Abstract
Purpose
Hypovolemia decreases preload and cardiac stroke volume. Cardiac stroke volume (SV) and its variability (cardiac stroke volume variability, SVV) have been proposed as clinical tools for detection of acute hemorrhage. We compared three non-invasive SV measurements and investigated if respiration-induced fluctuations in SV may detect mild and moderate hypovolemia in spontaneously breathing humans.
Methods
Ten healthy subjects underwent experimental central hypovolemia induced by lower body negative pressure to −60 mmHg or onset of presyncopal symptoms. SV beat-to-beat was estimated simultaneously by ultrasound Doppler, finger arterial blood pressure curve and impedance cardiography. SVV was calculated by spectral analysis between 0.15 and 0.40 Hz.
Results
Relative changes in SV did not show significant differences between the methods. The SVV measured by ultrasound Doppler and arterial blood pressure curve decreased at −30 mmHg to 32 % (ultrasound Doppler: 95 % CI 18–47, arterial blood pressure curve: 95 % CI 21–43) and at maximal simulated hypovolemia to 23 % (ultrasound Doppler: 95 % CI 14–81) and 21 % (arterial blood pressure curve: 95 % CI 9–33) of baseline variability. The variability in cardiac stroke volume from the impedance cardiography did not change significantly during the simulated hypovolemia, to 88 and 76 % of baseline variability.
Conclusion
Cardiac stroke volume estimated by ultrasound Doppler and by arterial blood pressure curve showed parallel variations beat-to-beat during simulated hemorrhage, whereas impedance cardiography did not appear to track beat-to-beat changes in cardiac stroke volume. The variability in cardiac stroke volume was decreased during mild and moderate hypovolemia and could be used for early detection of hypovolemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Uncontrolled hemorrhage is one of the leading causes of civilian trauma deaths (Sauaia et al. 1995), and the main cause of death on the battlefield (Kelly et al. 2008). During the early stages of hemorrhage, the physiological compensatory mechanisms of the body preserve adequate blood pressure in an attempt to maintain sufficient perfusion to vital organs. At the sudden onset of cardiovascular collapse, blood pressure falls without warning, and it may be too late to initiate lifesaving treatment. Early detection of acute hemorrhage is, therefore, crucial for increasing survival rates. We are in need of tools to detect hemorrhage at an early stage.
Venous return shows a relatively immediate reduction during central hypovolemia, for example, during hemorrhage, and reduced preload causes a rapid change in cardiac stroke volume (SV) (Fu and Levine 2014; Goswami et al. 2009; Hanson et al. 1998). Monitoring of SV changes has been proposed as a clinical tool for early detection of acute hemorrhage and assessment of its severity (Convertino et al. 2006; Johnson et al. 2014; Leonetti et al. 2004). The drop in SV during hemorrhage reflects the degree of blood loss, but it is nonetheless difficult to track SV continuously in patients who are hemorrhaging (Convertino et al. 2006).
To estimate the respiratory variability in SV (SVV) by power spectral analysis, continuous beat-to-beat recordings of SV lasting a few minutes are needed. There are several non-invasive ways of obtaining such recordings, there is but no generally accepted standard method. Three commonly used non-invasive techniques to estimate SV are: (a) from the arterial blood pressure curve (Bogert and van Lieshout 2005); (b) by ultrasound Doppler (Eriksen and Walloe 1990); (c) by impedance cardiography (Fortin et al. 2006).
SVV is already in clinical use for detection of hypovolemia in mechanically ventilated patients, where an increase in SVV is an indicator of fluid-responsive hypovolemia (Marik et al. 2009). In a pre-hospital setting, the patient is spontaneously breathing and we are, therefore, in need of a detector that is operating in spontaneously breathing humans. We have previously found that SVV differentiates between normovolemia and hypovolemia during mild hypovolemia and spontaneous breathing by one method of SV estimation (Elstad and Walløe 2015). In this study, we wanted to simulate both mild and moderate hypovolemia and hypothesized that SVV would be an efficient way of tracking the development of a simulated hemorrhage. The primary aim of this study was to investigate SVV as a candidate for detection of central hypovolemia in the early stages of hemorrhage. The secondary aim was to compare three non-invasive methods of simultaneously measured SV and their ability to track SV beat-to-beat.
Methods
Subjects
Ten young, healthy non-smoking volunteers (five females) [median and 95 % confidence interval (CI): age 21.5 years (20, 23.5 years), height 174 cm (167.5, 179.5 cm), weight 67.5 kg (58.5, 76.5 kg), exercise level 7 h per week (4, 10 h per week)] underwent experimental central hypovolemia through LBNP until −60 mmHg or onset of presyncope (defined below). Prior to the experiment, the subjects were asked not to eat (2 h before), to refrain from strenuous exercise and consumption of caffeine (12 h before), and not to consume alcohol (24 h before). All female subjects delivered a urine pregnancy test on the same day as the experiment. The subjects received written and oral information and were familiarized with the experimental protocol and the procedures in a separate session. Written informed consent was obtained from all participants, and the study was submitted to and approved by the Regional Ethical Committee (REK reference number S-08774d). All the experiments conformed to the Declaration of Helsinki (revised 2008).
