Abstract
The objective of this study was to examine the effect of experimental knee-related pain on postural control. Twelve healthy subjects stood as quietly as possible on a movable force platform (that measured the centre of pressure and provided fast perturbations) before, during, and after experimental knee-related pain. Lower limb electromyographic (EMG) activity and joint angles were measured. Experimental pain was induced by injecting hypertonic saline into the infrapatellar fat pad (unilateral and bilateral) and isotonic saline was used for control sessions. Compared with the baseline and control sessions, unilateral and bilateral knee-related pain during quiet standing evoked (1) an increased sway displacement in the anterior–posterior direction (P < 0.05), (2) larger knee flexion (P < 0.05), and (3) larger EMG changes. Bilateral pain also induced (1) larger medial–lateral sway displacement and speed (P < 0.05) and (2) larger left hip flexion (P < 0.05). During forward perturbations, subjects leaned forward during both painful conditions when compared with baseline (P < 0.05). The additional impairment by bilateral pain suggests that the non-painful limb in unilateral pain conditions compensates for the impaired postural control. These results show that knee-related pain impairs postural stability during quiet standing, indicating the vulnerability of patients with knee pain to falls. This measure could potentially help clinicians who seek to assess how pain responses may contribute to patient’s postural control and stability during quiet standing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain in elderly population has been estimated to be 10–71% (McAlindon et al. 1992). Osteoarthritic (OA) pain around the knees is one of the most common pain conditions (Davis 1988; Felson 1988) with potential impaired knee proprioception and postural stability (Hinman et al. 2002; Messier et al. 2002; Wegener et al. 1997) and, consequently, an increased risk of falling (Blyth et al. 2007; Foley et al. 2006; Leveille et al. 2002; Yagci et al. 2007).
The main task in postural control is to maintain the body’s projection of the centre of gravity (COG) within the base of support delimited by the feet, therefore maintaining upright posture. Once beyond the base of support boundaries, the COG position generates forces that destabilize the body and, therefore, requires additional strategies to avoid falls. In general, healthy subjects easily recover their balance after destabilization of the body; however, in the presence of pain, healthy subjects and patients showed impaired postural control, mainly reflected by increased body sway (Blouin et al. 2003; Corbeil et al. 2004; Foley et al. 2006; Hirata et al. 2010, 2011; Pradels et al. 2011; Vuillerme and Pinsault 2009).
Although several studies have shown that pain impairs balance in knee OA patients (Hinman et al. 2002; Wegener et al. 1997), alleviation of pain by anaesthetising the knee joint of these patients does not improve balance (Hassan et al. 2002). These controversial pain-related effects illustrate the complex scenario in knee OA patients, where the pain effects in association with additional confounding factors (structural changes in the joint, loss of muscular strength and proprioceptive impairments) impair balance (Hassan et al. 2001). It is also important to note that anaesthetising the joint will diminish the proprioceptive information from the knee which may also affect the balance. Efforts have been made to understand how the presence of pain per se around the knee joint changes postural control in healthy subjects by injecting hypertonic saline in muscles around the knee joint (Hirata et al. 2011) and in the infrapatellar fat pad (Bennell et al. 2004, 2005; Bennell and Hinman 2005; Hodges et al. 2009). The infrapatellar fat pad pain model is a good proxy for knee pain since the pain location is close to the medial part of the knee (Bennell et al. 2004). Additionally, this model allows one to understand the isolated effects of pain in a healthy system, where patients have other confounding factors, such as loss of strength, flexibility and mobility, interacting with pain effects when controlling posture (Wegener et al. 1997). Experimental muscle pain around the knee joint impaired postural control in healthy subjects, potentially indicating the importance of this joint in controlling posture (Hirata et al. 2011). However, only Bennell and Hinman (2005) tested the effect of experimental non-muscular knee-related pain on postural stability. The authors applied unilaterally experimental infrapatellar fat pad pain during quiet standing and external postural perturbations, eliminating possible confounding factors due to experimental pain (hypertonic saline) applied in the muscle tissue, such as excitation of other axons due to changes in intramuscular ion concentration or simply changes in muscle activity to avoid pain provocation during contraction (Hodges et al. 2009). No differences in the sway pattern during quiet standing or in the postural responses to floor perturbations were reported. The potential compensatory effect provided by the non-painful leg was a possible explanation for the absence of changed postural stability but was excluded by the authors. Clinically, most patients with knee OA report pain in both knees (White et al. 2011), and bilateral experimental infrapatellar fat pad pain could therefore provide a better understanding of the complex impaired behaviour of patients with knee OA when controlling the upright stance. Furthermore, most of falls happens when balance is challenged (Winter 1995) and therefore it is relevant to assess how bilateral knee-related pain affects body reactions after perturbations.
