Abstract
The use of electrical stimulation (ES) can contribute to our knowledge of how our neuromuscular system can adapt to physical stress or unloading. Although it has been recently challenged, the standard technique used to explore central modifications is the twitch interpolated method which consists in superimposing single twitches or high-frequency doublets on a maximal voluntary contraction (MVC) and to compare the superimposed response to the potentiated response obtained from the relaxed muscle. Alternative methods consist in (1) superimposing a train of stimuli (central activation ratio), (2) comparing the MVC response to the force evoked by a high-frequency tetanus or (3) examining the change in maximal EMG response during voluntary contractions, if this variable is normalized to the maximal M wave, i.e. EMG response to a single stimulus. ES is less used to examine supraspinal factors but it is useful for investigating changes at the spinal level, either by using H reflexes, F waves or cervicomedullary motor-evoked potentials. Peripheral changes can be examined with ES, usually by stimulating the muscle in the relaxed state. Neuromuscular propagation of action potentials on the sarcolemma (M wave, high-frequency fatigue), excitation–contraction coupling (e.g. low-frequency fatigue) and intrinsic force (high-frequency stimulation at supramaximal intensity) can all be used to non-invasively explore muscular function with ES. As for all indirect methods, there are limitations and these are discussed in this review. Finally, (1) ES as a method to measure respiratory muscle function and (2) the comparison between electrical and magnetic stimulation will also be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well-known that not only the muscles (e.g. Aagaard et al. 2001; Sale 1988; Zierath and Hawley 2004) but also the nervous system (e.g. Aagaard et al. 2002; Sale 1988; Yue et al. 1999) are subject to plasticity resulting from aging, training/detraining, long-term spaceflight, dietary changes or environmental conditions such as hypoxia. In addition to these chronic modifications, adaptations/alterations occur during acute conditions such as fatigue (Gandevia 2001; Millet et al. 2003a). Over the years different methods have been used to assess neuromuscular function (NMF), in particular maximal voluntary isometric or isokinetic contractions. It is accepted that comparing voluntary and evoked force or electromyography (EMG) in response to artificial stimuli gives more insight into the performance and fatigability of NMF. Among the different artificial stimuli that can be used (magnetic, mechanic, chemical) to investigate NMF in clinical and research fields, electrical stimulation (ES) is probably the most popular technique. Several muscles or muscle groups can be stimulated through their motor nerves, e.g. knee extensor (femoral nerve), plantar flexor (tibial nerve), elbow flexors (musculocutaneous nerve), tibialis anterior (peroneal nerve), etc., and superficial muscles can also be directly stimulated through electrodes placed on the muscle (intramuscular branches of the nerve) (Hultman et al. 1983).
Alterations/improvements of NMF are due to central (neural) and/or peripheral (muscular) changes, which appear to be mutually dependent. In fact, recruitment and firing of motoneurones is dependent on a descending drive from supraspinal sites as well as recurrent inhibition, but it is also controlled through a combination of influences including excitatory and inhibitory reflex inputs from different groups of muscle and cutaneous afferents (Gandevia 1998). Combining different types of ES with EMG and force measurements on contracted or relaxed muscles may help investigate the chronic or acute plasticity of NMF. For instance, it has been shown during a 2-min sustained maximal voluntary contractions (MVC) that strength loss and peripheral fatigue were less in neuromuscular patients (facioscapulohumeral dystrophy, myotonic dystrophy, motor and sensory neuropathy type I) than in healthy subjects whereas central fatigue did not differ between the two groups (Schillings et al. 2007). On the other hand, central activation at rest was much lower in the neuromuscular patients. Other examples can be found in (1) training adaptations which can be evidenced by ES often combined with voluntary contractions and EMG measurements (Van Cutsem et al. 1998) or (2) fatigue in athletes. Another example is the fact that extreme running (over 24 h) induces large central fatigue and changes at the muscle level that are highly variable and dependent on the course profile and muscle group (Martin et al. 2010; Millet et al. 2011).
The first two parts of this review will examine the potential interest of using ES to non-invasively assess central drive and peripheral response in the fields of pathology and fundamental or applied research. For both aspects, limits of utilization and interpretation will be highlighted. This is important because ES can be used not only in fundamental research but also in the diagnosis of pathology, to evaluate the effect of a therapy/retraining program or to follow the history of a disease in patients although many restrictions due to stimulation tolerance exist. The third section will be dedicated to ES as a method of investigating the NMF of respiratory muscles and the fourth a comparison between ES and magnetic stimulation. Describing in detail the methodology of each technique presented is beyond the scope of this paper and can be found in other publications (Aagaard et al. 2002; Gandevia et al. 1996, 1999; Goodall et al. 2009; Martin et al. 2004b; Merton 1954; Place et al. 2007; Polkey et al. 1996; Swallow et al. 2007; Taylor and Gandevia 2001; Todd et al. 2003; Verges et al. 2009; Zehr 2002). Here, our purpose is to review the potential interests and limits of ES as an evaluation tool in the fields of sport and pathology.
Use of ES to assess central drive
Voluntary activation has been defined as the level of voluntary drive during an effort (Gandevia 2001). To determine the level of maximal voluntary activation (%VA), the standard technique (Merton 1954) is the interpolated twitch technique (ITT) which consists in superimposing electrically evoked single twitch to MVC and to compare the superimposed response to the potentiated response evoked on the relaxed muscle (Allen et al. 1995). A derived method consists in superimposing high-frequency (e.g. 100 Hz) paired-pulses which are compared with the same stimulation on the relaxed muscle (Fig. 1). While it has been argued that there was no significant difference in the ITT sensitivity between twitches, doublets or quintuplets (Behm et al. 1996), ITT with high-frequency potentiated paired-pulses are now usually recommended (Duchateau 2009; Place et al. 2007). ITT is often but not always applied in isometric conditions but when performed in dynamic conditions, the contraction speed is generally low (Babault et al. 2001) even if some studies have applied ITT to angular velocities as high as 300° s−1 (Gandevia et al. 1998). Whether the interpolated twitch provides a valid measure of %VA is still debated (de Haan et al. 2009; Taylor 2009), but authors agree that it helps in the detection of altered drive to muscles, for instance with fatigue (Gandevia 2001) or pathology, at least semi-quantitatively (de Haan et al. 2009). Superimposed stimulations have been used in fundamental research as well as to investigate the central drive in different diseases such as stroke (Horstman et al. 2008), chronic heart failure (Harridge et al. 1996), respiratory diseases (Vallier et al. 2011) or neuromuscular disorders (Allen et al. 1994; Schillings et al. 2007). In the context of pathology, it is interesting to report that muscle (rather than nerve) stimulation can be used to determine %VA. Similar %VA changes were reported between supramaximal stimulation of the femoral nerve and muscle stimulation with the following intensities: (1) maximally tolerated muscle stimulation (Rutherford et al. 1986), (2) 100 mA (Place et al. 2010) or (3) intensity to obtain a tetanus at 80 Hz equal to 50% of the subject’s MVC (Martin et al. 2004b).
