Abstract
The purpose of this study was to investigate the acute effects of passive stretching on the electromechanical delay (EMD), peak twitch force (PTF), rate of force development (RFD), and compound muscle action potential (M-wave) amplitude during evoked twitches of the plantar flexor muscles. 16 men (mean age ± SD = 21.1 ± 1.7 years; body mass = 75.9 ± 11.4 kg; height = 176.5 ± 8.6 cm) participated in this study. A single, square-wave, supramaximal transcutaneous electrical stimulus was delivered to the tibial nerve before and after passive stretching. The stretching protocol consisted of nine repetitions of passive assisted stretching designed to stretch the calf muscles. Each repetition was held for 135 s separated by 5–10 s of rest. Dependent-samples t tests (pre- vs. post-stretching) were used to analyze the EMD, PTF, RFD, and M-wave amplitude data. There were significant changes (P ≤ 0.05) from pre- to post-stretching for EMD (mean ± SE = 4.84 ± 0.31 and 6.22 ± 0.34 ms), PTF (17.2 ± 1.3 and 15.6 ± 1.5), and RFD (320.5 ± 24.5 and 279.8 ± 28.2), however, the M-wave amplitude did not change (P > 0.05). These findings suggested that passively stretching the calf muscles affected the mechanical aspects of force production from the onset of the electrically evoked twitch to the peak twitch force. These results may help to explain the mechanisms underlying the stretching-induced force deficit that have been reported as either “mechanical” or “electrical” in origin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent evidence has shown that a bout of stretching may temporarily reduce the force producing capabilities of a muscle (Avela et al. 1999, 2004; Behm et al. 2001; Costa et al. 2009a; Cramer et al. 2004, 2005, 2007; Evetovich et al. 2003; Fowles et al. 2000; Herda et al. 2008b; Kokkonen et al. 1998; Kubo et al. 2001; Nelson et al. 2001a, b; Nelson and Kokkonen 2001; Power et al. 2004; Ryan et al. 2008b; Weir et al. 2005). This has been demonstrated during voluntary isokinetic (Costa et al. 2009a; Cramer et al. 2004, 2005, 2007; Evetovich et al. 2003; Nelson et al. 2001b), isotonic (Kokkonen et al. 1998; Nelson and Kokkonen 2001), and isometric (Avela et al. 1999, 2004; Behm et al. 2001; Fowles et al. 2000; Herda et al. 2008b; Kubo et al. 2001; Nelson et al. 2001a; Ogura et al. 2007; Power et al. 2004; Ryan et al. 2008b; Weir et al. 2005) muscle actions as well as involuntary, evoked twitches (Avela et al. 2004; Behm et al. 2001; Cè et al. 2008; Ryan et al. 2008b). This transient reduction in force production after stretching has been termed the “stretching-induced force deficit” (Ryan et al. 2008b), and it has been implicated as detrimental to athletic performance (Rubini et al. 2007; Shrier 2004). Therefore, practical recommendations have been made to either discontinue static stretching prior to athletic events (Kokkonen et al. 1998; Nelson et al. 2001b, 2005; Nelson and Kokkonen 2001; Shrier 2004) and rehabilitation testing (Costa et al. 2009a, b; Marek et al. 2005), engage in other types of pre-exercise stretching (i.e., dynamic stretching) (Yamaguchi and Ishii 2005), or conduct stretching regiments after exercise or performances to attain the benefits of chronic stretching (Shrier 2004). Understanding the mechanisms that are responsible for the stretching-induced force deficit may provide insight regarding such practical recommendations (Kokkonen et al. 1998; Shrier 2004; Yamaguchi and Ishii 2005). Although the precise mechanisms are unknown, a growing body of literature has suggested that the stretching-induced force deficit is caused by neural factors that reduce muscle activation, mechanical factors that affect the transmittal of force and/or the length-tension relationship, or a combination of both the neural and mechanical factors (Avela et al. 1999; Behm et al. 2001, 2004; Cè et al. 2008; Cramer et al. 2004, 2005, 2007; Evetovich et al. 2003; Fowles et al. 2000; Herda et al. 2008a, b; Kokkonen et al. 1998; Marek et al. 2005; McHugh and Nesse 2008; Nelson et al. 2001a; Power et al. 2004; Rosenbaum and Hennig 1995).