The aim of the present study was to investigate the effect of experimental infrapatellar fat pad pain (unilateral and bilateral) on postural sway (1) during quiet posture and (2) stability after controlled perturbations.
Methods
Subjects
Twelve healthy subjects (2 women) participated in this study. None of the subjects reported muscular, neurological, or other impairments that could affect postural control. The subjects were on average (standard deviation) 27 (5) years old and 177 (8) cm tall, and had 72 (13) kg of body mass. Subjects were given a detailed verbal explanation and signed an informed consent form. The study was conducted in accordance with the Helsinki Declaration and was approved by the local Ethics Committee (VN 20080022).
Protocol
This experiment was randomized, blinded, and placebo-controlled, and separated in two sessions (days) with at least 1 week between sessions. Four different experimental interventions were included (two in each session/day). Each session included six trials consisting of 1 min of quiet standing followed by ten random perturbations. The first and fourth trials served as the baseline recording for the following two trials defined as ‘during’ and ‘post-pain’ interventions (saline injection into the infrapatellar fat pad). Each intervention was separated by at least 1 h, and its corresponding post-pain trial was not initiated until the pain from the previous intervention had vanished (VAS equal to 0).
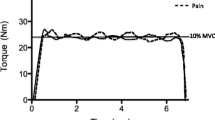
Subjects stood on a movable force platform that could be translated quickly. Each trial began with recording of 1 min of quiet standing, and subsequently, ten translations of the force platform were imposed. The translations of the force platform were randomly assigned (5 forward and 5 backward, 10 cm displacement with a velocity of 25 cm/s) and applied once every 15 s, although the exact timing was varied to reduce subject’s anticipation (±5 s). The force platform remained in the translated position for 10 s, after which the platform returned to its initial position at a velocity of 2 cm/s. The subjects were instructed to ‘stand as quietly as possible’ while looking at a fixed point (cross 10 × 10 cm) located 4 m in front of them. They were instructed to recover their balance as fast as possible after the perturbation and could take a step if necessary to avoid a fall.
The centre of pressure (COP), ankle, knee, and hip angles, and bilateral surface electromyography (EMG) from back and leg muscles were recorded or calculated.
Experimental muscle pain
Injections of sterile hypertonic saline (0.2 ml, 6%) or isotonic saline (0.2 ml, 0.9%) were administered in the right or both (left and right) infrapatellar fat pads: (1) bilateral hypertonic injection (each injection separated by 5–10 s), (2) bilateral isotonic injection (each injection separated by 5–10 s), (3) unilateral (right knee) hypertonic injection, and (4) unilateral (right knee) isotonic injection. During the injection, the subjects remained seated on a chair with the knees flexed at 90º. After the fat pad region was palpated, a 25-gauge needle mounted in a 1-ml syringe was inserted at an angle of 45° in a superolateral direction to a depth of approximately 10 mm (Bennell et al. 2004). The subjects were submitted two different injection paradigms per day, and the order of injections was randomized and blinded (type of saline) to the subject.
The experimental pain intensity was assessed on a 10-cm electronic visual analogue scale (VAS) with an external handheld slider to adjust the scale. The VAS was anchored with ‘no pain’ and ‘maximum pain’, 0 and 10 cm, respectively. The signal from the VAS was recorded during the entire trial (sample frequency of 1 Hz). The mean VAS score for the 1 min of quiet standing and 15 s during the perturbed trials was extracted. The subjects were asked to update the VAS score only between trials where no data were acquired until the next warning signal was triggered. In this way, movements from the VAS slider did not affect the postural sway measurements. Furthermore, after completion of each painful condition, the subjects were asked to score the average pain intensity on the VAS for each knee and to report if the pain was located around the knee join, shank or thigh.