Experimental protocol
The subjects rested in a supine position with their lower extremities inside the LBNP chamber, which was air sealed at the level of the iliac crest. Our custom-built LBNP chamber and pressure control system are designed to induce rapid (within 0.3 s) or gradual changes in LBNP (Hisdal et al. 2003). LBNP is a valid method for studying hemodynamic parameters during simulated hemorrhage (Hinojosa Laborde et al. 2014; Johnson et al. 2014). The subjects wore thick socks to keep their feet warm despite the decrease in pressure inside the LBNP chamber. The noise level from the LBNP device is similar to that from a vacuum cleaner. A standard vacuum cleaner was switched on during the experiments to minimize variations in the background noise level, and thus reduce the known physiological effects that abrupt noise has on human physiology (Wesche et al. 1998). The room temperature was kept at 25–28 °C so that the lightly dressed subjects were in their thermoneutral zone (Elstad et al. 2014).
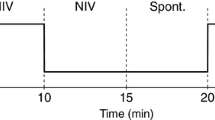
The experimental protocol included a stepwise introduction, a ramp phase and a plateau phase for the tolerant subjects. The protocol had five different phases as illustrated in Fig. 1a; 5 min at baseline (atmospheric pressure, 0 mmHg) followed by a sudden decrease in pressure to −30 mmHg; 3 min at −30 mmHg; a gradual decrease in pressure from −30 to −60 mmHg during a 10-min period; 3 min at −60 mmHg; 5-min recovery at 0 mmHg. We chose this combination of step and ramp protocol to achieve both rapid and slow changes in cardiovascular parameters. LBNP of −30 mmHg has been shown to simulate a moderate blood loss and −60 mmHg simulates severe blood loss (Cooke et al. 2004). The subjects breathed spontaneously during the experiments. The protocol was prematurely halted if the subject suffered a sudden fall in heart rate of >15 beats/min, a sudden fall in blood pressure of >15 mmHg or systolic blood pressure <70 mmHg. LBNP was terminated immediately if the subject wished to stop the experiment or if any symptoms of presyncope occurred, such as dizziness, nausea, tinnitus, sweating, heat sensation, or reduced field of vision.
The experimental protocol. a The lower body negative pressure (LBNP) protocol. The horizontal lines indicate the four phases used for data analysis. b Raw data of stroke volume from one subject who completed the full protocol. The black curve shows stroke volume from ultrasound Doppler (SVusd), the light gray curve stroke volume from the arterial blood pressure curve (SVbpc) and the dark gray curve stroke volume from impedance cardiography (SVimp). The discontinued vertical lines indicate where the LBNP was turned on and off. LBNP lower body negative pressure
Measurements
Heart rate (HR) was obtained from the duration of each R–R interval of the three-lead ECG signal (VINGMED SD 100, Horten, Norway). Respiratory chest movement was obtained using a belt around the upper abdomen (Respiration and Body Position Amplifier, Scan-Med a/s, Drammen, Norway). Mean arterial blood pressure (MAP) was calculated by the integration of the blood pressure wave divided by the RR interval (program for real-time data acquisition (version REGIST3), Morten Eriksen, Oslo, Norway). Pulse pressure (PP) was calculated in REGIST3 by subtracting minimal pressure from maximal pressure within each RR interval. Continuous SV was measured simultaneously by three different, non-invasive methods during the experimental protocol. Each method is described separately below.
Beat-to-beat SV from the left side of the heart was obtained by ultrasound Doppler (SVusd) (VINGMED SD 100, Horten, Norway) (Eriksen and Walloe 1990). The diameter of the rigid aortic ring used in the calculation of SV estimated by ultrasound Doppler was determined by parasternal 2D ultrasound imaging (VIVID 7, GE Vingmed, Horten, Norway) during a separate session before the experimental day. As the aortic ring is rigid, the diameter measured at rest would not differ from the diameter during the application of LBNP. The ultrasound Doppler recorded beat-to-beat SV from estimates of the blood velocity in the aorta (Eriksen and Walloe 1990). An angle of 20° between the direction of the sound beam and the bloodstream was assumed in the calculations. The output of the SD-100 maximum velocity estimator was transferred online to the recording computer. SVusd was calculated by multiplying the value obtained by numerical integration of the recorded instantaneous maximum velocity during each R–R interval by the area of the orifice (Eriksen and Walloe 1990). SVusd has been validated against thermodilution (Eriksen and Walloe 1990).
Finger arterial pressure was recorded continuously from the middle left finger positioned at heart level (FINOMETER, Finapres Medical System, Amsterdam, The Netherlands) (Bogert and van Lieshout 2005; van Lieshout et al. 2003). The Finometer provided arterial blood pressure, from which pulse rate (PR) and SV from blood pressure curve (SVbpc) were calculated by ModelFlow (Bogert and van Lieshout 2005). PR from the Finometer was needed for the subsequent processing. SVbpc measured by ModelFlow is in good accordance with SVusd during supine rest (van Lieshout et al. 2003) and reflects the progression of SV during LBNP (Reisner et al. 2011).
