, and Graves’ disease in other 3 cases. One patient had TT associated with central neck dissection and ipsilateral modified radical neck dissection because of papillary thyroid carcinoma with lymph node metastasis; one patient had TT associated with central neck dissection and ipsilateral modified radical neck dissection because of medullary thyroid carcinoma; one patient had TT associated with central neck dissection and bilateral modified radical neck dissection because of medullary thyroid carcinoma.
In the normocalcemia group, no patient underwent parathyroid autotransplantation, no parathyroid glands were found in the surgical specimen and no decompressing incision was made on parathyroid glands. Overall, five parathyroid glands were identified in 1 patient, four glands in 59 patients, and three glands in other 6 patients.
Serum iPTH levels of patients with hypocalcemia had a negative slope from preoperative mean value of 40.81 to 8.07 pg/mL at 6 h after the operation (with a maximum decrease of 80.2 % from the preoperative value); iPTH slope was then positive until a mean iPTH value of 11.15 pg/mL at 48 h. This difference in repeated iPTH measurements of hypocalcemic patients was significant (p = 0.002). On the other hand, serum iPTH level of patients without hypocalcemia had a negative slope from preoperative mean value of 51.24 to 37.38 pg/mL detected at 24 h after the operation (with a maximum decrease of 27.0 % from the preoperative value); iPTH slope was then positive with a mean iPTH value of 44.26 pg/mL at 48 h. This difference in repeated iPTH measurements of normocalcemic patients was not significant (p = 0.103; Fig. 1).
Serum calcium level of patients with hypocalcemia had a negative slope from mean preoperative value of 9.41 to 7.29 mg/dL at 48 h after the operation (with a maximum decrease of 22.5 % from the preoperative value). This difference in repeated serum calcium measurements was significant (p = 0.022). Conversely, serum calcium level of patients without hypocalcemia had a negative slope from mean preoperative value of 9.58 to 8.52 mg/dL at 48 h after the operation (with a maximum decrease of 11.1 % from the preoperative value). The difference in repeated serum calcium measurements of normocalcemic patients was significant (p = 0.035; Fig. 2). However, calcium serum levels were over the cutoff of 8.0 mg/dL, which defined hypocalcemia (p values of Figs. 1 and 2 were calculated by ANOVA)
ROC curve analysis of iPTH 6 h/postoperative hypocalcemia is shown in Table 2. The AUC was calculated as 0.930 with a 95 % confidence interval from 0.865 to 0.969 (p < 0.0001). The criterion value of iPTH with minimal false-negative and false-positive results was calculated as ≤12.1 pg/mL, which was the threshold index score of iPTH with the highest sensitivity and specificity in predicting hypocalcemia (84.8 and 93.7 %, respectively). The PPV and NPV of iPTH level detected after 6 h from the operation were 84.9 and 93.6 %, respectively.
Five patients with hypocalcemia and postoperative iPTH level >12.1 pg/mL represented the false-negative results, whereas four patients without hypocalcemia (serum calcium level >8.0 mg/dL) and postoperative iPTH level <12.1 pg/mL represented the false-positive results (Table 3).
ROC curve results of calcium 24 h/postoperative hypocalcemia are shown in Table 2. The AUC was calculated as 0.969 with a 95 % confidence interval from 0.917 to 0.992 (p < 0.0001). The criterion value of calcemia with minimal false-negative and false-positive results was calculated as ≤7.97 mg/dL, which was the threshold index score of calcemia value with the highest sensitivity and specificity in predicting hypocalcemia (93.9 and 100.0 %, respectively). The PPV and NPV of calcium level detected after 24 h from the operation were 100.0 and 97.5 %, respectively.
Two patients with normal serum calcium level at 24 h after the operation represented the false-negative results because they developed hypocalcemia 48 h after the operation (in both cases iPTH level was 3.0 pg/mL; Table 3).
