Abstract
Background
In recent years, total or near-total thyroidectomy has emerged as a surgical option to treat patients with multinodular goiter, especially in endemic iodine-deficient regions. The aim of this study was to compare the complication rates of total and near-total thyroidectomy in multinodular goiter and the incidence of thyroid cancer requiring radioactive iodine ablation and completion thyroidectomy between groups.
Study design
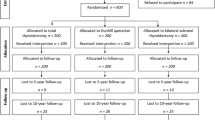
Patients with euthyroid multinodular goiter without any preoperative suspicion of malignancy, history of familial thyroid cancer, or previous exposure to radiation were randomized (according to a random table) to total thyroidectomy (group 1, n = 104) and near-total thyroidectomy leaving less than 2 g (group 2, n = 112).
Results
There were no persistent complications. The incidence of transient hypoparathyroidism in group 1 (26%) was significantly higher than in group 2 (9.8%) (p < 0.001). The rate of asymptomatic hypocalcemia in group 2 (7.4%) was lower than in group 1 (27%) (p < 0.001). The incidence of papillary cancer was 9.6% in group 1 and 12.5% in group 2 (p > 0.05). None of the patients underwent completion thyroidectomy before ablative therapy. Ten patients were found to have the histological criteria for radioactive iodine ablation. Of these 10 patients, four were in group 1 and six were in group 2 (p > 0.05).
Conclusion
In conclusion, we recommend near-total thyroidectomy in multinodular goiter instead of total or subtotal thyroidectomy. While near-total thyroidectomy and total thyroidectomy obviate the need for completion thyroidectomy in incidentally found thyroid cancer, and while there is no difference in the rate of recurrent laryngeal nerve palsy between the two methods, near-total thyroidectomy causes a significantly lower rate of hypoparathyroidism compared to total thyroidectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thyroidectomy is one of the most frequent operations performed in iodine-deficient regions [1, 2]. The surgical treatment of multinodular thyroid disease remains controversial, but in recent years total thyroidectomy (TT) or near-total thyroidectomy (NTT) has emerged as a surgical option to treat patients with multinodular goiter especially in endemic iodine-deficient regions [2–5]. The goal of surgical treatment in thyroid disease should be to eliminate the disease with low complication rates and to minimize reoperation for incidental thyroid cancer in multinodular goiter [1, 2, 6].
The main postoperative complications are recurrent laryngeal nerve (RLN) palsy and hypoparathyroidism. Even experienced surgeons report inadvertent injury to the nerve and persistent RLN palsy in about 1–2% of patients [7–13]. In several studies, the incidence of hypoparathyroidism varied from 1.6 to above 50%. The etiologic factor of hypoparathyroidism is the iatrogenic surgical trauma to parathyroid glands, extent of surgery, the experience of the surgeon, and the number of functioning glands left behind [13–15].
The aim of this study was to compare the complication rates of TT and NTT in multinodular goiter and the incidence of thyroid cancer requiring radioactive iodine (RAI) ablation and completion thyroidectomy in TT and NTT.
Subjects and methods
Patients
From September 2003 to September 2005, a total of 216 consecutive patients with nontoxic multinodular goiter underwent TT or NTT. The patients’ data were collected prospectively. Patients were selected according to the number on the random table for two different extensions of surgical procedures. Two hundred eighteen patients with multinodular goiter were included in the study. The patients were divided into two groups according to the surgical procedure performed: bilateral TT (group 1, n = 104) and NTT (group 2, n = 112).
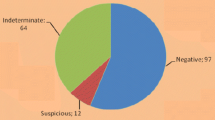
The indications for surgery were large goiter with compression effect in all patients. All of the patients were evaluated by physical examination, thyroid function tests, thyroid ultrasonography (US), and thyroid scan. US-guided biopsy was routinely employed for nodules greater than 1.5 cm in diameter whether palpated or not. Fine-needle aspiration biopsy (FNAB) was performed for nodules <1 cm when US indicated suspicious findings (i.e., hypoechoic nodule in association with punctate calcifications and/or intranodular vascularity and/or irregular borders). In all patients, thyroid scanning and US revealed multinodular goiter with or without a dominant nodule. All patients were euthyroid and had no history of hyperthyroidism, radiation exposure, or familial thyroid cancer. Any patient with preoperative or perioperative suspicion of malignancy was excluded. The study plan was reviewed and approved by our institutional ethical committee, and informed consent was obtained for all patients.
