Abstract
Purpose
Chronic pain following inguinal hernia repair is a complex problem. Mesh fixation with sutures may be a contributing factor to this pain. The aim of this study was to compare the incidence of chronic pain and limitation of activities of daily living following inguinal hernia repair using a sutured mesh to a self-adhesive mesh, 6 months and 1 year following surgery.
Methods
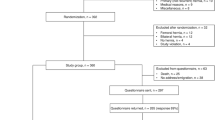
All consecutive patients presenting to NHS Fife for open hernia repair between January 2009 and January 2010 were included in our analysis. A prospective survey of postoperative pain and activities of daily living was conducted at 6 months and 1 year following hernia repair. Chronic pain was assessed using the SF-36 questionnaire. The primary end points for analysis were incidence of chronic pain and limitation of activities of daily living.
Results
Overall, 132 of 215 patients completed the questionnaire, 69 in the sutured group and 63 in the self-adhesive mesh group. The need for analgesics was similar during the first 24 h after surgery. Wound infections were detected in one patient in the Lichtenstein group and two in the second group. The incidence of chronic pain was 21 and 7.9 % at 6 months and 18.8 and 6.3 % at 1 year (p < 0.05). Moderate and vigorous activities were found to be limited some to all of the time in nine patients (60 %) in the suture fixation group and in one patient in the self-adhesive group (20 %, p < 0.02).
Conclusions
Open inguinal hernia repair with a self-adhesive mesh may lead to less chronic pain and less restriction of activities of daily living than a sutured mesh fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lichtenstein hernioplasty is a tension-free open technique for inguinal hernia repair; a polypropylene mesh is used to support the inguinal muscular layer. Chronic pain may occur in 10–30 % of procedures. The pain may be caused by irritation or damage to the inguinal nerves by sutures or mesh [1–3], an inflammatory reaction against the mesh [4] or simply scar tissue [5]. Pain is often reported to be neuropathic in character, related to younger age, and exists during physical activity; it is more often associated with recurrent hernia surgery. The routine use of mesh techniques reduces the risk of hernia recurrence compared with non-mesh methods.
The original technique for fixation of mesh in Lichtenstein hernioplasty used non-absorbable sutures placed medially near the pubic periosteum and the upper corner of the mesh and continuous sutures along the inguinal ligament [6, 7]. Others described using absorbable sutures [8] and various tissue glues [9, 10]. A randomised control trial has described some benefit using a self-fixation mesh [11]. The primary goal of these methods of fixation was to reduce chronic neuropathic pain (and to speed up surgery). The present study aimed to compare the incidence of chronic pain and limitation of activities of daily living following inguinal hernia repair using a sutured mesh to a self-adhesive mesh, 6 months and 1 year following surgery.
Methods
All patients who underwent a unilateral open primary inguinal hernia repair in Fife NHS Trust in Scotland between January 2009 and January 2010 were included in our analysis. The Department of General Surgery comprises of ten surgeons with six surgeons performing all the open hernia repairs. Three surgeons used absorbable sutures for mesh placement. The remaining three used the self-adhesive mesh instead. All operations were performed by a consultant surgeon or by a trainee under direct supervision. Patients with recurrent hernias or those requiring emergency repair were excluded from this study. Patients were identified from a prospective hospital database. The East of Scotland Ethics Committee approved the study 11/GA/136.
Tension-free hernioplasty was performed with a 6 × 11-cm prolene mesh (Ethicon Edinburgh) or ProGrip (Covidien, Germany). Indirect hernia sacs were transfixed at the base and excised. In the sutured fixation repair, a mesh was placed between the conjoint tendon, the inguinal ligament, the pubic tubercle and the internal oblique muscle overlapping the inguinal ligament by approximately 5 mm. The mesh was secured with suture to the pubic tubercle without placing through the periosteum, the inguinal ligament and the conjoint tendon. The mesh was divided beyond the internal ring to accommodate the cord and mesh fixed to the internal oblique muscle. The ilioinguinal, genitofemoral and iliohypogastric nerves were identified and preserved if possible in each case. Care was taken not to include the nerves with the sutures. With sutureless fixation, the Parietene ProGrip (Covidien, Germany) was used. This is a low-density, macroporous polypropylene mesh with resorbable polylactic acid microhooks. Full details are available at www.covidien.com. The self-gripping flap of the mesh is released and loosely closed around the cord away from the deeper part of wound. The mesh is oriented in position, and fixation was achieved by applying pressure on the mesh starting caudally on the pubic bone then medially onto the internal oblique structures. The mesh is fixed under the external oblique aponeurosis. In its final position, the mesh is anchored into the tissue both at the transversalis structures, as well as to the ligament and external oblique aponeurosis. In both repairs, the external oblique aponeurosis and skin were closed with absorbable sutures. The procedures were performed under local, regional or general anaesthesia.
