Abstract
Background
Neoadjuvant systemic chemotherapy is being increasingly used prior to liver resection for colorectal metastases. Oxaliplatin has been implicated in causing structural changes to the liver parenchyma, and such changes may increase the morbidity and mortality of surgery.
Patients and Methods
A retrospective study was undertaken of 101 consecutive patients who had undergone liver resection for colorectal metastases in two HPB centers. Preoperative demographic and premorbid data were gathered along with liver function tests and tumor markers. A subjective assessment of the surgical procedure was noted, and in-hospital morbidity and mortality were calculated. The effect of preoperative chemotherapy on short-term and long-term outcome was analyzed, and actuarial 1 and 3 year survival was determined.
Results
Patients who received neoadjuvant chemotherapy had a higher number of metastases (median 2, range 1–8 versus median 1, range 1–5; P = 0.019) and more had synchronous tumors (24 patients versus 8; P < 0.001). Overall morbidity was 37% and hospital mortality was 3.9%. Operative and in-hospital outcome was not influenced by chemotherapy. Long-term survival was worse in patients who had received preoperative chemotherapy (actuarial 3-year survival 62% versus 80%; P = 0.04).
Conclusions
This study shows no evidence that neoadjuvant chemotherapy, and in particular oxaliplatin, increases the risk associated with liver resection for colorectal metastases. Long-term outcome is reduced in patients receiving preoperative chemotherapy, although they have more advanced disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Liver resection is currently the only treatment that offers the chance of long-term survival in patients with colorectal cancer (CRC) liver metastases. Five year survival rates following surgery range from 25% to 47%,1–5 with some studies showing 10-year survival up to 26%.2,6 This compares to almost no survivors at 5 years if the metastases are left untreated.7 At major centers, the perioperative mortality of liver surgery is less than 5%, with complication rates ranging between 20% and 50%.8,9 At presentation only 10%–25% of patients are suitable for hepatectomy2,10; hence recent efforts have been directed at increasing resectability rates. Downstaging chemotherapy, two-stage liver resections and portal vein embolizations are effective methods of rendering some unresectable patients amenable to curative resection, and these new strategies may increase the resectability rate by as much as 20%.11
The use of oxaliplatin or irinotecan has been shown to downstage some tumors initially deemed to be too extensive or poorly positioned for safe surgery, to a level where hepatectomy can be performed.12–14 The combination of 5-fluorouracil and folinic acid (5FU/FA) with oxaliplatin has been shown to give a response rate of 50% in patients with colorectal metastases.15 Follow-up studies of patients who had undergone liver resection after downstaging neoadjuvant chemotherapy have shown overall 5-year survival of 35%–50% in patients who were initially deemed unresectable.16,17 This survival is comparable to that in patients who have not required downstaging treatment. Neoadjuvant therapy has also recently been shown in a retrospective, nonrandomized study to offer a survival advantage in patients with a large number of bilobar metastases.18
The role of systemic chemotherapy in patients with resectable CRC liver metastases has not been established. It is common practice in the UK, however, for patients to be administered chemotherapy prior to or synchronously with referral for resection, especially if they have synchronous metastases. The prognosis of these patients following resection is worse than that for patients with metachronous disease, and they may therefore benefit more from systemic chemotherapy. Operating on livers pre-exposed to systemic chemotherapy is therefore becoming more common.
Hepatobiliary surgeons report an alteration to the appearance and texture of the liver post-chemotherapy. These changes manifest as a mottled, friable, and hemorrhagic liver that makes parenchymal dissection a more hazardous procedure and hemostasis more difficult to achieve.12,18,19 The use of oxaliplatin has been associated with the development of hepatic sinusoidal obstruction,20 and a recent study by Fernandez et al. of 37 patients demonstrated steatohepatitis after the preoperative administration of irinotecan or oxaliplatin, particularly in the obese.21 A structural parenchymal change and a higher postoperative complication rate compared with patients receiving no chemotherapy have been noted in patients who have received locoregional chemotherapy. Hepatic arterial infusion of floxuridine has been shown to cause acute hepatitis and dose-related hepatocyte necrosis, steatosis, micronodular cirrhosis, and portal triad fibrosis that can be fatal.22–24 Elias et al. described hepatectomy following this treatment as more difficult, with elevated intrahepatic venous pressure and an unusually high blood loss. They reported 10 postoperative complications in 8 patients, although there were no deaths.25
There are few studies analyzing the effect of preoperative systemic chemotherapy on the perioperative outcome of liver resection and only one related to the use of oxaliplatin. A prospective study of 35 patients conducted in 2000 suggested that preoperative systemic 5FU/FA did not increase hospital morbidity and mortality after liver resection.19 A retrospective study by Tanaka et al. demonstrated no difference in median blood transfusion volume in patients undergoing major hepatectomy after neoadjuvant oxaliplatin chemotherapy for five or more bilobar metastases (627.1 ml versus 612.2 ml in the no-neoadjuvant group). The median hospital stay was shorter in patients who had neoadjuvant chemotherapy (13.2 days versus 19.9 days, P = 0.03), and the complication rate was the same.18 Direct comparison of the differences in hospital stay was difficult as the study involved two departments in different health insurance systems. Adam et al. reported that preoperative FOLFOX increased the risk of operative bleeding due to vascular changes, but it was not associated with an increase in surgical morbidity or mortality.26 There have been no reports of the analysis of individual clinical variables showing the outcome of liver resection in relation to patients’ operative chemotherapy status in a large number of patients, however.