Typical torque trace (black line) during knee extensor maximal voluntary contraction and determination of the maximal activation level, as well as high- and low-frequency doublets (100 and 10 Hz, respectively), and single twitch (Tw), before (a) and after (b) an ultra-marathon. From (Millet et al. 2011). The black arrows indicate the timing of delivery of the stimuli. EMG is represented with a gray line. Of note are the outsized evoked responses when the muscle is in relaxed state to compare with maximal voluntary contraction. This was due to large central fatigue after the race
Alternative methods of ITT consist in (1) central activation ratio superimposing a train of stimuli (or to single/double pulses) to MVC (Bigland-Ritchie et al. 1978; Martin et al. 2010; Rutherford et al. 1986), (2) comparing the MVC response to the force evoked by a high-frequency tetanus (Martin et al. 1999) or (3) examining the change in RMS · M−1 which is the root mean square of maximal EMG response during voluntary contractions normalized to maximal M wave, i.e. EMG response to a single stimulus (Baudry et al. 2007; Millet et al. 2003b). This latter technique is less reproducible since intraday coefficients of variation (CV) were found to be ≤2.5% for ITT or central activation ratio versus >10% for RMS · M−1 (Place et al. 2007; Todd et al. 2004) and similar results were found for interday CVs. However, it allows the examination of modified activation (maximal EMG activity) in the individual muscles of a muscle group, something which is not feasible with any other technique based on force measurement. For instance, RMS · M−1 of the vastus lateralis, vastus medialis and rectus femoris can be measured while only %VA of knee extensors is quantified. In addition, EMG measurements may represent the only way to assess central changes during high-velocity contractions. Comparison of some of these techniques can be found elsewhere (Behm et al. 2001; Place et al. 2007).
ES is also useful to investigate changes at the spinal level, by using either the Hoffmann reflex (H-reflex), cervicomedullary motor-evoked potentials (CMEP) or F waves. For years, adaptations within the spinal cord, e.g. due to training (Aagaard et al. 2002) or fatigue, have been assessed in humans by using the H-reflex (Aagaard et al. 2002; Duchateau et al. 2006; Garland and McComas 1990; Zehr 2002), which includes a monosynaptic connection between group Ia afferents and the α-motor neurons (Mnα). Unfortunately, although many investigators have used the H-reflex as an index of Mnα excitability, the connection between the afferents and the Mnα is modulated by presynaptic mechanisms that directly affect neurotransmitter release at the Ia/Mnα synapse (Zehr 2002). The factors that affect presynaptic inhibition include afferent feedback from other peripheral receptors (e.g. Golgi tendon organs, cutaneous mechano-receptors, group III and IV afferent fibers) and descending supraspinal commands (Zehr 2002). Thus, the H-reflex must be evoked under the same experimental conditions (ambient noise, position of the head, etc.) to minimize extraneous factors that can alter its amplitude. In particular, it is necessary to ensure that the stimulus remains the same between sessions, because H-reflex response is heavily modulated by minor changes in stimulus intensity. This is usually performed by using a stimulation intensity that produces a certain percentage of maximal M wave response (Aagaard et al. 2002). Also, it has been shown that H-reflex excitability measured during MVCs increased with strength training but this was not the case for resting H-reflex amplitude (Aagaard et al. 2002). It was then suggested that H-reflexes evoked during voluntary contractions likely represent a more functional estimate of the motoneurone excitability (including presynaptic inhibition) than measurements of the H-reflex at rest. To distinguish cortical from spinal changes (see next paragraph), motor-evoked potentials (MEPs) induced by transcranial magnetic stimulation (TMS) over the motor cortex have been compared with H-reflexes. Both responses are influenced by the level of motoneurone excitability, but the H-reflex does not test the same input axons or synapses as does corticospinal input to motoneurones (Petersen et al. 2002). This is one reason why CMEPs have recently been popularized. Another advantage is that they are not subject to pre-synaptic inhibition. CMEPs consist in subcortical stimulations of the descending corticospinal tract (Gandevia et al. 1999; Petersen et al. 2002). For instance, Gandevia et al. (1999) demonstrated a CMEP reduction following a 2-min MVC task, reflecting a reduction in the effectiveness of corticospinal actions on Mnα at the corticomotoneuronal synapse level. CMEPs have to be normalized to M wave responses to account for any peripheral alteration of the EMG signal, particularly during fatigue studies since the M wave’s properties are influenced by the type of fatigue (Cupido et al. 1996; Darques et al. 2003) and differ between muscles. Another type of stimulation is the F wave produced by antidromic motoneurone activation. This technique is not ideal because F waves test only a small portion of the Mnα pool (Taylor and Gandevia 2001). The respective use of these different indexes also depends on the muscle tested.
Limits of ES in assessing central drive
The main limit of the techniques used for measuring %VA is that none of them allows differentiation of the spinal from supraspinal mechanisms implicated in central adaptations. In fact, the methods described above only reflect the neural drive provided by the central nervous system to the muscles and not changes in their ability to generate output from the motor cortex. A way to gain insight into the supraspinal drive is to measure changes in the V wave response (Upton et al. 1971), which has already been used to assess adaptation to training/unloading (Aagaard et al. 2002; Del Balso and Cafarelli 2007; Pensini and Martin 2004; Seynnes et al. 2011) and occasionally for central fatigue (Racinais et al. 2007). A methodological concern of the V wave is that it could be confounded by recurrent F wave responses (Aagaard et al. 2002). Also, supraspinal %VA can be investigated by using TMS (see Fig. 2 and last section).
Measurement of supraspinal voluntary activation (%VA) of the quadriceps Superimposed twitches are magnetically evoked to the motor cortex at 50, 75 and 100% of maximal voluntary contraction (MVC) (a, b). The reference twitch is not directly measured as in Fig. 1 but interpolated (SIT) from the regression shown in c. Trials 1, 2 and 3 highlight the good intra-day and inter-day reproducibility (Goodall et al. 2009). With transcranial magnetic stimulation (TMS), electrical stimulation (ES) of the femoral nerve is required to normalize the motor-evoked potential to the maximal M wave and to compare supraspinal %VA with ‘classic’ %VA determined using ES of the femoral nerve. Adapted from (Goodall et al. 2009); (Sidhu et al. 2009b)
Another important limitation of the techniques to determine maximal %VA is probably that they all require an MVC which may be problematic with patients or subjects not familiar with maximal contractions. The cause of the large central activation failure in patients is unclear and could be due to reduced concentration, motivation or effort (Schillings et al. 2007). However, it is not recommended to extrapolate the relationship between interpolated twitch and voluntary force to predict maximal force (Taylor 2009). An additional limit in the determination of %VA is the fact that the superimposed stimulus is not always delivered on the force plateau. Correction factors (Strojnik and Komi 1998) and automatic methods (torque-based triggering or time-based triggering methods) (Krishnan et al. 2009) have been proposed to resolve this problem. Other potential methodological limits of this technique can be found elsewhere (de Haan et al. 2009; Taylor 2009). Finally, it has been argued that maximal %VA may be associated with different capacities of activation at high-speed dynamic contractions, i.e. the force over the first 40 ms of a contraction. This latter factor was highly correlated with the initial EMG, indicating that differences in neural drive underlie this variation (de Ruiter et al. 2004).
