Abstract
Aims
Combined head up tilt (HUT) and lower body negative pressure (LBNP) can be used to exploit the full spectrum of cardiovascular control mechanisms and to reveal characteristics of individual blood pressure control. We studied whether the response to combined HUT and LBNP was reproducible within subjects and whether characteristic response patterns could be distinguished between different subjects.
Materials and methods
Ten healthy young males were subjected to combined HUT and graded LBNP to achieve a presyncopal end point in four tests, each separated by more than 2 weeks. Heart rate, blood pressure and thoracic impedance were monitored, cardiac output and peripheral vascular resistance were computed.
Results
From supine control to presyncope, heart rate, mean arterial blood pressure, pulse pressure and stroke index changed as expected. The time courses of heart rate and stroke volume as well as orthostatic tolerance times (15 ± 6 to 18 ± 7 minutes, n.s) appeared reproducible between trials within subjects but different between different subjects.
Conclusion
LBNP-tilt approach was repeatable in time and pattern. Furthermore, differences observed between subjects indicated preferred activation of selected pathways of blood pressure control in different individuals while at the same time, reproducibility measured within the same subject showed that preferential mechanisms were highly conserved within the same individual. These characteristics are a prerequisite to use the combined graded orthostatic paradigm for hemodynamic testing and identification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Combined head-up tilt (HUT) and lower body negative pressure (LBNP) induce cardiovascular and neuroendocrine changes, which depend on stress intensity and duration. The initial effects of upright posture occur due to fluid shifts related to hydrostatic changes. Because the arterial hydrostatic indifference point between supine and upright is located at heart level, and the venous hydrostatic indifference point below it [10], respectively, both carotid baroreceptor loading and cardiac filling are reduced upon assumption of an upright position. The firing rates from carotid and cardiopulmonary receptors decrease, medullary feedback patterns change and trigger neurohumoral responses, including sympathetic activation [22, 23, 32]. Additional LBNP diminishes cardiac preload even further [1, 6], so that the stimulus combination eventually leads to cerebral underperfusion and consequently a presyncopal situation.
The rationale of this study was to explore the combination of HUT and graded LBNP as an approach to identify potentially characteristic individual cardiovascular stress response patterns. A well-defined combined stress, therefore, would stimulate a reproducible response when repeated in the same subject while it would evoke different responses when applied to different subjects. It was not the aim to identify underlying physiological mechanisms causing a given response but to analyze the measured data by statistical means.
Materials and methods
Subjects
The study was done in healthy, non-obese, non-medicated and non-smoking males who were free from any somatic or mental condition as assessed in a medical exam before the test. The study criteria were met by ten subjects of 25 ± 3 years of age with a body mass of 75 ± 12 kg, a body height of 179 ± 6 cm, a heart rate of 65 ± 10 bpm at supine rest. To avoid effects of confounding variables such as height, gender, or athletic training on orthostatic tolerance [13], subjects had to be physically fit; their maximum specific power output was 4.3 ± 0.45 W/kg. In one subject, data were only available from 3 tests, as a result 39 test runs entered final analysis.
Each subject was studied 4 times with an interval of 2 weeks or more between tests. Subjects were told to refrain from vigorous exercise, smoking or alcohol during any part of the study. All subjects were advised to keep their fluid and salt intake according to their usual dietary habits [4, 35]. We, however, did not attempt to monitor sodium balance as sodium balance is a controversial issue which goes beyond classical concepts [34]; inter-compartmental sodium shifts occur from and to the interstitial (“third”) compartment which potentially invalidate the significance of day to day sodium input (dietary analysis) or output (urinary measurements), respectively [16, 33]. We have observed earlier that sodium intake (between 3 and 10 g NaCl per day) does not influence extracellular volume estimates from bioimpedance changes in normotensive men [17].
Subjects were familiarized with the test protocol and gave written informed consent to participate in the study. The study was approved by the Graz University Ethics Board and performed in accordance with the 1989 WMA Declaration of Helsinki.
Protocol
Experiments were carried out between 9 and 11 am in a semi-dark, quiet room maintained at 23–24°C and 50–55% humidity. The test persons were fasting and voided before commencement of the experiments.