The present study therefore examined a large cohort of patients undergoing liver resection for colorectal metastases and related preoperative, intraoperative, and postoperative outcome variables (both in-hospital and long term) with the prior use of systemic chemotherapy.
PATIENTS AND METHODS
Patient Demographics
A retrospective study of the clinical records of 101 consecutive patients who had undergone hepatectomy for colorectal liver metastases was undertaken. The operations were carried out between May 1999 and September 2003 within the departments of Hepatobiliary Surgery at The Royal Free (n = 86) and The Royal London (n = 15) Hospitals, London, UK. All patients who underwent hepatectomy for colorectal metastases were included, and none had concomitant extrahepatic disease.
Demographic data were collected including age, sex, and preoperative comorbidity, including alcohol intake (units/week), smoking history (cigarettes/day), and the presence of pre-existing liver disease. The site and Dukes stage of the colorectal primary tumor were recorded, as were the presence of synchronous metastases and the number of tumor deposits found during pathological analysis of the resected liver specimen. The pre-hepatectomy chemotherapy status of the patient was recorded and grouped into neoadjuvant (given between the diagnosis of the liver metastasis and hepatectomy), adjuvant (following colorectal cancer resection), or no chemotherapy. The chemotherapy drugs and treatment duration were noted, as was the use of preoperative portal vein embolization (PVE).
Liver function immediately prior to surgery was noted. This included measurements of serum albumin, bilirubin, aspartate transaminase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), lactate dehydrogenase (LDH), and International Normalized Ratio (INR), as well as the tumor markers CEA and CA19-9.
Hepatectomy
Preoperative PVE was used selectively in patients with an anticipated future liver remnant (FLR) of < 30% of the total tumor free liver parenchyma as measured by magnetic resonance volumetry. Parenchymal dissection was carried out with an ultrasonic surgical aspirator (CUSA ExcelTM, Valleylab, Boulder, CO, USA) after division of the hilar structures. Hilar inflow occlusion (Pringle maneuver) was used in cases where there was significant parenchymal blood loss.
Operative data included the duration of surgery, blood loss, the operative transfusion of blood and blood products, and the inflow occlusion time if the Pringle maneuver was used. The duration of stay on the intensive care unit (ITU) or surgical high dependency unit (SHDU) and overall hospital stay were noted. Comments from the operation note as to the nature of the parenchyma and difficulty of surgery were also recorded.
Liver Parenchymal Histopathology
Part of the routine dissection protocol of the resection specimen within the Department of Histopathology included a sample of normal liver parenchyma, approximately 1 cm3, as far away from the main tumor bulk as possible. Once removed, the tissue was fixed in formalin and embedded in paraffin wax. These specimens were then cut and stained with hematoxylin and eosin, and a report made by the histopathologist documenting the histological features identified in these specimens. These reports were examined in the study. Note was made of any abnormalities of the background liver that had been recorded, as well as their degree and type, and they were then compared with the subjective assessment of the liver substance made by the operating surgeon.
Postoperative Outcome
Postoperative morbidity was considered in detail. Complications were divided into major (those that resulted in delayed discharge from or readmission to ITU or SHDU, or reoperation); and minor (resulting in delayed discharge from hospital only) and grouped according to the systems affected. Cardiovascular complications included newly diagnosed atrial fibrillation, myocardial infarction or ischemia, congestive cardiac failure, pulmonary embolism, or cardiovascular collapse requiring inotropic support. Respiratory complications included respiratory failure (major if requiring mechanical ventilation or continuous positive airway pressure [CPAP]), pleural effusions, pneumothorax, or respiratory tract infection.
Renal complications included acute renal failure (major if requiring renal replacement therapy), urinary retention, or urinary tract infection. Hepatic complications were recorded when there was an acute deterioration in liver function tests with signs of hepatic failure or encephalopathy.