Use of ES to evaluate peripheral response
From single stimulation to high-frequency tetanus
Peripheral changes can be investigated with ES, usually by stimulating the motor nerve when the muscle is in its relaxed state. The standard method is to first determine optimal intensity by progressively increasing the intensity of the stimulus to optimal intensity, which is defined as the intensity of the stimulation required to attain maximal isometric twitch torque (Pt) or M wave amplitude. Supramaximal intensity—generally 120 to 150% of optimal intensity—is usually chosen to ascertain full spatial recruitment with small changes in electrode position even if such high intensity may induce co-activation in some muscle groups, e.g. dorsiflexors when stimulating plantar flexors through the tibial nerve. The same is true for motor point stimulation, e.g. the triceps brachii can be inadvertently stimulated if the stimulus intensity applied to the biceps brachii is excessive (Awiszus et al. 1997).
Pt cannot be measured from nerve stimulation of every muscle, even when the nerve is superficial enough. For instance, stimulation of the musculocutaneous nerve to evoke a motor response of the elbow flexors induces co-contraction of the elbow extensors invalidating the mechanical response. In this case, nerve stimulation can be used to obtain the M wave but motor point stimulation is required to measure the mechanical response (e.g. Todd et al. 2003). When conditions of nerve stimulation are met, another methodological point has to be considered during repeated contractions: the contradictory effects of potentiation and fatigue (Millet and Lepers 2004; Rankin et al. 1988; Rassier and Macintosh 2000). Indeed, the net twitch tension depends on potentiation (the primary mechanism being phosphorylation of the myosin light chains, which is known to induce increased Ca2+ sensitivity, Rassier and Macintosh 2000) and fatigue-associated effects. This is why it is recommended to measure Pt in the fully potentiated condition (Place et al. 2007). The activation needed to fully potentiate the twitch response may depend on the muscle, i.e. after three 5-s MVCs in the quadriceps (Kufel et al. 2002) versus only one for inspiratory muscles (Mador et al. 1994). Potentiation may actually depend on the force–time integral produced before the twitch (Mettler and Griffin 2010). Despite the potentiated twitch being a more sensitive index of contractile fatigue than the unpotentiated twitch (Kufel et al. 2002), full potentiation has not been systematically used in the literature [e.g. (Millet et al. 2002)]. In addition to potentiation, other parameters such as musculo-tendinous stiffness may also affect the mechanical response to a single ES pulse. For instance, when measured in similar conditions in two different exercises at the same relative power (55% VO2max) and duration (5 h), Pt has been found to decrease in cycling (Lepers et al. 2002) and increase in running (Place et al. 2004).
Another solution for assessing peripheral changes is to induce high-frequency tetanus (Duchateau and Hainaut 1984; Millet et al. 2003a). The problem with this method when applied to large muscle groups is its ‘brutality’. Depending on the muscle groups, this type of stimulation may be painful and/or induce cramping. Alternatively, the use of absolute electrically evoked force when a tetanus induced by nerve stimulation at supramaximal intensity (high-frequency stimulation) is superimposed on an MVC (i.e. similar to the central activation ratio method) as an index of ‘intrinsic’ force (Martin et al. 2010) has also been proposed. While it is a little less painful than evoked high-frequency tetanus on a relaxed muscle (Millet et al. 2003a), the level of discomfort remains high. In addition, it may lead to injuries, for example, a knee cap dislocated during an experiment (Bigland-Ritchie et al. 1978). A compromise for examining contractile response might be to use high-frequency paired pulses (Place et al. 2007; Verges et al. 2009), even if this measure is still prone to be affected by potentiation and stiffness changes.
The force–frequency relationship is another tool used to characterize a muscle’s contractile properties. This relationship can be deduced from several trains of stimulation at different frequencies (Binder-Macleod and McDermond 1992; Edwards et al. 1977) or from a single prolonged stimulus that includes several frequencies (Orizio et al. 2004). During in vivo studies conducted in humans, particularly during fatigue experiments, it is possible to use only two trains of stimulation at low- (below the fusion frequency, e.g. 10–20 Hz) and high-frequency (above the fusion frequency, e.g. 80–100 Hz). From the ratio of the mechanical response at low- and high-frequency, the type of peripheral fatigue can be determined. Low-frequency fatigue (LFF) is characterized by a higher relative loss of force at low frequencies of stimulation (Fig. 3) and slow recovery (Edwards et al. 1977; Jones 1996; Metzger and Fitts 1987). Because LFF is frequently but improperly used to describe fatigue induced by low-frequency stimulation, the term ‘prolonged low-frequency force depression’ has been proposed to avoid confusion (Bruton et al. 2008). LFF is usually associated with a failure in the excitation–contraction coupling; intracellular measurements have shown that LFF is due to a reduction in Ca2+ release (Hill et al. 2001; Westerblad et al. 1993), but decreased myofibrillar Ca2+ sensitivity, which could be mediated by reactive oxygen species (Bruton et al. 2008), may also play a role. LFF is mostly seen after eccentric exercises (Martin et al. 2004a, b, 2005; Verges et al. 2009). A recent study suggests that this might be due to a reduced level of the proteins involved in transverse (T)-tubule and sarcoplasmic reticulum membrane apposition named junctophilins (Corona et al. 2010). Conversely, high-frequency fatigue is characterized by an excessive loss of force at high stimulation frequencies and is attributed, at least in part, to an accumulation of extra-cellular K+. For this type of fatigue, rapid recovery of force occurs when the frequency is reduced (Jones 1996). Changes in M wave characteristics have also been used to investigate the neuromuscular propagation of action potentials on the sarcolemma (Bigland-Ritchie 1981) but the automatic correspondence between M wave amplitude/duration and neuromuscular propagation of action potentials has been questioned (Dimitrova and Dimitrov 2002).
Low-frequency fatigue (also named ‘prolonged low-frequency force depression’, Bruton et al. 2008) is characterized by a relative loss of force of stimulation at low frequency (e.g. 20 Hz, a) compared to the force at high-frequency (e.g. 80 Hz, b). This is typical response after an exhaustive eccentric exercise, e.g. here intermittent one-legged downhill running, from (Martin et al. 2005)
An important problem in the evaluation of a patient’s muscular fatigability is motivation since every evaluation assumes that the patients give their best at each test. It has been reported that the variations in performance for time-to-exhaustion are much higher in patients than in controls and that patients show greater variations in MVCs (Vallier et al. 2011). By using ES (or magnetic stimulation) on the relaxed muscle regularly over a test imposing a given load (force or power), it would be possible to make the results of muscle fatigability independent of the patient’s will and motivation. To the best of our knowledge, such a standardized test does not exist.
