Abstract
The aim was to investigate the influence of a daily mixed nutritional supplement during an 8-week arduous training programme on immune indices and mediators including circulating leucocyte counts; bacterially stimulated neutrophil degranulation; interleukin-6 (IL-6), cortisol and saliva secretory immunoglobulin-A (SIgA). Thirty men (mean (SD): age 25 (3) years; body mass, 80.9 (7.7) kg) received a habitual diet (CON, n = 15) or received a habitual diet plus an additional food supplement (SUP, n = 15). From weeks 0–6, CON received 14.0 MJ day−1 and SUP received 19.7 MJ day−1, and during a final 2-week field exercise in weeks 7 and 8, CON received 17.7 MJ day−1 and SUP received 21.3 MJ day−1. Blood and saliva were taken at rest after an overnight fast at weeks 0, 6 and 8. Body mass loss over the 8 weeks was greater in CON (CON, 5.0 (2.3); SUP, 1.6 (1.5) kg: P < 0.001). Training-induced decreases in circulating total leucocytes (CON: weeks 0, 8.0 (2.1); weeks 8, 6.5 (1.6) 109 l−1, P < 0.01), lymphocytes (21%, P < 0.01) and monocytes (20%, P < 0.01) were prevented by the nutritional supplement. Saliva SIgA secretion rate increased approximately twofold by week 8 in SUP (P < 0.01) and was greater at week 8 compared with CON (P < 0.01). Circulating neutrophils, bacterially stimulated neutrophil degranulation, IL-6 and cortisol were similar in CON and SUP at week 8. In conclusion, a daily mixed nutritional supplement prevented the decrease in circulating total leucocytes, lymphocytes and monocytes and increased saliva SIgA output during an 8-week arduous training programme. The increase in saliva SIgA with nutritional supplementation during training may reduce susceptibility to upper respiratory infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Military personnel and athletes often experience prolonged periods of nutritional insufficiency, coupled with the additional stress of demanding training regimens. It is widely acknowledged that nutritional restriction can impair immune function, which in-turn may increase an individual’s susceptibility to infection (Walsh et al. 2011b). Laboratory studies show that nutritional restriction for periods of 2–7 days temporarily decreases various aspects of immune function including: circulating total leucocyte and lymphocyte subset number (Laing et al. 2008b); lymphocyte cytokine release in response to stimulation (Savendahl and Underwood 1997); saliva secretory immunoglobulin-A (SIgA) responses (Oliver et al. 2007); and neutrophil chemotaxis (Walrand et al. 2001). These findings are unsurprising given that nutrient availability is required for immune cell replication, metabolism and antioxidant defences (Bishop et al. 1999). In addition, nutrient restriction may weaken immune function through raised hypothalamic–pituitary–adrenal activation and sympathetic–adrenal–medullary activation, resulting in increased stress hormones, which can have immunosuppressive effects (Gleeson 2007).
Intensive periods of training in soldiers and athletes have been shown to decrease cellular, humoral and mucosal immunity and to increase circulating metabolic and inflammatory indicators (e.g. interleukin (IL)-6) and symptoms of upper respiratory illness (URI) (Baj et al. 1994; Gomez-Merino et al. 2005; Tiollier et al. 2005; Whitham et al. 2006). The multi-stressor nature and the lack of experimental control in many military field studies make it difficult to identify the role that energy deficit plays in the observed decrease in immune health. Soldiers simultaneously experience stressors including heavy exertion, energy restriction, sleep deprivation and exposure to environmental extremes: all of these stressors have been shown to modulate immune function independently (Walsh et al. 2011a; Walsh and Whitham 2006). One recent study showed that soldiers training for 7 days with an estimated 16 MJ day−1 energy deficit experienced a 35% increase in resting circulating cortisol (Kyröläinen et al. 2008). Given the likely role for stress hormones in the modulation of immune function with heavy training (Pedersen and Hoffman-Goetz 2000), we might expect that the energy-deficit-evoked increase in circulating cortisol during arduous training accounts, at least in part, for the observed decrease in immune function in military training studies; however, this remains unsubstantiated. Unfortunately, well-controlled field studies have not been conducted to show whether providing additional energy intake to reduce the energy deficit prevents the decrease in immune function during military training. Blunting the energy deficit with additional feeding during a 2-month army ranger course (4.0 MJ day−1 vs. 4.9 MJ day−1) induced a less-severe suppression of in vitro T-lymphocyte responses (Kramer et al. 1997). However, study limitations include the variable timing of blood sampling after the last bout of exercise, some problems with blood sample viability and that soldiers receiving the additional supplementation experienced considerable body mass losses by the end of the course (13%).