Patients were observed for 60–120 min postoperatively and then discharged from the ambulatory unit with routine instructions. Regular paracetamol and ibuprofen were prescribed for postoperative pain unless contraindicated.
The primary outcome of the study was chronic pain during the first postoperative year. Secondary outcomes included wound complications and recurrences. The International Association for the Study of Pain has defined chronic pain as pain lasting more than 3 months, and this definition was applied to this study [12]. Patients completed a SF-36 pain questionnaire to assess the degree of postoperative pain and interference with activities of daily living. Patients were assessed 6 months and 1 year postoperatively. Follow-up was also provided by telephone interview. The surgical team examined all patients who reported wound haematomas, infections, recurrences or chronic pain. Hernia recurrence was confirmed by ultrasound on helical CT. The postoperative questionnaires were completed by a specialist registrar (AJQ) or specialist nurse (KMW).
Statistical analysis
Statistical analysis was performed using Pearson's chi-squared test using SPSS version 17.0 for Windows (SPSS, Chicago, Illinois, USA).
Results
During the study interval, 215 patients underwent an open hernia repair. One hundred thirty-two patients completed the questionnaire survey, 63 in the self-adhesive group and 69 in the suture fixation group. All patients that completed the questionnaire at 6 months also completed it at 1 year postoperatively. There were no significant differences in patient demographics between the two groups (Table 1). All patients were discharged at the same day of surgery. There were three superficial wound infections requiring a course of antibiotics prescribed by the general practitioner, two in the self-adhesive group and one in the sutured group. No patients required readmission for wound complications or pain management. After 1 year of follow-up, one patient has a confirmed recurrence in the sutured group.
The incidence of pain 6 months and 1 year postoperatively was significantly decreased in the self-adhesive group. At 6 months, 21 % of the patients in the sutured fixation group described pain compared to 7.9 % in the self-fixation group (p < 0.05). A similar trend was observed at 1 year postoperatively with 18.8 % experiencing pain in the suture fixation group and 6.3 % in the self-fixation group. The impact of chronic pain postoperatively on activities of daily living was assessed using the SF-36 questionnaire. Chronic pain was found to affect moderate and vigorous activities some to all of the time in nine patients (60 %) in the suture fixation group. In the self-adhesive group, this was described in one patient (20 %, p < 0.02).
Discussion
The results of this study indicated that the use of the self-adhesive mesh during open hernia repair had similar outcomes in terms of wound infection and recurrence compared with sutured mesh fixation. However, the method of mesh fixation influenced the incidence of chronic postoperative pain with a reduced incidence when using a self-adhesive mesh at 6 months and 1 year following open hernia repair compared to standard repair with sutured mesh fixation.
In the past, the recurrence rate was a major outcome measure in inguinal hernia repair studies. However, with the introduction of alloplastic materials and new surgical techniques, the recurrence rate has dropped substantially with most surgeons achieving a rate of less than 5 % [14–16]. The Lichtenstein procedure is one of the most frequently used open techniques. It is easy to learn and associated with a low complication rate [17].
Consequently, outcome measures have shifted focus to adverse outcomes following inguinal hernia surgery. Chronic pain has emerged as a common and sometimes severe problem that can significantly affect patient health-related quality of life [18]. Postoperative discomfort or pain is classified as chronic pain if it lasts longer than 3 months [18]. In a recent review of the literature, the incidence of chronic pain was reported to range between 25 and 30 % for the majority of studies [19]. Postoperative pain has been shown to persist for over 5 years in 1.8 % of patients, 10 % of inguinal hernia repair patients suffer from severe pain significantly affecting daily activities [20, 21] and as many as 7.5 % of cases may be in more pain than before the operation [22].