Septic episodes were confirmed with positive microbiological cultures (major if showing signs of systemic sepsis), and multiple organ failure (MOF) was diagnosed as two or more organ systems failing with the patient being treated on ITU or SHDU. The number and type of postoperative endoscopic and radiological interventions performed were also noted.
Long-term Outcome
After discharge, patients were followed up on a 3-monthly basis. Details of the patients’ clinical status on a specified date were then obtained. This was achieved by the retrospective analysis of the hospital notes or outpatient clinic records, or by direct contact with the general practitioner. If the patient had died in the period since surgery, the date of death was noted and the number of months of postoperative survival was calculated. Surviving patients were divided into one of two groups: those with recurrence of the tumor (with the site noted) and those without recurrence. From these data, overall and disease-free survival post-hepatectomy was determined for this series. Patients were then divided into one of four groups according to their preoperative chemotherapy status. The first classification was of patients receiving neoadjuvant chemotherapy and the second was of patients who did not receive neoadjuvant chemotherapy. There were two groups in each classification: group 1 (NA Ox), patients who had received neoadjuvant oxaliplatin and 5FU/FA, and group 2 (NA 5FU), patients who had received neoadjuvant 5FU/FA alone; group 3 (AD 5FU), patients who had received adjuvant 5FU/FA after their initial colorectal resection, but no prehepatectomy chemotherapy, and group 4 (None), patients who had received no chemotherapy at all, either after the initial colorectal resection or pre-hepatectomy.
Statistical Analysis
Data were entered directly into a specifically designed Microsoft Access database and analyzed using a combination of proprietary statistical software packages (Microsoft Excel, GraphPad Prism 4, and SPSS for Windows). Categorical variables were compared between groups using the chi-square test, and quantitative variables were compared with the Kruskal-Wallis test for multiple groupings. Survival rates were calculated according to the Kaplan-Meier actuarial technique and curve comparison using the logrank test. Significance was assumed when P < 0.05.
RESULTS
Demographic and Preoperative Data
Of the 101 patients included in the study, 46 had undergone neoadjuvant chemotherapy, 25 with oxaliplatin + 5FU/FA and 21 with 5FU/FA alone. Fifty-five patients had no neoadjuvant chemotherapy, 34 receiving 5FU/FA after the original colorectal resection, and 21 patients receiving no chemotherapy.
Table 1 shows demographic data. The groups were well matched for age, sex, and site of colorectal primary with greater than 60% of tumors originating in either the sigmoid colon or the rectum. Neoadjuvant chemotherapy had been given as part of a strategy to downstage disease and to facilitate resection in 7 patients who underwent PVE. The remaining 39 patients received chemotherapy for resectable metastases.
There were significantly higher numbers of patients with synchronous metastases who received neoadjuvant chemotherapy (24/46, 52%) than in the no neoadjuvant groups (8/55, 14.5%; P < 0.001). There was also a significantly higher number of metastases in the neoadjuvant groups (median 2, range 1–8, versus median 1, range 1–5; P = 0.019). The majority of patients underwent major liver resections, with over half undergoing right or extended right hepatectomy. There were more multiple segmentectomies in the neoadjuvant than in the no neoadjuvant groups, although this difference was not statistically significant (11/46, 24% versus 6/55, 11%; P = 0.08). The patients who underwent resection after PVE over this time period had all received neoadjuvant chemotherapy.
Comorbidity is shown in Table 2. As would be expected, patient selection resulted in a low incidence of severe comorbid disease that was equally distributed between the groups. There were no significant differences between the number of patients within each group who had a preoperative morbidity (P = 0.2). No patient had pre-existing liver disease, and alcohol intake was moderate. The morbidities were mainly cardiovascular in nature, with hypertension the most frequent. There were a higher number of patients on anticoagulant therapy in the neoadjuvant groups that reflected the presence of indwelling venous catheters used for the chemotherapy; anticoagulation, however, was discontinued, and coagulopathy was corrected in all cases prior to surgery.
Liver function tests taken on the day before the operation and results of the preoperative tumor marker profiles CEA and CA 19-9 are shown in Table 3. There were no significant differences in the groups, although the median values of GGT in the two neoadjuvant groups and the no-chemotherapy groups were above the normal range (56, 48.5, 36 U/l, respectively) as was the LDH level in the NA Ox group (499 U/l). Median values of CEA were above normal in all groups.
