Abstract
Purpose
The relationship between neo-adjuvant chemotherapy prior to hepatectomy in patients with resectable colorectal liver metastases and post-operative morbidity still has to be clarified.
Methods
Data from 242 patients undergoing hepatectomy for colorectal liver metastases, judged resectable at first observation, were reviewed and their clinical outcome was related to neo-adjuvant chemotherapy (125 patients). Selection biases were outlined and properly handled by means of propensity score analysis.
Results
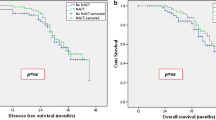
Post-operative death was 1.2% and morbidity 40.9%. Pre-operative chemotherapy was only apparently related to higher morbidity (P = 0.021): multivariate analysis identified extension of hepatectomy and intra-operative blood loss as independent prognostic variables (P < 0.05). Patients receiving and not receiving neo-adjuvant chemotherapy were significantly different for several covariates, including extension of hepatectomy (P = 0.049). After propensity score adjustment, 94 patients were identified as having similar covariate distribution (standardized differences <|0.1|) except for neo-adjuvant treatment (47 patients for each group). In this matched sample, mortality was similar and post-operative complications were only slightly higher (hazard ratio = 1.38) in treated patients. A significantly higher need for fluid replacement was only observed in patients receiving neo-adjuvant chemotherapy (P = 0.038).
Conclusions
Neo-adjuvant chemotherapy showed a limited role in determining post-operative morbidity after hepatic resection and did not modify mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is a leading cause of cancer-related morbidity and mortality worldwide [1, 2]. The liver is the most common site of metastases, observed in up to 25% of patients at the time of initial diagnosis and within 3 years after primary colonic surgery in more than 50% of stage III patients [3–5]. Neo-adjuvant chemotherapy has become an integral part of the multidisciplinary management of metastatic colorectal cancer. It can result in the down-staging of disease and thus improve hepatic resection rates by 13–20% [6, 7]. The practice of administering neo-adjuvant chemotherapy in patients with resectable colorectal liver metastases has recently increased. This practice is aimed at assessing response to treatment, limiting the extent of liver resection, reducing R1 resection rates, and avoiding surgery in patients with rapidly progressive disease as a result of chemotherapy resistance, thereby improving patient selection [8]. The drawbacks include the potential induction of chemotherapy-associated steato-hepatitis and veno-occlusive changes that manifest as a mottled, friable, and hemorrhagic liver that makes parenchymal dissection a more hazardous procedure and hemostasis more difficult to achieve, with a consequent expected increase in perioperative morbidity and mortality [9–13]. In the EORTC trial of Nordlinger et al. in 2008, an increased occurrence of reversible post-operative complication was reported in patients receiving neo-adjuvant chemotherapy in comparison to patients who were submitted to surgery alone [13], whereas retrospective analyses from various series reported contrasting results [14–18]. These discrepancies are probably the consequence of population selection biases typical of observational retrospective studies. In fact, patients submitted to neo-adjuvant chemotherapy often have a more extended tumor burden or synchronous metastases, and they more frequently undergo more extended hepatectomy or concomitant bowel resection in comparison to those not submitted to pre-operative chemotherapy [9–12, 14–18]. To be fair, treated and untreated subjects must be compared as if they were similar in terms of everything able to affect the outcome, except for the receipt of treatment. Propensity score methods are increasingly being used in medical research to reduce the impact of treatment selection bias in the estimation of causal treatment effects in observational data [19–22]. The propensity score is a subject’s probability of receiving a specific treatment conditional on the observed covariates. Matching on the propensity score makes it possible to balance measured variables between treated and untreated subjects. Propensity scores are an alternative method of estimating the effect of receiving treatment when random assignment of treatments to subjects (randomized controlled trials; RCT) is not feasible. In observational studies, random assignment to treatments is not possible. The primary limitation of an observational study is that there may be random selection of subjects but not random allocation of treatments to subjects. When there is lack of randomization, casual inferences (i.e., multivariate models) cannot be made because it is not possible to determine whether the difference in outcome between the treated and control subjects is due to the treatment or differences between subjects in other characteristics.