The evaluation of RLN palsy and hypoparathyroidism
Direct laryngoscopic examination was used to evaluate vocal cord motility before and after surgery in all patients. Postoperative cord palsy was defined as the presence of an immobile vocal cord or decreased movement of the vocal cord during phonation. Laryngoscopy was also performed 1 and 6 months later in case of disphonia with vocal cord injury. Permanent vocal cord palsy is defined as persistent dysfunction and clinical dysphonia lasting for more than 6 months postoperatively.
Hypocalcemia was defined as a serum calcium level less than 8 mg/dl after operation. The presence of clinical symptoms or signs of hypocalcemia was reported and included facial paresthesia, positive Chvostek’s or Trousseau’s signs, and muscular spasm. Persistent hypoparathyroidism was defined as serum parathyroid hormone levels below 10 pg/mL in patients requiring treatment to maintain calcemia for more than 3 months. All of the patients were followed-up until February 2006.
Operative technique
All patients were operated on by four experienced endocrine surgeons (S. Özarmağan, A. Bozbora, Y. Erbil, and U. Barbaros). TT was performed by extracapsular dissection. NTT was performed by the capsular dissection method, leaving less than 1 g of remnant tissue around the Berry ligament. In our clinic, NTT was performed in two ways. In case of the presence of a dominant nodule, lobectomy was performed on the lobe containing the nodule and near-total resection was performed on the conralateral lobe. In the absence of a dominant nodule and in patients with multiple nodules in both lobes, bilateral NTT was performed. The total amount of remnant thyroid tissue was intended to be none in group 1 and less than 1 g in group 2. The amount of remnant tissue was estimated as 1 cm3 equals 1 g.
RLN and parathyroid identification
Identification of the RLN was performed during all thyroid operations. Our surgical approach to identify the nerve is to search for the point where it crosses the inferior thyroid artery. The artery and the middle thyroid vein and its branches are ligated and the lobe is retracted medially. Then, the cricothyroid joint and tracheosophageal groove are searched.
The observation and preservation of all parathyroid glands were tried. The number of parathyroid glands observed was noted. For this reason, all vessels were ligated close to the thyroid gland, especially the branches of the inferior thyroid artery. When the parathyroid gland was damaged it was autotransplanted into the sternocleidomastoid muscle.
Histological criteria for RAI therapy
Histological criteria for RAI therapy included a tumor size greater than 1.5 cm, any size of tumor with thyroid capsule or extrathyroidal invasion, or multicentricity (two tumor foci). The departments of general surgery and endocrinology collaborate to conduct the treatment of patients with thyroid cancer at our institute. The histological criteria for postoperative RAI ablation [100 mCi (3,700 MBq)] was established as a result of this cooperative work and has been our policy for the past two decades. The thyroid-stimulating hormone (TSH) values were required to be more than 30 mIU/L to refer the patient to RAI ablation therapy.
Amount of remnant thyroid tissue
Total amount of remnant thyroid tissue in patients with incidentally found thyroid carcinoma was evaluated by US. A sonologist experienced in small-parts sonography conducted the examinations with different sonographic equipments (SI 400, Siemens, Erlangen, Germany; Logic 7, GE, Fairfield, CT, USA; Sonoline Antares, Siemens), using high-frequency linear probes (7.5 to 13 MHz). The operation site was examined to find remnant thyroid tissue. When it was found, volumetric measurements were made by measuring remnant tissue in three perpendicular planes, using axial and sagittal images and volume calculation software available within the equipments. The remnant thyroid volume was estimated through the equation \(V = length \times width \times depth \times \raise0.7ex\hbox{$\pi $} \!\mathord{\left/ {\vphantom {\pi 6}}\right.\kern-\nulldelimiterspace}\!\lower0.7ex\hbox{$6$} \). The evaluation of remnant thyroid tissue was performed by US and the radioactive iodine uptake test at the first postoperative month. In early postoperative periods (the first week), tissue edema, architectural distortion, and fluid collections make the examination more difficult and sometimes a reexamination is scheduled. In later periods, scar tissue can be a diagnostic problem, as it can mimic thyroid tissue, but it is generally possible to make the differential diagnosis.
We undertook a prospective study to compare the rates of postoperative recurrent laryngeal nerve palsy and hypoparathyroidism and postoperative thyrotropin (TSH) values. In addition to this, the number of parathyroid glands identified during thyroidectomy, the incidence of thyroid cancer, and thyroid cancer requiring RAI ablation and completion thyroidectomy were assessed in both groups.