Centre of pressure
The subjects stood barefoot and adopted a standard position with their feet comfortably positioned side-by-side (about shoulder-width apart), while standing on the moveable force platform (Doornik and Sinkjaer 2004). The position of the feet was marked with tape to ensure that the subjects always used the same position over all trials. The arms were positioned in front of the body, and both hands held the slider for the VAS.
The ground reaction forces and torques were used to calculate the COP position. The ground reaction forces and torques were recorded with a moveable force platform (AMTI, USA), amplified, low-pass filtered at 10 Hz, and sampled at 1 kHz. For the quiet standing and posture perturbation condition, sway displacement and speed in both directions (anterior–posterior and medial–lateral), sway area (Takagi et al. 1985), and the distance from the mean COP position (both directions) in relation to the baseline COP position were estimated. Sway performance in the anterior–posterior direction after perturbation was estimated using the time returning to an equilibrium position proposed by Horak et al. (1989) where the time returning to an equilibrium point was identified as the time point when the COP changed the displacement direction, i.e. provoking a peak in the sway displacement that was identified automatically. Furthermore, during perturbations the COP range and COP speed were calculated. Using a time window of 5 s (starting from 500 ms before the perturbation onset) the mean COP position in the anterior–posterior direction was estimated.
EMG recordings
Surface EMG was recorded bilaterally with bipolar pairs of electrodes (Neuroline 72001-k; AMBU, Denmark) from the tibialis anterior, medial gastrocnemius, soleus, vastus lateralis, vastus medialis, biceps femoris, and erector spinae muscles. The electrodes were placed in the direction of the fibres, after the skin was prepared (shaved and cleaned), according to the SENIAM recommendations (Hermens et al. 2000). The EMG signals were amplified with a gain of 2,000 (EMG-USB, LISiN; OT Bioelettronica, Turin, Italy), band-pass filtered (4th order Butterworth filter, bandwidth 10–450 Hz), sampled at 2,048 Hz, and A/D converted to a 12-bit representation. The EMG signals were full-wave rectified and low-pass filtered (Butterworth, 2nd order, 10 Hz cut-off frequency) to generate the enveloped EMG signal.
For quiet standing posture (50 s, the first 5 and last 5 s were discarded), the root-mean-square (RMS) value was extracted from the enveloped EMG signal. In the perturbed standing posture (the first 4 s from each of the 10 perturbations), the RMS value, peak-value, onset, and time to peak activity were extracted from the enveloped EMG signals. The time to activation onset was extracted automatically and identified when the activation exceeded the threshold of two standard deviations from the pre-perturbation RMS value (5 s preceding the perturbation). In addition, it was required that the activation be sustained above the threshold for 25 ms. For comparison between multiple sessions, the EMG data were normalized to the baseline values of each session. For both conditions, quiet standing and perturbed standing, the integrated EMG (iEMG) was calculated in its respective window (same as used for RMS) using a trapezoidal function on the enveloped EMG.
In addition, for each muscle the absolute percentage iEMG difference between the pain and the baseline condition was extracted (deltaEMG), and these were averaged across all muscles for each subject (defined as total-deltaEMG). Pain leads to adaptations in multiple levels of the motor system, such as changes in the excitability of the cortex, afferents, and efferent neurons (Hodges and Tucker 2011). The final motor output in presence of pain is dependent of all these changes and may vary between individuals. The deltaEMG accounts for the individual muscular activation changes according to the baseline condition, although it does not allow an increase to be distinguished from a decrease in the muscular activation.