ROC curve analysis of combined iPTH 6-h calcium 24 h/postoperative hypocalcemia is shown in Table 2. The AUC was calculated as 1.000 with a 95 % confidence interval from 0.967 to 1.000 (p < 0.0000). Thus, the combined iPTH cutoff ≤12.1 pg/dL at 6 h postoperatively (iPTH drop ≥70.5 % of preoperative value), together with the calcium serum cutoff ≤7.97 mg/dL at 24 h postoperatively (serum calcium drop ≥18.5 % of preoperative value) showed the highest sensitivity and specificity in predicting postoperative hypocalcemia (100.0 % for both parameters).
The AUC of phosphorus 6 h/postoperative hypocalcemia was 0.557, while it was 0.725 at 24 h after the operation. Phosphorus measurement at 6 h after the operation failed in predicting hypocalcemia and its diagnostic accuracy was fair at 24 h (Table 2).
Among 33 patients who developed postoperative hypocalcemia, 16 patients (48.5 %) had significant symptoms and they were started on intravenous calcium gluconate (10 %) and then on oral calcium carbonate 3 g daily associated with 1,25-dihydroxycholecalciferol 0.50 μg daily; 10 patients (30.3 %) had mild symptoms and they were started on oral calcium carbonate 2–3 g daily; 7 patients (21.2 %) had no symptoms and oral calcium supplement was not required. These patients experienced no tetany. It is noteworthy that no patient was started on calcium or vitamin D before the blood sample of 24 h after surgery.
The mean postoperative hospital stay was 3.1 days in the normocalcemic group vs. 3.5 days in the hypocalcemic one. As a result of the study, those patients with normal iPTH level at 6 h after operation and normal serum calcium level at 24 h after operation were considered eligible for discharge.
At 6-months follow-up, one patient of the hypocalcemia group died of unrelated disease and 30 patients were normocalcemic and normoparathyrinemic without supplementation. Oral calcium administration was still required in two patients who were considered as having permanent hypoparathyroidism (overall incidence of 1.6 %–2/112).
Following these results, we only check iPTH and serum calcium 6 and 24 h after the operation, respectively. Finally, we recommend the decisional algorithm about postoperative clinical pathway of patients undergoing TT, which is shown in Fig. 3.
Discussion
Postoperative hypocalcemia is the most frequent complication following thyroid surgery, and it is the commonest reason of delay in patients’ discharge after TT [1, 2, 9, 14]. Usually, clinically relevant hypocalcemia can be ascribed to impaired parathyroid function following intraoperative devascularization or accidental removal of parathyroid glands [10, 15]. The risk of postoperative neck hematoma and airway obstruction is considered to be higher within 8 h from surgery [1]. On the other hand, symptoms of hypocalcemia become clinically evident in the first and in the second postoperative day [4, 16, 17]. When the risk of airway obstruction has receded, the need for repeated serum calcium and phosphorus measurement has been the main cause of prolonged hospital stay after TT [8].
Several approaches have been proposed to identify patients eligible for early discharge as well as to achieve early prediction of postoperative hypocalcemia. Some authors suggested routine administration of calcium and vitamin D supplementation to all patients undergoing TT [18–20], while others recommended serial postoperative serum calcium measurements as the standard protocol of care [7, 21]. The use of quick PTH assay during thyroidectomy has also been advocated for predicting postoperative parathyroid function [22, 23]. However, it was clear that waiting several hours after completing surgery improved the predictive capabilities of the PTH assay [3]. The utility of postoperative iPTH measurement for determining which patient will become significantly hypocalcemic after thyroid surgery has gained acceptance among surgeons [5, 24–26]. Recently, concomitant or combined postoperative iPTH and serum calcium measurement are deemed to be better than serum calcium or serum iPTH measurement alone in early prediction of hypocalcemia [3, 8, 9, 27]. Nevertheless, there is no consensus regarding what is considered the gold standard testing of hypocalcemia complicating thyroid surgery. The above considerations justify the search for further predictive factors, which could allow for immediate clinical management decisions to be made.