The main aim of the present study was to assess the effective role of neo-adjuvant chemotherapy in the early post-operative period in a large prospectively collected database from a single-institution experience over the last decade. The impact of population selection bias in determining post-operative course was handled by means of propensity score match. Thus, treated and untreated subjects were adequately matched and post-operative morbidity and mortality were assessed in the matched sample of patients having the same covariate distribution. This approach allows us to identify the potential confounding variables that can explain the differences reported in post-operative morbidity in relationship with neo-adjuvant chemotherapy and to conduct an analysis similar to an RCT aimed at assessing the effective role of neo-adjuvant chemotherapy in determining the outcome of hepatic resection for colorectal liver metastases.
Methods
Patient selection
Between 1st January 2001 and 31st December 2009, 274 patients underwent potentially curative surgery for colorectal liver metastases at our institution. In order to reduce the impact of potentially confounding variables in the assessment of post-operative complications, the following exclusion criteria were applied to select the study population: repeated hepatectomy (21 patients), pre-operative portal vein embolization (six patients), simultaneous pulmonary resection (four patients), or nephrectomy (one patient). The study population consisted of 242 patients. All patient data were prospectively entered into a database over the years. These data included demographic variables, characteristics of primary and metastatic colorectal cancer, details regarding pre-operative chemotherapy, type and duration of surgery, intra- and post-operative course, and length of in-hospital stay. Macrovesicular steatosis was also assessed on the histological specimen and defined as hepatocytes containing one large vacuole of fat displacing the nucleus peripherally and was graded as absent versus present [10–12].
Main outcome measures
The main aim of the present study was to assess which pre-operative variables could affect post-operative morbidity, paying special attention to the role of neo-adjuvant chemotherapy. For the purpose of defining post-operative complications, the classification proposed by Clavien and coworkers was applied [23] and complications were defined as mild (grade I), moderate (grade II), severe without general anesthesia (GA) (grade IIIa) and under GA (grade IIIb), and severe with single- or multiorgan system failure (grade IV). A grade V complication was death of the patient: death was counted as any mortality during hospital stay or within 30 days of surgery. The following liver-related complications were also collected for all patients and graded according to Clavien’s classification [22, 23]: occurrence of refractory ascites was defined as a grade II complication when it caused a delay in the removal of surgical drainages or as grade IIIa when treated with an invasive procedure without GA (paracentesis); an increase of bilirubin level above 3 mg/dL (294 μmol/L) was graded as a grade II complication because it was not treated with any specific drug; alteration of coagulation factors requiring fresh frozen plasma (FFP) infusion with an INR above 1.50 (in the absence of serum bilirubin level above 12 mg/dL) was graded as grade II because it required pharmacological treatment with drugs other than those allowed for mild complications; renal impairment, defined as blood urea nitrogen above 2.00 g/L and/or increase of serum creatinine above 2.00 mg/dL (182 μmol/L), was graded as grade I complications when treated with only loop diuretics, as grade II in cases of treatment with dopamine or terlipressin or as grade IV in cases of renal impairment that required dialysis.
Neo-adjuvant chemotherapy
The treating medical oncologist determined the indication for chemotherapy and the regimen used; all patients receiving neo-adjuvant chemotherapy included in the present analysis were judged to have initially resectable metastases at diagnosis. Chemotherapy was adopted in 125 of the 242 patients forming the study group (51.7%). Firstline treatment consisted of fluoropyrimidine (5-fluorouracil, 5-FU)-based regimes in the majority of cases (5-FU + leucovorin in 21 patients, 16.8%, 5-FU + oxaliplatin alone in 50, 40.0%, 5-FU + irinotecan alone in 16, 12.8%) and other regimes were adopted in the remaining proportion (38 patients, 30.4%). Within other regimes, the associated use of oxaliplatin and irinotecan was adopted in 11 patients (8.8%); bevacizumab was combined with oxaliplatin in 4 (3.2%) and with irinotecan in 11 (8.8%); cetuximab and panintumumab were adopted in one case each, in combination with oxaliplatin in both cases (1.6%). Raltitrexed or capecitabine were adopted in the remaining proportion of patients (ten patients, 8.0%). Chemotherapy was administered for a median of 6 cycles before liver resection (range 3–10 cycles), and ended at least 4 weeks before surgery in the majority of patients (120 out of 125, 96%). Adjuvant chemotherapy after resection usually restarted 45 weeks after surgery. Experimental protocols were approved by the appropriate institutional review committee and met the guidelines of their responsible governmental agency. Informed written consent was obtained from all patients included in the analysis.