Limits of ES in assessing peripheral changes
As for central drive assessment, limits have to be acknowledged when ES is used to determine muscle function. For instance, the absence of modification of the low-to-high-frequency ratio after fatiguing exercise (e.g. Place et al. 2004; Martin et al. 2010) could result from the combined effects of LFF, which preferentially depresses low-frequency response, and hyperpolarization, which preferentially depresses high-frequency response. Potentiation and stiffness may also affect the low-frequency response. More importantly, as explained above, the main problem that is encountered with patients is the discomfort associated with supramaximal nerve stimulation so that this testing is not always suitable with fragile populations such as the elderly. Some stimuli are not well tolerated because of discomfort/pain, particularly nerve trunk stimulation of large muscle groups. Consequently, stimulation protocols must be modified for use with frail people. In this regard, submaximal evoked torques could be used but this type of measurement also has limitations. For instance, submaximal quadriceps muscle ES preferentially recruits motor units near the stimulating electrode which are more likely to be fast-twitch ones. Because these motor units are more fatigable than their slow-twitch counterparts, this could lead to an overestimation of the fatigability of the whole muscle. As we explained above muscle damage is partly responsible for LFF after eccentric exercises but because muscle damage is heterogeneously distributed in the muscle, the use of submaximal ES may lead to wrong conclusions. In addition, submaximal muscle ES can activate sensory axons, provide excitatory synaptic input to the Mnα. and produce contractions through a central mechanism (Dean et al. 2007). Despite these limits, we have shown that LFF is comparable when evaluated with nerve and muscle stimulation (Martin et al. 2004b). We also recently suggested that LFF could be evaluated by using low- and high-frequency doublets (Verges et al. 2009) but further studies (e.g. comparing the two methods to assess high-frequency fatigue) are needed to confirm this result. Another method to minimize discomfort would be to use peripheral magnetic stimulation (see last chapter).
Use of electrical stimulation to assess inspiratory and expiratory muscles
The diaphragm is the main inspiratory muscle and is of critical functional significance both for healthy subjects (e.g. during exercise-induced hyperpnoea) and patients (e.g. those with respiratory diseases or neuromuscular dysfunctions). It is innervated exclusively by the phrenic nerve. Functional ES of the phrenic nerve can be used to restore diaphragm muscle activity and thereby ameliorate patient dependency on mechanical ventilation (Shehu and Peli 2008; Sieck and Mantilla 2009). Phrenic nerve stimulation (PNS) also provides the opportunity to specifically investigate the diaphragm independently of other accessory inspiratory muscles. Indexes such as surface EMG, mouth pressure, esophageal or gastric pressures, although not specific for diaphragm contraction when measured during voluntary maneuvers, relate exclusively to the diaphragm when they are derived from PNS. PNS can provide important information regarding the mechanical function of the diaphragm independently of patient cooperation and the influence of the central nervous system. PNS superimposed on naturally occurring or voluntary contractions (i.e. ITT) can also provide an objective estimate of the maximal %VA of the diaphragm.
Different PNS techniques have been used in healthy subjects, less often in patients. Needle stimulation (Aubier et al. 1981) and implanted wire stimulation (Hubmayr et al. 1989) are invasive and rarely used due to the risk of hematoma and phrenic nerve damage. Transcutaneous electrical PNS has been more extensively used in both research and clinical settings. By using electrical PNS, diaphragm fatigue in healthy subjects has been described following loaded breathing (Aubier et al. 1981; Bellemare and Bigland-Ritchie 1987) and intense exercise (Johnson et al. 1993), while diaphragm weakness has been described in several patient populations such as lung diseases (Mier-Jedrzejowicz et al. 1988; Similowski et al. 1991).
In addition to the important methodological aspects developed above for ES which also apply to PNS, specific points have to be considered. A major condition for evaluating the pressure response to PNS is adequate relaxation of the respiratory muscles at the same lung volume, usually the functional residual capacity (Mier et al. 1990). Maintenance of a similar relaxed posture, including thoraco-abdominal configuration (Chen et al. 2000), is also critical because pressure responses to PNS depend on the load the diaphragm acts against, and therefore on the mechanical characteristics of the rib cage and abdominal wall. The phrenic nerve is usually found underneath the posterior border of the sternocleidomastoid muscle, at the level of the cricoid cartilage (Dionne et al. 2009). Maintaining optimal contact between the stimulating electrode and the nerve can be difficult and it may be necessary to impose a significant degree of pressure on the soft tissues of the neck which can be painful for subjects. Furthermore, it is sometimes impossible to dissociate PNS from brachial plexus stimulation, particularly at high current intensities. This can be a source of discomfort for subjects and can theoretically modify the characteristics of the rib cage. Finally, the use of PNS-derived pressures to study the mechanical action of the diaphragm assumes that stimulation is bilateral, and therefore the phrenic nerves have to be stimulated similarly on both sides. Consequently, the technical expertise required for effective electrical PNS may be a source of variability in research studies and limit its use in the clinical field. This explains why cervical magnetic stimulation was developed and validated as an easier and faster method for PNS (see next chapter). Intraday CVs of 7–8% for electrical PNS and 5–7% for cervical magnetic stimulation have been reported (Mador et al. 1996; Wragg et al. 1994).
In addition to the inspiratory muscles, the abdominal muscles are major contributors to respiration, both through their expiratory action on the rib cage and their mechanical linkage with the diaphragm. Their function can be explored by voluntary maneuvers but also by ES, allowing quantification of muscle strength and fatigue (Gandevia et al. 1990; Lim et al. 2007; Mier et al. 1985; Suzuki et al. 1999). For instance, Suzuki et al. (1999) reported a CV of 3% for gastric twitch pressure evoked by abdominal muscle ES as well as a significant alteration in twitch pressure following sit-ups in healthy subjects. From a therapeutic point of view, its use has also been considered to enhance cough in patients with cervical cord injury (Linder 1993). However, direct ES is painful and supramaximality is difficult to achieve. It is also complicated to activate all the abdominal muscle groups at once.
Electrical versus magnetic stimulation
Merton and Morton (1980) were among the first to stimulate the cerebral cortex of intact human subjects using ES. According to Rothwell and co-workers (Rothwell 1991, Rothwell et al. 1991), response to electric stimulation is less affected by the level of cortical excitability than is magnetic stimulation since a higher proportion of the descending volley is initiated directly on the axons of the pyramidal cells. However, two main inconveniences of this technique are that (1) only a small fraction of the current applied to the scalp goes through the brain and (2) the large currents that flow on the surface cause a contraction in nearby scalp muscles which makes the stimulation uncomfortable (Rothwell et al. 1991). This is why cortical stimulation is preferably performed using TMS, with the exception of transcranial direct current stimulation (tDCS) which is still used as an alternative to repetitive TMS (rTMS).
Supraspinal %VA can be investigated using TMS (Gandevia et al. 1996; Todd et al. 2003), which has recently been applied on the knee extensors (Goodall et al. 2009; Sidhu et al. 2009a, b). This method is derived from the ITT except that the resting twitch is not measured directly as it is for nerve stimulation but is an extrapolation from the linear regression between the superimposed twitch and voluntary force at different force levels (Fig. 2).
TMS over the motor cortex can elicit short-latency excitatory responses, i.e. MEPs (Taylor and Gandevia 2001). This response is considered to be both direct (D wave) and indirect (I wave, probably due to excitation of corticospinal neurons by different sets of cortical axons). Similar to CMEPs, MEPs have to be normalized to M wave responses. However, this is not sufficient because when using MEPs to interpret changes at the cortical level, information from more distal motor pathways (as described above) are needed, i.e. ES is still required when using TMS. When TMS is delivered during a voluntary contraction, MEPs are followed by a period of EMG silence called the cortical silent period (CSP), which is too long (sometimes more than 200 ms) to be representative of reduced Mnα excitability. Thus, CSP reflects intracortical inhibition mediated by GABAB receptors (Taylor and Gandevia 2001). It has been shown that an impairment of supraspinal %VA after sustained isometric MVC persists if the muscle is maintained in full ischemia, despite MEPs and CSPs returning to initial values (Gandevia et al. 1996). It was concluded that inadequate neural drive ‘upstream’ of the motor cortex participated in central fatigue.