The third SVimp measurement was estimated from impedance cardiography using Task Force Monitor (SVimp) (sampling rate 40 kHz, TASK FORCE MONITOR®, Model 3040i, CNSystems Medizintechnik, Graz, Austria) (Fortin et al. 2006; Gratze et al. 1998). This impedance cardiography device uses two sensors on the neck and two sensors on the thorax, which detect electrical impedance changes in the thorax. Impedance varies in inverse proportion to fluid/volume in the thorax, i.e., greater impedance to current flow with reduced thoracic volume and is assumed to be related to the instantaneous blood flow in the aorta (Marik 2013). The impedance changes are used to calculate hemodynamic parameters (Gratze et al. 1998), including SV (Fortin et al. 2006). Impedance cardiography provides satisfactory estimates of SV in resting conditions (Warburton et al. 1999). Both absolute values for SVimp and changes in SVimp are similar to SV estimated by echocardiography during LBNP (Gotshall et al. 1999).
Data processing
ECG, arterial blood pressure wave, respiration signal and maximal aortic blood velocity were transferred online (sampled at 100 Hz) to a recording computer running a dedicated data collection and analysis program (program for real-time data acquisition; Morten Eriksen, Oslo, Norway), which calculated SVusd from velocity time integral and area. The recordings were further processed in a MATLAB program specifically designed for this purpose (MATLAB® R2013b, MathWorks® Inc, http://www.mathworks.com). Each recording was processed to filter the calibration signal from blood pressure recording. Every calibration signal lasted three to five heartbeats and there were between 0 and 2 calibration signals in each analyzed interval. The calibration signal was recognized and linear interpolation was made beat-to-beat between the last successful and first successful measurement. Each filtration was also visually checked. The data files sampled beat-by-beat were added to the data file sampled at 100 Hz, and this file was resampled at 4 Hz with the custom-built program in MATLAB (Elstad et al. 2009).
PR and SVbpc were calculated by the Finometer, and the output was delayed by approximately 1.5 s before it was transferred to the recording computer. To adjust these curves to fit the time of recording, the continuous recordings were shifted by approximately −1.5 s (individually between 1.25 and 1.75 s), so that the PR was matched to the HRusd. The signal from cardiothoracic impedance was recorded on a separate computer. The HRimp was used to adjust SVimp with the time of recording, so that the HRimp was matched to the HRusd, both derived from ECG. Every recorded signal from each experimental run was visually inspected, and only time intervals with successful recordings were included in the subsequent analysis. A successful recording is a recording of physiological data without loss of signal and minimum noise. Four time intervals for each subject were included for further analysis, wherever possible.
Analysis
The time alignment between the recordings was visually inspected in GraphPad (GRAPHPAD Prism 6; GraphPad Software, Inc., La Jolla, California, USA). The data reported were analyzed in four time epochs of 120 s; baseline (0 mmHg LBNP), −30 mmHg LBNP, maximal LBNP and recovery (0 mmHg LBNP). Maximal LBNP is given as the range of lowest pressures completed by ten subjects: during the transient increase of LBNP from −40 to −60 mmHg (7 subjects) or during the plateau at −60 mmHg LBNP (3 subjects). The 120-s long time epochs were selected on the base of successful recordings.
Variability analysis
SV varies with respiration, due to variations in intrathoracic pressure, and subsequent effects on preload (Toska and Eriksen 1993; Elstad et al. 2001). These respiration-related variations can be quantified by applying variability analysis at respiratory frequency (Johnson et al. 2014; Marik et al. 2009; Reisner et al. 2011). To calculate SVV through variability analysis, beat-to-beat recordings of SV are needed (Elstad 2012).
Cardiovascular variability during respiration was calculated from the fast Fourier transform spectral analysis integral between 0.15 and 0.4 Hz during four phases of the experimental protocol, using epochs of 120-s duration as mentioned above, in Sigview (SIGVIEW, version 2.5.1, http://www.sigview.com). Variability analysis computed as power integral between 0.15 and 0.4 Hz was applied to all three SV methods. Because the Finometer signal was lost during maximal LBNP in one subject, SVVbpc could only be calculated for nine subjects at this stage. SVVimp was calculated for nine subjects because recordings from the tenth subject were unsatisfactory (as this subject had variations in SVimp >100 ml/beat). The comparison between the methods was performed on the maximal subjects available at each stage, 8–10 subjects.
Statistics
The non-parametric median and 95 % confidence intervals (CI) given by Hodges–Lehmann estimation were calculated from epochs of 120 s for SV and SVV at four previously described phases, by StatXact® (CYTEL STUDIO 10, Cytel Inc., Cambridge, MA, USA). 95 % CI found by Hodges–Lehmann estimation corresponds to the Wilcoxon one-sample test (Hollander and Wolfe 1999). Kruskal–Wallis one-way analysis of variance by ranks for three groups was used to test for difference in the three methods between baseline and −30 mmHg LBNP (http://vassarstats.net/kw3.html, Høyland and Walløe 1977). Wilcoxon matched-pair sign rank test was used to compare methods. The slope and regression coefficient (r 2) between LBNP and SV from the three methods was estimated by linear regression during the ramp part of the protocol in GraphPad. P < 0.05 was considered significant. Unless otherwise specified, results are given as medians with 95 % Hodges–Lehmann’s confidence interval.