Therefore, the aim of this study was to investigate the influence of daily mixed nutritional supplementation on resting circulating total and differential leucocyte counts, bacterially stimulated neutrophil degranulation, saliva SIgA and on circulating cortisol and IL-6 responses during an 8-week arduous training programme. We hypothesised that reducing the daily energy deficit with nutritional supplementation would attenuate the immune modulation during arduous training.
Methods
Participants
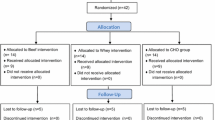
Thirty healthy men (mean (SD): age, 25 (3) years; height, 178 (5) cm; body mass, 80.9 (7.7) kg; body fat, 15.4 (3.3) %) were self-selected from two platoons of soldiers undertaking the 8-week section commanders battle course at the Infantry Battle School, Brecon, UK, during the winter of 2009/2010. This training course is a promotion-qualifying course with successful soldiers promoted to full corporal. All participants gave written informed consent before commencing the study, which received ethical approval from the Ministry of Defence (UK) Research Ethics Committee.
Experimental design and procedures
A mixed model, repeated measures design was used to monitor two platoons at three time points during the 8-week training programme: at baseline (week 0), pre-field exercise (end of week 6) and post-field exercise (the day following completion of field exercise, week 8). During the first 6 weeks, soldiers resided in barracks and completed daily training excursions. This was followed by a 2-week field exercise where soldiers resided in the field and underwent more rigorous training. Soldiers completing this training programme have previously been shown to be in energy deficit resulting in body mass loss of 5.1 (2.6) kg. The estimated energy expenditure using doubly labelled water was 19.7 MJ day−1 during weeks 0–6 and 21.3 MJ day−1 during the field exercise (Richmond et al. 2010). In the present study, one platoon formed the control group (CON, n = 15) and consumed a habitual diet alone and one platoon formed the supplemented group (SUP, n = 15) and received a habitual diet plus an additional daily mixed nutritional supplement. All soldiers were given the habitual diet of ~14.0 MJ day−1 during in-barrack feeding between weeks 0 and 6 (estimated energy shortfall of 5.7 MJ day−1) and 17.7 MJ day−1 during the final 2-week field exercise (estimated energy shortfall of 3.6 MJ day−1). The SUP group received an additional 5.7 MJ day−1 during weeks 0–6 and 3.6 MJ day−1 during the field exercise. These values were derived from previous data taken during this battle course where soldiers experienced an estimated average energy deficit of 2.7 MJ day−1 for the 8-week training programme despite self-supplementing their diet by ~2.9 MJ day−1 (Richmond et al. 2010). Since we did not want soldiers in SUP using the nutritional supplement as an alternative to food they might normally purchase and accounting for a small increase in food provision (0.5 MJ day−1), we provided a nutritional supplement to cover both the estimated energy deficit (2.7 MJ day−1) and self-supplementation (2.9 MJ day−1), thus providing an average of 5.1 MJ day−1 for the 8-week training programme. To assess supplement adherence, all food wrappers and packaging that the supplement was provided in were collected daily, with any uneaten foods accurately weighed. It was assumed that CON would self-supplement their diet as previously shown. The macronutrient breakdown of the supplement was ~45% carbohydrate, ~40% fat and ~15% protein in order to match the composition of the habitual diet.
Body composition, estimation of energy deficit and physical activity
Body composition was assessed at baseline and post-field exercise using whole body dual-energy X-ray absorptiometry (DEXA; Hologic 4500A, Bedford, USA) and body fat mass, lean body mass and per cent body fat were calculated. Estimations of energy deficit over the 8-week training period were calculated based upon DEXA estimated changes in fat mass and lean mass as previously described (Westerterp et al. 1995). The energy densities of fat mass and lean mass were assumed to be 38 and 6 MJ kg−1, respectively (with lean mass comprising 73% water and 27% protein). Physical activity was monitored continuously throughout the field exercise by an accelerometer (3DNX, BioTel, Bristol, UK) worn around the waist and positioned at the base of the spine, as previously described (Carter et al. 2008).
