Abstract
Aims
Chronic pain following inguinal hernia repair may be related to the handling of cutaneous nerves. This study aims to investigate the frequency of cutaneous nerve division in routine practice and the effect that nerve division has on long-term pain outcomes.
Methods
The outcomes of 172 patients who underwent open inguinal hernia repair over a two-year period during the course of a clinical trial were recorded prospectively for 1 year. Pain scores for patients in whom one of the nerves was divided were compared with those of patients in whom all three were preserved.
Result
All nerves were preserved in 95 cases (55.2%). The ilioinguinal, genital and iliohypogastric nerves were divided in 33 (19.2%), 12 (7.0%) and 14 (8.1%) cases, respectively. There was no significant difference in pain scores between any of the nerve division groups compared to the group in which all three were preserved. There were three (1.7%) cases of significant chronic pain, two in which no nerves were divided.
Conclusion
The division of cutaneous nerves during inguinal hernia repair has no significant effect on postoperative pain. However, there are very few adverse outcomes, and so, a pragmatic approach of dividing nerves when they would otherwise be damaged may be appropriate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia is a common condition, with an annual incidence of approximately 105,000 in the UK [1]. Chronic pain following inguinal hernia repair is a significant adverse outcome that affects around 12% of patients [2]. Routine excision or division of the ilioinguinal and iliohypogastric nerves during inguinal hernia repair has been proposed as a means of avoiding postoperative neuralgia due to damage, entrapment or inflammation affecting the nerve. Recent studies have reported various outcomes following nerve division during inguinal hernia repair, ranging from a lower incidence of postoperative neuralgia to no improvement in postoperative pain and even an increased incidence of adverse effects, such as severe parasthesia. This study aims to investigate the frequency with which the ilioinguinal, genital and iliohypogastric nerves are divided in the routine practice of one surgeon and the effect of nerve division on early and long-term pain scores after open mesh repair of inguinal hernias.
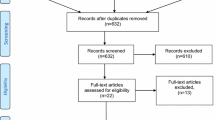
Methods
A total of 172 patients who underwent inguinal hernia repair between 1 June 2003 and 31 May 2005 had a comprehensive set of data collected prospectively as part of an ongoing randomised controlled study. All patients were over 18, undergoing elective open mesh repair of a primary uncomplicated unilateral hernia. All of the procedures were carried out at the Plymouth Hernia Service at the Derriford Hospital in Plymouth, UK. The surgery was performed by one consultant surgeon or a trainee under direct supervision of that consultant. Intraoperative data included information on whether the ilioinguinal, iliohypogastric and genital nerves were identified and, if so, whether they were preserved or divided. The nerves were preserved unless it was felt that they would hinder the placement of the mesh or would become entrapped by the mesh or suture material, in which case, they were divided cleanly at the edge of the wound. All patients were followed up at intervals by telephone for 1 year by a Hernia Nurse Specialist and pain scores were recorded using a visual analogue scale from 0 to 10 immediately prior to surgery and at days 3, 7 and 14 and at 6 months and 1 year postoperatively. The pain scores at each of the points of follow up for patients in whom the ilioinguinal, iliohypogastric or genital nerves only were divided were compared with those for patients in whom all three nerves were preserved. Patients in whom more than one nerve was divided, or one or more nerves was not identified, were not included in the analysis. Statistical analysis was performed using the Mann-Whitney U test. A P value of less than 0.05 was used to determine statistical significance.
Results
The data regarding which nerves were identified and whether they were divided or preserved was available for all 172 cases, as was the data for postoperative complications. The data for postoperative pain scores was complete for 97 patients (56.4%). More than one postoperative pain score was missing for 41 patients (23.8%). These cases were included in the analysis. The median age was 57 (range 19–87). There were 159 male and 13 female patients (M:F ratio 12:1).
All three nerves were identified and preserved in 95 cases (55.2%). One or more nerves were not identified in 25 cases (14.5%). At least one nerve was divided in 53 cases (30.8%). The total number of patients in which each of the three nerves was not identified or divided is shown in Table 1. The ilioinguinal nerve was the only nerve to be divided in 26 cases (15.1%), the genital nerve in nine cases (5.2%) and the iliohypogastric in 11 cases (6.4%).
There was no significant difference in the median baseline pain scores between any of the three groups in which a nerve was divided compared to the group in which all three nerves were preserved (Table 2). Postoperatively, there was no significant difference in the median pain scores between any of the three groups in which a nerve was divided compared to the group in which all three nerves were preserved at any of the follow up points (Table 3).
Postoperative complications other than parasthesia and pain were reported in 11 patients (6.4%). These included six wound infections, two haematomas, two recurrences and one seroma. As would be expected, these complications had no correlation with the division or preservation of cutaneous nerves.
There were only two cases (1.1%) of significant parasthesia, occurring in the distribution of the genitofemoral nerve, both in patients whose genital nerves only were divided. There were no other complaints of significant numbness or parasthesia during follow up. However, objective testing of the loss of sensation was not carried out.
There were only three patients (1.7%) who felt that chronic postoperative pain was a problem. One patient, whose genital nerve only was divided, had a significantly high pain score of 8 at 1 year. Two patients, in both of whom all three nerves were preserved, complained of testicular pain that was still ongoing at the end of the study and scrotal pain during sexual intercourse, respectively. However, their pain scores at 12 months were low at 4 and 1, respectively.