Several studies have shown that an acute bout of stretching may cause decreases in muscle activation (Avela et al. 1999; Behm et al. 2001, 2004; Cramer et al. 2004, 2005; Evetovich et al. 2003; Fowles et al. 2000; Kokkonen et al. 1998; Marek et al. 2005; Nelson et al. 2001a; Power et al. 2004). For example, Avela et al. (1999), Behm et al. (2001), and Fowles et al. (2000) have demonstrated 15–20% decrements in electromyographic (EMG) amplitude following stretching. Specifically, Fowles et al. (2000) found a 15% decrease in EMG amplitude after 30 min of passive stretching of the plantar-flexors and reported that 57% of the force decreases were attributed to neural factors. In addition, Behm et al. (2001) found 20% decreases in EMG amplitude following 20 min of stretching and suggested that the decrements in force observed post-stretching were primarily due to neural rather than mechanical factors. Cramer et al. (2005) found decreases in force and EMG amplitude in the stretched and unstretched leg extensor muscles, which tentatively suggested that the stretching-induced force deficit may have been caused in part by an unidentified central nervous system inhibitory mechanism.
Other studies have indicated that mechanical factors may also explain the stretching-induced force deficit. For example, Fowles et al. (2000) reported that most of the force decreases from stretching were attributed to alterations in the mechanical properties of the musculotendinous unit rather than neural factors. The authors suggested that the stretching may have altered the length–tension relationship and/or caused plastic deformation of the connective tissues that help to transfer force from the contractile component to the bone (Fowles et al. 2000). In addition, Nelson et al. (2001a) was among the first to report joint-angle specific decreases in isometric force at the shortest muscle length (i.e., 162° of leg extension), but no decreases were found at the longer muscle lengths (i.e., 90°, 108°, 126°, and 144° of leg extension), which was further evidence suggesting that stretching may alter the length-tension relationship. Other studies have shown similar acute effects of stretching in the hamstrings muscles (Herda et al. 2008a; McHugh and Nesse 2008). Similarly, Cramer et al. (2007) reported that an acute bout of stretching the leg extensors “flattened” the shape of the isokinetic angle-torque curve, although the area under the curve was unaltered by the stretching. These findings tentatively suggested that stretching may decrease the peak torque, but may allow for greater torque production at the extremes of the range of motion (Cramer et al. 2007). The authors further conjectured that these findings may also translate to how stretching may affect the sarcomeric length–tension relationship (Cramer et al. 2007). Furthermore, acute stretching is thought to provoke transient decreases in musculotendinous stiffness (Kubo et al. 2001; Magnusson et al. 1996; Morse et al. 2008; Ryan et al. 2008a), which have largely been attributed to alterations in the viscoelastic properties of the stretched tissues—particularly the noncontractile connective tissues. Since these connective tissues are responsible for transferring force from the sarcomeres to the bone, stretching may transiently affect the efficiency of this force transfer.
A time delay exists from the onset of muscle activation to the onset of force development (Cavanagh and Komi 1979). This time delay has been termed the electromechanical delay (EMD) (Cavanagh and Komi 1979; Conforto et al. 2006; Gabriel and Boucher 1998; Hopkins et al. 2007; Vint et al. 2001). It is thought that the elongation of the series elastic component (SEC) of the musculotendinous unit may account for a major portion of the EMD (Cavanagh and Komi 1979), and there may be an inverse relationship between the EMD and musculotendinous stiffness (Grosset et al. 2009). If the EMD is inversely proportional to musculotendinous stiffness and an acute bout of stretching decreases musculotendinous stiffness (Kubo et al. 2001; Magnusson et al. 1996; Morse et al. 2008; Ryan et al. 2008a), then it is possible that the EMD may also be affected by stretching. Furthermore, if the EMD is measured during electrically evoked twitches, it may help to control for any neural factors that may contribute to the stretching-induced force deficit, which in turn, may allow the research study to focus on any potential mechanical factors. Therefore, the purpose of the present study was to investigate the acute effects of passive stretching on the EMD during evoked twitches of the plantar flexor muscles.