Blood collection and analysis
After an overnight fast, and 12 h since the last exercise bout, samples were collected between 0530 and 0600 hours at baseline, pre-field exercise and post-field exercise. Blood samples were collected by venepuncture from an antecubital vein into one K3EDTA-coated vacutainer and one lithium heparin–coated vacutainer (Becton–Dickinson, Oxford, UK). For each sample taken, a 2-ml aliquot of K3EDTA whole blood was kept at room temperature prior to haemotological analysis. Haematological analysis of circulating total and differential leucocyte counts was performed using an automated cell counter (Gen-S, Beckman Coulter, High Wycombe, UK). A 1-ml aliquot of lithium heparin whole blood was used to determine bacterially stimulated neutrophil release. The remaining K3EDTA- and lithium heparin-treated blood was centrifuged at 1,500g for 10 min in a refrigerated centrifuge. Plasma was aliquoted into eppendorf tubes and immediately frozen at −40°C for later analysis.
Bacterially stimulated neutrophil degranulation
A 1-ml aliquot of lithium heparin whole blood was added to 50 μl of bacterial stimulant solution (Stimulant, Sigma, Poole, UK) and gently vortex mixed. Samples were immediately incubated for 60 min at 37°C, with gentle inversion at 30 min, as previously described (Laing et al. 2008a; Robson et al. 1999). After incubation, samples were centrifuged at 5,000g for 2 min, and the supernatant was frozen at −40°C for later analysis. Bacterially stimulated and unstimulated lithium heparin plasma samples were analysed for concentrations of elastase using a high-sensitivity ELISA kit (Biovendor, Heidelberg, Germany). The unstimulated elastase concentration was subtracted from the bacterially stimulated elastase concentration and corrected for the individual neutrophil count to determine neutrophil degranulation (elastase release per neutrophil). All samples for elastase release were run on the same day, with standards and controls on each plate. The intra-assay coefficient of variation for elastase concentration was 5.0%.
Plasma IL-6 and cortisol concentration
Plasma IL-6 concentration was determined on K3EDTA plasma using a commercially available high-sensitivity IL-6 ELISA (RnD systems, Minneapolis, USA). Aliquots of lithium heparin plasma were used to determine cortisol concentration by ELISA according to the manufacturer’s instructions (DRG Instruments, Marburg, Germany). All samples for plasma IL-6 and cortisol were run on the same day, with standards and controls on each plate. The intra-assay coefficient of variation for plasma IL-6 and cortisol was 5.1 and 1.9%, respectively.
Saliva collection and analysis
Unstimulated whole saliva samples were collected from participants using a passive dribble for 5 min into a pre-weighed universal tube (HR 120-EC, A & D instruments, Tokyo, Japan) between 0530 and 0600 hours at baseline, pre-field exercise and post-field exercise (Costa et al. 2010). All saliva samples were collected while the participant sat quietly after first rinsing their mouth with water and swallowing. Saliva collections were performed with minimal orofacial movements. Saliva volume was measured by weighing the samples to the nearest milligram immediately after collection. Saliva flow rate was determined by dividing the volume collected, by the time of collection, and assuming the density of saliva to be 1.00 g ml−1 (Cole and Eastoe 1988). The samples were frozen immediately at −40°C. Saliva samples were analysed for SIgA concentration using a commercially available competitive ELISA (Salimetrics, Pennsylvania, USA). Salivary SIgA secretion rate was calculated by multiplying the SIgA concentration by the saliva flow rate. All samples for SIgA were run on the same day, with standards and controls on each plate. The intra-assay coefficient of variation was 3.0%.
Statistical analysis
Sample size was estimated using data for immune indices from a previous military training study (Whitham et al. 2006) and alpha (Type I error rate) set at 0.05, and power (Type II error rate) at 0.9 (G*Power software, version 3.1.2). Data in the text and tables are presented as mean (SD), and statistical significance was accepted at P < 0.05. For clarity, data in figures are presented as mean (SEM). Independent sample t tests were used to assess differences between the two groups in demographic data; physical activity; body mass loss; lean body mass loss; fat mass loss and estimated energy deficit. A two-way mixed model ANOVA (2 independent groups × 3 time points) was used to compare all other data. The data were checked for sphericity and the Greenhouse-Geisser adjustments to the degrees of freedom were applied where necessary. Tukeys honestly significant (HSD) difference post hoc tests were used to determine within- and between-group main effects. All data were analysed using SPSS version 14.