Results
Subject response to LBNP
Ten subjects underwent simulated hypovolemia. In seven of the ten subjects, the protocol was terminated prematurely in response to presyncopal signs or symptoms: a fall in systolic blood pressure to <70 mmHg (one subject), a sudden fall in blood pressure of more than 15 mmHg (five subjects), or dizziness plus reduced field of vision (one subject). For these seven subjects, the protocol was terminated at LBNP levels of −40, −41, −44, −45, −51, and −56 mmHg (the latter for two subjects). The hemodynamic response is given in Table 1.
Stroke volume during LBNP
Raw data from one subject show a similar progressive decrease in SV with all three methods, which clearly reflects the progression of LBNP (Fig. 1b). The same trend is apparent from group data (n = 10) of absolute values of SV obtained by the three methods, as displayed in Fig. 2a. A decrease of approximately 36 ml from baseline to the maximal LBNP stage can be seen for all three methods. At group level, the baseline values for SV differed somewhat between the three methods (SVusd 78 ml/beat, SVbpc 88 ml/beat and SVimp 99 ml/beat) (Table 1). The three methods also gave different absolute values for SV from the same subject.
Absolute and relative stroke volume measured by three different methods during lower body negative pressure (LBNP). a Stroke volume in ml. b Relative stroke volume. The squares represent stroke volume from ultrasound Doppler, the circles stroke represent cardiac stroke volume from the arterial blood pressure curve, and the triangles represent stroke volume from impedance cardiography. Bars indicate the 95 % confidence interval and the dots their median by Hodges–Lehmann estimation. Asterisk indicates p < 0.05 as compared to baseline. Group data, n = 10. LBNP lower body negative pressure, SV bpc stroke volume from arterial blood pressure curve, SV usd stroke volume from ultrasound Doppler, SV imp stroke volume from impedance cardiography
We normalized the SV values thus displaying relative changes for the three methods at group level (Fig. 2b). Normalized values of SV from group data show that SVusd decreased by 45 % (95 % CI 37 %, 52 %), SVbpc by 39 % (95 % CI 27 %, 45 %) and SVimp by 37 % (95 % CI 24 %, 49 %) from baseline to the lowest individual level of LBNP (Fig. 2b). Differences between the three methods were not statistically significant. Neither absolute SV values (at baseline and −30 mmHg LBNP) nor relative SV changes at −30 mmHg predicted tolerance to LBNP.
Regression analysis of group data (n = 10) shows that in the ramp part of the protocol (from −30 mmHg LBNP to −60 mmHg LBNP), HR increased significantly during pressure reduction, with a regression of 0.9 bpm/mmHg [95 % CI 0.6, 1.3 bpm/mmHg, r 2 = 0.55 (95 %CI 0.34, 0.75)] (Fig. 3). SVusd, SVbpc and SVimp decreased significantly and similarly during pressure reduction, by −0.9 ml/mmHg decrease in LBNP for all three methods [95 % CI SVusd −1.2, −0.6 ml/mmHg, r 2 = 0.51 (0.35, 0.66); 95 % CI SVbpc −1.6, −0.5 ml/mmHg, r 2 = 0.70 (0.51, 0.79); 95 % CI SVimp −1.3, −0.3 ml/mmHg, r 2 = 0.38 (0.17, 0.59)] in the ramp part of the protocol (Fig. 3).
Linear regression between stroke volume (SV) and degree of lower body negative pressure during the ramp part of the protocol (from −30 to −60 mmHg LBNP) in two of the three methods in one representative subject. The black line shows stroke volume from ultrasound Doppler (SVusd, r 2 = 0.61), the light gray curve stroke volume from the arterial blood pressure curve (SVbpc, r 2 = 0.79). Stroke volume from impedance cardiography (SVimp) (not shown, overlapping with SVbpc) had in this subject r 2 = 0.47. LBNP lower body negative pressure, SV bpc stroke volume from arterial blood pressure curve, SV usd stroke volume from ultrasound Doppler, SV imp stroke volume from impedance cardiography
Stroke volume variability during LBNP
Figure 4 shows raw data from 10 s of recordings of SV, measured by three methods, and the index of thorax volume at baseline. The absolute cardiovascular variability is given in Table 2, and the relative cardiovascular variability is illustrated in Fig. 5b. The three methods for estimating SV did not give the same decrease in SVV from baseline to −30 mmHg of LBNP (Kruskal–Wallis test, p = 0.029). SVVimp had a significantly lower variability at baseline compared to SVVbpc (p = 0.04). Both SVVusd and SVVbpc changed significantly (p = 0.002), dropping to 32 % (95 % CI SVVusd 18 %, 47 %, 95 % CI SVVbpc 21 %, 43 %) of baseline values at −30 mmHg of LBNP. In contrast, SVVimp was 88 % (95 % CI 42 %, 182 %) (n = 9) of the baseline value at −30 mmHg of LBNP (Fig. 4), which was not a significant decrease (p = 0.82). SVVusd was 23 % (95 % CI 14 %, 81 %) of baseline value at maximal LBNP (p = 0.006). SVVbpc was 21 % (95 % CI 9 %, 33 %) (n = 9) of baseline value at maximal LBNP (p = 0.004). Further, at maximal LBNP, SVVimp was not significantly different from its value at −30 mmHg of LBNP, and remained at 76 % (95 % CI 23 %, 126 %) (n = 9) of baseline value (p = 0.77). SVVbpc, SVVusd and SVVimp were restored during recovery to 94 % (95 % CI 64 %, 124 %), 98 % (95 % CI 50 %, 203 %) and 96 % (95 % CI 47 %, 335 %), respectively, of baseline values.