Methods
Subjects
Sixteen men (mean age ± SD = 21.1 ± 1.7 years; body mass = 75.9 ± 11.4 kg; height = 176.5 ± 8.6 cm) volunteered for this study that was approved by The University of Oklahoma Institutional Review Board for the protection of human subjects. Prior to the start of testing, all subjects read and signed an informed consent form and completed a health status questionnaire. Ten men reported engaging in 1–5 h week−1 of aerobic exercise, ten reported 2–6 h week−1 of resistance training, and seven reported 1–5 h week−1 of recreational sports. Only one subject did not report some form of weekly exercise. In addition, none of the participants reported any past hip-, knee-, or ankle-related injuries. Therefore, these subjects might be best classified as healthy, college-aged, recreationally active men.
Research design
A repeated measures design (pre- vs. post-stretching) was used to investigate the acute effects of passive stretching on the EMD, PTF, RFD, and the M-waves of the SOL and MG muscles. Subjects visited the laboratory on two occasions separated by 48–120 h. The first visit was a familiarization session, and the subsequent visit was the experimental trial. Familiarization included a practice of the evoked twitch procedure that would be completed during the experimental trial. In addition, the maximum amount of passive torque the participant could tolerate during a stretch (i.e., the point of discomfort, but not pain as acknowledged by the participant) was identified. This stretching intensity (i.e., passive torque) was used to stretch the plantar flexors during the experimental trial. Furthermore, the passive stretching exercises were performed during the familiarization trial to ensure that each subject could tolerate the stretches. During the experimental trial, subjects completed the pre-stretching assessments, the passive stretching protocol, and the post-stretching assessments. The time elapsed from the end of stretching to the start of the post-stretching assessment was approximately 2 min.
Pre- and post-stretching assessments
Each participant was seated with restraining straps over the pelvis and thigh, with a leg flexion angle of 0° below the horizontal plane (full extension) on a custom-built apparatus equipped with a load cell (Omegadyne, model LC402, range 0–500 lbs; Stamford, CT, USA) that was designed to isolate the plantar flexor muscle contributions (Fig. 1). This apparatus was also connected to a calibrated isokinetic dynamometer (Biodex System 3, Biodex Medical Systems, Inc. Shirley, NY, USA, 1998), which allowed the subject to be stretched in “passive mode” while remaining in the apparatus. The lateral malleolus of the fibula was aligned with the input axis of the dynamometer. The foot was secured in a thick rubber heel cup attached to the footplate of the apparatus with straps over the toes and metatarsals (distal to the malleoli). A single, square-wave, supramaximal transcutaneous electrical stimulus was delivered to the tibial nerve before and after passive stretching. Transcutaneous electrical stimuli were delivered to the tibial nerve using a high-voltage (maximal voltage = 400 V), constant-current stimulator (Digitimer DS7AH, Herthfordshire, UK). The cathode was a metal probe (8 mm diameter) with the tip covered in a saline-soaked sponge, which was pressed over the tibial nerve in the popliteal fossa. The anode was a 9 × 5 cm rectangular self-adhesive electrode (Durastick Supreme, Chattanooga Group, Hicton, TN, USA) that was positioned between the tibial tuberosity and the patella. Single stimuli were administered to the tibial nerve at a low current (amperage = 20 mA) to determine the optimal probe location based on the visual inspection of the compound muscle action potential (M-wave) and Hoffmann reflex (H-reflex) of the SOL muscle that were monitored on an external computer. Once the location was determined and marked, the maximal M-wave was achieved with incremental (5 mA) amperage increases until a plateau in the peak-to-peak (p-p) M-wave was observed after three successive amperage increases. To assure a supramaximal stimulus, 120% of the stimulus that elicited the maximal M-wave was used during the evoked twitch procedures. A single stimulus was defined as a 200-μs duration square wave impulse. The EMD was defined as the time (ms) that elapsed between the onset of the M-wave and the onset of the twitch response recorded from the load cell mounted in the apparatus. These onsets were manually determined off-line by an experienced investigator (P.B.C.) using custom-written software that provided interactive graphs viewing the force and EMG signals in 20 ms windows for an accurate visual representation.