Following the results of our investigation, combining iPTH measurement 6 h after TT and calcium measurement after 24 h showed the highest sensitivity and specificity in predicting hypocalcemia. The combined iPTH cutoff of 12.1 pg/dL 6 h postoperatively with an iPTH drop ≥70.5 %, together with the calcium serum cutoff of 7.97 mg/dL 24 h postoperatively with a serum calcium drop ≥18.5 %, showed the highest diagnostic accuracy in predicting postoperative hypocalcemia. These results allowed us to identify those patients eligible for early and safe discharge on postoperative day one, and to early start patients on supplementation treatment, thus avoiding or reducing the severity of hypocalcemia symptoms.
Our policy appears to be effective in the clinical decision-making when compared to other postoperative protocols of thyroidectomy patients. Routine administration of calcium and/or vitamin D could overtreat the normocalcemic patient and mask the hypocalcemic one [28]. Monitoring for postoperative calcium slope by repeated calcium measurement is not useful for planning an early discharge, as the nadir of hypocalcemia is not reached until the second postoperative day [4, 17]. The largest prospective study evaluating the utility of postoperative iPTH measurement alone showed that iPTH measured 4 h postoperatively was not accurate enough in predicting clinically relevant postoperative hypocalcemia and in identifying those patients who may be safely discharged early from the hospital [7]. The same study also advocated the integration of iPTH cutoff levels with preoperative and postoperative serum calcium concentrations to improve the overall diagnostic accuracy in predicting hypocalcemia [7]. Indeed, the predictive capabilities of iPTH assay 1 to 6 h after thyroidectomy are improved when early calcium levels are measured as well [3, 14, 29]. In our investigation and in accordance with other authors [28], the 6-h iPTH level was chosen because we believe that it is the optimal time when an early decision about discharge can be made. We also found that testing iPTH 24 to 48 h after TT is unnecessary, as its predictive power is no longer increased. Moreover, in our experience the predictive power of 6-h iPTH measurement reached the highest value with 100.0 % capability of predicting hypocalcemia when 24-h calcium levels were combined as well. In 2005, Payne et al. showed that patients with no other complications could be sent home after the 6-h iPTH and concomitant serum calcium results [9]. However, in our study the 6-h serum calcium level was not sensitive enough as it was at 24 h. More recently, Jumaily et al. in an analysis of pooled individual data from three observational studies showed that testing iPTH 5 to 6 h postoperatively reached the highest predictive capability of postoperative hypocalcemia [3]. Nevertheless, concomitant iPTH and serum calcium measurements were not significantly better than using iPTH measurement alone [3], as the nadir of hypocalcemia usually occurs later [4, 10, 17]. In the series of Asari and coworkers, measuring iPTH level 24 h after TT in combination with serum calcium level on the second postoperative day allowed the highest prediction of postoperative hypocalcemia [8]. The results of our study corroborate the clinical validity of combined measurement of iPTH and serum calcium, but our patients were eligible for safe discharge on postoperative day one rather than on day 2. Reducing hospitalization could improve the overall healthcare system savings with minimal supplementary laboratory expenses, the cost of iPTH and serum calcium measurement in our hospital being 15 and 8 euros, respectively.
Another important goal that could be achieved by an early and safe discharge is the satisfaction of patients, which is an established indicator of quality care [9]. On the other hand, when iPTH and serum calcium levels are unfavorable, both prevention and/or alleviation of symptoms from hypocalcemia could be obtained at an early stage [7, 29].
Currently, we only check iPTH and serum calcium 6 and 24 h after the operation, respectively. The safe management of patients following TT is now based on the decisional algorithm, which is shown in details in Fig. 3. This protocol allows surgeons to discharge normocalcemic and normoparathyrinemic patients early and safely. Hypocalcemic and hypoparathyrinemic patients can be immediately started on supplementation treatment avoiding an unnecessary morbidity. Close monitoring for serum calcium levels and hypocalcemia symptoms are still required for undetermined patients such as hypocalcemic and normoparathyrinemic or normocalcemic and hypoparathyrinemic.