While ES has been utilized for years to evoke motor responses, the use of magnetic stimulation for peripheral measurements has recently gained popularity, particularly with patients (e.g. Kremenic et al. 2004; O’Brien et al. 2008; Polkey et al. 1996) for the same reason as the use of TMS compared with transcranial electrical stimulation, i.e. to minimize discomfort. Magnetic nerve stimulation has mostly been used for quadriceps assessment (Amann and Dempsey 2008; Decorte et al. in press) using adequate coils (Tomazin et al. 2010). We (Verges et al. 2009) ascertained the correspondence between electrical stimulation (supramaximal intensity) and magnetic stimulation (Fig. 4) of the femoral nerve. We also reported no activation of antagonistic muscles during magnetic stimulation, as during femoral nerve ES (Verges et al. 2009). Magnetic stimulation also allows a valid quantification of %VA levels using the ITT (O’Brien et al. 2008), even with superimposed high-frequency doublets, provided a bi-stimulator is used. Thus, peripheral magnetic stimulation may be useful from a clinical point of view (Laghi 2009). However, further limits exist with this latter technique, in particular for overweight subjects. In fact, we (Tomazin et al. 2011) have shown that the conditions of utilization may not be met in overweight and obese subjects. Supramaximality is also problematic for ES but the limit is usually associated with patients’ discomfort rather than any limitation in stimulator power output as is the case with magnetic stimulation. Moreover, it is usually recommended that optimal intensity must be increased by +20 to +50% to take into account movements of the stimulating tool (see above). In the case of fatigue, it also allows hypoexcitability to be taken into account, i.e. the fact that the activation threshold of motor nerve axons increases after minutes of repetitive use (e.g. Burke 2002; Vagg et al. 1998). Thus, magnetic stimulation at the peripheral level may be limited for fatigue studies even with slightly overweight subjects.
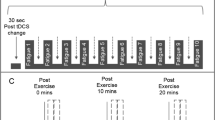
Comparison of changes induced by fatigue in quadriceps peak force evoked by a single twitch (a) and in high-frequency paired-pulses (b) using three stimulation methods: supramaximal electrical stimulation of the femoral nerve (ES), supramaximal magnetic stimulation of the femoral nerve (MS) and submaximal electrical muscle stimulation (EMS). Measurements were performed before (Pre), immediately after (Post) and 30 min after (Post30) the fatiguing exercise which consisted in a 30-min downhill run. Adapted from (Verges et al. 2009)
Regarding diaphragm function testing, cervical magnetic stimulation has been developed and validated as an easier and faster method than PNS for evaluating diaphragm function. The subjects’ tolerance is also improved using cervical magnetic stimulation compared with ES. Nevertheless, there is some co-contraction of the upper rib cage and neck muscles, stiffening the rib cage, so that transdiaphragmatic pressure may be greater than that with electrical PNS (Laghi et al. 1996). As for PNS, magnetic stimulation over the vertebral column at the level of the eighth to tenth thoracic vertebra has been proposed as an interesting alternative to ES for nonvolitional assessment of abdominal muscle strength (Kyroussis et al. 1996, 1997). Again, this allows a decreased level of discomfort for the tested subjects.
As explained earlier, an important difficulty with patients in the evaluation of fatigability is their motivation. To completely remove the influence on the central nervous system, one solution is to use repeated ES contractions and measure the decrement in the kinetics of force, but this induces high levels of discomfort. Assessing muscular endurance by repetitive peripheral magnetic stimulation has been demonstrated to be feasible and well-tolerated in clinical studies (Swallow et al. 2007). According to Taylor (2007), the day-to-day reproducibility of magnetic muscle stimulation measurements is better than ES measurements if the coil is carefully positioned and the same stimulus intensity is used. This may help to easily determine changes in muscle properties with pathology, after exercise, or with training.
Conclusions
In conclusion, electrical stimulation is not only an interesting tool to improve force and muscular endurance in sport and rehabilitation but it also allows the examination of NMF when coupled with force and EMG measurements. A combination of (1) electrical nerve or muscle stimulation, (2) single or multiple (doublets or trains) pulses at different frequencies, (3) stimulations on relaxed or fully contracted muscles, can help to investigate central (mostly at the spinal level) and peripheral adaptations (Fig. 5). For cortical stimulation but also more recently for peripheral stimulation, the use of electrical stimulation for testing purposes may sometimes be advantageously completed by the slightly more comfortable magnetic stimulation, although this latter technique has its own limits. Bearing in mind the limitations of each of these techniques, clinicians should be encouraged to use electrical and magnetic stimulation—associated with both EMG and force response—to assess their patients in their daily practice.