Joint angles
Twenty-six reflective markers were attached bilaterally to the lower limb (pelvis, femur, tibia/fibula, and foot) according to descriptions by Cappozzo et al. (1995), acquired (sampling rate of 500 Hz) by eight infrared cameras (Oqus, Qualysis Motion Capture System, Sweden), and digitalised (Motion Track Manager, version 2.5, Sweden). The joint angles in the joint coordinate system were calculated bilaterally for the hip, knee, and ankle joints (Grood and Suntay 1983; Wu et al. 2002). The signals were low-pass filtered (5 Hz), amplified (1,000–10,000), and sampled at 1 kHz. The joint angle velocity and acceleration were extracted as the first and second derivative of the joint angle position, respectively, after additional low-pass filtering (5 Hz) for each derivation. For the quiet standing, the mean angular position and mean velocity were calculated. Additionally, for the perturbed standing, range of motion, maximum angular speed, and time for maximum angular speed were also extracted. The ankle joint was normalized at 90°; positive values represent dorsal flexion, and negative values represent plantar flexion. For the knee joint, 180° was used as the reference to normalize the angles; positive values represent knee flexion, and negative values are knee extension. Positive values in the hip joint represent flexion in relation to a 180° reference, and negative values represent extension.
Statistics
Only perturbation trials where subjects lost the balance and took a step to avoid falling were excluded from the analysis. The data are presented as the mean and standard error of the mean (SEM). A two-way repeated measurement analysis of variance (RM-ANOVA) was used to analyse all sway and joint position parameters. The first factor was the injection paradigm with four levels (bilateral hypertonic, bilateral isotonic, unilateral hypertonic, and unilateral isotonic). The second factor was time with three levels (before, during, and post-pain). For EMG parameters, two-way RM-ANOVA was used for each muscle with the same factors as above. For the total-deltaEMG parameter, two-way RM-ANOVA was used with the first factor with four levels (bilateral hypertonic injection, bilateral isotonic, unilateral hypertonic, and unilateral isotonic) and the second factor with two levels (during pain and post-pain conditions). When the VAS data were analysed, the second factor was time with ten levels (perturbation). In the case of a significant RM-ANOVA, the Newman–Keuls (NK) post hoc test was used to perform multiple comparisons. Pearson’s correlation analysis was performed between the pain intensity scores and the variables that were significantly affected during the pain conditions. Significance was accepted at P < 0.05.
Results
Pain perception
All painful injections induced pain around the knee join. The pain intensity (VAS scores) after the unilateral and bilateral hypertonic saline injections was higher than the control saline injections during quiet standing (Fig. 1a; RM-ANOVA: F(3,33) = 10.9, P < 0.001; NK: P < 0.01) and perturbations (Fig. 1b; RM-ANOVA: F(3,33) = 13.1, P < 0.001; NK: P < 0.01) with no interactions between the perturbations (time) and the injection paradigm, meaning no difference in pain intensity over time. Additionally, there was no difference in the pain intensity between unilateral (average VAS 4.8 ± 0.9 cm) and bilateral (4.5 ± 0.6 cm for the right knee and 4.2 ± 1.3 cm for the left knee) hypertonic saline injections.
Mean (+SEM, N = 12) VAS scores after infrapatellar fat pad injection of hypertonic and isotonic saline, unilaterally and bilaterally. a VAS scores during the 1-min quiet standing posture. b Mean VAS scores during ten perturbations. Significantly different from the respective control injections (*NK: P < 0.01)
Centre of pressure
Representative data can be seen in Fig. 2a. Compared with the baseline and control conditions, both painful conditions (unilateral and bilateral) increased medial–lateral sway displacement during the quiet standing task (Table 1; RM-ANOVA: F(6,66) = 3.5, P < 0.01; NK: P < 0.01). The bilateral painful injection also increased the sway speed in the medial–lateral and anterior–posterior directions (Table 1; RM-ANOVA: F(6,66) > 2.3, P < 0.04; NK: P < 0.01). The mean COP position relative to the baseline COP position in the medial–lateral direction was significantly shifted toward the left foot during the unilateral painful condition (right) compared with the other conditions (Table 1; RM-ANOVA: F(3,33) = 6.27, P = 0.002, NK: P < 0.01). Due to insufficient data, one subject had to be excluded in the sway analyses during perturbations. During forward perturbation, the mean COP position was shifted forward compared with baseline conditions for both painful conditions and control injection for bilateral painful condition (Fig. 3; RM-ANOVA: F(6,60) = 2.25, P ≤ 0.05, NK: P < 0.05).