Range of motion assessment
The range of motion (ROM) of the plantar flexors was examined pre- and post-stretching for each participant using the isokinetic dynamometer (Biodex System 3, Biodex Medical Systems, Inc. Shirley, NY, USA, 1998) programmed in passive isokinetic mode. The dynamometer lever arm moved at an angular velocity of 5° s−1 until the subject verbally acknowledged the point of discomfort, but not pain. Two assessments were performed pre- and post-stretching and the averages of the two ROM assessments were used to calculate the ROM data. Maximal ROM was calculated as the ROM attained from 90° (between foot and leg) to the maximum tolerable point of passive dorsiflexion.
Surface electromyography
Pre-amplified, bipolar surface EMG electrodes (EL254S, Biopac Systems Inc.; Santa Barbara, CA, USA, gain = 350) with a fixed center-to-center inter-electrode distance of 20 mm were taped over the SOL and MG muscles of the right leg. For the SOL, the electrodes were placed along the longitudinal axis of the tibia at 66% of the distance between the medial condyle of the femur and the medial malleolus. For the MG, the electrodes were placed on the most prominent bulge of the muscle in accordance with the recommendations of Hermens et al. (1999). A single pre-gelled, disposable electrode (Ag–AgCl, Quinton Quick Prep, Quinton Instruments Co., Bothell, WA, USA) was placed on the spinous process of the 7th cervical vertebrae to serve as a reference electrode. To reduce inter-electrode impedance and increase the signal-to-noise ratio, local areas of the skin were shaved and cleaned with isopropyl alcohol prior to placement of the electrodes.
Signal processing
The EMG and force signals were recorded simultaneously with a Biopac data acquisition system (MP150WSW, Biopac Systems, Inc.; Santa Barbara, CA, USA) during each assessment. The force (N) signal from the load cell and the EMG signals from the SOL and MG muscles were sampled at 2 kHz using a 16-bit analog-to-digital converter (DHQCard-6036E, National Instruments, Austin, TX, USA) interfaced with a laptop computer (Inspiron 8200, Dell Inc., Round Rock, TX, USA). All signals were recorded, stored, and processed off-line with custom-written software (LabView 8.5, National Instruments, Austin, TX, USA). EMG signals from the SOL and MG muscles were analog filtered with a pass band of 10–500 Hz. The subsequent M-waves from the SOL and MG were expressed as peak-to-peak (p-p) amplitude values. A digital low-pass filter was applied to the force signal with a cutoff frequency of 20 Hz, and all subsequent force-related variables were computed using the filtered force signal. PTF values (N) were calculated as the highest mean of 20 consecutive data points that occurred at the apex of the evoked twitch. RFD values (N s−1) were represented as the peak of the first derivative of the force signal that occurred between the onset of force production and the apex of the evoked twitch (Cè et al. 2008).
Passive stretching
The right plantar flexor muscles were stretched by an isokinetic dynamometer (Biodex System 3, Biodex Medical Systems, Inc. Shirley, NY, USA, 1998) programmed in passive mode. The dynamometer lever arm was attached to the custom-built apparatus used for testing (Fig. 1). The dynamometer lever arm passively dorsiflexed the foot at 5° s−1 until the maximum tolerable torque threshold (identified during the familiarization trial) was achieved. The dynamometer maintained this torque while the plantar flexors were stretched for 135 s. Approximately 5–10 s elapsed between each passive stretching repetition, which was the time it took for the dynamometer to move the foot to 10° of plantar flexion in order to start the subsequent stretching repetition. The stretching protocol consisted of nine repetitions of passive stretches for a total of 1,215 s (i.e., 20.25 min) of time under stretch.
Statistical analyses
Six separate dependent-samples t tests (pre- vs. post-stretching) were used to analyze the EMD, RFD, PTF, p-p amplitudes for the M-waves of the SOL and MG muscles, and ROM. Pearson product moment correlation coefficients (r) were used to quantify the relationship between EMD and PTF as well as EMD and RFD pre- and post-stretching. An alpha level of P ≤ 0.05 was considered statistically significant for all comparisons. SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analysis. Coefficients of variation (CV) were used to calculate the variability among the passive evoked twitch properties. Table 1 contains the baseline coefficients of variations and standard errors for all dependent variables analyzed.