Chemotherapy Durations and Regimens (Values Marked with an Asterisk are Median)
Neoadjuvant oxaliplatin + 5FU/FA group
Of the 25 patients within the neoadjuvant OX + 5FU/FA group, 20 (80%) had also received adjuvant chemotherapy with 5FU/FA after their initial colorectal resection (6* cycles, range 1–16) with 1 patient also receiving irinotecan. After diagnosis of the liver metastases, these patients underwent 6* cycles of neoadjuvant chemotherapy (range 3–12 cycles) that was stopped 64* days prior to surgery (range 11–240 days). In 3 patients (12%) the treatment was stopped early because they developed peripheral sensory neuropathy. One of the 3 was changed to tomudex. The dosage regimen was modified according to the individual patient and the preference of the oncologist, but it was based on a schedule consisting of oxaliplatin given as a 2-h infusion (85 mg/m2) followed by 5FU (400 mg/m2 bolus, 600 mg/m2, 22-h continuous infusion), and folinic acid (200 mg/m2, 2-h infusion) repeated on consecutive days.
Neoadjuvant 5FU/FA Group
Seventeen (81%) of the neoadjuvant 5FU/FA patients had undergone adjuvant chemotherapy with 5FU/FA for 6* cycles (range 2–30) after the initial colorectal resection. After diagnosis of the metastases, neoadjuvant 5FU/FA therapy was given for 6* cycles (range 2–30) and was stopped 58* days prior to surgery (range 20–250).
Adjuvant 5FU/FA Group
Patients receiving adjuvant 5FU/FA underwent 12* cycles of chemotherapy (range 1–30) after their initial colorectal resection. None of these patients were diagnosed with metastatic disease during this period of adjuvant chemotherapy.
Operative Data
Operative outcome data are represented in Figure 1. The overall median duration of surgery was 7 h (range: 2–14.5 h), blood loss 2 l (range 0–27 l), blood transfusion 2 units (range 0–40 units), and blood product transfusion 2 units (range 0–20 units). Nineteen patients required hilar inflow occlusion (2 patients in the NA Ox group (median duration 40.5 min, range 36–45 min); 6 in the NA 5FU group (median 41 min, range 12–77 min); 9 in the AD 5FU group (median 25 min, range 15–69 min), and 2 patients in the no-chemotherapy group (median 26 min, range 25–27 min). These differences were not statistically significant (P = 0.6). Comparison of the operative end points between the four groups showed no significant differences.
Operative data represented using box-and-whiskers plots, grouped and compared in the four patient chemotherapy groups. a. Operation duration (P = 0.6†) b. Estimated blood loss (P = 0.5). c. Operative blood transfusion (P = 0.5). d. Operative blood product transfusion (P = 0.3). The box length of the box-and-whisker plots represents the interquartile range that contains the median value shown as a horizontal line. The whiskers represent the 95% confidence intervals. †Kruskal-Wallis test.
The subjective assessment of the difficulty of dissection and the quality of the parenchyma made by the operating surgeon showed inter-group variation. Abnormal parenchymal appearance and difficulty in division of the parenchyma was noted in 8 patients in the NA Ox group (32%), 6 in the NA 5FU group (28%), 5 of the AD 5FU group (15%), and 2 patients in the no-chemotherapy group (9.5%). These subjective differences were significant (P = 0.03). If the patients were grouped into those receiving neoadjuvant chemotherapy (NA Ox and NA 5FU), or not (AD 5FU and None), a significant difference was again seen. Fourteen of 46 (30%) who had received neoadjuvant therapy were noted to have abnormal parenchyma compared with 7 of 55 (13%) in the no-neoadjuvant therapy group (P = 0.03).
Histopathology
The routine histopathological reports of the nature of the background liver parenchyma of 91 patients were obtained and examined. Results from the remaining 10 patients were either unavailable, or staining had not been carried out. Sixty-two patients (68%) had reports indicating abnormal liver parenchyma, with 29 (32%) reports documenting either normal parenchyma or no comment made. There was an equal distribution of the number of abnormal reports made between the chemotherapy groups (17/23 (74%) in the NA Ox group; 12/18 (67%) in the NA 5FU group; 23/32 (72%) in the AD 5FU group; and 10/18 (56%) in the no-chemotherapy group [P = 0.6]).
The reports were broken down further, and individual fat and inflammation scores were noted. Where the grade of steatosis or inflammation was not specified, it was included in the mild category. There was an equal distribution of these reported abnormalities between the four groups, with the majority being mild. Moderate or severe steatosis was noted in 3 specimens from the NA OX group (13%), 3 in the NA 5FU group (17%), 3 in the AD 5FU group (9%), and 2 in the no-chemotherapy group (11%) (P = 0.9). There were only 2 cases of severe steatosis noted, with one each in the neoadjuvant chemotherapy groups. No cases of severe inflammatory change were noted by the histopathologists.
Comments of increased fat content of the liver were made by the surgeon in 9 (9%) cases as opposed to 45 (49%) by the pathologist in the report. There was, however, good correlation between the surgeons and the pathologists scoring, as in only one case was the liver described as fatty by the surgeon and subsequently judged as showing no signs of steatosis by the pathologist. Abnormalities of perfusion or congestion were noted in 7 cases by the surgeon (7%), and 11 cases of parenchymal friability were noted.