Representative examples of COP trajectory, knee angle positions, and tibialis anterior muscles activities. a Bidimensional displacement of COP sway in the horizontal plane for bilateral pain (red, right side) and baseline control (blue, left side). b EMG envelope for the tibialis anterior muscle (right and left side) during bilateral pain and baseline control. c Knee flexion/extension angle (left and right side) in the joint coordinate system during bilateral pain and baseline control
Mean (+SEM, N = 11) COP position in the anterior–posterior direction during forward perturbations. During both painful conditions the subjects shifted their COP forward when compared with baseline conditions. Significantly different from the respective baseline and control (#NK: P < 0.01). Significantly different from the respective baseline (*NK: P < 0.01)
Muscle activity
Although 12 subjects participated in the study, three had to be excluded in the EMG analyses due to insufficient or corrupted data, leaving the EMG analyses with nine subjects. Analysis of the iEMG values across subjects did not reveal a consistent pattern in the muscle activity (e.g. no individual muscle showed increased muscle activity due to pain). However, during the quiet standing posture the total-deltaEMG (i.e. the average across all muscles of absolute EMG changes from baseline) was higher during bilateral painful injections when compared with the control and post-pain conditions (Fig. 4; RM-ANOVA: F(3,24) = 6.59, P < 0.01; NK: P < 0.05). Additionally, both tibialis anterior muscles showed higher deltaEMG during the bilateral hypertonic (painful) injection when compared with the post-pain and isotonic (control) injection (Table 2; RM-ANOVA: F(3,24) = 5.01, P < 0.01; NK: P < 0.05) during the quiet standing posture. Representative data for both tibialis anterior muscles can be seen in Fig. 2b.
Mean (+SEM, N = 9) total-deltaEMG index (the mean averaged absolute difference from baseline across all muscles) during quiet standing. Bilateral knee pain inflicted larger muscular activity changes compared with the control injection and the post-pain condition. Significantly different from the respective control injections (*NK: P < 0.01)
Knee and hip angle
During the pain conditions (unilateral and bilateral), the flexion in both knees was increased when compared with the baseline and control injections (Table 3; RM-ANOVA: F(6,66) > 2.5, P < 0.03; NK: P < 0.01). Representative data for the knee angle can be seen in Fig. 2c. During bilateral pain injection, the flexion in the left hip was increased when compared with the baseline and control injections (Table 3; RM-ANOVA: F(6,66) > 2.5, P < 0.05, NK: P < 0.01).
Discussion
During quiet standing, knee-related pain evoked larger sway displacement in the medial–lateral direction and higher sway speed in both directions (medial lateral and anterior posterior), altered both knee joint positions, and changed the general muscular activation, mainly pronounced in the tibialis anterior muscles.
Effect of knee-related pain on postural control during quiet standing
The present study applied a similar approach as Bennell and Hinman (2005), although the unilateral painful condition in the present study increased the postural sway in the medial–lateral direction. During this pain condition, the subjects flexed both knees (on average, 6° for the right injected knee and 2° for the left knee) when compared with the baseline. Furthermore, the subjects unloaded the right knee, observed by the shift in the mean COP position in the medial–lateral direction (leading to an asymmetrical position). Accordingly, a similar load/unload mechanism was observed during calf muscle pain (Hirata et al. 2010), where changes mainly in the medial–lateral direction were reported when the subjects leaned on the non-painful limb. No asymmetrical posture was reported by Bennell and Hinman (2005), which can explain the difference in the results from this present study since asymmetry per se has been shown to affect the COP amplitude and speed in both directions (Anker et al. 2008). The authors forced the subjects to adopt various asymmetrical weight-bearing positions guided by visual feedback of the subjects’ COP, therefore decreasing postural stability.