Results
Physical activity, body composition and estimated energy deficit
There was no difference at baseline between CON and SUP for demographic data. There was also no difference between CON and SUP for physical activity counts during the field exercise (CON, 130 (18); SUP, 133 (19) 103). Body mass decreased significantly in both CON and SUP throughout the 8-week training programme (interaction F(1,28) = 21.3, P < 0.01). However, body mass loss (t(28) 4.6, P < 0.001), lean mass loss (t(28) 2.6, P < 0.05) and fat mass loss (t(28) 3.4, P < 0.01) were all significantly greater in the CON group over the 8-week training period (Table 1). By collecting all food wrappers and weighing uneaten supplement product, it was estimated that the supplement group consumed on average 66 (13) % of the daily mixed supplement (64% during weeks 0–6, and 77% during weeks 6–8). Estimated daily energy deficit during the training programme was significantly greater in the CON group than in the SUP group (t(28) 3.8, P < 0.001).
Circulating total leucocyte, neutrophil, lymphocyte and monocyte counts
A significant trial × time interaction was observed for circulating total leucocyte (F(1.6,43.5) = 3.7, P < 0.05; Fig. 1a), lymphocyte (F(2,56) = 3.4, P < 0.05; Fig. 1c) and monocyte counts (F(2,56) = 4.9, P < 0.05; Fig. 1d), but no significant interaction or main effects were observed for neutrophil count (Fig. 1b). In the CON group, circulating leucocyte, lymphocyte and monocyte counts decreased significantly post-field exercise compared with baseline (P < 0.01) and lymphocyte counts were also significantly lower at post-field exercise compared with pre-field exercise (P < 0.01). The addition of a daily mixed nutritional supplement prevented the decrease in circulating leucocyte (P < 0.01), lymphocyte (P < 0.01) and monocyte (P < 0.05) counts at post-field exercise compared with CON.
Circulating total leucocyte (a), neutrophil (b), lymphocyte (c) and monocyte (d) count response to an 8-week military training programme where soldiers consumed either a habitual diet alone (CON open circle), or a habitual diet plus a daily mixed nutritional supplement (SUP, filled square). Data are mean (SEM). **P < 0.01 versus baseline; §§ P < 0.01 versus pre-field exercise; # P < 0.05 and ## P < 0.01 versus CON
Bacterially stimulated neutrophil degranulation
There was no significant trial × time interaction or main effect for time or trial for unstimulated plasma elastase concentration. A significant trial × time interaction was observed for bacterially stimulated neutrophil degranulation (elastase release per neutrophil; F(1.6,56) = 5.8, P < 0.01). Neutrophil degranulation was not significantly different between CON and SUP at baseline or post-field exercise. However, at pre-field exercise, neutrophil degranulation increased significantly on CON (vs. baseline: P < 0.01) and was greater than SUP (P < 0.01) at this time (baseline, 529 (112); pre-field exercise, 675 (175); post-field exercise, 557 (134) fg cell−1). Neutrophil degranulation remained unchanged in the SUP group (baseline, 553 (128); pre-field exercise, 531 (130); and post-field exercise, 534 (156) fg cell−1).
Plasma IL-6 and cortisol concentration
There was no trial × time interaction for plasma IL-6 concentration. However, a significant main effect of time was observed (F(2,52) = 5.9, P < 0.01). Plasma IL-6 concentration for both groups pooled was significantly greater at post-field exercise (0.97 (0.59) pg ml−1) than at baseline (0.68 (0.35) pg ml−1) and pre-field exercise (0.60 (0.58) pg ml−1) (P < 0.05). No trial × time interaction was observed for plasma cortisol concentration. However, there was a main effect of time (F(2,56) = 5.1, P < 0.01). Plasma cortisol concentration was 519 (104) nmol l−1 at baseline and increased from pre-field exercise (494 (85) nmol l−1) to post-field exercise (548 (83) nmol l−1; P < 0.01) in the whole cohort (n = 30).
Saliva SIgA responses
A main effect of time was observed for saliva flow rate (F(1.2,31.8) = 5.0, P < 0.05; Fig. 2a) and saliva SIgA concentration (F(2,54) = 8.46, P < 0.01; Fig. 2b). Saliva flow rate was significantly lower at post-field exercise than at baseline (P < 0.05), and saliva SIgA concentration was significantly greater at pre-field exercise and post-field exercise than at baseline (P < 0.01). A trial × time interaction was observed for saliva SIgA secretion rate (F(2,54) = 3.2, P < 0.05; Fig. 2c), which was significantly greater at post-field exercise in the SUP group compared with the CON group (P < 0.01). Furthermore, within the SUP group, saliva SIgA secretion rate significantly increased from baseline to pre-field exercise (P < 0.05) and from baseline to post-field exercise (P < 0.05).