Ten seconds of a 30-min recording of stroke volume measured by three different methods and thorax volume (respiration) at baseline raw data from one subject. The black curve shows stroke volume from ultrasound Doppler, the light gray curve stroke volume from the arterial blood pressure curve and the dark gray curve stroke volume from impedance cardiography. The lowest curve shows respiration, where an upward slop indicated inspiration (arrow). SV bpc stroke volume from arterial blood pressure curve, SV usd stroke volume from ultrasound Doppler, SV imp stroke volume from impedance cardiography, Resp index of thorax volume, LBNP lower body negative pressure
Relative stroke volume variability during LBNP. Bars indicate the 95 % confidence interval and the dots their median by Hodges–Lehmann estimation. The squares represent stroke volume variability from ultrasound Doppler (n = 10), the circles represent stroke volume variability from the arterial blood pressure curve (n = 9 at −40 to −60 mmHg of LBNP) and the triangles represent stroke volume variability from impedance cardiography (n = 9). Asterisk indicates p < 0.05 as compared to baseline. LBNP lower body negative pressure, SVV bpc stroke volume variability from arterial blood pressure curve, SVV usd stroke volume variability from ultrasound Doppler, SVV imp stroke volume variability from impedance cardiography
To differentiate between normovolemia and hypovolemia, SVVusd ≤12 ml2 detected mild hypovolemia (−30 mmHg) (SVVbpc p = 0.07, SVVusd p = 0.004). SVVbpc and SVVusd ≤10 ml2 (SVVbpc p = 0.01, SVVusd p = 0.03) were both predictive of hypovolemia.
Discussion
We tested if SVV can detect simulated hypovolemia in spontaneously breathing volunteers, and investigated how three different non-invasive methods of SV measurement track SV beat-to-beat. Our main findings were that changes in SVV revealed the early stages of simulated hypovolemia, and that impedance cardiography did not appear to track beat-to-beat changes in SV. We suggest that SVV is a possible detector of mild hypovolemia in spontaneously breathing humans; however, impedance cardiography should be used with caution when estimating SVV.
Comparison of three non-invasive methods of measuring beat-to-beat stroke volume
We compared three non-invasive techniques for beat-to-beat SV monitoring. Despite somewhat different absolute values from the three methods at baseline and throughout the protocol, we found that all three SV methods decreased by 0.9 ml/mmHg during the gradual decrease in LBNP from −30 to −60 mmHg. This shows that SV tracks a gradual hypovolemia, and thus our data support other studies where changes in SV clearly indicate the progression of simulated and actual hemorrhage (Convertino et al. 2006; Cooke et al. 2004; Leonetti et al. 2004; Marik 2013; Reisner et al. 2011). In three of the subjects, the SVbpc signal was lost for part of the time at maximal LBNP, possibly due to either a decrease in blood pressure or profound vasoconstriction (Imholz et al. 1998). SVimp showed the same progressive decrease during the protocol as SVusd and SVbpc. Further, the upper group confidence interval of SVimp contained non-physiological values at all stages of the protocol (Fig. 2a). In fact, in three of the subjects, SVimp increased as the simulated hypovolemia progressed, contrary to what would be expected as a normal physiological response when the preload decreases, as during hemorrhage. We speculate that the LBNP method influences the configuration of the thorax during chamber decompression, and blood-filled organs may be displaced during LBNP and during the respiratory cycle. During LBNP, both the hematocrit and the hemoglobin levels increased due to a plasma volume shift in the lower body (Johnson et al. 2014). These plasma volume changes could also influence SVimp during LBNP, independent of actual changes in central blood volume.
We found a decrease in SVV during simulated hypovolemia in spontaneously breathing subjects in two of the three methods for non-invasive SV measurement, as previously described in mild hypovolemia for SVVbpc (Shin et al. 2010; Elstad and Walløe 2015). SVVusd and SVVbpc gave similar results and both methods tracked SV beat-to-beat, whereas SVVimp did not appear to do so. SVVimp was low at baseline compared to SVVbpc (p = 0.04) (Table 2) and remained low throughout the experiments. We, therefore, recommend caution if impedance cardiography is to be used for beat-to-beat SV estimation.
Variability in cardiac stroke volume as a detector of central hypovolemia
SVV is already in clinical use to detect central hypovolemia in mechanically ventilated patients. During mechanical ventilation, SVV increases with fluid-respondent hypovolemia, and performs better than SV in detecting hypovolemia (Marik et al. 2009). However, in a clinical setting when a patient is suffering from hypovolemia due to hemorrhage, the patient will often breathe spontaneously, especially in a pre-hospital setting. It is, therefore, desirable to find a method of detecting hypovolemia in spontaneously breathing humans. Hemodynamic variability in both time domain and frequency domain is suggested to detect simulated central hypovolemia in healthy volunteers (Alian et al. 2011a, b). A previous study found that patients with dilated cardiomyopathy had larger SVV than controls (Caiani et al. 2002). There is a possibility that dilated heart disorders need different hemodynamic criteria to estimate the degree of hypovolemia.