Hospital Outcome
The median length of stay on ITU or SHDU was 2 days (range 1–24 days) and the majority of patients were discharged from hospital on postoperative day 14 (range 7–49 days). There were no significant differences in the durations of stay between the four groups (Figure 2a–b).
Hospital outcome data represented using box-and-whiskers plots, grouped and compared in the four patient chemotherapy groups. a. Length of stay on ITU/SHDU (P = 0.7†). b. Length of hospital stay (P = 0.4). The box length of the box-and-whisker plots represents the interquartile range that contains the median value shown as a horizontal line. The whiskers represent the 95% confidence intervals. †Kruskal-Wallis Test.
Twenty-three patients (7 in the neoadjuvant groups and 16 in the no neoadjuvant groups) underwent 45 separate radiological or endoscopic interventions in the recovery period. These included percutaneous drainage of pleural, subphrenic, and intra-abdominal fluid collections; endoscopic retrograde cholangiopancreatography (ERCP), and chest drain insertion for pneumothorax. These differences were not statistically significant (P = 0.3).
A total of 37 patients (37%) developed 53 separate postoperative complications (Table 4). Of these 53 complications, 33 (62%) were classified as minor. There were no significant differences demonstrated between the number of patients within each group developing complications (P = 0.5) or the number of complications per patient within the groups (P = 0.8). The type and severity of complication were comparable, the most common being respiratory disorders, most of which were minor, although 9 patients required respiratory support on ITU or SHDU postoperatively. Hospital mortality was 3.9% and this also showed no significant inter-group variation (Table 1).
Four patients died in the hospital, two of them from the NA OX group. The first patient in this group bled from an intraoperative IVC tear that was repaired but required a massive blood transfusion. The patient subsequently deteriorated on ITU with acute respiratory distress syndrome (ARDS), acute renal failure, and subsequent Gram-negative septicemia, and died of multiple organ failure on postoperative day 7. The second patient developed an acute deterioration in liver function on ITU following an extended right hepatectomy. Encephalopathy developed and was followed by acute renal and respiratory failure. The patient died of cardiovascular and respiratory failure on postoperative day 16.
One patient died in each of the non-neoadjuvant groups. The first patient developed an infected intra-abdominal fluid collection, and attempts at radiological guided drainage were unsuccessful. Re-laparotomy was required on day 13, after the patient developed a secondary hemorrhage. Overwhelming sepsis required increasing doses of inotropes, and the patient died of septic shock on postoperative day 15. The second patient died after a portal vein injury that required an extensive intraoperative blood transfusion. The patient subsequently underwent re-laparotomy for continued hemorrhage within 24 h. Both ARDS and acute renal failure developed, and the patient died of multiple organ failure 22 days after the initial operation.
Long-term Outcome
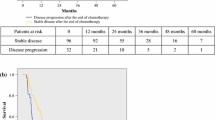
Long-term outcome data were obtained in 87 patients. They were grouped according to whether they had received neoadjuvant chemotherapy (n = 42), or not (n = 45). Information on the remaining 10 patients was not obtained as the clinical records were unavailable or information from a general practitioner not supplied. Median follow-up was 23 months (range 6–54 months). Overall survival at 1 and 3 years was 93% and 71%, respectively. Survival without recurrence at the same time points was 91% and 40% with a median disease-free survival of 29 months (Figure 3a). Of the 47 patients with recurrent disease, 40 had metastasis to the liver, with only 7 having single-site extrahepatic metastases.
Long-term outcome data. a. Postoperative survival (overall and disease-free (P = 0.0005). b. Overall survival (P = 0.04). c. Disease-free survival (P = 0.14). d. Overall survival, synchronous metastases (P = 0.12). Patients are grouped according to their chemotherapy status (either neoadjuvant [NA], no neoadjuvant chemotherapy [No NA], or tumor stage at presentation (either synchronous or metachronous). Survival end points are either overall or disease-free (DFS). Curve comparison and P value obtained using logrank test.
Overall survival of the patients who had received no neoadjuvant chemotherapy was significantly better than those in the neoadjuvant groups (3-year survival of 80% versus 62%, P = 0.04) (Figure 3b). Disease-free survival comparison, however, showed no difference, with a median time to recurrence of 25 months in the neoadjuvant versus 34 months in the no-neoadjuvant groups (Figure 3c).
There were no deaths on follow-up of the 8 patients with synchronous metastases who had not received neoadjuvant chemotherapy, whereas 4/19 (21%) of patients in the neoadjuvant therapy group with synchronous metastases died within the same time period (Figure 3d). This difference was not statistically significant (P = 0.12).