Saliva flow rate (a), saliva SIgA concentration (b) and saliva SIgA secretion rate (c) response to an 8-week military training programme where soldiers consumed either a habitual diet alone (CON open circle) or a habitual diet plus a daily mixed nutritional supplement (SUP, filled square). Data are mean (SEM). † P < 0.05 and †† P < 0.01 versus baseline (main effect of time); *P < 0.05 versus baseline; ## P < 0.01 versus CON
Discussion
The aim of the present study was to determine the effect of daily mixed nutritional supplementation on resting immune indices during an 8-week arduous training programme. Compared with many previous field studies, particular strengths of the present study were the inclusion of a comparative control group and standardisation of both the time of day when samples were collected and the time between the last exercise bout and sample collection. In line with our hypothesis, daily mixed nutritional supplementation prevented the training-induced decrease in circulating total leucocyte, lymphocyte and monocyte counts. Particularly novel was our finding that nutritional supplementation increased saliva SIgA secretion rate during training: this finding can be considered favourable for host defence. However, nutritional supplementation did not significantly alter circulating neutrophil counts, plasma IL-6 or cortisol concentration. These data indicate that daily mixed nutritional supplementation can modulate selected immune indices during training in the absence of a significant treatment effect on circulating cortisol.
Soldiers completing the 8-week training course experienced an average energy deficit in the CON group of 2.2 MJ day−1, which was smaller in the SUP group (0.7 MJ day−1). Soldiers in SUP were provided with the same basal diet as CON, with, on average, an additional 5.1 MJ day−1 provided as a daily supplement during training. We assumed, based upon previous findings (Richmond et al. 2010), that self-supplementation by CON (~2.9 MJ day−1) would lead to a theoretical difference in energy deficit between the two groups of ~2.2 MJ day−1. The difference in estimated energy deficit between CON and SUP was 1.5 MJ day−1: this is likely explained by the finding that SUP consumed on average only 66% of the supplement. The resulting body mass losses (6% for CON and 2% for SUP) are relatively modest compared with those reported in other military field studies (Friedl et al. 1994; Kramer et al. 1997; Nindl et al. 2007). For example, soldiers experienced ~16% body mass losses during a 2-month army ranger course where the energy deficit was 4.9 MJ day−1 (Kramer et al. 1997). The modest energy restriction experienced by soldiers in this study likely explains the limited effect we observed on resting circulating cortisol and IL-6 concentration. It is likely that a more severe energy deficit is required to substantially increase circulating cortisol and IL-6. In support of this contention is the finding of one study that showed a 35% increase in circulating cortisol when soldiers trained with a 16 MJ day−1 energy deficit but a return to baseline levels when soldiers subsequently trained with a similar energy deficit to the present study (~2 MJ day−1) (Kyröläinen et al. 2008). Given the widely accepted role for stress hormones in mediating immune alterations with heavy training (Pedersen and Hoffman-Goetz 2000) and the absence of a significant effect of nutritional supplementation on circulating cortisol, we might anticipate no significant effect of nutritional supplementation on the various immune indices we measured. In contrast, we observed significant training-induced decreases in circulating total leucocyte, lymphocyte and monocyte counts that were prevented with nutritional supplementation sufficient to offset two-thirds of the estimated energy deficit. The mechanism(s) responsible for altered leucocyte trafficking with heavy training and the modulatory effect of nutritional supplementation remain unclear. Possible explanations for training-induced decreases in circulating leucocytes include, but are not limited to, decreased bone marrow production, increased apoptosis and plasma volume expansion. That offsetting some of the energy deficit prevented the training-induced decrease in circulating leucocytes points to the interesting possibility that a modest energy deficit, as commonly experienced by an athlete or soldier, may account, at least in part, for the lower circulating leucocyte counts in those under heavy training (Horn et al. 2010). The mechanism(s) responsible for this observation (e.g. energy deficit per se or specific macronutrient or micronutrient deficit) remains unclear. Nevertheless, current thinking indicates that the modest influence of training on circulating leucocyte numbers that we, and others, have observed (i.e. decrease within the normal clinical range: 4.5–11 × 109 l−1) reflects an adaptive response that is not pathological (Horn et al. 2010). Athletes engaged in heavy training typically have lower circulating and differential leucocyte counts than their sedentary counterparts when blood samples are collected in the morning following an overnight rest (Horn et al. 2010). In the present study, soldiers underwent 6 weeks of light skill acquisition training prior to baseline sampling. This may account for the higher baseline circulating total leucocyte count in soldiers undertaking light training (7.9 × 109 l−1) than previously reported for endurance athletes undertaking heavy training (e.g. Triathletes: 5.9 × 109 l−1) (Horn et al. 2010). In addition, its noteworthy that the mean baseline circulating total leucocyte count of 7.9 × 109 l−1 falls in the middle of the normal clinical range and is comparable with rested soldiers reported elsewhere (Brenner et al. 2000; Whitham et al. 2006). Although we observed similar bacterially stimulated neutrophil degranulation before and after training in CON and at post-field exercise in CON and SUP, it remains unclear why we observed an increase in neutrophil degranulation at pre-field exercise in the CON group.