Enlarged postural sway in the medial–lateral direction and increased sway speed in both directions enlarged sway displacement in the anterior–posterior direction, increased knee and left hip flexion angles, and significant changes in the activity of both tibialis anterior muscles were found during bilateral knee-related pain when compared with the baseline and control injections. Unlike the unilateral knee pain condition, no significant difference in the COP mean position was found during bilateral knee pain, where the simple load/unload mechanism (asymmetry) cannot explain the changes observed in postural control during the bilateral knee pain. Instead of shifting the weight to one specific side, as observed in the unilateral pain condition, the subjects might alternatively have tried alternating the weight between sides in the bilateral pain condition in an attempt to decrease the pain. This asymmetry may also be related to asymmetry observed in the hip angles. During the double-injection condition, both hips were flexed (although only the left hip was significantly different) in comparison with the single injection that only showed a trend of higher hip flexion in the right side. Additionally, changes in the right knee were larger when compared with the left knee, probably indicating that subjects utilized mainly the right limb to compensate the impairments due to pain.
The presence of pain in knee osteoarthritis patients has been associated with impaired proprioceptive acuity in the knee joint (Felson et al. 2009; Hassan et al. 2001; Shakoor et al. 2008) leading to a more unstable posture when compared with healthy subjects. Experimental pain in healthy subjects has also been suggested to impair postural control via deficits in the sensorimotor mechanisms (Blouin et al. 2003; Corbeil et al. 2004; Hirata et al. 2010; Vuillerme and Pinsault 2009). Experimental pain applied in the thigh muscles, close to the knee joint, provoked changes in the postural control in healthy subjects during quiet standing and after perturbations, probably indicating the importance of the knee joint structures in controlling posture.
The VAS scores after the unilateral and bilateral pain conditions provoked similar pain intensity. The effect of the earliest injection of the bilateral pain condition could explain the similarity in pain intensity, when compared with the unilateral painful condition, due to diffuse noxious inhibitory controls (DNIC) effects. However, this effect is not likely to occur, since it would also be expected that the average VAS score from individual sides were different from the unilateral injection, which was not observed in the results. Additionally, the spatial summation effect due to the double injection (therefore increasing the pain intensity when compared with the single injection) would be expected if both injection sites were located close to each other (Graven-Nielsen et al. 1997), which is not the case in the present study. Bilateral knee pain induced impairments in postural sway accompanied by changes in muscular activity, although both unilateral and bilateral pain provoked comparable pain intensity, muscle activity, and kinematic adjustments. This may reveal that the non-painful limb provided enough sensory information to preserve the sway balance where the load/unloading mechanism found in this situation not only unloaded the non-painful knee, maybe partly relieving the pain, but also may reflect a re-weight sensory strategy (compensatory strategy) to optimize postural control in altered sensory environments (Oie et al. 2002) due to pain. This strategy would increase the gain of information from the healthy leg, therefore maintaining the balance.
The scenario of similar pain intensity following unilateral and bilateral painful injections, leading to different postural impairments in the two conditions may reflect the complexity and adaptability of the postural control in altered sensory environments, where isolated changes alone cannot explain changes observed in the postural sway. The dissociation between similar pain intensity perception and different pain-evoked postural changes may indicate the importance of the healthy leg (not painful) when controlling posture. Since pain may induce loss of proprioception (Djupsjobacka et al. 1995; Matre et al. 2002) the re-weighting strategy (Oie et al. 2002) can increase the gain of information from the non-affected areas providing correct information with regard to the position of the body in relation to the surroundings (therefore, maintaining the balance). In the present study, the overall muscle activity changes support that the task performed (quiet standing) has multiple degrees of freedom, allowing the subjects to maintain the posture using many different strategies, and therefore controlling the muscles in many different ways in presence of pain. Instead of a stereotypical change throughout all the subjects, pain seems to elicit increase, decrease or redistribution of the muscle activity while performing the task (Hodges and Tucker 2011). Additionally, both tibialis anterior muscles had significant changes during bilateral pain, perhaps the reason why only bilateral pain affected sway in the anterior–posterior direction, given that such muscles, together with ankle plantar flexors, control the sway in this direction (Winter 1995; Winter et al. 1996).