Discussion
Chronic pain has been reported to be a significant problem following inguinal hernia repair, although, in this series, the incidence was relatively low (1.7%). The identification of the ilioinguinal, genital and iliohypogastric nerves during open inguinal hernia surgery is usually straightforward and, therefore, the opportunity to ensure that they are preserved or to purposefully divide them is usually available.
A number of studies have supported the theory that the division of these nerves may reduce postoperative pain. Dittrick et al. [3] conducted a retrospective review of 90 patients who had undergone Lichtenstein repair with either routine excision of the ilioinguinal nerve (n = 66) or nerve preservation (n = 24). They found a significantly lower incidence of postoperative neuralgia in the neurectomy group compared to the nerve preservation group at 6 months (3% vs. 26%, P<0.001) and at 1 year (3% vs. 25%, P = 0.003). There was no significant difference in postoperative parasthesia, although there was a trend towards an increased incidence of parasthesia in the neurectomy group.
Tsakayannis et al. [4] looked at 191 patients undergoing primary unilateral inguinal hernia repair using a plug and sutured mesh technique. In each case, an effort was made to identify and divide both the ilioinguinal and iliohypogastric nerves. Following surgery, patients were followed up at 1 month, 6 months and 1 year. None of the patients complained of any moderate or severe postoperative pain. Numbness was reported in 18 patients (9.4%) at 1 month but this reduced to 12 (6.3%) at 6 months and 1 year.
Neurectomy has also been advocated as a later procedure for patients suffering from chronic pain following inguinal hernia repair. Aasvang and Kehlet [2] performed a literature review and found 14 papers describing neurectomy of the ilioinguinal, iliohypogastric, genitofemoral or lateral femoral cutaneous nerves. They reported that, overall, there was a favourable outcome but methodological quality was poor in all studies.
The association between reduced chronic pain and neurectomy has not, however, been reproduced in randomised controlled studies. Ravichandran et al. [5] studied 20 men undergoing open mesh repair of primary bilateral hernias and randomised the sides for the preservation or division of the ilioinguinal nerve. They were followed up 1 day and at 4 weeks and 6 months after surgery. Median pain scores were not significantly different between the divided and preserved sides at day 1 (2.9 vs. 2.5, P = 0.98). At 6 months, two patients complained of minor wound discomfort, one on the divided side and one on the preserved side. There were two complaints of numbness on the divided side at 6 months.
Picchio et al. [6] randomised a much larger group of 813 patients with primary inguinal hernia to ilioinguinal nerve preservation (n = 408) or division (n = 405) during open mesh repair. Division of the nerve was performed lateral to the deep ring and was confirmed with histological analysis. Follow up was carried out by blinded assessors for up to 12 months following surgery. No significant difference in pain scores was found between the two groups, with 63% of the preservation group and 66% of the division group reporting an absence of pain at 6 months and 76% and 73%, respectively, at 1 year. However, it was found that touch sensation was significantly decreased when the ilioinguinal nerve was divided, although the authors do not comment as to whether this was subjective.
The present study has looked prospectively at a relatively large series of patients undergoing routine open inguinal hernia repair and showed that the ilioinguinal, genital and iliohypogastric nerves may be identified in most cases. In the routine practice of one surgeon, it was felt necessary to divide at least one of the nerves in almost one third of cases. However, this study is unable to demonstrate a significant beneficial effect on chronic postoperative pain following the division of cutaneous nerves. A confounding factor may well be that the nerves were only divided when it was felt that they would otherwise hinder mesh placement with the risk of entrapment or damage. It is possible that these patients would have suffered more severe pain had the nerves not been divided and, furthermore, that if the group in which the nerves hindered placement of the mesh or suture had been randomised to nerve division or preservation, then a difference might have been found.
At present, there is little convincing evidence that routine neurectomy has a significant effect on chronic pain following open inguinal hernia surgery; indeed, most evidence is against this. However, this study and others have shown that there are few adverse effects of this procedure. There may also be some evidence supporting the use of neurectomy as a later procedure for the treatment of chronic pain following inguinal hernia repair. Therefore, a pragmatic approach of dividing the ilioinguinal, genital and iliohypogastric nerves when they are otherwise likely to be damaged may be appropriate.
References
National Institute for Clinical Excellence (NICE) (2001) Guidance on the use of laparoscopic surgery for inguinal hernia. NICE, London, UK. Available online at http://www.nice.org.uk/pdf/Laphernias_Full_guidance.pdf
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92(7):795–801
Dittrick GW, Ridl K, Kuhn JA, McCarty TM (2004) Routine ilioinguinal nerve excision in inguinal hernia repairs. Am J Surg 188(6):736–740
Tsakayannis DE, Kiriakopoulos AC, Linos DA (2004) Elective neurectomy during open, “tension free” inguinal hernia repair. Hernia 8(1):67–69
Ravichandran D, Kalambe BG, Pain JA (2000) Pilot randomized controlled study of preservation or division of ilioinguinal nerve in open mesh repair of inguinal hernia. Br J Surg 87(9):1166–1167
Picchio M, Palimento D, Attanasio U, Matarazzo PF, Bambini C, Caliendo A (2004) Randomized controlled trial of preservation or elective division of ilioinguinal nerve on open inguinal hernia repair with polypropylene mesh. Arch Surg Chicago 139(7):755–758
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bartlett, D.C., Porter, C. & Kingsnorth, A.N. A pragmatic approach to cutaneous nerve division during open inguinal hernia repair. Hernia 11, 243–246 (2007). https://doi.org/10.1007/s10029-007-0209-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-007-0209-4