Some studies have observed decreased saliva SIgA concentration (Gomez-Merino et al. 2003; Tiollier et al. 2005) and increased URI symptoms (Tiollier et al. 2005) during periods of heavy training in soldiers experiencing a range of stressors including, amongst others, notable energy deficit. Potential explanations for lower saliva SIgA during energy deficit include decreased plasma cell IgA synthesis (Revillard and Cozon 1990) and decreased availability of polymeric Ig receptor (Ha and Woodward 1998) albeit the latter was shown in intestinal mucous secretions in a mouse model of protein-energy malnutrition. Nevertheless, there is some evidence in malnourished children that free secretory component is decreased in secretions such as tear fluid: secretory component is the extracellular fragment of the polymeric Ig receptor responsible for transport of dimeric IgA into saliva (Watson et al. 1985; Woof and Kerr 2006). A strength of the present study is that we present saliva SIgA as both concentration and secretion rate: by considering flow rate and SIgA concentration, saliva SIgA secretion rate reflects the total availability of SIgA at the oral surface (Walsh et al. 1999). As we did not observe a significant decrease in either saliva SIgA concentration or secretion rate, these results indicate that mucosal immunity was preserved despite the modest energy deficit during training (~2.2 MJ day−1). Work from our laboratory indicates that saliva SIgA availability may have been compromised in the present study had the soldiers trained with a more severe energy deficit (~11 MJ day−1 in the previous study) particularly when accompanied by fluid restriction (Oliver et al. 2007). The particularly novel finding in the present study is the increase in saliva SIgA secretion rate during training in soldiers who received daily mixed nutritional supplements (Fig. 2c). Studies are required to identify potential roles for increased plasma cell IgA synthesis or increased IgA transcytosis via increased polymeric Ig receptor availability. The observed increase in saliva SIgA output in the SUP group might, in small part, be explained by the trend for a smaller decrease in saliva flow rate during training in SUP than CON (−31% vs. −61% for post-field exercise vs. baseline). We speculate that hydration status was better maintained in the SUP group and that this accounts for the smaller decrease in saliva flow rate compared with CON (Walsh et al. 2004a, b). This contention is supported by lower plasma osmolality (SUP: 289 (3) and CON: 293 (4) mOsmol kg−1) and urine colour (SUP: 3 (1) and CON: 5 (1) using 1–8 scale (Armstrong et al. 1994)) at post-field exercise in CON: these hydration assessments were made to achieve other study objectives. To summarise, the novel finding that saliva SIgA output increased during training in soldiers who received daily mixed nutritional supplementation, sufficient to offset two-thirds of the estimated energy deficit, might be favourable for immune health, particularly when the soldier is exposed to more severe stressors known to compromise host defence.
We recognise that a limitation of the current study is that we were unable to record daily URI symptoms during or shortly after the training programme: however, the validity of self-reporting URI has recently come under scrutiny (Cox et al. 2008; Walsh et al. 2011b). Future training studies should assess the influence of similar feeding regimens on other aspects of immune function important to host defence such as natural killer cell cytotoxic activity and T-cell function or, better still, the responses to clinically relevant in vivo immune challenge, e.g., using delayed-type hypersensitivity (Bruunsgaard et al. 1997) or contact hypersensitivity tests (Harper Smith et al. 2011). In conclusion, daily mixed nutritional supplementation during an 8-week arduous training programme prevented the decrease in circulating total leucocyte, lymphocyte and monocyte counts and increased saliva SIgA secretion rate. Alterations in these immune indices occurred despite no effect of daily mixed nutritional supplementation on circulating cortisol concentration.