DISCUSSION
Preoperative chemotherapy is being used more and more often in patients with resectable colorectal metastases either on a neoadjuvant basis as a part of clinical trials27 or for downstaging unresectable disease.12 As a consequence, operating on patients who have been pre-exposed to systemic chemotherapy is becoming increasingly common.28 Some studies suggest a change in the liver parenchyma following chemotherapy and use of the term “post-chemotherapy liver” is becoming more widespread. In the study by Parc et al., the liver parenchyma was judged at the time of liver resection to be abnormal by the surgeon in 7 of 17 cases (41%) following chemotherapy, as opposed to 3 of 18 (17%) in the non-chemotherapy group.19 Livers subjected to prolonged chemotherapy have also been noted to be more fragile and hemorrhagic.12 The study by Fernandez et al. demonstrated an increased risk of severe steatohepatitis associated with irinotecan and oxaliplatin chemotherapy (although only four patients had received oxaliplatin alone), and suggested that this may affect the hepatic reserve and the percentage of the liver volume that can be safely resected.21 Interim safety results of 346 patients enrolled into the EORTC randomized phase III study comparing preoperative chemotherapy with FOLFOX 4 with surgery alone were reported in abstract form in the 2005 ASCO Annual Meeting.29 Surgical morbidity and mortality rates were low although there were more episodes of transient liver failure, wound and intra-abdominal infections in the chemotherapy group. Survival data are expected in 2007. These data when published however will only give the perioperative risk for one chemotherapy group in comparison to control. To date there have been no studies that have specifically investigated hospital and long term clinical outcomes in a large number of patients who have received chemotherapy immediately prior to liver resection. It is vital therefore that any potentially negative impacts of neoadjuvant chemotherapy on the short- or long-term outcomes of liver resection are established.
The patients in this study were well matched for age, sex and comorbidity. Patients in the neoadjuvant groups had more advanced disease. They had a higher number of metastases and were more likely to have synchronous tumors at diagnosis. Chemotherapy was given to all patients undergoing PVE, as venous embolization can stimulate cancer growth in both the embolized and non-embolized liver lobe.30,31 As PVE is a further approach for downstaging unresectable tumors, 32 these patients often have large-volume disease that is associated with their poorer long-term survival following resection.5
An underlying abnormality in liver function preoperatively was suggested by the liver function tests. The levels of GGT were above normal in the two neoadjuvant and the no chemotherapy groups. The LDH level was elevated in the NA Ox group although all other median values lay within normal limits. Routine liver function tests however are relatively crude measures of hepatic function. The elevated gamma-glutamyl transpeptidase (GGT) reflects a mild derangement in biliary excretion that was found in both the chemotherapy and no-chemotherapy groups any may therefore be due to the liver metastases. The elevated lactate dehydrogenase (LDH) reflected hepatocyte damage with chemotherapy but may be minimal as aspartate transaminase (AST) and alanine aminotransferase (ALT) levels were within the normal ranges. Oxaliplatin is not metabolized in the liver, but it has been shown to cause limited effects on liver function tests,24 unlike other platinum agents that can cause significant dose-related hepatotoxicity.33,34 Only rarely has 5FU been implicated in causing hepatotoxicity when it is given intravenously, even though the liver plays a key role in its catabolism.35 It is therefore unlikely that these systemic drugs would give rise to abnormal liver function tests, especially when the length of time that had passed since the last dose of chemotherapy is taken into account (median of 64 and 58 days in the two neoadjuvant groups).
The operative mortality, overall blood loss, and transfusion requirements documented in this study are comparable to those from other series. Reported operative mortality rates vary from 0%–8%, and postoperative morbidity rates of 10%–50% have been described.1,8,9,36,37 This compares with 3.9% mortality and 37% overall morbidity in the present study. An overall median blood loss of 1,000 ml was reported in 100 consecutive hepatectomies by Cunningham et al., with blood transfusion required in 59%. The patients were also found to be more likely to need transfusion if they underwent major hepatectomy.38 Other studies have described median blood losses of between 645 ml and 3,400 ml,9,39 with median transfusion requirements ranging from 0.9 to 8 units.39,40 Overall median blood loss in this study was 2,000 ml, with a blood and blood product transfusion requirement of median 2 U per patient. Most patients stay in hospital for 10–13 days postoperatively,36 which compares with median 14 days in the present study. This study also demonstrated that the duration of operation, blood loss volume, and intraoperative transfusion requirements were not significantly increased in patients who had received neoadjuvant chemotherapy. The duration of high dependency or intensive care support, as well as the number of complications suffered and postoperative procedures performed, and the overall hospital length of stay were similar to patients who had not received chemotherapy.