There are other methods to estimate the grade of hypovolemia from the arterial waveform. The changing features in the arterial waveform obtained from the photoplethysmograph of an oximeter are suggested as a measure of the individual capacity to compensate for hypovolemia (Moulton et al. 2013). During paced breathing in healthy subjects, graded hypovolemia resulted in decreased SVVbpc (Shin et al. 2010) and SVVimp (Siebert et al. 2004). Pulse pressure variability (PPV) is suggested as another surrogate measure of SVV in hypovolemia (Marik et al. 2009), but is still debated in spontaneously breathing subjects (Michard 2005; Hoff et al. 2014).
During spontaneous breathing, as used in the current study, SVusd and SVbpc decreased by 23 and 17 % from baseline to −30 mmHg of LBNP, respectively (Fig. 2b), whereas both SVVusd and SVVbpc decreased by 68 % during the same time interval (Fig. 5b). The current study also shows that increased hypovolemia (from −30 to −60 mmHg of LBNP) further decreased SVVbpc and SVVusd. Thus, SVV tracks minor changes during hypovolemia, which suggests that it is a more potent variable for detecting hypovolemia than SV alone. As SVV decreases to a much greater extent during early hypovolemia compared to SV, it could be advantageous to monitor SVV instead of SV. The possibility of capturing these fine, rapid variations using SVV may prove particularly useful in early pre-hospital detection of hemorrhage, and lead to more successful treatment. Further studies are needed to test whether a single measurement of SVV can detect hypovolemia in spontaneously breathing subjects.
We observed that subjects who tolerated the highest level of LBNP (−60 mmHg for 3 min) also tolerated low levels of SV without a decrease in MAP (median SVbpc: subjects with high tolerance 39 ml versus 48 ml for subjects with low tolerance). This suggests that there is no cutoff figure for an absolute value of SV that indicates presyncope or hemodynamic decompensation during hemorrhage. On the other hand, SVV has a cutoff value of 10–12 % for hypovolemia detection in mechanically ventilated patients (Guinot et al. 2014). In the current study, we found a cutoff of ≤10 ml2 for detection of mild hypovolemia in both SVVusd and SVVbpc, similar to Elstad and Walløe (2015). Further testing in a pre-hospital setting is needed to explore the potential of SVV as a diagnostic tool for detection of hypovolemia.
Limitations
First, our study included a limited number of subjects. In addition, in seven of the subjects, we terminated LBNP during the transient decrease in LBNP. During maximal LBNP, the SV varied due to respiration as during rest and mild hypovolemia, but also due to the increased physiological challenge (Fig. 3) and technical difficulties (manual holding of ultrasound signal during decreased signal intensity and peripheral vasoconstriction). Consequently, the confidence interval of SV and SVV during maximal LBNP became wider, compared to previous time intervals (Figs. 2, 5). LBNP has a limited ability to model severe hemorrhagic and traumatic shock. The LBNP method does not take into consideration numerous co-existing variables usually present in a clinical situation, such as tissue injury, anesthesia, pain and fear (Cooke et al. 2004), and subjects cannot be taken to a level resulting in more severe central hypovolemia for safety reasons.
The method we used to produce central hypovolemia has some limitations. During simulated blood loss through LBNP, the circulation is intact and the circulatory volume is constant, with an increase in storage of blood in the distensible veins in the legs. The simulated blood loss initiates numerous physiological mechanisms comparable to those elicited during actual acute hemorrhage. However, during actual blood loss, there is a real decrease in blood volume, leading to several physiological mechanisms including changes in vascular properties such as venous capacitance and arterial compliance that might not be the same response as during simulated hemorrhage. In addition, the LBNP response (and thus the volume sequestered to the lower body) may depend on lower body size, lower body compliance and vascular compliance.
In the tables we report PP and PPV. We need to emphasize that the computation of variability from frequency domain is different from most studies on PPV, which report variability in time domain.
All three non-invasive SV measuring techniques examined in this study have limitations. SVusd is operator dependent. SVbpc may be unreliable at low arterial blood pressure levels since hypovolemia results in peripheral vasoconstriction and redistribution of blood during hemorrhage. Impedance cardiography has been shown to be sensitive to several factors, for instance the siting of the electrodes on the body, body motion and electrical noise such as may be expected in a laboratory or intensive care unit (Marik 2013). These methods may thus be fraught with logistical and technical difficulties in a pre-hospital setting, and further testing of SV measurement devices that could be used for calculation of SVV are needed before the application in a pre-hospital setting.
Clinical implications
SVV could in future be used as an early marker for hypovolemia in spontaneously breathing patients, for instance during the first encounter with a trauma patient at an accident site, during transportation or during triage in military combat and hereby try to prevent the development of hypovolemic shock. SVV could be used to detect a volume deficit in potentially volume-depleted patients and be used as a guide for monitoring the effects of fluid therapy and lead to faster appropriate treatment.