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences 11.0 for Windows. Results were expressed as mean ± SD. Chi-square and Wilcoxin were used for statistical analysis and p < 0.05 was accepted as significant.
Results
Preoperative evaluation
The mean ± SD age in group 1 (47.3 ± 12 years) did not show any statistically significant difference compared with group 2 (45.7 ± 11 years) (p = .02). The male–female ratio was 10:94 and 14:98 in groups 1 and 2, respectively (p = .63). A dominant nodule was found in 157 patients (73%), including 73 in group 1 and 84 in group 2. There was not any significant difference between preoperative TSH values of the two groups (1.2 ± 0.2 vs 1.5 ± 0.5 mIU/L). TT and NTT were performed in 104 (48%) and 112 (52%) patients, respectively.
The evaluation of the complications
There was no operative mortality. Persistent hypoparathyroidism and vocal cord paralysis were not encountered in both groups. The incidence of RLN palsy in group 1 (0.9%) and group 2 (0.9%) did not show any statistically significant difference. The incidences of transient hypoparathyroidism in group 1 and group 2 were 26% (27/104) and 9.8% (11/112), respectively. The incidence of transient hypoparathyroidism in group 1 was significantly higher than in group 2 (p < 0.001). The rate of asymptomatic hypocalcemia in group 1 (7.4%) was lower than in the group 2 (27%) (p < 0.001).
Twenty seven out of 104 patients in group 1 received treatment for hypocalcemia. Hypocalcemic treatment was conducted for 8 ± 2.2 weeks (ranging from 3 to 12 weeks) postoperatively. Eleven out of 112 patients in group 2 received treatment for hypocalcemia. Hypocalcemic treatment was conducted for 3 ± 1.5 weeks (ranging from 1 to 6 weeks) postoperatively. The treatment for hypocalcemia in group 2 was discontinued earlier than with group 1. All of the patients, except those with hypocalcemia, were discharged 24 h following the operation. The hospitalization period for patients with hypocalcemia was longer in group 1 (3.8 ± 1.5 days) patients than in group 2 (2.7 ± 0.4 days) patients (p = 0.03). We performed power analysis (alfa=0.05 power=0.84 beta=0.16).
The evaluation of complications according to the number of parathyroid glands identified during thyroidectomy
During thyroidectomy, it was attempted to identify all parathyroid glands on their normal localizations. In group 1, four parathyroid glands were identified in 40 (36%) patients, three parathyroid glands were identified in 42 (40%) patients, two parathyroid glands were identified in 18 (17%) patients, and one parathyroid gland was identified in four (4%) patients. The number of identified parathyroid glands in patients who developed hypocalcemia was less than in those patients who didn’t develop hypocalcemia. In group 2, four parathyroid glands were identified in 46 (41%) patients, three parathyroid glands were identified in 40 (36%) patients, two parathyroid glands were identified in 12 (11%) patients, and one parathyroid gland was identified in 14 (12%) patients. The number of identified parathyroid glands in patients who developed hypocalcemia was less than in those patients who didn’t develop hypocalcemia (Fig. 1).
Histopatologic evaluation
Papillary cancer was detected in 24 patients (11%), of whom 20 (83%) had papillary microcarcinoma (<1 cm). The tumor size was greater than 1 cm in four patients. The range of tumor size was 2–7 mm for microcarcinomas and 11–14 mm for macrocarcinomas. Mean ± SD size of the all tumors was 5.5 ± 4.3 mm (range 2–14 mm). All tumors were papillary carcinomas with three cases of follicular variants, six cases with extrathyroid invasion, five cases with thyroid capsule invasion, and six cases with vascular invasion. The carcinomas were multifocal in six patients. The patients were classified as a low-risk group according to their MACIS scores. The incidence of papillary cancer was 9.6% (10/104) in group 1 and 12.5% (14/112) in group 2 (p = .36). The mean ± SD sizes of the tumors in group 1 and group 2 patients were 5.3 ± 4 mm (range 3–14 mm) and 5.6 ± 3.4 mm (range 2–12 mm), respectively (p = 0.258). Table 1 is shown the histological feature of papillary cancer in groups 1 and 2.
The evaluation of the remnant thyroid tissue in patients with papillary carcinoma
No remnant thyroid tissue was detected on US examinations of TT patients. The mean volume of the remnant thyroid tissue in NTT patients was measured 0.98 ± 0.12 cm3 (ranging from 0.2 to 2 cm3).