Statistical analysis
Continuous variables were expressed as mean and standard deviation and/or median and range. Categorical variables were reported as the number of cases and prevalence. Student’s t-test, Mann–Whitney test, and Fisher exact test were applied as appropriate. Logistic regression was applied to verify the relationship between clinical, demographical, tumoral, and surgical variables considered and the occurrence of a post-operative complication. Variables significantly related to morbidity at univariate analysis were entered in a multivariate backward logistic regression model. Continuous variables were categorized on the basis of their median value.
In order to investigate the relationship existing between neo-adjuvant chemotherapy and the main outcome measure (morbidity), a one-to-one match was created using propensity score analysis. In an observational study of the effect of treatments, exposures, or interventions, the propensity score is the probability of treatment assignment conditional on observed baseline covariates [20–22]. For this purpose, an iterative matching method was adopted until the baseline variables were balanced between treated and untreated subjects. Propensity score was calculated through a logistic regression model having as independent variables those variables significantly different between treated and untreated subjects and/or related to the main outcome measure and with the neo-adjuvant chemotherapy variable selected as a dependent variable. Match was performed by using the nearest neighbor matching method, without replacement, using a specified caliper of 0.2 of the standard deviation of the logit of the propensity score, without replacement until all possible matches had been formed. This caliper was selected because it was shown to result in optimal estimation compared with other choices of caliper [24]. Balance in the matched sample was assessed iteratively through standardized differences (d) calculation. Once the final matched groups had been obtained, the treatment effect on intraoperative and post-operative course was assessed by paired t-tests for continuous variables and by the McNemar test for correlated binary proportion. P values asless than 0.05 were considered as statistically significant. All calculations were performed using SPSS 12.0 (SPSS, Inc, Chicago, IL, USA).
Results
Patient characteristics, mortality, and morbidity
Patient demographics and clinical and tumor characteristics are detailed in Table 1. Post-operative death was 1.2% (three cases) and overall morbidity was 40.9% (99 cases). The median in-hospital stay was 8 days (range, 4–74 days). Mild (28.1%) and moderate (38.8%) complications were those most frequently observed. In particular, infection and/or fever requiring a change of antibiotics was the most frequent (20.2%) followed by pleural effusion or atelectasis on chest radiography (18.6%). Severe complications requiring general anesthesia (3.3%) and organ system failure (1.2%) were infrequent and this latter complication led to patient death in the three reported cases. A detailed list of post-operative complications is reported in the “Electronic supplementary material” (Table S1). Overall, 98 patients (40.5%) experienced at least one minor complication (grade I–II) whereas 24 patients (9.9%) experienced at least one major complication (grade III–IV). One patient experienced only one severe complication not requiring general anesthesia (grade IIIa) and without any associated minor complication (need for continuous positive air pressure, CPAP).
Table 2 reports relationships observed between demographical, clinical, tumoral, and surgical characteristics considered and morbidity at univariate analysis. It should be noted that the administration of neo-adjuvant chemotherapy proved to be significantly related to complication occurrence (P = 0.021). However, results from the multivariate analysis, reported in Table 3, showed that extension of hepatectomy (P = 0.012) and the need for intra-operative red blood cells transfusion (P = 0.002) were the only variables independently associated with complications after surgery, whereas the use of neo-adjuvant chemotherapy did not prove independently related to morbidity (P = 0.277). Of particular note is the finding that morbidity of treated patients submitted to major hepatectomy was 62.7% (37/59) while that of untreated patients was 42.5% (17/40; P = 0.038); conversely, morbidity of treated patients submitted to minor hepatectomy was 34.8% (23/66) while that of untreated patients was 28.6% (22/77; P = 0.266).