Conclusions
Beat-to-beat SV measured during LBNP using ultrasound Doppler, finger arterial blood pressure curve and impedance cardiography showed that SV clearly reflects the development of a simulated hemorrhage. The three different methods showed the same relative changes in SV during simulated hemorrhage. SV estimated by ultrasound Doppler and by arterial blood pressure curve showed parallel variations beat-to-beat during simulated hemorrhage, whereas impedance cardiography did not appear to track beat-to-beat changes in cardiac stroke volume. SVV decreases during the early phase of hypovolemia in spontaneously breathing subjects. SVV detects simulated hypovolemia, and further studies could evaluate its capacity to detect hemorrhage in a preclinical and hospital setting.
Abbreviations
- bpc:
-
Arterial blood pressure curve
- HR:
-
Heart rate
- HRV:
-
Heart rate variability
- imp:
-
Impedance cardiography
- LBNP:
-
Lower body negative pressure
- MAP:
-
Mean arterial blood pressure
- MAPV:
-
Mean arterial blood pressure variability
- PP:
-
Pulse pressure
- PPV:
-
Pulse pressure variability
- Resp:
-
Index of thorax volume
- SV:
-
Stroke volume
- SVV:
-
Stroke volume variability
- usd:
-
Ultrasound Doppler
References
Alian A, Galante N, Stachenfeld N, Silverman D, Shelley K (2011a) Impact of central hypovolemia on photoplethysmographic waveform parameters in healthy volunteers. Part 2: Frequency domain analysis. J Clin Monit Comput 25:387–396
Alian A, Galante N, Stachenfeld N, Silverman D, Shelley K (2011b) Impact of central hypovolemia on photoplethysmographic waveform parameters in healthy volunteers. Part 1: Time domain analysis. J Clin Monit Comput 25:377–385
Bogert LW, van Lieshout JJ (2005) Non-invasive pulsatile arterial pressure and stroke volume changes from the human finger. Exp Physiol 90:437–446
Caiani EG, Turiel M, Muzzupappa S, Colombo LP, Porta A, Baselli G (2002) Noninvasive quantification of respiratory modulation on left ventricular size and stroke volume. Physiol Meas 23:567–580
Convertino VA, Cooke WH, Holcomb JB (2006) Arterial pulse pressure and its association with reduced stroke volume during progressive central hypovolemia. J Trauma 61:629–634
Cooke WH, Ryan KL, Convertino VA (2004) Lower body negative pressure as a model to study progression to acute hemorrhagic shock in humans. J Appl Physiol 96:1249–1261
Elstad M (2012) Respiratory variations in pulmonary and systemic blood flow in healthy humans. Acta Physiol (Oxf) 205(3):341–348
Elstad M, Walløe L (2015) Heart rate variability and stroke volume variability to detect central hypovolemia during spontaneous breathing and supported ventilation in young, healthy volunteers. Physiol Meas 36:671–681
Elstad M, Toska K, Chon KH, Raeder EA, Cohen RJ (2001) Respiratory sinus arrhythmia: opposite effects on systolic and mean arterial pressure in supine humans. J Physiol 536:251–259
Elstad M, Nadland IH, Toska K, Walloe L (2009) Stroke volume decreases during mild dynamic and static exercise in supine humans. Acta Physiol (Oxf) 195:289–300
Elstad M, Vanggaard L, Lossius AH, Walloe L, Bergersen TK (2014) Responses in acral and non-acral skin vasomotion and temperature during lowering of ambient temperature. J Therm Biol 45:168–174
Eriksen M, Walloe L (1990) Improved method for cardiac output determination in man using ultrasound Doppler technique. Med Biol Eng Comput 28:555–560
Fortin J, Habenbacher W, Heller A, Hacker A, Grullenberger R, Innerhofer J, Passath H, Wagner C, Haitchi G, Flotzinger D, Pacher R, Wach P (2006) Non-invasive beat-to-beat cardiac output monitoring by an improved method of transthoracic bioimpedance measurement. Comput Biol Med 36:1185–1203
Fu Q, Levine BD (2014) Pathophysiology of neurally mediated syncope: role of cardiac output and total peripheral resistance. Auton Neurosci 184:24–26
Goswami N, Roessler A, Lackner H, Schneditz D, Grasser E, Hinghofer Szalkay H (2009) Heart rate and stroke volume response patterns to augmented orthostatic stress. Clin Auton Res 19:157–165
Gotshall RW, Davrath LR, Sadeh WZ, Coonts CC, Luckasen GJ, Downes TR, Tucker A (1999) Validation of impedance cardiography during lower body negative pressure. Aviat Space Environ Med 70:6–10
Gratze G, Fortin J, Holler A, Grasenick K, Pfurtscheller G, Wach P, Schonegger J, Kotanko P, Skrabal F (1998) A software package for non-invasive, real-time beat-to-beat monitoring of stroke volume, blood pressure, total peripheral resistance and for assessment of autonomic function. Comput Biol Med 28:121–142
Guinot PG, de Broca B, Bernard E, Abou Arab O, Lorne E, Dupont H (2014) Respiratory stroke volume variation assessed by oesophageal Doppler monitoring predicts fluid responsiveness during laparoscopy. Br J Anaesth 112:660–664