Schematic view of the different electrical and magnetic stimulation techniques to investigate the neuromuscular function. Adapted from (Aagaard et al. 2002). ES electrical stimulation; TMS: transcranial magnetic stimulation, PMS peripheral magnetic stimulation; %VAsuprasp supraspinal maximal voluntary activation, MEP M−1: motor-evoked potential normalized to M wave amplitude; CSP: cortical silent period, V M −1 V wave normalized to M wave amplitude, CAR central activation ratio, %VAper maximal voluntary activation measured from motor nerve stimulation; RMS M −1: EMG (root-mean-square) measured during MVC normalized to M wave amplitude, H M −1 H reflex normalized to M wave amplitude, CMEP M −1 cervicomedullary motor-evoked potential normalized to M wave amplitude, M wave EMG response to motor nerve single stimulation, HFtet tetanus at high frequency of stimulation (>50 Hz); Db100: force evoked by double-pulse at high frequency (usually 100 Hz), LF/HFmax and submax ratio of force evoked at low-frequency of stimulation (usually 10–20 Hz) to force evoked at high-frequency of stimulation (>50 Hz), it can be muscle (submaximal) or nerve (supramaximal) stimulation, Pt peak twitch = force evoked by single-pulse, MVC maximal voluntary contraction. Asterisk means suitable with ‘fragile’ population. Normalization to M wave amplitude is particularly important for fatigue studies
References
Aagaard P, Andersen JL, Dyhre-Poulsen P, Leffers AM, Wagner A, Magnusson SP, Halkjaer-Kristensen J, Simonsen EB (2001) A mechanism for increased contractile strength of human pennate muscle in response to strength training: changes in muscle architecture. J Physiol 534:613–623
Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P (2002) Neural adaptation to resistance training: changes in evoked V wave and H-reflex responses. J Appl Physiol 92:2309–2318
Allen GM, Gandevia SC, Neering IR, Hickie I, Jones R, Middleton J (1994) Muscle performance, voluntary activation and perceived effort in normal subjects and patients with prior poliomyelitis. Brain 117(Pt 4):661–670
Allen GM, Gandevia SC, McKenzie DK (1995) Reliability of measurements of muscle strength and voluntary activation using twitch interpolation. Muscle Nerve 18:593–600
Amann M, Dempsey JA (2008) Locomotor muscle fatigue modifies central motor drive in healthy humans and imposes a limitation to exercise performance. J Physiol 586:161–173
Aubier M, Farkas G, De Troyer A, Mozes R, Roussos C (1981) Detection of diaphragmatic fatigue in man by phrenic stimulation. J Appl Physiol 50:538–544
Awiszus F, Wahl B, Meinecke I (1997) Influence of stimulus cross talk on results of the twitch-interpolation technique at the biceps brachii muscle. Muscle Nerve 20:1187–1190
Babault N, Pousson M, Ballay Y, Van Hoecke J (2001) Activation of human quadriceps femoris during isometric, concentric, and eccentric contractions. J Appl Physiol 91:2628–2634
Baudry S, Klass M, Pasquet B, Duchateau J (2007) Age-related fatigability of the ankle dorsiflexor muscles during concentric and eccentric contractions. Eur J Appl Physiol 100:515–525
Behm DG, St-Pierre DM, Perez D (1996) Muscle inactivation: assessment of interpolated twitch technique. J Appl Physiol 81:2267–2273
Behm DG, Power K, Drinkwater E (2001) Comparison of interpolation and central activation ratios as measures of muscle inactivation. Muscle Nerve 24:925–934
Bellemare F, Bigland-Ritchie B (1987) Central components of diaphragmatic fatigue assessed by phrenic nerve stimulation. J Appl Physiol 62:1307–1316
Bigland-Ritchie B (1981) EMG and fatigue of human voluntary and stimulated contractions. Ciba Found Symp 82:130–156
Bigland-Ritchie B, Jones DA, Hosking GP, Edwards RH (1978) Central and peripheral fatigue in sustained maximum voluntary contractions of human quadriceps muscle. Clin Sci Mol Med 54:609–614
Binder-Macleod SA, McDermond LR (1992) Changes in the force-frequency relationship of the human quadriceps femoris muscle following electrically and voluntarily induced fatigue. Phys Ther 72:95–104
Bruton JD, Place N, Yamada T, Silva JP, Andrade FH, Dahlstedt AJ, Zhang SJ, Katz A, Larsson NG, Westerblad H (2008) Reactive oxygen species and fatigue-induced prolonged low-frequency force depression in skeletal muscle fibres of rats, mice and SOD2 overexpressing mice. J Physiol 586:175–184
Burke D (2002) Effects of activity on axonal excitability: implications for motor control studies. Adv Exp Med Biol 508:33–37
Chen R, Kayser B, Yan S, Macklem PT (2000) Twitch transdiaphragmatic pressure depends critically on thoracoabdominal configuration. J Appl Physiol 88:54–60
Corona BT, Balog EM, Doyle JA, Rupp JC, Luke RC, Ingalls CP (2010) Junctophilin damage contributes to early strength deficits and EC coupling failure after eccentric contractions. Am J Physiol 298:C365–C376
Cupido CM, Galea V, McComas AJ (1996) Potentiation and depression of the M wave in human biceps brachii. J Physiol 491(Pt 2):541–550
Darques JL, Bendahan D, Roussel M, Giannesini B, Tagliarini F, Le Fur Y, Cozzone PJ, Jammes Y (2003) Combined in situ analysis of metabolic and myoelectrical changes associated with electrically induced fatigue. J Appl Physiol 95:1476–1484
de Haan A, Gerrits KH, de Ruiter CJ (2009) Counterpoint: the interpolated twitch does not provide a valid measure of the voluntary activation of muscle. J Appl Physiol 107:355–357 (discussion 357–358)
de Ruiter CJ, Kooistra RD, Paalman MI, de Haan A (2004) Initial phase of maximal voluntary and electrically stimulated knee extension torque development at different knee angles. J Appl Physiol 97:1693–1701
Dean JC, Yates LM, Collins DF (2007) Turning on the central contribution to contractions evoked by neuromuscular electrical stimulation. J Appl Physiol 103:170–176
Decorte N, Lafaix PA, Millet GY, Wuyam B, Verges S (in press) Central and peripheral fatigue kinetics during exhaustive constant-load cycling. Scandinavian journal of medicine & science in sports
Del Balso C, Cafarelli E (2007) Adaptations in the activation of human skeletal muscle induced by short-term isometric resistance training. J Appl Physiol 103:402–411
Dimitrova NA, Dimitrov GV (2002) Amplitude-related characteristics of motor unit and M wave potentials during fatigue.A simulation study using literature data on intracellular potential changes found in vitro. J Electromyogr Kinesiol 12:339–349
Dionne A, Parkes A, Engler B, Watson BV, Nicolle MW (2009) Determination of the best electrode position for recording of the diaphragm compound muscle action potential. Muscle Nerve 40:37–41
Duchateau J (2009) Stimulation conditions can improve the validity of the interpolated twitch technique. J Appl Physiol 107:361 (discussion 367–368)
Duchateau J, Hainaut K (1984) Isometric or dynamic training: differential effects on mechanical properties of a human muscle. J Appl Physiol 56:296–301
Duchateau J, Semmler JG, Enoka RM (2006) Training adaptations in the behavior of human motor units. J Appl Physiol 101:1766–1775
Edwards RH, Hill DK, Jones DA, Merton PA (1977) Fatigue of long duration in human skeletal muscle after exercise. J Physiol 272:769–778