The shift in mean COP position found in both painful conditions during forward perturbation probably reflects an attempt to keep the body COG forward in the anterior–posterior direction. This strategy has been previously described when subjects aim to increase stability after forward perturbations (Lin and Woollacott 2002). Such strategy increases the distance between the COG and the posterior boundary of the base of support, allowing larger COG displacements after forward perturbations without losing balance or requiring major changes in the postural reactions (Lin and Woollacott 2002). In line with Bennell and Hinman (2005), no differences were found in postural responses after floor perturbations during experimental knee pain, perhaps also due to the low perturbation speed applied. With high-speed perturbations, Hirata et al. (2010, 2011) showed impairments in postural recovery in the presence of pain, once again indicating the consequence of the perturbation speed in the postural responses.
As expected, bilateral experimental knee-related pain impaired postural control during quiet standing more than unilateral injection, suggesting inappropriate changes in the motor control strategy and decreasing postural stability. The results support the importance of information from the non-painful knee joint in quiet standing control in the presence of pain, suggesting that clinical approaches to reduce pain may lead to improvements in balance, especially for people with knee pathologies, such as OA.
Reference
Anker LC, Weerdesteyn V, van Nes IJ, Nienhuis B, Straatman H, Geurts AC (2008) The relation between postural stability and weight distribution in healthy subjects. Gait Posture 27:471–477
Bennell KL, Hinman RS (2005) Effect of experimentally induced knee pain on standing balance in healthy older individuals. Rheumatology (Oxford) 44:378–381
Bennell K, Hodges P, Mellor R, Bexander C, Souvlis T (2004) The nature of anterior knee pain following injection of hypertonic saline into the infrapatellar fat pad. J Orthop Res 22:116–121
Bennell K, Wee E, Crossley K, Stillman B, Hodges P (2005) Effects of experimentally-induced anterior knee pain on knee joint position sense in healthy individuals. J Orthop Res 23:46–53
Blouin JS, Corbeil P, Teasdale N (2003) Postural stability is altered by the stimulation of pain but not warm receptors in humans. BMC Musculoskelet Disord 4:23
Blyth FM, Cumming R, Mitchell P, Wang JJ (2007) Pain and falls in older people. Eur J Pain 11:564–571
Cappozzo A, Catani F, Croce UD, Leardini A (1995) Position and orientation in space of bones during movement: anatomical frame definition and determination. Clin Biomech (Bristol, Avon) 10:171–178
Corbeil P, Blouin JS, Teasdale N (2004) Effects of intensity and locus of painful stimulation on postural stability. Pain 108:43–50
Davis MA (1988) Epidemiology of osteoarthritis. Clin Geriatr Med 4:241–255
Djupsjobacka M, Johansson H, Bergenheim M, Wenngren BI (1995) Influences on the gamma-muscle spindle system from muscle afferents stimulated by increased intramuscular concentrations of bradykinin and 5-HT. Neurosci Res 22:325–333
Doornik JV, Sinkjaer T (2004) Hydraulically actuated platform for human gait and posture analysis. In: Second international conference on biomechanical engineering (IASTED), Austria
Felson DT (1988) Epidemiology of hip and knee osteoarthritis. Epidemiol Rev 10:1–28
Felson DT, Gross KD, Nevitt MC, Yang M, Lane NE, Torner JC, Lewis CE, Hurley MV (2009) The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum 61:1070–1076
Foley SJ, Lord SR, Srikanth V, Cooley H, Jones G (2006) Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian Older Adult Cohort study. Osteoarthr Cartil 14:533–539
Graven-Nielsen T, Arendt-Nielsen L, Svensson P, Jensen TS (1997) Quantification of local and referred muscle pain in humans after sequential i.m. injections of hypertonic saline. Pain 69:111–117
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Hassan BS, Mockett S, Doherty M (2001) Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis 60:612–618
Hassan BS, Doherty SA, Mockett S, Doherty M (2002) Effect of pain reduction on postural sway, proprioception, and quadriceps strength in subjects with knee osteoarthritis. Ann Rheum Dis 61:422–428
Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G (2000) Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol 10:361–374