The rate of RAI ablation
Of 24 patients with papillary cancer, 14 (58%) had microcarcinoma with no local invasion or multicentricity. These patients were scheduled for follow-up only. The remaining 10 patients were found to have histological criteria for RAI ablation. Of these 10 patients, four were in group 1 and six were in group 2 (p = 0.25). None of the patients underwent completion thyroidectomy before ablative therapy.
The mean ± SD value of the TSH value at the first postoperative month was significantly higher in group 1 than in group 2 (89.3 ± 27 vs 58.5 ± 22 mIU/L) (p < .001). The TSH values of all patients were above 30 mIU/L and these patients did not undergo completion thyroidectomy before ablative therapy.
Discussion
In the present study, the rate of RLN palsy was not significantly different between both groups. NTT was associated with a lower risk for transient hypoparathyroidism than TT. Histopathological examination of the thyroid tissue in patients with nontoxic multinodular goiter showed the presence of thyroid cancer in 14% of the cases, none of them with any clinical or imaging signs suggestive of malignancy pre- or perioperatively. The performance of TT or NTT obviates the need for completion thyroidectomy in patients with multinodular goiter with incidentally found thyroid cancer.
Disorders of the thyroid gland are the second most common endocrine disease, next to diabetes mellitus. Thyroid surgery is one of the most frequent operations performed in iodine-deficient regions [2–4]. The goal of surgical treatment in thyroid disease should be to eliminate the disease with low complication rates and to minimize the necessity for reoperative procedures. The most frequent complications of thyroid surgery are RLN palsy and hypoparathyroidism [6, 9–12].
Although the overall complication rate is low, RLN palsy is a devastating life-long handicap when it occurs. The incidence of RLN injury in literature varies from 0 to 4% and is greater in extensive resection and in case of reoperation, thyroid carcinoma, and Graves disease [6, 14, 15]. Even experienced surgeons report inadvertent injury to the nerve and persistent RLN palsy in about 1–2% of patients [12, 13, 15, 16].
The reported incidence of RLN palsy has decreased over the past several decades due to the identification of the nerve [6, 7, 11]. Several studies have demonstrated that RLN palsy is more common when it is not routinely identified. Despite the identification of RLN during thyroidectomy, RLN palsy still occurs with reported incidences of up to 5% transient and 0.5% persistent paralysis in a recent study.
Recently, TT and NTT have emerged as alternative surgical procedures to bilateral subtotal thyroidectomy in the management of benign thyroid disorders [2–5, 17, 18]. However, some surgeons object to its routine use for the management of benign thyroid disorders, due to high complication rates associated with TT. However, many authors have reported remarkably low complication rates of TT in the hands of experienced surgeons [12, 14]. In our study, the rate of RLN palsy was not significantly different between both groups.
TT creates a potential risk for all parathyroid glands. Hypocalcemia, whether asymptomatic or not, is frequently encountered after thyroid surgery [6]. In several studies, the incidence of hypoparathyroidism varied from 1.6 to above 50% [6, 12, 13]. The etiology of hypoparathyroidism seems to be a multifactorial phenomenon but the most important factor is the iatrogenic surgical trauma to parathyroid glands, extent of surgery, the experience of the surgeon, and the number of functioning glands left behind. Hypoparathyroidism from thyroid surgery occurs when the parathyroid gland is removed and not reimplanted, the gland infarcts from manipulation, or the blood supply is disrupted [12–14].
The problem of how many parathyroids must be preserved to maintain a normal serum calcium level remains unresolved. Although some authors believe that a single functioning gland is enough to restore normal parathyroid activity, others believe that the integrity of at least three glands is necessary [6, 13–15]. Our study has demonstrated that the number of identified parathyroid glands in patients who developed hypocalcemia was less than in those patients who didn’t develop hypocalcemia. In our study, NTT was performed by the capsular dissection method, leaving less than 1 g of remnant tissue around the Berry ligament. With this method, at least the superior parathyroid glands’ vascularization is preserved. We think that the lower incidence of hypocalcemia in NTT is related to the preservation of vascularization in at least two parathyroid glands.
Some surgeons believe that it is prudently important to save some thyroid tissue around the nerve junction to the larynx to prevent injury of RLN and parathyroid glands. The risk of RLN injury might increase during the hemostasis of the remnant thyroid tissue in NTT. However, the risk of hypoparathyroidism is lower in NTT compared to TT. In our study, the rates of RLN palsy and hypoparathyroidism were 2.1 and 13.5%, respectively, after TT and 0.3 and 2.4%, respectively, after NTT.