The role of neo-adjuvant chemotherapy
Among the 125 patients who received neo-adjuvant chemotherapy, 60 (48.0%) experienced at least one complication, whereas nine patients (7.2%) also experienced at least one major complication (grade III–IV). Neo-adjuvant chemotherapy with 5FU + oxaliplatin was related to a morbidity of 46.0% (23/50), 5FU + irinotecan was related to a morbidity of 58.3% (9/16), 5FU + leucovorin was related to a morbidity of 38.1% (8/21), and other chemotherapeutic regimes to a morbidity of 52.6% (20/38) (P = 0.547). As outlined in Table 4, patients undergoing surgery with or without neo-adjuvant chemotherapy differed significantly from each other as regards demographic, clinical, tumor, and surgical characteristics. Patients receiving neo-adjuvant chemotherapy were younger (P = 0.001), with a higher prevalence of synchronous metastases (P = 0.001), a lower platelet count (P = 0.008), higher pre-operative levels of gamma glutamyl transferase (P = 0.026), higher tumor number (P = 0.001), and Nordlinger score (P = 0.001) and were more frequently submitted to major hepatectomy (P = 0.049) and synchronous bowel resection (P = 0.043). Consequently, to adequately compare morbidity of the treated and untreated subjects, they were first matched for these covariates.
Analysis of neo-adjuvant chemotherapy after matching
The results of the propensity score analysis are reported in Table 5. Forty-seven patients of the 125 receiving neo-adjuvant chemotherapy (37.6%) and an equal number of the 117 patients not receiving neo-adjuvant chemotherapy (40.2%) of the whole study group were matched after covariate adjustment; thus, 78 patients with neo-adjuvant and 70 without neo-adjuvant chemotherapy were excluded because their propensity score was not matchable. The new study group of 94 patients was now well matched and covariates that significantly affected morbidity in the whole study group were equally distributed over the two matched groups (d-value lower than the absolute value of 0.1; d < |0.1|). In particular, extension of hepatectomy was identical between treated and un-treated subjects: wedge resection or segmentectomy 34.0%, bi-segmentectomy 19.1%, major hepatectomy 46.8% in both groups. The matched sample of 94 patients had an overall morbidity of 39.3% (38 cases) and a post-operative death of 1.1% (one case).
Details regarding intra- and post-operative course are reported in Table 6. Patients submitted to neo-adjuvant chemotherapy required a significantly higher amount of fluid infusion (including crystalloids, colloids, RBC and FFP transfusions and albumin) during surgery (P = 0.038). In particular, the 17 patients submitted to neo-adjuvant chemotherapy and receiving RBC transfusion required a median of 500 ml of RBC (range, 250–2,1500) whereas the 16 non-treated patients required a median of 600 ml (range, 250–3,300). The ten patients submitted to neo-adjuvant chemotherapy and receiving FFP transfusion required a median of 600 ml of FFP (range 150–2,100) whereas the nine non-treated patients required a median of 300 ml of FFP (range, 150–600). Post-operative complications were higher in patients receiving neo-adjuvant chemotherapy but not statistically significant at the paired McNemar test. In particular, the pair-matched odds ratio for overall morbidity was 1.38 (95% C.I. = 0.55–3.42) for patients receiving neo-adjuvant chemotherapy and for minor complications it was 1.50 (95%C.I. = 0.61–3.67); in other words, to detect this latter increase with 80% power at two-sided 5% significance levels, a population with at least 254 patients for each arm would be necessary to observe statistical significance. Finally, post-operative in-hospital stay was similar between the two groups (P = 0.397).