Each experiment started with a 30-minute supine rest to acquire cardiovascular steady state conditions. At minute zero, the tilt table was brought to 70° head-up position. After five more minutes, −20 mmHg LBNP was added, and increased by 10 mmHg every 3 minutes. As soon as presyncopal signs or symptoms occurred, the table was brought back to 0° and LBNP was stopped at once. The criteria of presyncope were any of the following: (a) arterial blood pressure drop below systolic 80 mmHg or by ≥25 mmHg/minute, diastolic by ≥15 mmHg/minute, and/or heart rate decrease by ≥15 bpm, (b) lightheadedness, dizziness, visual disturbances, nausea, stomach awareness, clammy skin, excessive sweating, or skin pallor [18].
During the test, the subjects were instructed to avoid undue movements of the lower limbs and to breathe normally. Test persons were secured and had access to an emergency shutdown (automatic return to supine and pressure neutralization) at all times.
Perturbation
The test was carried out at the Institute of Adaptive and Spaceflight Physiology (http://www.meduni-graz.at/iap/AHST.htm) using a tiltable LBNP chamber equipped with a footrest. The sealing was maintained at the iliac crest, as sealing position has been shown to affect hemodynamic responses [12]. The transition from supine to upright position as well as changes in the chamber pressure buildup were completed within 10 seconds. Suction was provided using a commercially available vacuum cleaner located in an adjacent room. The execution of the pre-programmed test protocol and synchronous recording of all data from the cardiovascular monitoring system was managed by LabView®.
Measurements
Electrodes were placed at the neck and thoracic regions, the latter specifically at the midclavicular line at the xiphoid process level [8]. Continuous hemodynamic monitoring included blood pressure, heart rate (3-lead ECG), and thoracic impedance (Task Force Monitor®, CNSystems, Graz, Austria). Total peripheral resistance index (TPRI) was calculated as mean arterial blood pressure/cardiac index [14]. Thoracic impedance (TI) was used to estimate changes in thoracic fluid content [29].
Sample size and analysis of data
Sample size
Means and standard deviations of orthostatic tolerance times were calculated from previous studies [9, 22, 23]. Using these values in an online power and sample size calculator http://biostat.mc.vanderbilt.edu/twiki/bin/view/Main/PowerSampleSize), the number of subjects required, for an 80% test power, was n = 10. All data are presented as mean ± SD. Significance was assumed for an alpha error probability <0.05.
Cross-correlation (CC) analysis was used to assess reproducibility of heart rate and stroke volume responses as a function of time, as well as heart rate to stroke volume relationships comparing consecutive trials per person using Matlabs XCORR algorithm. This algorithm produces an estimate of the correlation between two random sequences:
XCORR, an unbiased estimator, normalizes the sequence so that the autocorrelations at zero-lag are equal to unity (MatLab R2007a, The MathWorks Inc.).
To characterize the non-linear dynamic features of the test by appropriate statistical means, datasets were created from the original signal by computing the Fourier transform and randomizing the imaginary part in the frequency domain. Following this randomization in the frequency domain, data were then transformed back to the time domain by inverse Fourier transformation. Such data have the same mean, standard deviation, and power spectrum as the original data [33] and can be used as so-called “surrogate” data for statistical analysis. For every original dataset, 100 such datasets were calculated and correlated with the original signal. The 95th percentile of the correlation coefficient of this comparison was then used to reject the null hypothesis, namely that there was no difference between a random signal produced by the original trial and a signal from another trial. Comparisons were done using a paired t test. Thus, if the correlation coefficient of the 95th percentile (taking in account alpha error p < 0.05) of the randomized signal was lower than the correlation coefficient in another trial, the differences between runs were more likely to be due to physiological mechanisms than to the randomization itself.
As orthostatic tolerance was different between subjects, intra-individual responses were studied using data 64 seconds before HUT commencement and 64 seconds preceding a fully completed LBNP run.
Baseline and presyncopal hemodynamic variables shown are calculated for a time frame of 60 seconds before graded orthostatic stress and before presyncope.
Coefficient of variation (CV, in percent) was used for comparing the degree of variation of one data series to another (that is, inter-individual and intra-individual variabilites).
Results
From supine control to presyncope, heart rate increased from 65 ± 10 to 141 ± 20 bpm, mean arterial blood pressure dropped from 90 ± 10 to 76 ± 12 mmHg, pulse pressure from 51 ± 9 to 30 ± 9 mmHg, stroke index from 53 ± 8 to 27 ± 3 ml/m2 and total peripheral resistance index from 2130 ± 655 to 1560 ± 403 dyne second m2/cm5, respectively (all changes p < 0.05).