Gandevia SC (1998) Neural control in human muscle fatigue: changes in muscle afferents, motoneurones and motor cortical drive [corrected]. Acta Physiol Scand 162:275–283
Gandevia SC (2001) Spinal and supraspinal factors in human muscle fatigue. Physiol Rev 81:1725–1789
Gandevia SC, McKenzie DK, Plassman BL (1990) Activation of human respiratory muscles during different voluntary manoeuvres. J Physiol 428:387–403
Gandevia SC, Allen GM, Butler JE, Taylor JL (1996) Supraspinal factors in human muscle fatigue: evidence for suboptimal output from the motor cortex. J Physiol 490(Pt 2):529–536
Gandevia SC, Herbert RD, Leeper JB (1998) Voluntary activation of human elbow flexor muscles during maximal concentric contractions. J Physiol 15(Pt 2):595–602
Gandevia SC, Petersen N, Butler JE, Taylor JL (1999) Impaired response of human motoneurones to corticospinal stimulation after voluntary exercise. J Physiol 521(Pt 3):749–759
Garland SJ, McComas AJ (1990) Reflex inhibition of human soleus muscle during fatigue. J Physiol 429:17–27
Goodall S, Romer LM, Ross EZ (2009) Voluntary activation of human knee extensors measured using transcranial magnetic stimulation. Exp Physiol 94:995–1004
Harridge SD, Magnusson G, Gordon A (1996) Skeletal muscle contractile characteristics and fatigue resistance in patients with chronic heart failure. Eur Heart J 17:896–901
Hill CA, Thompson MW, Ruell PA, Thom JM, White MJ (2001) Sarcoplasmic reticulum function and muscle contractile character following fatiguing exercise in humans. J Physiol 531:871–878
Horstman AM, Beltman MJ, Gerrits KH, Koppe P, Janssen TW, Elich P, de Haan A (2008) Intrinsic muscle strength and voluntary activation of both lower limbs and functional performance after stroke. Clin Physiol Funct Imaging 28:251–261
Hubmayr RD, Litchy WJ, Gay PC, Nelson SB (1989) Transdiaphragmatic twitch pressure. Effects of lung volume and chest wall shape. Am Rev Respir Dis 139:647–652
Hultman E, Sjoholm H, Jaderholm-Ek I, Krynicki J (1983) Evaluation of methods for electrical stimulation of human skeletal muscle in situ. Pflugers Arch 398:139–141
Johnson BD, Babcock MA, Suman OE, Dempsey JA (1993) Exercise-induced diaphragmatic fatigue in healthy humans. J Physiol 460:385–405
Jones DA (1996) High-and low-frequency fatigue revisited. Acta Physiol Scand 156:265–270
Kremenic IJ, Ben-Avi SS, Leonhardt D, McHugh MP (2004) Transcutaneous magnetic stimulation of the quadriceps via the femoral nerve. Muscle Nerve 30:379–381
Krishnan C, Allen EJ, Williams GN (2009) Torque-based triggering improves stimulus timing precision in activation tests. Muscle Nerve 40:130–133
Kufel TJ, Pineda LA, Mador MJ (2002) Comparison of potentiated and unpotentiated twitches as an index of muscle fatigue. Muscle Nerve 25:438–444
Kyroussis D, Mills GH, Polkey MI, Hamnegard CH, Koulouris N, Green M, Moxham J (1996) Abdominal muscle fatigue after maximal ventilation in humans. J Appl Physiol 81:1477–1483
Kyroussis D, Polkey MI, Mills GH, Hughes PD, Moxham J, Green M (1997) Simulation of cough in man by magnetic stimulation of the thoracic nerve roots. Am J Respir Crit Care Med 156:1696–1699
Laghi F (2009) Advancing femoral nerve stimulation into the stage of science. J Appl Physiol 106:356–357
Laghi F, Harrison MJ, Tobin MJ (1996) Comparison of magnetic and electrical phrenic nerve stimulation in assessment of diaphragmatic contractility. J Appl Physiol 80:1731–1742
Lepers R, Maffiuletti NA, Rochette L, Brugniaux J, Millet GY (2002) Neuromuscular fatigue during a long-duration cycling exercise. J Appl Physiol 92:1487–1493
Lim J, Gorman RB, Saboisky JP, Gandevia SC, Butler JE (2007) Optimal electrode placement for noninvasive electrical stimulation of human abdominal muscles. J Appl Physiol 102:1612–1617
Linder SH (1993) Functional electrical stimulation to enhance cough in quadriplegia. Chest 103:166–169
Mador MJ, Magalang UJ, Kufel TJ (1994) Twitch potentiation following voluntary diaphragmatic contraction. Am J Respir Crit Care Med 149:739–743
Mador MJ, Rodis A, Magalang UJ, Ameen K (1996) Comparison of cervical magnetic and transcutaneous phrenic nerve stimulation before and after threshold loading. Am J Respir Crit Care Med 154:448–453
Martin A, Carpentier A, Guissard N, van Hoecke J, Duchateau J (1999) Effect of time of day on force variation in a human muscle. Muscle Nerve 22:1380–1387
Martin V, Millet GY, Lattier G, Perrod L (2004a) Effects of recovery modes after knee extensor muscles eccentric contractions. Med Sci Sports Exerc 36:1907–1915
Martin V, Millet GY, Martin A, Deley G, Lattier G (2004b) Assessment of low-frequency fatigue with two methods of electrical stimulation. J Appl Physiol 97:1923–1929
Martin V, Millet GY, Lattier G, Perrod L (2005) Why does knee extensor muscles torque decrease after eccentric-type exercise? J Sports Med Phys Fitness 45:143–151
Martin V, Kerhervé H, Messonnier LA, Banfi JC, Geyssant A, Bonnefoy R, Féasson L, Millet GY (2010) Central and peripheral contributions to neuromuscular fatigue induced by a 24-h treadmill run. J Appl Physiol 108:1224–1233
Merton PA (1954) Voluntary strength and fatigue. J Physiol 123:553–564
Merton PA, Morton HB (1980) Stimulation of the cerebral cortex in the intact human subject. Nature 285:227
Mettler JA, Griffin L (2010) What are the stimulation parameters that affect the extent of twitch force potentiation in the adductor pollicis muscle? Eur J Appl Physiol 110:1235–1242
Metzger JM, Fitts RH (1987) Fatigue from high- and low-frequency muscle stimulation: contractile and biochemical alterations. J Appl Physiol 62:2075–2082
Mier A, Brophy C, Estenne M, Moxham J, Green M, De Troyer A (1985) Action of abdominal muscles on rib cage in humans. J Appl Physiol 58:1438–1443
Mier A, Brophy C, Moxham J, Green M (1990) Influence of lung volume and rib cage configuration on transdiaphragmatic pressure during phrenic nerve stimulation in man. Respir Physiol 80:193–202
Mier-Jedrzejowicz A, Brophy C, Moxham J, Green M (1988) Assessment of diaphragm weakness. Am Rev Respir Dis 137:877–883
Millet GY, Lepers R (2004) Alterations of neuromuscular function after prolonged running, cycling and skiing exercises. Sports Med 34:105–116
Millet GY, Lepers R, Maffiuletti NA, Babault N, Martin V, Lattier G (2002) Alterations of neuromuscular function after an ultramarathon. J Appl Physiol 92:486–492
Millet GY, Martin V, Lattier G, Ballay Y (2003a) Mechanisms contributing to knee extensor strength loss after prolonged running exercise. J Appl Physiol 94:193–198
Millet GY, Martin V, Maffiuletti NA, Martin A (2003b) Neuromuscular fatigue after a ski skating marathon. Can J Appl Physiol 28:434–445
Millet GY, Tomazin K, Verges S, Vincent C, Bonnefoy R, Boisson RC, Gergele L, Bonnefoy R, Féasson L, Martin V (2011) Neuromuscular consequences of an extreme mountain ultra-marathon. PLoS ONE 6:e17059
O’Brien TD, Reeves ND, Baltzopoulos V, Jones DA, Maganaris CN (2008) Assessment of voluntary muscle activation using magnetic stimulation. Eur J Appl Physiol 104:49–55