Traditionally, subtotal thyroidectomy has been considered the standard surgical treatment for multinodular goiter due to low complication rates. Subtotal thyroidectomy does not completely avoid the risk of postoperative complications [19]. In addition to this, subtotal thyroidectomy leads to recurrent goiter in up to 23% of patients. Leaving residual abnormal tissue exposes the patient to the risk of recurrent disease and subsequent reoperation [19, 20]. Suppressive hormonal treatment after partial resection often does not prevent regrowth in the thyroid remnant [19]. A considerable number of patients undergoing subtotal resection as initial surgical treatment need reoperation for incidentally found thyroid carcinoma [2–4]. For this reason, TT or NTT has been usually performed at our clinic as the treatment of choice for nontoxic or toxic multinodular goiter.
Multinodular goiter patients are evaluated using sonography and FNAB to detect the presence of malignancy. While there are sonographic signs suggestive of neoplastic proliferation (like microcalcifications and irregular borders), not all of the cases have pathognomic characteristics. Also, the presence of multiple nodules makes this task more difficult. So, it is not uncommon to detect the presence of thyroid cancer postoperatively. Solitary cold nodules have always been considered more dangerous for malignancy than multinodular goiter. However, recent studies documented that multiple nodules carry the same risk as solitary nodules for neoplastic proliferation [21–23]. FNAB was performed on patients with dominant nodules and we found out that the location of the tumor outside the dominant nodule and the presence of papillary carcinoma were the most important factors to yield to false negative results of FNAB. Of the four patients with papillary thyroid carcinoma larger than 1 cm and with false negative FNAB results, the tumors were outside the dominant nodule. The dominant nodules’ sizes in these patients were greater than 1.5 cm. We think that the main diagnostic pitfalls in FNAB resulted from papillary microcarcinoma and location of the tumor outside the dominant nodule in multinodular goiter.
The treatment of microcarcinomas is still a matter of discussion. Many microcarcinomas may remain occult and are diagnosed as an incidental finding during surgery for benign thyroid disorders. However, some microcarcinomas may have a negative outcome, including distant metastasis and patient death [24–27]. Pellegriti et al. [28] found loco regional metastasis in 1/4 of 299 carcinoma patients with tumors smaller than 1.5 cm. Multivariate analysis found lymph node positivity at presentation, multicentricity and nonincidental tumor presence as prognostic factors. Recent studies report that microcarcinomas show extrathyroidal invasion regardless of the tumor size, and local recurrences are frequently observed.
In our country (Turkey), a number of patients operated on for thyroid carcinoma, while not being a majority, show noncompliance to the postoperative follow-up programs due to geographic and sociocultural reasons. This group of patients can be accessed only when there are serious complications causing them to seek medical help. Therefore, we prefer to take into account those behaviors when deciding on RAI treatment, despite the presence of a low-risk score. For RAI ablation therapy to be effective, the preferred TSH level should be higher than 30 mIU/L. Since 1998, TT and NTT have been performed at our clinic as the treatment of choice for benign thyroid disease with the exception of solitary unilateral nodules. Reoperation should be performed in patients with incidentally found thyroid cancer if the histological criteria mandate RAI ablation and if there is a large volume of thyroid remnant. In the present study, no patient required reoperation.
In conclusion, we recommend NTT in multinodular goiter instead of total or subtotal thyroidectomy. While NTT and TT obviate the need for completion thyroidectomy in incidentally found thyroid cancer and there is no difference in the rate of RLN palsy between two methods, NTT causes a significantly lower rate of hypoparathyroidism than TT.