Thoracic impedance, measured from the last 60 seconds of baseline to 60 seconds preceding presyncope, increased from 28 ± 5 (CV of 7 ± 3%) to 33 ± 5 (CV of 6 ± 1%) Ohms (all persons across 4 trials). Inter-individual range of the thoracic impedance in these two phases was 23–35 (CV 6 ± 4%) and 27–41 (CV 6 ± 3%), respectively.
Individual orthostatic tolerance, quantified as the time from HUT to the development of presyncopal signs or symptoms, ranged from 8.4 to 30.0 minutes for all persons across 4 trials (Fig. 1). For the whole group, the tolerance time was 16.4 ± 6 minutes with a CV of 14.5 ± 4.9%.
Orthostatic tolerance (quantified as the time from tilting until presyncope) in all subjects across all trials. Each dot represents a trial and the line between the dots is the individual mean orthostatic tolerance, respectively. In subject E, only three runs are shown (as in the first trial a machine failure occurred and presyncopal state was not reached)
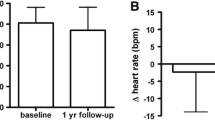
Orthostatic tolerance was quite different between persons, but well reproducible on an individual basis across trials. Repetitions of the trials did not seem to influence orthostatic tolerance from the 1st to the 4th trial (15 ± 6 to 18 ± 7 minute, n.s.). However, the CV between the subjects in the trials ranged from 7.9 to 20.6%.
Figures 2 and 3 demonstrate, for two individuals (I and J), different patterns of heart rate and stroke volume time course during graded orthostatic stress leading to syncope as a typical example. In test subject I, heart rate (panel 2a) and stroke volume (panel 2b) changed rather steadily during the protocol.
Heart rate and stroke volume during different stages of the four trials in person J. Panels as in Fig. 2
In contrast, subject J increased heart rate and reduced stroke volume in a stepwise fashion at the beginning of orthostasis (Fig. 3).
Heart rate and stroke volume were inversely related in all persons (Table 1).
While in some subjects values of heart rate and stroke volume appeared to be rather homogeneously distributed along the inverse heart rate to stroke volume relationship (e.g. subject I, Fig. 2), data appeared to be heterogeneous and clustered in other subjects (for example subject J, Fig. 3).
Reproducibility with regard to heart rate and stroke volume responses (Tables 2 and 3, respectively) was measured among different trials (1, 2, 3 and 4) by cross correlation (CC). T-tests for CC1,2 versus CC1,S, CC1,3 versus CC1S, etc., resulted in p values <0.001 for all comparisons to the surrogate data.
Discussion
Using the combined orthostatic stress paradigm, our cardiovascular stress protocol resulted in reproducible heart rate and stroke volume responses across persons. The close reproducibility of heart rate and stroke volume, when individual trials are separated by at least 2-week intervals, suggests surprisingly consistent physiological order within individual subjects. Strategies for maintaining blood pressure in orthostatically induced central hypovolemia, were different between subjects, but specific hemodynamic mechanisms were employed each time to maintain blood pressure within subjects.
The major finding of this study was that physiological reproducibility in heart rate and stroke volume differed from the “surrogate” data across the trials. By comparing surrogate data with original ones across trials, we concluded that the correlation between trials was higher than between trial and surrogate data from the trial. This confirmed that physiological reproducibility in heart rate and stroke volume differed from the simulated “surrogate” data across the trials thus suggesting that these represented real physiological responses rather than by chance [2].
Syncope is a common clinical condition. It can arise in normal subjects on standing up from a supine, or crouched, position or on return from the microgravity environments of bed rest or spaceflight. In physiological terms, typical syncope develops because cardiac preload critically decreases due to low venous blood return. This ultimately reduces brain perfusion below a certain level, which triggers a “neurocardiogenic” reflex response (“vasovagal attack”) that reduces heart rate, cardiac output, and consequently blood pressure [28]. Presyncope is a state immediately preceding a syncopal event, defined as a sudden, transient loss of consciousness that is specifically due to decreased cerebral perfusion [21].