Orizio C, Gobbo M, Diemont B (2004) Changes of the force-frequency relationship in human tibialis anterior at fatigue. J Electromyogr Kinesiol 14:523–530
Pensini M, Martin A (2004) Effect of voluntary contraction intensity on the H-reflex and V wave responses. Neurosci Lett 367:369–374
Petersen NT, Taylor JL, Gandevia SC (2002) The effect of electrical stimulation of the corticospinal tract on motor units of the human biceps brachii. J Physiol 544:277–284
Place N, Lepers R, Deley G, Millet GY (2004) Time course of neuromuscular alterations during a prolonged running exercise. Med Sci Sports Exerc 36:1347–1356
Place N, Maffiuletti NA, Martin A, Lepers R (2007) Assessment of the reliability of central and peripheral fatigue after sustained maximal voluntary contraction of the quadriceps muscle. Muscle Nerve 35:486–495
Place N, Casartelli N, Glatthorn JF, Maffiuletti NA (2010) Comparison of quadriceps inactivation between nerve and muscle stimulation. Muscle Nerve 42:894–900
Polkey MI, Kyroussis D, Hamnegard CH, Mills GH, Green M, Moxham J (1996) Quadriceps strength and fatigue assessed by magnetic stimulation of the femoral nerve in man. Muscle Nerve 19:549–555
Racinais S, Girard O, Micallef JP, Perrey S (2007) Failed excitability of spinal motoneurons induced by prolonged running exercise. J Neurophysiol 97:596–603
Rankin LL, Enoka RM, Volz KA, Stuart DG (1988) Coexistence of twitch potentiation and tetanic force decline in rat hindlimb muscle. J Appl Physiol 65:2687–2695
Rassier DE, Macintosh BR (2000) Coexistence of potentiation and fatigue in skeletal muscle. Braz J Med Biol Res 33:499–508
Rothwell JC (1991) Physiological studies of electric and magnetic stimulation of the human brain. Electroencephalogr Clin Neurophysiol 43:29–35
Rothwell JC, Thompson PD, Day BL, Boyd S, Marsden CD (1991) Stimulation of the human motor cortex through the scalp. Exp Physiol 76:159–200
Rutherford OM, Jones DA, Newham DJ (1986) Clinical and experimental application of the percutaneous twitch superimposition technique for the study of human muscle activation. J Neurol Neurosurg Psychiatry 49:1288–1291
Sale DG (1988) Neural adaptation to resistance training. Med Sci Sports Exerc 20:S135–S145
Schillings ML, Kalkman JS, Janssen HM, van Engelen BG, Bleijenberg G, Zwarts MJ (2007) Experienced and physiological fatigue in neuromuscular disorders. Clin Neurophysiol 118:292–300
Seynnes OR, Maffiuletti NA, Horstman AM, Narici MV (2011) Increased H-reflex excitability is not accompanied by changes in neural drive following 24 days of unilateral lower limb suspension. Muscle Nerve 42:749–755
Shehu I, Peli E (2008) Phrenic nerve stimulation. Eur J Anaesthesiol Suppl 42:186–191
Sidhu SK, Bentley DJ, Carroll TJ (2009a) Cortical voluntary activation of the human knee extensors can be reliably estimated using transcranial magnetic stimulation. Muscle Nerve 39:186–196
Sidhu SK, Bentley DJ, Carroll TJ (2009b) Locomotor exercise induces long-lasting impairments in the capacity of the human motor cortex to voluntarily activate knee extensor muscles. J Appl Physiol 106:556–565
Sieck GC, Mantilla CB (2009) Novel method for physiological recruitment of diaphragm motor units after upper cervical spinal cord injury. J Appl Physiol 107:641–642
Similowski T, Yan S, Gauthier AP, Macklem PT, Bellemare F (1991) Contractile properties of the human diaphragm during chronic hyperinflation. N Engl J Med 325:917–923
Strojnik V, Komi PV (1998) Neuromuscular fatigue after maximal stretch-shortening cycle exercise. J Appl Physiol 84:344–350
Suzuki J, Tanaka R, Yan S, Chen R, Macklem PT, Kayser B (1999) Assessment of abdominal muscle contractility, strength, and fatigue. Am J Respir Crit Care Med 159:1052–1060
Swallow EB, Gosker HR, Ward KA, Moore AJ, Dayer MJ, Hopkinson NS, Schols AM, Moxham J, Polkey MI (2007) A novel technique for nonvolitional assessment of quadriceps muscle endurance in humans. J Appl Physiol 103:739–746
Taylor JL (2007) Magnetic muscle stimulation produces fatigue without effort. J Appl Physiol 103:733–734
Taylor JL (2009) Point: the interpolated twitch does/does not provide a valid measure of the voluntary activation of muscle. J Appl Physiol 107:354–355
Taylor JL, Gandevia SC (2001) Transcranial magnetic stimulation and human muscle fatigue. Muscle Nerve 24:18–29
Todd G, Taylor JL, Gandevia SC (2003) Measurement of voluntary activation of fresh and fatigued human muscles using transcranial magnetic stimulation. J Physiol 551:661–671
Todd G, Gorman RB, Gandevia SC (2004) Measurement and reproducibility of strength and voluntary activation of lower-limb muscles. Muscle Nerve 29:834–842
Tomazin K, Verges S, Decorte N, Oulerich A, Millet GY (2010) Effects of coil characteristics for femoral nerve magnetic stimulation. Muscle Nerve 41:406–409
Tomazin K, Verges S, Decorte N, Oulerich A, Maffiuletti NA, Millet GY (2011) Fat tissue alters quadriceps response to femoral nerve magnetic stimulation. Clin Neurophysiol 122:842–847
Upton ARM, McComas AJ, Sica REP (1971) Potentiation of “late” responses evoked in muscles during effor. J Neurol Neurosurg Psychiatry 34:699–711
Vagg R, Mogyoros I, Kiernan MC, Burke D (1998) Activity-dependent hyperpolarization of human motor axons produced by natural activity. J Physiol 507(Pt 3):919–925
Vallier JM, Gruet M, Mely L, Pensini M, Brisswalter J (2011) Neuromuscular fatigue after maximal exercise in patients with cystic fibrosis. J Electromyogr Kinesiol (in press)
Van Cutsem M, Duchateau J, Hainaut K (1998) Changes in single motor unit behaviour contribute to the increase in contraction speed after dynamic training in humans. J Physiol 513(Pt 1):295–305
Verges S, Maffiuletti NA, Kerherve H, Decorte N, Wuyam B, Millet GY (2009) Comparison of electrical and magnetic stimulations to assess quadriceps muscle function. J Appl Physiol 106:701–710
Westerblad H, Duty S, Allen DG (1993) Intracellular calcium concentration during low-frequency fatigue in isolated single fibers of mouse skeletal muscle. J Appl Physiol 75:382–388
Wragg S, Aquilina R, Moran J, Ridding M, Hamnegard C, Fearn T, Green M, Moxham J (1994) Comparison of cervical magnetic stimulation and bilateral percutaneous electrical stimulation of the phrenic nerves in normal subjects. Eur Respir J 7:1788–1792
Yue GH, Ranganathan VK, Siemionow V, Liu JZ, Sahgal V (1999) Older adults exhibit a reduced ability to fully activate their biceps brachii muscle. J Gerontol 54:M249–M253
Zehr PE (2002) Considerations for use of the Hoffmann reflex in exercise studies. Eur J Appl Physiol 86:455–468
Zierath JR, Hawley JA (2004) Skeletal muscle fiber type: influence on contractile and metabolic properties. PLoS Biol 2:e348
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Roberto Bottinelli.
Rights and permissions
About this article
Cite this article
Millet, G.Y., Martin, V., Martin, A. et al. Electrical stimulation for testing neuromuscular function: from sport to pathology. Eur J Appl Physiol 111, 2489–2500 (2011). https://doi.org/10.1007/s00421-011-1996-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-1996-y