References
Armstrong LE, Maresh CM, Castellani JW, Bergeron MF, Kenefick RW, LaGasse KE, Riebe D (1994) Urinary indices of hydration status. Int J Sport Nutr 4:265–279
Baj Z, Kantorski J, Majewska E, Zeman K, Pokoca L, Fornalczyk E, Tchorzewski H, Sulowska Z, Lewicki R (1994) Immunological status of competitive cyclists before and after the training season. Int J Sports Med 15:319–324
Bishop NC, Blannin AK, Walsh NP, Robson PJ, Gleeson M (1999) Nutritional aspects of immunosuppression in athletes. Sports Med 28:151–176
Brenner IK, Severs YD, Rhind SG, Shephard RJ, Shek PN (2000) Immune function and incidence of infection during basic infantry training. Mil Med 165:878–883
Bruunsgaard H, Hartkopp A, Mohr T, Konradsen H, Heron I, Mordhorst CH, Pedersen BK (1997) In vivo cell-mediated immunity and vaccination response following prolonged, intense exercise. Med Sci Sports Exerc 29:1176–1181
Carter J, Wilkinson D, Blacker S, Rayson M, Bilzon J, Izard R, Coward A, Wright A, Nevill A, Rennie K, McCaffrey T, Livingstone B (2008) An investigation of a novel three-dimensional activity monitor to predict free-living energy expenditure. J Sports Sci 26:553–561
Cole AS, Eastoe JE (1988) Biochemistry and oral biology. Wright, London, pp 476–477
Costa RJ, Smith AH, Oliver SJ, Walters R, Maassen N, Bilzon JL, Walsh NP (2010) The effects of two nights of sleep deprivation with or without energy restriction on immune indices at rest and in response to cold exposure. Eur J Appl Physiol 109:417–428
Cox AJ, Gleeson M, Pyne DB, Callister R, Hopkins WG, Fricker PA (2008) Clinical and laboratory evaluation of upper respiratory symptoms in elite athletes. Clin J Sport Med 18:438–445
Friedl KE, Moore RJ, Martinez-Lopez LE, Vogel JA, Askew EW, Marchitelli LJ, Hoyt RW, Gordon CC (1994) Lower limit of body fat in healthy active men. J Appl Physiol 77:933–940
Gleeson M (2007) Immune function in sport and exercise. J Appl Physiol 103:693–699
Gomez-Merino D, Chennaoui M, Burnat P, Drogou C, Guezennec CY (2003) Immune and hormonal changes following intense military training. Mil Med 168:1034–1038
Gomez-Merino D, Drogou C, Chennaoui M, Tiollier E, Mathieu J, Guezennec CY (2005) Effects of combined stress during intense training on cellular immunity, hormones and respiratory infections. Neuroimmunomodulation 12:164–172
Ha CL, Woodward B (1998) Depression in the quantity of intestinal secretory IgA and in the expression of the polymeric immunoglobulin receptor in caloric deficiency of the weanling mouse. Lab Invest 78:1255–1266
Harper Smith AD, Coakley SL, Ward MD, Macfarlane AW, Friedmann PS, Walsh NP (2011) Exercise-induced stress inhibits both the induction and elicitation phases of in vivo T-cell-mediated immune responses in humans. Brain Behav Immun 25:1136–1142. doi:10.1016/j.bbi.2011.02.014
Horn PL, Pyne DB, Hopkins WG, Barnes CJ (2010) Lower white blood cell counts in elite athletes training for highly aerobic sports. Eur J Appl Physiol 110:925–932
Kramer TR, Moore RJ, Shippee RL, Friedl KE, Martinez-Lopez L, Chan MM, Askew EW (1997) Effects of food restriction in military training on T-lymphocyte responses. Int J Sports Med 18:S84–S90
Kyröläinen H, Karinkanta J, Santtila M, Koski H, Mäntysaari M, Pullinen T (2008) Hormonal responses during a prolonged military field exercise with variable exercise intensity. Eur J Appl Physiol 102:539–546
Laing SJ, Jackson AR, Walters R, Lloyd-Jones E, Whitham M, Maassen N, Walsh NP (2008a) Human blood neutrophil responses to prolonged exercise with and without a thermal clamp. J Appl Physiol 104:20–26
Laing SJ, Oliver SJ, Wilson S, Walters R, Bilzon JL, Walsh NP (2008b) Neutrophil-degranulation and lymphocyte-subset response after 48 h of fluid and/or energy restriction. Int J Sport Nutr Exerc Metab 18:443–456
Nindl BC, Barnes BR, Alemany JA, Frykman PN, Shippee RL, Friedl KE (2007) Physiological consequences of US Army Ranger training. Med Sci Sports Exerc 39:1380–1387
Oliver SJ, Laing SJ, Wilson S, Bilzon JL, Walters R, Walsh NP (2007) Salivary immunoglobulin A response at rest and after exercise following a 48 h period of fluid and/or energy restriction. Br J Nutr 97:1109–1116