Hanson JM, Van Hoeyweghen R, Kirkman E, Thomas A, Horan MA (1998) Use of stroke distance in the early detection of simulated blood loss. J Trauma 44:128–134
Hinojosa Laborde C, Shade R, Muniz G, Bauer C, Goei K, Pidcoke H, Chung K, Cap A, Convertino V (2014) Validation of lower body negative pressure as an experimental model of hemorrhage. J Appl Physiol 116:406–415
Hisdal J, Toska K, Walloe L (2003) Design of a chamber for lower body negative pressure with controlled onset rate. Aviat Space Environ Med 74:874–878
Hoff IE, Hoiseth LO, Hisdal J, Roislien J, Landsverk SA, Kirkeboen KA (2014) Respiratory variations in pulse pressure reflect central hypovolemia during noninvasive positive pressure ventilation. Crit Care Res Pract 2014:712728
Hollander M, Wolfe DA (1999) Nonparametric statistical methods. Wiley, New York
Høyland A, Walløe L (1977) Elementær statistikk. Tapir, Trondheim
Imholz BP, Wieling W, van Montfrans GA, Wesseling KH (1998) Fifteen years experience with finger arterial pressure monitoring: assessment of the technology. Cardiovasc Res 38:605–616
Johnson BD, van Helmond N, Curry TB, van Buskirk CM, Convertino VA, Joyner MJ (2014) Reductions in central venous pressure by lower body negative pressure or blood loss elicit similar hemodynamic responses. J Appl Physiol (1985) 117:131–141
Kelly JF, Ritenour AE, McLaughlin DF, Bagg KA, Apodaca AN, Mallak CT, Pearse L, Lawnick MM, Champion HR, Wade CE, Holcomb JB (2008) Injury severity and causes of death from Operation Iraqi Freedom and Operation Enduring Freedom: 2003–2004 versus 2006. J Trauma 64:S21–S26 (Discussion S26–S27)
Leonetti P, Audat F, Girard A, Laude D, Lefrere F, Elghozi JL (2004) Stroke volume monitored by modeling flow from finger arterial pressure waves mirrors blood volume withdrawn by phlebotomy. Clin Auton Res 14:176–181
Marik P (2013) Noninvasive cardiac output monitors: a state-of the-art review. J Cardiothorac Vasc Anesth 27:121–134
Marik PE, Cavallazzi R, Vasu T, Hirani A (2009) Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 37(9):2642–2647
Michard F (2005) Changes in arterial pressure during mechanical ventilation. Anesthesiology 103(2):419–428
Moulton SL, Mulligan J, Grudic GZ, Convertino VA (2013) Running on empty? The compensatory reserve index. J Trauma Acute Care Surg 75:1053–1059
Reisner AT, Xu D, Ryan KL, Convertino VA, Rickards CA, Mukkamala R (2011) Monitoring non-invasive cardiac output and stroke volume during experimental human hypovolaemia and resuscitation. Br J Anaesth 106:23–30
Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT (1995) Epidemiology of trauma deaths: a reassessment. J Trauma 38:185–193
Shin WJ, Choi JM, Kong YG, Song JG, Kim YK, Hwang GS (2010) Spectral analysis of respiratory-related hemodynamic variables in simulated hypovolemia: a study in healthy volunteers with spontaneous breathing using a paced breathing activity. Korean J Anesthesiol 58:542–549
Siebert J, Drabik P, Lango R, Szyndler K (2004) Stroke volume variability and heart rate power spectrum in relation to posture changes in healthy subjects. Med Sci Monit 10:MT31–MT37
Toska K, Eriksen M (1993) Respiration-synchronous fluctuations in stroke volume, heart rate and arterial pressure in humans. J Physiol 472:501–512
van Lieshout JJ, Toska K, van Lieshout EJ, Eriksen M, Walloe L, Wesseling KH (2003) Beat-to-beat noninvasive stroke volume from arterial pressure and Doppler ultrasound. Eur J Appl Physiol 90:131–137
Warburton DE, Haykowsky MJ, Quinney HA, Humen DP, Teo KK (1999) Reliability and validity of measures of cardiac output during incremental to maximal aerobic exercise. Part II: Novel techniques and new advances. Sports Med 27:241–260
Wesche J, Orning O, Eriksen M, Walloe L (1998) Electrophysiological evidence of reinnervation of the transplanted human heart. Cardiology 89:73–75
Acknowledgments
We are grateful to Professor Lars Walløe for advice on statistical methods and discussions on the manuscript. We would like to thank Espen Ringvold for technical assistance during the experiments and John Fredriksen for donating the Task Force equipment to Rikshospitalet, Oslo University Hospital. Nathalie Holme was a student at the Medical Student Research Program at the University of Oslo. The study received funding from the Research Council of Norway (Grant No. 230354).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Additional information
Communicated by Massimo Pagani.
Rights and permissions
About this article
Cite this article
Holme, N.L.A., Rein, E.B. & Elstad, M. Cardiac stroke volume variability measured non-invasively by three methods for detection of central hypovolemia in healthy humans. Eur J Appl Physiol 116, 2187–2196 (2016). https://doi.org/10.1007/s00421-016-3471-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-016-3471-2