We intended to investigate the full range of cardiovascular stress response up to the point when syncope is imminent. During simulated spaceflight missions and to study etiologies of syncope in clinical practice, it is necessary to create and to deal with situations that produce high levels of cardiovascular stress. Combined HUT and LBNP have been used—sometimes as a surrogate for centrifuge rides—to study features of cardiovascular and humoral regulation under severe stress conditions and to induce presyncopal signs and symptoms [6, 20, 24, 30]. Previously, we have also used combined orthostatic stress to observe sex-based differences in the neurohormone galanin [18] and cardiovascular effects of Chinese herbs [9]. The advantage of combined graded orthostatic stress is the absence of medication to induce syncope. For example, in nitroglycerin induced vasovagal syncope studies [11] the effects of this drug on the cardiac output make it difficult to ascertain what would be the hemodynamic responses in subjects who are healthy or not on this medication. Furthermore, we avoided intravenous cannulation, which has been shown to spuriously affect cardiovascular responses and orthostatic tolerance [31].
Neurally mediated syncope is presumably a result of venous blood pooling in the lower body [26]. Central hypovolemia induced by the combined HUT and graded LBNP observed in our study is similar to what has been reported [27]. Parasympathetic traffic between heart and brainstem interferes with sympathetic activity, resulting in a drop in peripheral vascular resistance and heart rate [26]. Blood pressure decreased in the last 60 seconds before presyncope in all of our ten test subjects, and in all runs, which is in agreement to previous findings [6, 20, 24]. Brown et al. [3] found a decay in the stress induced increase of total peripheral resistance (TPR) falling from 40% at 2 minutes of stress to 20% in 1 minute before presyncope occurred. In our study, TPRI was 27% below supine control when presyncope was reached (a significant result, pointing toward a rather homogenous response pattern in this group of subjects). This indicates that peripheral vasoconstriction protected arterial pressure as long as sympathetic activity was high. When syncope became imminent, a loss in TPR occured fairly quickly.
Orthostatic tolerance has been studied using vasodilators, body tilt and/or LBNP under various circumstances [7, 11, 19]. Orthostatic tolerance times within our subjects were neither extremely short nor particularly long (Fig. 1). Depending on individual characteristics, this stress elicited a wide range of orthostatic tolerance times and heart rate to stroke volume relationships when measured in a group of healthy individuals. However, the response re-examined in the same individual was highly reproducible. It is possible that the lack of difference observed in our study could be attributed to the minimization of several confounding variables in our study such as age, height, gender and duration of LBNP at specific levels. In our protocol, test subjects reached presyncope much faster than those in other studies did and it is possible that this could have led to this highly reproducible pattern in the responses.
Reproducibility of LBNP tolerance has been demonstrated when the same protocol was used at the same time of day [19]. These investigators also reported that subjects adapted to repeated LBNP sessions with increased LBNP tolerance on the third successive exposure. This was also confirmed in another study [5] that demonstrated an increase in tolerance times following one week of tilt training in patients. Conversely, applying graded orthostatic stress to the same subjects four times, separated by 72 hours [25] or two weeks (Goswami et al. 2008, unpublished observations) demonstrated no differences in the tolerance times to presyncope across trials. Since no objective end point exists for an LBNP tolerance it is possible that some differences between studies can be attributed to ambiguity associated with LBNP tolerance end point determination [19] or to a lay-off effect when tests are more than one week apart. For example, aircrews that have not flown at high gravitational acceleration G for a week develop a reduction in G tolerance on return to flying [15].
There is a variety of efferent pathways to control blood pressure, and the gains for the various actuators such as heart rate, cardiac contractility, venous compliance, and peripheral resistance can be different to reach the same goal. Heart rate and stroke volume responses across the trials showed high reproducibility across the entire graded orthostatic stress in all the persons. However, the rate of increases or decreases in these variables showed clear inter-individual differences. From Figs. 2 and 3, it can be seen that these two persons apparently maintained blood pressure in a different way despite having similar orthostatic tolerance times. To maintain blood pressure and cardiac output in some persons, for example, both heart rate and total peripheral resistance increased during the orthostatic stress (while stroke volume showed drastic reductions during HUT) while in others the fall in stroke volume was more gradual across the entire protocol and these persons responded by heart rate increases alone, with minimal change in total peripheral resistance. These patterns appeared to be typical for individual persons.
Limitations
It appeared that the orthostatic tolerance in trial 4 was longer than trial 1 for most subjects thus suggesting that some degree of physiological adaptation to the orthostatic stress actually existed. Considering that this indicated different stages of LBNP the reproducibility may appear less remarkable and needs to be considered in follow up studies. However, statistically we did not observe any differences in the tolerance over the trials. It is possible that we were unable to statistically demonstrate its existence due to our small sample size.