Discussion
Pre-operative chemotherapy is currently being used more and more often in patients with colorectal metastases either on a neo-adjuvant basis for already resectable tumors or for down-staging unresectable disease. As a consequence, hepatic resection in patients who have already been exposed to systemic chemotherapy is becoming increasingly common in surgical practice [8]. Some studies suggest a change in the liver parenchyma following chemotherapy: oxaliplatin was associated with an increase in sinusoidal injury [9, 10, 25, 26], whereas irinotecan was associated with an increased risk of steato-hepatitis [10, 27, 28]. The effect of chemotherapy on early post-operative outcome is still controversial in the literature, especially when results come from retrospective observational studies [9–12, 14–18]. Propensity score analysis can help in reducing the impact of confounding variables, and matching on the propensity score makes it possible to balance measured variables between treated and untreated subjects.
The first result of the present study is that patients receiving neo-adjuvant chemotherapy only apparently experienced more complications after surgery in comparison to those who did not receive pre-operative chemotherapy. The bias related to population selection is highlighted by both the multivariate analysis that showed that extension of hepatectomy was the sole variable related to post-operative morbidity and the relatively small proportion of treated and untreated patients having similar characteristics and available for propensity score match (26.4%). This small proportion is the result of the fact that treated and un-treated patients were significantly different from each other. Such a population selection bias is typical of observational retrospective studies and the contrasting results reported by previous studies could be the consequence of comparing apples with oranges [19]. Differences in the covariate distribution between patients receiving neo-adjuvant chemotherapy or not can be found in most of the studies regarding safety of hepatic resection for colorectal liver metastases [9–12, 15–18, 25, 27, 28], except one [13]. In the Nordlinger RCT, the bias was reduced by the nature of the study itself. Even if the study was not planned to detect an increase in morbidity, reversible post-operative complications were found to occur more frequently after chemotherapy than after surgery alone (P = 0.040) with a calculated odds ratio of 1.78 (95% C.I. = 1.03–3.07). At present, this is the only study with a level I of evidence that showed an increased morbidity after neo-adjuvant chemotherapy. The present propensity score analysis showed that a slight increase in post-operative minor complications could be expected with an observed odds ratio of 1.50 (thus, within the 95% C.I. reported by Nordlinger et al.), but it failed to detect a statistically significant difference because of the small size of the matched population, as highlighted by the sample size calculation: to detect the observed increase with 80% power at two-sided 5% significance levels, a population with at least 254 patients for each arm was required.
Livers subjected to pre-operative chemotherapy have been noted to be more fragile and hemorrhagic. In the present analysis, extension of hepatectomy and the need for intra-operative red blood cells transfusion were the sole variables independently associated with complications after surgery. The presence of sinusoidal injury or macroscopic signs of steato-hepatitis could lead to a more difficult to obtain hemostasis during surgery, especially when performing major hepatectomy [6, 15, 29]. These macroscopic features can also lead surgeons to carry out less frequent or shorter pedicle clamping because of fear of ischemia–reperfusion injury, thus increasing blood loss. In the present study, a significant increase in fluid replacement was observed in patients receiving neo-adjuvant chemotherapy in the matched population. As also observed in the present multivariate analysis, higher intra-operative blood loss is an established risk factor for post-operative morbidity and mortality [15, 30, 31], so it is reasonable to suppose a role for this factor in determining the increase of morbidity observed in treated subjects of the present study population. Neo-adjuvant chemotherapy can lead to increased intra-operative blood loss that, in turn, could lead to a relative increase in morbidity. This effect is probably magnified in the presence of lower residual liver volume as can be expected after a major hepatectomy, as suggested by the finding that morbidity of treated patients was significantly higher only in patients submitted to major hepatic resection.