Finally, patients with serum calcium level ≤7.97 mg/dl and iPTH ≤12.1 pg/ml must be considered at major risk for developing hypocalcemia. After retroactively applying the decisional algorithm, 67 % of patients would have been discharged early and safely, while 25 % of patients would have been started early on supplementation treatment. However, the apparent good results of this study need to be validated and reproduced in the clinical routine of a larger number of hospitals. Definitive recommendations cannot be made without verifying the applicability of our guidelines by a larger prospective randomized study, well matching the results of combined iPTH and calcium measurement with those of traditional management of patients undergoing thyroid surgery.
References
Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, Pelizzo MR, Pezzullo L (2004) Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 28:271–276
Wilson RB, Erskine C, Crowe PJ (2000) Hypomagnesemia and hypocalcemia after thyroidectomy: a prospective study. World J Surg 24:722–726
Jumaily JS, Noordzij JP, Dukas AG, Lee SL, Bernet VJ, Payne RJ, McLeod IK, Hier MP, Black MJ, Kerr PD, Raffaelli M, Bellantone CP, Lombardi CP, Dietrich MS (2010) Prediction of hypocalcemia after using 1- to 6-hour postoperative parathyroid hormone and calcium levels: an analysis of pooled individual patient data from 3 observational studies. Head Neck 32:427–434
Grodski S, Campbell P, Cook MJ, Delbridge L, Farrell S, Gough I, Jalaludi B, Magarey C, Palazzo F, Serpell J, Sidhu S, Soon P, Sywak M, Yeh M (2007) Australian endocrine surgeons guidelines AES06/01. Postoperative parathyroid hormone measurement and early discharge after total thyroidectomy: analysis of Australian data and management recommendations. ANZ J Surg 77:199–202
Lombardi CP, Raffaelli M, Princi P, Santini S, Boscherini M, De Crea C, Traini E, D’Amore AM, Carrozza C, Zuppi C, Bellantone R (2004) Early prediction of post thyroidectomy hypocalcemia by one single iPTH measurement. Surgery 136:1236–1241
Alia P, Moreno P, Rigo R, Francos JM, Navarro MA (2007) Post resection parathyroid hormone and parathyroid hormone decline accurately predict hypocalcemia after thyroidectomy. Am J Clin Pathol 127:592–597
Lombardi CP, Raffaelli M, Trinci P, Dobrinja C, Carrozza C, Di Stasio E, D’Amore AM, Zuppi C, Bellantone R (2006) Parathyroid hormone levels 4 hours after surgery do not accurately predict post-thyroidectomy hypocalcemia. Surgery 140:1016–1025
Asari R, Passler C, Kaczirek K, Scheuba C, Niederle B (2008) Hypoparathyroidism after total thyroidectomy: a prospective study. Arch Surg 143:132–137
Payne RJ, Hier MP, Tamilia M, Mac Namara E, Young J, Black MJ (2005) Same-day discharge after total thyroidectomy: the value of 6-hours serum parathyroid hormone and calcium levels. Head Neck 27:1–7
Pattou F, Combemale F, Fabre S, Carnaille B, Decoulx M, Wemeau JL, Racadot A, Proye C (1998) Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg 22:718–724
Pisanu A, Di Chiara B, Reccia I, Uccheddu A (2010) Oncocytic cell tumors of the thyroid: factors predicting malignancy and influencing prognosis, treatment decisions and outcomes. World J Surg 34:836–843
http://www.medcalc.org/manual/roc-curves.php. Accessed 30 March 2012
http://gim.unmc.edu/dxtests/ROC3.htm. Accessed 30 March 2012