The histological reports described abnormal background liver parenchyma in 68% of specimens. Most of these reports, however, described only mild to moderate features of steatosis and inflammation, and they were descriptive and inaccurate measures of the degree of abnormality. The pathologists were making a quick subjective assessment of the parenchyma to determine any gross features of underlying liver disease that may have had an impact on the clinical recovery of the patient or their further treatment. Different pathologists of varying experience graded these changes, and there was no structured scoring system in place.
Comments made by the operating surgeon about the nature of the liver tissue were similarly subjective and prone to observer error, as there was no obligation of the surgeon to comment on the parenchyma. It may have been that in some cases, patients with an abnormal macroscopic parenchyma at operation had no comment made by the surgeon in the notes as it was not thought to be a significant finding. There were different surgeons operating and writing the notes, and that may have led to interobserver error. Each surgeon was also aware of the chemotherapy status of the patient on whom they were operating; hence perceived steatosis and parenchymal friability may have been attributed inappropriately to chemotherapy. Despite these shortcomings, there remained a perceived surgical difference in the nature of the background liver following chemotherapy that was similar to previous observation.12,19
Overall 5-year survival of patients following hepatectomy for colorectal liver metastases has been reported up to 47%,4 although most studies report survival rates of 25%–32%.1–4 Survival up to 10 years has also been documented in up to 26% of patients.2,6 Five-year survival information was not available on our data set, although a 3-year survival of 71% may be better than that from other studies (55%4 and 44%3).
The poorer long-term survival of the patients receiving neoadjuvant chemotherapy may be related to the more advanced nature of the disease in these patients. They had significantly higher numbers of metastases, and more of them had synchronous lesions at presentation than the patients who had not received preoperative chemotherapy. Both of these factors are associated with a poorer long-term outlook.5 As the overall survival of the NA chemotherapy patients was significantly less than for those with no NA chemotherapy, although the disease-free survival was similar, it is likely that the outcome of patients developing recurrence who had previously received oxaliplatin was reduced. This difference may be related to the chemosensitivity that develops with repeated administration, the objective responses to failed second-line chemotherapy being low.41
This study demonstrated no disadvantages related to the use of preoperative systemic oxaliplatin and 5FU-based chemotherapy in terms of operative or hospital outcome, when compared with patients who had not received this treatment. Long-term survival was poorer in patients who had received neoadjuvant chemotherapy, and this may be attributed to the more advanced nature of their disease at presentation. This study would suggest that the administration of 5FU and oxaliplatin chemotherapy prior to liver resection does not increase morbidity, mortality, or hospital stay.
References
Adson MA, van Heerden JA, Adson MH, et al. Resection of hepatic metastases from colorectal cancer. Arch Surg 1984;119:647–651
Scheele J, Stang R, Altendorf-Hofmann A, et al. Resection of colorectal liver metastases. World J Surg 1995;19:59–71
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Française de Chirurgie. Cancer 1996;77:1254–1262
Nagashima I, Oka T, Hamada C, et al. Histopathological prognostic factors influencing long-term prognosis after surgical resection for hepatic metastases from colorectal cancer. Am J Gastroenterol 1999;94:739–743
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 1999;230:309–318
Minagawa M, Makuuchi M, Torzilli G, et al. Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg 2000;231:487–499
Scheele J, Stangl R, Altendorf-Hofmann A. Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br J Surg 1990;77:1241–1246
Gayowski TJ, Iwatsuki S, Madariaga JR, et al. Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery 1994;116:703–710
Holm A, Bradley E, Aldrete JS. Hepatic resection of metastasis from colorectal carcinoma. Morbidity, mortality, and pattern of recurrence. Ann Surg 1989;209:428–434
Scheele J. Hepatectomy for liver metastases. Br J Surg 1993;80:274–276
Fusai G, Davidson BR. Strategies to increase the resectability of liver metastases from colorectal cancer. Dig Surg 2003;20:481–496
Bismuth H, Adam R, Levi F, et al. Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg 1996;224:509–520