The pathogenesis of chronic pain following hernia repair is poorly understood. It is well known that traditional inguinal hernia repairs (Bassini, Shouldice, McVay, etc.) may cause chronic pain owing to tension [23]. Yet, chronic pain is still reported after tension-free hernia repair. Some data supported the hypothesis that nerve handling or division is of importance for pain relief [24, 25]; however, this remains controversial with other studies demonstrating an increased incidence of chronic pain [3, 26, 27]. Others suggest that the use of low-weight and large-pore polypropylene meshes may be favourable in this respect [28]. Entrapment of nerves in fixation sutures has been recognised as a cause of severe pain that may be relieved on release of the entrapped nerve. A further reason for pain may be the surgical damage of the tissue; this includes perhaps the fixation sutures of the mesh.
Methods of mesh fixation in all hernia surgery remain controversial. The incidence of chronic pain has been the primary endpoint of many studies including this one, investigating different methods of mesh fixation. Studies have assessed the use of absorbable versus non-absorbable suture material [8] as well as staples versus suture fixation [29] with no significant differences detected. Reduced short-term morbidity with tissue glue has been demonstrated when fixing lightweight meshes with tissue glue compared to suture fixation; however, these results were not supported in a recent randomised control trials [30, 31]. The ProGrip mesh is a polypropylene self-fixation mesh that uses dissolvable microhooks to anchor itself to the surrounding tissues. Several reports have demonstrated a significant reduction of pain scores using a self-fixation mesh in the immediate postoperative period [11, 32–35]. The reduced incidence of chronic pain when not suture fixing the mesh may be attributed to iatrogenic damage or inclusion of nerves with suture placement; however, it is the authors' belief that the absence of suture fixation allows a true tension-free repair. Despite best efforts, suture fixation will inevitably cause a degree of tension, and it may be that it is this effect that results in the reduced incidence of chronic pain.
A limitation of this study is that three surgeons performed sutured mesh fixation and a further three used the self-adhesive mesh. The observed differences between the groups may be attributed to the differences in operative technique and tissue handling. However, the incidence of chronic pain in the suture fixation group is comparable to that in the published literature therefore suggesting a reduced overall incidence in the self-adhesive group. Evidence to support these findings requires an adequately powered randomised control trial.
In conclusion, the findings presented here support the existing literature suggesting that the use of the self-fixation mesh may reduce the incidence of pain following open inguinal hernia surgery. Furthermore, we provide further data demonstrating a reduced incidence of chronic pain, specifically chronic pain affecting activities of daily living.
References
Heise CP, Starling JR (1998) Mesh inguinodynia: a new clinical syndrome after inguinal herniorrhaphy? J Am Coll Surg 187:514–518
Wijsmuller AR, van Veen RN, Bosch JL, Lange JF, Kleinrensink GJ, Jeekel J (2007) Nerve management during open hernia repair. Br J Surg 94:17–22
Reinpold WM, Nehls J, Eggert A Nerve management and chronic pain after open inguinal hernia repair: a prospective two phase study. Ann Surg 254:163-168
Di Vita G, Milano S, Frazzetta M, Patti R, Palazzolo V, Barbera C, Ferlazzo V, Leo P, Cillari E (2000) Tension-free hernia repair is associated with an increase in inflammatory response markers against the mesh. Am J Surg 180:203–207
Nahabedian MY, Dellon AL (1997) Outcome of the operative management of nerve injuries in the ilioinguinal region. J Am Coll Surg 184:265–268
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Amid PK, Shulman AG, Lichtenstein IL (1996) Open "tension-free" repair of inguinal hernias: the Lichtenstein technique. Eur J Surg 162:447–453
Paajanen H (2002) Do absorbable mesh sutures cause less chronic pain than nonabsorbable sutures after Lichtenstein inguinal herniorraphy? Hernia 6:26–28
Canonico S, Santoriello A, Campitiello F, Fattopace A, Corte AD, Sordelli I, Benevento R (2005) Mesh fixation with human fibrin glue (Tissucol) in open tension-free inguinal hernia repair: a preliminary report. Hernia 9:330–333