Regarding the potential association between the chemotherapy regime adopted and post-operative complications, the present study did not find any significant relationship between irinotecan, oxaliplatin, or bevacizumab and morbidity. Irinotecan and oxaliplatin were only apparently associated with more frequent complications but were not significantly related to the main outcome measure of the present study. These findings are still in keeping with the reported results of an increased prevalence of steato-hepatitis and sinusoidal obstruction syndrome in patients receiving irinotecan or oxaliplatin, respectively, and of their not clear significance in modifying the clinical outcome [10, 14, 26–28, 32]. It should be noted however that in the present experience, chemotherapy was administered for a median of 6 cycles before liver resection and ended at least 4 weeks before surgery in 96% of patients. Duration and timing of neo-adjuvant chemotherapy are covariates that have been reported to be related to complication occurrence [11, 33] and this feature can, on one hand, partly explain the slight difference observed in the post-operative assessment of morbidity of the two matched groups and in the relationship with the chemotherapy regime adopted; on the other hand, it outlines the importance of covariate adjustment in the interpretation of the results. Unfortunately, a sub-analysis of different neo-adjuvant chemotherapy regimes in the matched sample was impossible due to the low number of cases in each category (more than 30.0% of cells have an expected count of less than 5) and this factor represents another issue that needs to be adequately clarified through well-designed controlled studies.
In conclusion, the present study suggests a very limited role of neo-adjuvant chemotherapy in determining post-operative morbidity after hepatic resection. Most concerns related to contrasting results reported in the literature can be the end result of population selection bias since patients submitted to neo-adjuvant chemotherapy often have a more extended tumor burden or synchronous metastases, and they more frequently undergo more extended hepatectomy or concomitant bowel resection in comparison to those not submitted to pre-operative chemotherapy. More RCTs are needed to give a reliable estimation of the pre-operative role of chemotherapy in determining post-operative outcome because of the strong impact of the multitude of covariates able to affect the outcome as outlined by the present propensity score analysis.
References
Ries LAG, Melbert D, Krapcho M, SEER Cancer Statistics Review, 1975–2005, National Cancer Institute (2008) Bethesda, MD, based on November 2007 SEER data submission. [updated 2008; cited]. http://seer.cancer.gov/csr/1975_2005/
Cancer trends in the UK (2006) Available at http://www.cancerresearchuk.org/. Last accessed 01/02/2011
Scheele J, Stangl R, Altendorf-Hofmann A (1990) Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg 77:1241–1246
Sugarbaker PH (1990) Surgical decision making for large bowel cancer metastatic to the liver. Radiology 174:621–626
Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J (1994) Factors influencing the natural history of colorectal liver metastases. Lancet 343:1405–1410
Bismuth H, Adam R, Lévi F, Farabos C, Waechter F, Castaing D et al (1996) Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg 224:509–520
Adam R, Avisar E, Ariche A, Giachetti S, Azoulay D, Castaing D et al (2001) Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal. Ann Surg Oncol 8:347–353
Chua TC, Saxena A, Liauw W, Kokandi A, Morris DL (2010) Systematic review of randomized and nonrandomized trials of the clinical response and outcomes of neoadjuvant systemic chemotherapy for resectable colorectal liver metastases. Ann Surg Oncol 17:492–501
Nakano H, Oussoultzoglou E, Rosso E, Casnedi S, Chenard-Neu MP, Dufour P et al (2008) Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg 247:118–124
Vauthey JN, Pawlik TM, Ribero D, Wu TT, Zorzi D, Hoff PM et al (2006) Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol 24:2065–2072
Welsh FK, Tilney HS, Tekkis PP, John TG, Rees M (2007) Safe liver resection following chemotherapy for colorectal metastases is a matter of timing. Br J Cancer 96:1037–1042
Fong Y, Bentrem DJ (2006) CASH (chemotherapy-associated steatohepatitis) costs. Ann Surg 243:8–9
Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, EORTC Gastro-Intestinal Tract Cancer Group et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 371:1007–1016
Hewes JC, Dighe S, Morris RW, Hutchins RR, Bhattacharya S, Davidson BR (2007) Preoperative chemotherapy and the outcome of liver resection for colorectal metastases. World J Surg 31:353–364
Sahajpal A, Vollmer CM Jr, Dixon E, Chan EK, Wei A, Cattral MS et al (2007) Chemotherapy for colorectal cancer prior to liver resection for colorectal cancer hepatic metastases does not adversely affect peri-operative outcomes. J Surg Oncol 95:22–27
Scoggins CR, Campbell ML, Landry CS, Slomiany BA, Woodall CE, McMasters KM et al (2009) Preoperative chemotherapy does not increase morbidity or mortality of hepatic resection for colorectal cancer metastases. Ann Surg Oncol 16:35–41
Wicherts DA, de Haas RJ, Sebagh M, Saenz Corrales E, Gorden DL, Lévi F et al (2011) Impact of bevacizumab on functional recovery and histology of the liver after resection of colorectal metastases. Br J Surg 98:399–407
Tamandl D, Gruenberger B, Klinger M, Herberger B, Kaczirek K, Fleischmann E et al (2010) Liver resection remains a safe procedure after neoadjuvant chemotherapy including bevacizumab: a case-controlled study. Ann Surg 252:124–130
Zinsmeister AR, Connor JT (2008) Ten common statistical errors and how to avoid them. Am J Gastroenterol 103:262–266
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Blackstone EH (2002) Comparing apples and oranges. J Thorac Cardiovas Surg 123:8–15
Cucchetti A, Ercolani G, Vivarelli M, Cescon M, Ravaioli M, Ramacciato G et al (2009) Is portal hypertension a contraindication to hepatic resection? Ann Surg 250:922–928
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications—a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161
Tamandl D, Klinger M, Eipeldauer S, Herberger B, Kaczirek K, Gruenberger B et al (2011) Sinusoidal obstruction syndrome impairs long-term outcome of colorectal liver metastases treated with resection after neoadjuvant chemotherapy. Ann Surg Oncol 18:421–430
Rubbia-Brandt L, Audard V, Sartoretti P, Roth AD, Brezault C, Le Charpentier M et al (2004) Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol 15:460–466
Fernandez FG, Ritter J, Goodwin JW, Linehan DC, Hawkins WG, Strasberg SM (2005) Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg 200:845–853
Pawlik TM, Olino K, Gleisner AL, Torbenson M, Schulick R, Choti MA (2007) Preoperative chemotherapy for colorectal liver metastases: impact on hepatic histology and postoperative outcome. J Gastrointest Surg 11:860–868
Tanaka K, Adam R, Shimada H, Azoulay D, Lévi F, Bismuth H (2003) Role of neoadjuvant chemotherapy in the treatment of multiple colorectal metastases to the liver. Br J Surg 90:963–969
Gruttadauria S, Saint Georges Chaumet M, Pagano D, Marsh JW, Bartoccelli C, Cintorino D et al (2011) Impact of blood transfusion on early outcome of liver resection for colorectal hepatic metastases. Surg Oncol 103:140–147
Kooby DA, Stockman J, Ben-Porat L, Gonen M, Jarnagin WR, Dematteo RP et al (2003) Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg 237:860–869
Morris-Stiff G, Tan YM, Vauthey JN (2008) Hepatic complications following preoperative chemotherapy with oxaliplatin or irinotecan for hepatic colorectal metastases. Eur J Surg Oncol 34:609–614
Nordlinger B, Vauthey JN, Poston G, Benoist S, Rougier P, Van Cutsem E (2010) The timing of chemotherapy and surgery for the treatment of colorectal liver metastases. Clin Colorectal Cancer 9:212–218
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Table S1
Post-operative complications graded according to Clavien’s classification. One patient could experience more than one complication of any grade; consequently, the sum of each complication could be different from the overall count. Small bowel dysfunction included prolonged post-operative ileus and diarrhea; ECG abnormalities included atrial fibrillation, ST segment abnormalities. TPN total parenteral nutrition, CPAP continuous positive air pressure, FBS fibroscopic bronchoscopy, GA general anesthesia (DOC 26 kb)
Rights and permissions
About this article
Cite this article
Cucchetti, A., Ercolani, G., Cescon, M. et al. Safety of hepatic resection for colorectal metastases in the era of neo-adjuvant chemotherapy. Langenbecks Arch Surg 397, 397–405 (2012). https://doi.org/10.1007/s00423-011-0894-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0894-4