More pattern combinations than those observed in this study might exist, including differences according to gender, age, or ethnic origin. This study was carried out in healthy subjects with no history of syncope, and it cannot be ruled out that in diseased persons the cardiovascular system operates differently, with a possible resetting of baroreceptor reflexes or changed sensitivities due to medications which act at receptor level, such as beta blockers or angiotensin-2 antagonists. More studies are needed to understand potential differences between the developments of syncope in healthy persons vs. patients with a medical history of orthostatic instability.
Conclusions
Our data, using the method of surrogate data analysis, suggested that the combined HUT/LBNP stress paradigm reveals individually reproducible presyncopal stress response patterns and provides a promising technique for further analysis of cardiovascular control mechanisms.
No long-term (≥2 weeks) ‘learning effect’ was found, suggesting that the protocol used in this study might be useful as a standard tool for longitudinal studies of orthostatic competence. This can be of particular interest for clinical investigations where the goal is to evaluate drug effects on cardiovascular stability without involving additional (e.g. syncope-enhancing) agents and where cross-influence between drugs might blur properties of the treatment to be tested in the first place.
The combined orthostatic stress paradigm might give similar insight into individual cardiovascular stability as that attained by human centrifuge runs, albeit, with much lower operational demands. The test could also be used to develop algorithms for analysis of circulatory system parameters in healthy persons such as astronauts or in diseased persons. However, as indicated by the high intra-individual coefficient of variation across orthostatic tolerance times, caution must be observed when interpreting data especially in subjects undergoing repeated syncope or experimental interventions with novel medications.
References
Al-Shamma YM, Hainsworth R (1987) A quantitative comparison of the circulatory responses in humans to graded upright tilting and lower body negative pressure. In: Hainsworth R, McWilliam PG, Mary DASG (eds) Cardiogenic reflexes. Oxford University Press, New York, pp 431–433
Blaber AP, Yamamoto Y, Hughson RL (1995) Methodology of spontaneous baroreflex relationship assessed by surrogate data analysis. Am J Physiol Heart Circ Physiol 37:H1682–H1687
Brown CM, Hainsworth R (2000) Forearm vascular responses during orthostatic stress in control subjects and patients with posturally related syncope. Clin Auton Res 10:57–61
Cooper VL, Hainsworth R (2002) Effects of dietary salt on orthostatic tolerance, blood pressure and baroreceptor sensitivity in patients with syncope. Clin Auton Res 12:236–241
Ector H, Reybrouck T, Heidbuchel H (1998) Tilt training: A new treatment for recurrent neurocardiogenic syncope and severe orthostatic intolerance. Pace Pacing Clin Electrophysiol 21:193–196
El-Bedawi KM, Hainsworth R (1994) Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res 4:41–47
Evans JM, Stenger MB, Moore FB, Hinghofer-Szalkay H, Rossler A, Patwardhan AR (2004) Centrifuge training increases presyncopal orthostatic tolerance in ambulatory men. Aviat Space Environ Med 75:850–858
Fortin J, Habenbacher W, Heller A, Hacker A, Gruellenberger R, Innerhofer J (2006) Non-invasive beat-to-beat cardiac output monitoring by an improved method of transthoracic bioimpedance measurement. Comput Biol Med 36:1185–1203
Gao Y, Goswami N, Grasser E, Roessler A, Stoeger E, Hinghofer-Szalkay H (2008) Radix Astragali and orthostatic response: a double masked crossover study. Aviat Space Environ Med 79:8–94
Gauer OH, Thron HL (1965) Postural changes in the circulation. In: American Physiological Society (eds) Handbook of physiology—Circulation III. Bethesda, MD, pp 2409–2439
Gisolf J, Westerhof BE, Van Dijk N, Wesseling KH, Wieling W, Karemaker JM (2004) Sublingual nitroglycerin used in routine tilt testing provokes a cardiac output-mediated vasovagal response. J Am Coll Cardiol 44:588–593
Goswami N, Grasser E, Roessler A, Schneditz D, Hinghofer-Szalkay H (2008) The cardiovascular response to lower body negative pressure in humans depends on seal location. Physiol Res (Epub ahead of print)