Campanelli G, Champault G, Pascual MH, Hoeferlin A, Kingsnorth A, Rosenberg J, Miserez M (2008) Randomized, controlled, blinded trial of Tissucol/Tisseel for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: rationale and study design of the TIMELI trial. Hernia 12:159–165
Kapischke M, Schulze H, Caliebe A Self-fixating mesh for the Lichtenstein procedure—a prestudy. Langenbecks Arch Surg 395:317-322
Anonymous (1986) Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3:S1–226
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–6
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Fellander G, Heikkinen T (2005) One year results of a randomised controlled multi-centre study comparing Prolene and Vypro II-mesh in Lichtenstein hernioplasty. Hernia 9:223–227
Paajanen H (2007) A single-surgeon randomized trial comparing three composite meshes on chronic pain after Lichtenstein hernia repair in local anesthesia. Hernia 11:335–339
Shulman AG, Amid PK, Lichtenstein IL (1992) The safety of mesh repair for primary inguinal hernias: results of 3,019 operations from five diverse surgical sources. Am Surg 58:255–257
van Hanswijck de Jonge P, Lloyd A, Horsfall L, Tan R, O'Dwyer PJ (2008) The measurement of chronic pain and health-related quality of life following inguinal hernia repair: a review of the literature. Hernia 12:561–569
Ferzli GS, Edwards ED, Khoury GE (2007) Chronic pain after inguinal herniorrhaphy. J Am Coll Surg 205:333–341
Staal E, Nienhuijs SW, Keemers-Gels ME, Rosman C, Strobbe LJ (2008) The impact of pain on daily activities following open mesh inguinal hernia repair. Hernia 12:153–157
Grant AM, Scott NW, O'Dwyer PJ (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
Aasvang EK, Bay-Nielsen M, Kehlet H (2006) Pain and functional impairment 6years after inguinal herniorrhaphy. Hernia 10:316–321
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531
Dittrick GW, Ridl K, Kuhn JA, McCarty TM (2004) Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg 188:736–740
Mui WL, Ng CS, Fung TM, Cheung FK, Wong CM, Ma TH, Bn MY, Ng EK (2006) Prophylactic ilioinguinal neurectomy in open inguinal hernia repair: a double-blind randomized controlled trial. Ann Surg 244:27–33
Bartlett DC, Porter C, Kingsnorth AN (2007) A pragmatic approach to cutaneous nerve division during open inguinal hernia repair. Hernia 11:243–246
Picchio M, Palimento D, Attanasio U, Matarazzo PF, Bambini C, Caliendo A (2004) Randomized controlled trial of preservation or elective division of ilioinguinal nerve on open inguinal hernia repair with polypropylene mesh. Arch Surg 139:755–758, discussion 759
Weyhe D, Belyaev O, Muller C, Meurer K, Bauer KH, Papapostolou G, Uhl W (2007) Improving outcomes in hernia repair by the use of light meshes—a comparison of different implant constructions based on a critical appraisal of the literature. World J Surg 31:234–244
Mills IW, McDermott IM, Ratliff DA (1998) Prospective randomized controlled trial to compare skin staples and polypropylene for securing the mesh in inguinal hernia repair. Br J Surg 85:790–792
Paajanen H, Kossi J, Silvasti S, Hulmi T, Hakala T Randomized clinical trial of tissue glue versus absorbable sutures for mesh fixation in local anaesthetic Lichtenstein hernia repair. Br J Surg 98:1245-1251
Wong JU, Leung TH, Huang CC, Huang CS Comparing chronic pain between fibrin sealant and suture fixation for bilayer polypropylene mesh inguinal hernioplasty: a randomized clinical trial. Am J Surg 202:34-38
Chastan P (2009) Tension-free open hernia repair using an innovative self-gripping semi-resorbable mesh. Hernia 13:137–142
Pedano N, Pastor C, Arredondo J, Poveda I, Ruiz J, Monton S, Molina M, Hernandez-Lizoain JL (2012) Open tension-free hernioplasty using a novel lightweight self-gripping mesh: medium-term experience from two institutions. Langenbecks Arch Surg 397:291–295
Anadol AZ, Akin M, Kurukahvecioglu O, Tezel E, Ersoy E A prospective comparative study of the efficacy of conventional Lichtenstein versus self-adhesive mesh repair for inguinal hernia. Surg Today 41:1498-1503
Champault G, Torcivia A, Paolino L, Chaddad W, Lacaine F, Barrat C A self-adhering mesh for inguinal hernia repair: preliminary results of a prospective, multicenter study. Hernia 15:635-641
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quyn, A.J., Weatherhead, K.M. & Daniel, T. Chronic pain after open inguinal hernia surgery: suture fixation versus self-adhesive mesh repair. Langenbecks Arch Surg 397, 1215–1218 (2012). https://doi.org/10.1007/s00423-012-0949-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-0949-1