Bismuth H, Adam R. Reduction of nonresectable liver metastasis from colorectal cancer after oxaliplatin chemotherapy. Semin Oncol 1998;25:40–46
Pozzo C, Basso M, Cassano A, et al. Neoadjuvant treatment of unresectable liver disease with irinotecan and 5-fluorouracil plus folinic acid in colorectal cancer patients. Ann Oncol 2004;15:933–939
de Gramont A, Figer A, Seymour M, et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 2000;18:2938–2947
Adam R, Avisar E, Ariche A, et al. Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal cancer. Ann Surg Oncol 2001;8:347–353
Giacchetti S, Itzhaki M, Gruia G, et al. Long-term survival of patients with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgery. Ann Oncol 1999;10:663–669
Tanaka K, Adam R, Shimada H, et al. Role of neoadjuvant chemotherapy in the treatment of multiple colorectal metastases to the liver. Br J Surg 2003;90:963–969
Parc Y, Dugue L, Farges O, et al. Preoperative systemic 5-fluorouracil does not increase the risk of liver resection. Hepatogastroenterology 2000;47:1703–1705
Rubbia-Brandt L, Mentha G, Terris B. Sinusoidal obstruction syndrome is a major feature of hepatic lesions associated with oxaliplatin neoadjuvant chemotherapy for liver colorectal metastases. J Am Coll Surg 2006;202:199–200
Fernandez FG, Ritter J, Goodwin JW, et al. Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg 2005;200:845–853
Doria MI Jr, Shepard KV, Levin B, et al. Liver pathology following hepatic arterial infusion chemotherapy. Hepatic toxicity with FUDR. Cancer 1986;58:855–861
Shepard KV, Levin B, Faintuch J, et al. Hepatitis in patients receiving intraarterial chemotherapy for metastatic colorectal carcinoma. Am J Clin Oncol 1987;10:36–40
Pettavel J, Gardiol D, Bergier N, et al. Fatal liver cirrhosis associated with long-term arterial infusion of floxuridine. Lancet 1986;2:1162–1163
Elias D, Lasser P, Rougier P, et al. Frequency, technical aspects, results, and indications of major hepatectomy after prolonged intra-arterial hepatic chemotherapy for initially unresectable hepatic tumors. J Am Coll Surg 1995;180:213–219
Adam, R., Sebagh, M., Plasse, M. Impact of pre-operative systemic chemotherapy on liver histology and outcome of hepatic resection for colorectal cancer liver metastases (CRLM). J Clin Oncol 2005; 23(253S suppl 16, abstr 3529)
Fusai G, Davidson BR. Management of colorectal liver metastases. Colorectal Dis 2003;5:2–23
Bilchik AJ, Poston G, Curley SA, et al. Neoadjuvant chemotherapy for metastatic colon cancer: a cautionary note. J Clin Oncol 2005;23:9073–9078
Nordlinger, B, Sorbye, H, Debois, M, et al. Feasibility and risks of pre-operative chemotherapy (CT) with FOLFOX 4 and surgery for resectable colorectal cancer liver metastases (LM). Interim results of the EORTC Intergroup Randomised Phase III Study 40983. 2005 ASCO Annual Meeting Proceedings. J Clin Oncol 2005;23(16S, Part I of II, abstract 3528)
Kokudo N, Tada K, Seki M, et al. Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology 2001;34:267–272
Elias D, de Baere T, Roche A, et al. During liver regeneration following right portal embolization the growth rate of liver metastases is more rapid than that of the liver parenchyma. Br J Surg 1999;86:784–788
Azoulay D, Castaing D, Smail A, et al. Resection of nonresectable liver metastases from colorectal cancer after percutaneous portal vein embolization. Ann Surg 2000;231:480–486
Armand JP, Boige V, Raymond E, et al. Oxaliplatin in colorectal cancer: an overview. Semin Oncol 2000;27:96–104
Pollera CF, Ameglio F, Nardi M, et al. Cisplatin-induced hepatic toxicity. J Clin Oncol 1987;5:318–319
King PD, Perry MC. Hepatotoxicity of chemotherapy. Oncologist 2001;6:162–176
Doci R, Gennari L, Bignami P, et al. Morbidity and mortality after hepatic resection of metastases from colorectal cancer. Br J Surg 1995;82:377–381
Steele G Jr, Bleday R, Mayer RJ, et al. A prospective evaluation of hepatic resection for colorectal carcinoma metastases to the liver: Gastrointestinal Tumor Study Group Protocol 6584. J Clin Oncol 1991;9:1105–1112
Cunningham JD, Fong Y, Shriver C, et al. One hundred consecutive hepatic resections. Blood loss, transfusion, and operative technique. Arch Surg 1994;129:1050–1056
Melendez JA, Arslan V, Fischer ME, et al. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 1998;187:620–625
Delva E, Camus Y, Nordlinger B, et al. Vascular occlusions for liver resections. Operative management and tolerance to hepatic ischemia: 142 cases. Ann Surg 1989;209:211–218
Tournigand C, Andre T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 2004;22:229–237
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hewes, J.C., Dighe, S., Morris, R.W. et al. Preoperative Chemotherapy and the Outcome of Liver Resection for Colorectal Metastases. World J. Surg. 31, 353–364 (2007). https://doi.org/10.1007/s00268-006-0103-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-006-0103-8