Goswami N, Loeppky J, Hinghofer-Szalkay H (2008) LBNP: past protocols and technical considerations for experimental design. Aviat Space Environ Med 79:459–471
Gratze G, Rudnicki R, Urban W, Mayer H, Schlogl A, Skrabal F (2005) Hemodynamic and autonomic changes induced by ironman: prediction of competition time by blood pressure variability. J Appl Physiol 99:1728–1735
Green NDC (2006) Effects of long-duration acceleration. In: Rainford DJ, Gradwell DP (eds) Ernsting’s aviation medicine. Edward Arnold, New York, pp 137–158
Heer M, Baisch F, Kropp J, Gerzer R, Drummer C (2000) High dietary sodium chloride consumption may not induce body fluid retention in humans. Am J Physiol Renal Physiol 278:F585–F595
Hinghofer-Szalkay HG, Laszlo Z, Passath H, Pilz K, Rossler A, Jezova D, Scharfetter H (2004) Sodium intake does not influence bioimpedance derived extracellular volume loss in head-down rest. Aviat Space Environ Med 75:1036–1041
Hinghofer-Szalkay HG, Roessler A, Evans JM, Stenger MB, Moore FB, Knapp CF (2006) Circulatory galanin levels increase several fold with intense orthostatic challenge in healthy humans. J Appl Physiol 100:844–849
Howden R, Tranfield PA, Lightfoot JT, Brown SJ, Swaine IL (2001) The reproducibility of tolerance to lower-body negative pressure and its quantification. Eur J Appl Physiol 84:462–468
Julu PO, Cooper VL, Hansen S, Hainsworth R (2003) Cardiovascular regulation in the period preceding vasovagal syncope in conscious humans. J Physiol Lond 549:299–311
Kapoor WN (2000) Primary care—syncope. N Engl J Med 343:1856–1862
Laszlo Z, Rössler A, Hinghofer-Szalkay HG (1998) Cardiovascular changes during and after different LBNP levels in men. Aviat Space Environ Med 69:32–39
Laszlo Z, Rössler A, Hinghofer-Szalkay HG (2001) Cardiovascular and humoral readjustments after different levels of head-up tilt in humans. Aviat Space Environ Med 72:193–201
Lelorier PK, Krahn G, Raymond A, Skanes A, Shoemaker KJ (2003) Combined head-up tilt and lower body negative pressure as an experimental model of orthostatic syncope. J Cardiovasc Electrophysiol 14:920–924
Lightfoot JT, Hilton F, Fortney SM (1991) Repeatability and protocol comparability of presyncopal symptom limited lower body negative pressure exposures. Aviat Space Environ Med 62:19–25
Lurie KG, Benditt D (1996) Syncope and the autonomic nervous system. J Cardiovasc Electrophysiol 7:760–776
Matzen S, Perko G, Groth S, Friedman DB, Secher NJ (1995) Blood volume distribution during head up tilt induced central hypovolemia in man. Clin Physiol 11:411–422
Mosqueda-Garcia R, Furlan R, Tank J, Fernandez-Violante R (2000) The elusive pathophysiology of neurally mediated syncope. Circulation 102:2898–2906
Perko G, Payne G, Secher NH (1993) An indifference point for electrical-impedance in humans. Acta Physiol Scand 148:125–129
Stenger MB, Evans JM, Patwardhan AR, Moore FB, Hinghofer-Szalkay H, Roessler A, Ziegler MG, Knapp CF (2007) Artificial gravity training improves orthostatic tolerance in ambulatory men and women. Acta Astronautica 60:267–272
Stevens PM (1966) Cardiovascular dynamics during orthostasis and influence of intravascular instrumentation. Am J Cardiol 17:211–218
Stewart JM, Meadow MS, Montgomery LD (2003) Local vascular responses affecting blood flow in postural tachycardia syndrome. Am J Physiol Heart Circ Physiol 285:2749–2756
Theiler J, Eubank S, Longtin A, Galdrikian B, Farmer JD (1992) Testing for non-linearity in time series: the method of surrogate data. Physica D 58:77–94
Titze J (2008) Water-free Na+ retention: Interaction with hypertension and tissue hydration. Blood Purif 26:95–99
Wieling W, Lieshout Van, Hainsworth R (2002) Extracellular fluid volume expansion in patients with posturally related syncope. Clin Auton Res 12:242–249
Acknowledgments
We thank the volunteers for their time, patience, and collaboration in participating in this study. This study was supported by the Austrian Research Promotion Agency (FFG project 817086 ‘Orthocap’).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goswami, N., Roessler, A., Lackner, H.K. et al. Heart rate and stroke volume response patterns to augmented orthostatic stress. Clin Auton Res 19, 157–165 (2009). https://doi.org/10.1007/s10286-009-0001-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-009-0001-x