References
Bellantone R, Lombardi CP, Bossola M, Boscherini M, De Crea C, Alesina P, Traini E, Princi P, Raffaelli M (2002) Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg 26(12):1468–1471
Giles Y, Boztepe H, Terzioglu T, Tezelman S (2004) The advantage of total thyroidectomy to avoid reoperation for incidental thyroid cancer in multinodular goiter. Arch Surg 139(2):179–182
Mishra A, Agarwal A, Agarwal G, Mishra SK (2001) Total thyroidectomy for benign thyroid disorders in an endemic region. World J Surg 25(3):307–310
Bron LP, O’Brien CJ (2004) Total thyroidectomy for clinically benign disease of the thyroid gland. Br J Surg 91(5):569–574
Acun Z, Comert M, Cihan A, Ulukent SC, Ucan B, Cakmak GK (2004) Near-total thyroidectomy could be the best treatment for thyroid disease in endemic regions. Arch Surg 139(4):444–447
Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP (1998) Morbidity of thyroid surgery. Am J Surg 176(1):71–75
Sturniolo G, D’Alia C, Tonante A, Gagliano E, Taranto F, Lo Schiavo MG (1999) The recurrent laryngeal nerve related to thyroid surgery. Am J Surg 177(6):485–488
Bhattacharyya N, Fried MP (2002) Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg 128(4):389–392
Misiolek M, Waler J, Namyslowski G, Kucharzewski M, Podwinski A, Czecior E (2001) Recurrent laryngeal nerve palsy after thyroid cancer surgery: a laryngological and surgical problem. Eur Arch Otorhinolaryngol 258(9):460–462
Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, Dralle H (2000) Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 24(11):1335–1341
Chiang FY, Wang LF, Huang YF, Lee KW, Kuo WR (2005) Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery 137(3):342–347
Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, Pelizzo MR, Pezzullo L (2004) Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 28(3):271–276
Prim MP, de Diego JI, Hardisson D, Madero R, Gavilan J (2001) Factors related to nerve injury and hypocalcemia in thyroid gland surgery. Otolaryngol Head Neck Surg 124(1):111–114
Goncalves Filho J, Kowalski LP (2005) Surgical complications after thyroid surgery performed in a cancer hospital. Otolaryngol Head Neck Surg 132(3):490–494
Abboud B, Sargi Z, Akkam M, Sleilaty F (2002) Risk factors for postthyroidectomy hypocalcemia. J Am Coll Surg 195(4):456–461
Mishra A, Agarwal G, Agarwal A, Mishra SK (1999) Safety and efficacy of total thyroidectomy in hands of endocrine surgery trainees. Am J Surg 178(5):377–380
Ozbas S, Kocak S, Aydintug S, Cakmak A, Demirkiran MA, Wishart GC (2005) Comparison of the complications of subtotal, near total and total thyroidectomy in the surgical management of multinodular goitre. Endocr J 52(2):199–205
Koyuncu A, Dokmetas HS, Turan M, Aydin C, Karadayi K, Budak E, Gokgoz S, Sen M (2003) Comparison of different thyroidectomy techniques for benign thyroid disease. Endocr J 50(6):723–727
Rojdmark J, Jarhult J (1995) High long term recurrence rate after subtotal thyroidectomy for nodular goitre. Eur J Surg 161(10):725–727
Reeve TS, Delbridge L, Brady P, Crummer P, Smyth C (1988) Secondary thyroidectomy: a twenty-year experience. World J Surg 12(4):449–453
Chao TC, Jeng LB, Lin JD, Chen MF (1997) Reoperative thyroid surgery. World J Surg 21(6):644–647
Frates MC, Benson CB, Charboneau JW, Cibas ES, Clark OH, Coleman BG, Cronan JJ, Doubilet PM, Evans DB, Goellner JR, Hay ID, Hertzberg BS, Intenzo CM, Jeffrey RB, Langer JE, Larsen PR, Mandel SJ, Middleton WD, Reading CC, Sherman SI, Tessler FN (2005) Society of Radiologists in Ultrasound. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 237(3):794–800
Milas M, Stephen A, Berber E, Wagner K, Miskulin J, Siperstein A (2005) Ultrasonography for the endocrine surgeon: a valuable clinical tool that enhances diagnostic and therapeutic outcomes. Surgery 138(6):1193–2000
Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH (2003) Papillary microcarcinoma of the thyroid—prognostic significance of lymph node metastasis and multifocality. Cancer 58:31–40
Schlumberger M, Berg G, Cohen O et al (2004) Follow-up of low-risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol 150:105–112
Hay ID, Thompson GB, Grant CS et al (2002) Papillary thyroid carcinoma managed at the mayo Clinic during six decades (1990–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 26:879–885
Pearce EN, Braverman LE (2004) Editorial: papillary thyroid microcarcinoma outcomes and implications for treatment. J Clin Endocrinol Metab 89:3710–3712
Pellegriti G, Scollo C, Lumera G, Regalbuto C, Vigneri R, Belfiore A (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89:3713–3720
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erbil, Y., Barbaros, U., Salmaslıoğlu, A. et al. The advantage of near-total thyroidectomy to avoid postoperative hypoparathyroidism in benign multinodular goiter. Langenbecks Arch Surg 391, 567–573 (2006). https://doi.org/10.1007/s00423-006-0091-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-006-0091-z