Hinman RS, Bennell KL, Metcalf BR, Crossley KM (2002) Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology (Oxford) 41:1388–1394
Hirata RP, Arendt-Nielsen L, Graven-Nielsen T (2010) Experimental calf muscle pain attenuates the postural stability during quiet stance and perturbation. Clin Biomech (Bristol, Avon) 25:931–937
Hirata RP, Ervilha UF, Arendt-Nielsen L, Graven-Nielsen T (2011) Experimental muscle pain challenges the postural stability during quiet stance and unexpected posture perturbation. J Pain 12(8):911–919
Hodges PW, Tucker K (2011) Moving differently in pain: a new theory to explain the adaptation to pain. Pain 152:S90–S98
Hodges PW, Mellor R, Crossley K, Bennell K (2009) Pain induced by injection of hypertonic saline into the infrapatellar fat pad and effect on coordination of the quadriceps muscles. Arthritis Rheum 61:70–77
Horak FB, Diener HC, Nashner LM (1989) Influence of central set on human postural responses. J Neurophysiol 62:841–853
Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM (2002) Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc 50:671–678
Lin SI, Woollacott MH (2002) Postural muscle responses following changing balance threats in young, stable older, and unstable older adults. J Mot Behav 34:37–44
Matre D, Arendt-Neilsen L, Knardahl S (2002) Effects of localization and intensity of experimental muscle pain on ankle joint proprioception. Eur J Pain 6:245–260
McAlindon TE, Cooper C, Kirwan JR, Dieppe PA (1992) Knee pain and disability in the community. Br J Rheumatol 31:189–192
Messier SP, Glasser JL, Ettinger WH Jr, Craven TE, Miller ME (2002) Declines in strength and balance in older adults with chronic knee pain: a 30-month longitudinal, observational study. Arthritis Rheum 47:141–148
Oie KS, Kiemel T, Jeka JJ (2002) Multisensory fusion: simultaneous re-weighting of vision and touch for the control of human posture. Brain Res Cogn Brain Res 14:164–176
Pradels A, Pradon D, Vuillerme N (2011) Effects of experimentally induced pain of the plantar soles on centre of foot pressure displacements during unperturbed upright stance. Clin Biomech (Bristol, Avon) 26:424–428
Shakoor N, Furmanov S, Nelson DE, Li Y, Block JA (2008) Pain and its relationship with muscle strength and proprioception in knee OA: results of an 8-week home exercise pilot study. J Musculoskelet Neuronal Interact 8:35–42
Takagi A, Fujimura E, Suehiro S (1985) A new method of statokinesigram area measurement. Application of a statistically calculated ellipse. In: Igarashi M, Black O (eds) Vestibular and visual control on posture and locomotor equilibrium. Karger, New York, pp 74–79
Vuillerme N, Pinsault N (2009) Experimental neck muscle pain impairs standing balance in humans. Exp Brain Res 192:723–729
Wegener L, Kisner C, Nichols D (1997) Static and dynamic balance responses in persons with bilateral knee osteoarthritis. J Orthop Sports Phys Ther 25:13–18
White DK, Zhang Y, Felson DT, Niu J, Keysor JJ, Nevitt MC, Lewis CE, Torner JC, Neogi T (2011) The independent effect of pain in one versus two knees on the presence of low physical function in a multicenter knee osteoarthritis study. Arthritis Care Res (Hoboken) 62:938–943
Winter DA (1995) A.B.C. (anatomy, biomechanics, control) of balance during standing and walking. Waterloo Biomechanics, Ontario
Winter DA, Prince F, Frank JS, Powell C, Zabjek KF (1996) Unified theory regarding A/P and M/L balance in quiet stance. J Neurophysiol 75:2334–2343
Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech 35:543–548
Yagci N, Cavlak U, Aslan UB, Akdag B (2007) Relationship between balance performance and musculoskeletal pain in lower body comparison healthy middle aged and older adults. Arch Gerontol Geriatr 45:109–119
Acknowledgments
We thank the Danish Arthritis Association and the Danish Ministry of Health and Prevention for supporting this study and Hongling Nie, MD, PhD, for performing the injections.
Conflict of interest
There is no conflict of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Fausto Baldissera.
Rights and permissions
About this article
Cite this article
Hirata, R.P., Arendt-Nielsen, L., Shiozawa, S. et al. Experimental knee pain impairs postural stability during quiet stance but not after perturbations. Eur J Appl Physiol 112, 2511–2521 (2012). https://doi.org/10.1007/s00421-011-2226-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-2226-3