McLeod IK, Arciero C, Noordzij JP, Stojadinovic A, Peoples G, Melder PC, Langley R, Bernet V, Shriver CD (2006) The use of rapid parathyroid hormone assay in predicting postoperative hypocalcemia after total or completion thyroidectomy. Thyroid 16:259–265
Pisanu A, Cois A, Piu S, Altana ML, Uccheddu A (2003) Factors predicting outcome of hypocalcemia following total thyroidectomy. Chir Ital 55:35–40
Adams J, Andersen P, Everts E, Cohen J (1998) Early postoperative calcium levels as predictors of hypocalcemia. Laryngoscope 108:1829–1831
Del Rio P, Arcuri MF, Ferreri G, Sommaruga L, Sianesi M (2005) The utility of serum PTH assessment 24 hours after total thyroidectomy. Otolaryngol Head Neck Surg 132:584–586
Sahai A, Symes A, Jeddy T (2005) Short-stay thyroid surgery. Br J Surg 92:58–59
Roh JL, Park CI (2006) Routine oral calcium and vitamin D supplements for prevention of hypocalcemia after total thyroidectomy. Am J Surg 192:675–678
Tartaglia F, Giuliani A, Sgueglia M, Biancari F, Juvonen T, Campana FP (2005) Randomized study on oral administration of calcitriol to prevent symptomatic hypocalcemia after total thyroidectomy. Am J Surg 190:424–429
Husein M, Hier MP, Al-Abdulhadi K, Black M (2002) Predicting calcium status post-thyroidectomy with early calcium levels. Otolaryngol Head Neck Surg 127:289–293
Lo CY, Luk JM, Tam SC (2002) Applicability of intraoperative parathyroid hormone assay during thyroidectomy. Ann Surg 236:564–569
Richards ML, Bingener-Casey J, Pierce D, Strodel WE, Sirinek KR (2003) Intraoperative parathyroid hormone assay: an accurate predictor of symptomatic hypocalcemia following thyroidectomy. Arch Surg 138:632–636
Lam A, Kerr PD (2003) Parathyroid hormone: an early predictor of postthyroidectomy hypocalcemia. Laryngoscope 113:2196–2200
Payne RJ, Hier MP, Tamilia M, Young J, MacNamara E, Black MJ (2003) Postoperative parathyroid hormone level as a predictor of post-thyroidectomy hypocalcemia. J Otolaryngol 32:362–367
Barczynski M, Cichon S, Konturek A (2007) Which criterion of intraoperative iPTH assay is the most accurate in prediction of true serum calcium levels after thyroid surgery? Langenbecks Arch Surg 392:693–698
Lim JP, Irvine R, Bugis S, Holmes D, Wiseman SM (2009) Intact parathyroid hormone measurement 1 hour after thyroid surgery identifies individuals at high risk for the development of symptomatic hypocalcemia. Am J Surg 197:648–654
Fahad Al-Dhahri S, Al-Ghonaim YA, Suleiman Terkawi A (2010) Accuracy of postthyroidectomy parathyroid hormone and corrected calcium levels as early predictors of clinical hypocalcemia. J Otolaryngol Head Neck Surg 39:342–348
Noordzij JP, Lee SL, Bernet VJ, Payne RJ, Cohen SM, McLeod IK, Hier MP, Black MJ, Kerr PD, Richards ML, Lo CY, Raffaelli M, Bellantone R, Lombardi CP, Cohen JI, Dietrich MS (2007) Early prediction of hypocalcemia after thyroidectomy using parathyroid hormone: an analysis of pooled individual patients data from nine observational studies. J Am Coll Surg 205:748–754
Acknowledgments
This study was supported by a grant from the University of Cagliari, Italy (quota ex 60 %).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pisanu, A., Saba, A., Coghe, F. et al. Early prediction of hypocalcemia following total thyroidectomy using combined intact parathyroid hormone and serum calcium measurement. Langenbecks Arch Surg 398, 423–430 (2013). https://doi.org/10.1007/s00423-012-1017-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-1017-6