Pedersen BK, Hoffman-Goetz L (2000) Exercise and the immune system: regulation, integration, and adaptation. Physiol Rev 80:1055–1081
Revillard JP, Cozon G (1990) Experimental models and mechanisms of immune deficiencies of nutritional origin. Food Addit Contam 7(Suppl 1):S82–S86
Richmond VL, Horner FE, Wilkinson DM, Rayson MP, Wright A, Cook AC, Izard R (2010) Energy balance during the British Army Section Commanders’ Battle Course. Med Sci Sports Exerc 42(Suppl 1):287
Robson PJ, Blannin AK, Walsh NP, Castell LM, Gleeson M (1999) Effects of exercise intensity, duration and recovery on in vitro neutrophil function in male athletes. Int J Sports Med 20:128–135
Savendahl L, Underwood LE (1997) Decreased interleukin-2 production from cultured peripheral blood mononuclear cells in human acute starvation. J Clin Endocrinol Metab 82:1177–1180
Tiollier E, Gomez-Merino D, Burnat P, Jouanin JC, Bourrilhon C, Filaire E, Guezennec CY, Chennaoui M (2005) Intense training: mucosal immunity and incidence of respiratory infections. Eur J Appl Physiol 93:421–428
Walrand S, Moreau K, Caldefie F, Tridon A, Chassagne J, Portefaix G, Cynober L, Beaufrere B, Vasson MP, Boirie Y (2001) Specific and nonspecific immune responses to fasting and refeeding differ in healthy young adult and elderly persons. Am J Clin Nutr 74:670–678
Walsh NP, Whitham M (2006) Exercising in environmental extremes: a greater threat to immune function? Sports Med 36:941–976
Walsh NP, Blannin AK, Clark AM, Cook L, Robson PJ, Gleeson M (1999) The effects of high-intensity intermittent exercise on saliva IgA, total protein and alpha-amylase. J Sports Sci 17:129–134
Walsh NP, Laing SJ, Oliver SJ, Montague JC, Walters R, Bilzon JLJ (2004a) Saliva parameters as potential indices of hydration status during acute dehydration. Med Sci Sports Exerc 36:1535–1542
Walsh NP, Montague JC, Callow N, Rowlands AV (2004b) Saliva flow rate, total protein concentration and osmolality as potential markers of whole body hydration status during progressive acute dehydration in humans. Arch Oral Biol 49:149–154
Walsh NP, Gleeson M, Pyne DB, Nieman DC, Dhabhar FS, Shephard RJ, Oliver SJ, Bermon S, Kajeniene A (2011a) Position statement part two: maintaining immune health. Exerc Immunol Rev 17:64–103
Walsh NP, Gleeson M, Shephard RJ, Gleeson M, Woods J, Bishop NC, Fleshner M, Green C, Pedersen BK, Hoffman-Goetz LH, Rogers CJ, Northoff H, Abbasi A, Simon P (2011b) Position statement part one: immune function and exercise. Exerc Immunol Rev 17:6–63
Watson RR, McMurray DN, Martin P, Reyes MA (1985) Effect of age, malnutrition and renutrition on free secretory component and IgA in secretions. Am J Clin Nutr 42:281–288
Westerterp KR, Donkers JH, Fredrix EW, Boekhoudt P (1995) Energy intake, physical activity and body weight: a simulation model. Br J Nutr 73:337–347
Whitham M, Laing SJ, Dorrington M, Walters R, Dunklin S, Bland D, Bilzon JL, Walsh NP (2006) The influence of an arduous military training program on immune function and upper respiratory tract infection incidence. Mil Med 171:703–709
Woof JM, Kerr MA (2006) The function of immunoglobulin A in immunity. J Pathol 208:270–282
Acknowledgments
The study was sponsored by the Headquarters, Army Recruiting and Training Division, Ministry of Defence, UK. We would also like to thank the following people for their valuable assistance during data collection: Umberto Di Felice; Adam Harper Smith; Katharine Richardson; Tom Williams; Jodie Sherratt; James Morgan; Oly Perkin; Pieter Brown, Jason Graham and the training staff at the Infantry Battle School, Brecon, UK. We are also indebted to the participants for their time and cooperation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Susan A. Ward.
Rights and permissions
About this article
Cite this article
Diment, B.C., Fortes, M.B., Greeves, J.P. et al. Effect of daily mixed nutritional supplementation on immune indices in soldiers undertaking an 8-week arduous training programme. Eur J Appl Physiol 112, 1411–1418 (2012). https://doi.org/10.1007/s00421-011-2096-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-2096-8