Results
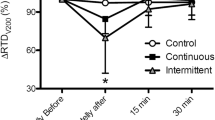
Table 2 contains the means and standard errors (SE) for the pre- and post-stretching values for all of the dependent variables. Figures 1 and 2 present the mean and SE for EMD, PTF, RFD, and p-p M-wave amplitudes values from the SOL and MG muscles before and after the stretching. Dependent t tests (pre- vs. post-stretching) for each variable indicated significant (P ≤ 0.05) stretching-induced changes in EMD, PTF, and RFD. EMD increased by 28%, RFD decreased by 13%, and PTF decreased by 9% from pre- to post-stretching. In addition, ROM had a significant (P ≤ 0.05) increase of 15% from 18.1° (SE = 2.27) to 20.8° (2.40) from pre- to post-stretching. There were no significant (P > 0.05) stretching-induced changes for p-p M-wave amplitude values recorded from the SOL or MG muscles. There were significant (P < 0.05) negative, linear relationships between EMD and PTF pre- and post-stretching (r = −0.52 and r = −0.75, respectively) as well as between EMD and RFD (r = −0.53 and r = −0.79, respectively).
Discussion
The primary findings of the present study indicated that passively stretching the plantar flexors for 20 min increased ROM and affected the mechanical twitch properties of the stretched muscles by increasing the EMD and decreasing the PTF and RFD (Fig. 2). Although this study was the first to examine the acute effects of stretching on the EMD, our findings were consistent with previous studies that have reported stretching-induced decreases in the PTF and the RFD (Cè et al. 2008; Ryan et al. 2008b). Overall, our findings were also consistent with the growing body of literature regarding the stretching-induced force deficit (Rubini et al. 2007), which has shown that an acute bout of stretching can inhibit muscle strength (Behm et al. 2001; Cramer et al. 2004, 2005; Evetovich et al. 2003; Fowles et al. 2000; Kokkonen et al. 1998; Nelson et al. 2001a, b; Power et al. 2004), and power (Cramer et al. 2002) production. Two basic mechanisms have been proposed as the causes of the stretching-induced force deficit: (a) mechanical mechanisms, such as stretching-induced alterations in the length-tension relationship and (b) neural mechanisms, such as decreases in muscle activation as a result of stretching (Avela et al. 1999; Behm et al. 2001, 2004; Cornwell et al. 2002; Cramer et al. 2004; 2005; Evetovich et al. 2003; Fowles et al. 2000; Kokkonen et al. 1998; Nelson et al. 2001a, b; Nelson and Kokkonen 2001; Power et al. 2004).
The EMD has been defined as the time elapsed between the onset of electrical activation of the muscle and the onset of force development (Cavanagh and Komi 1979; Conforto et al. 2006; Gabriel and Boucher 1998; Hopkins et al. 2007; Vint et al. 2001). Several factors may influence the EMD including the time course for the propagation of the action potential, the duration of the excitation–contraction coupling process, and the elongation of the series elastic component (SEC) (Grosset et al. 2009). In addition, the EMD may be influenced by the muscle length (Muro and Nagata 1985), gender (Winter and Brookes 1991), age (Grosset et al. 2005), fatigue (Minshull et al. 2007; Zhou et al. 1996, 1998), type of muscle action (Blanpied and Oksendahl 2006; Cavanagh and Komi 1979; Hopkins et al. 2007; Norman and Komi 1979; Vint et al. 2001; Zhou et al. 1995), training mode and status (Grosset et al. 2009; Linford et al. 2006), and muscle temperature (Zhou et al. 1998). It is believed, however, that the time elapsed during the elongation of the SEC may account for a major portion of the EMD (Cavanagh and Komi 1979). Furthermore, Grosset et al. (2009) recently compared the chronic effects of endurance and plyometric training on the EMD and reported a strong, inverse relationship between the EMD and musculotendinous stiffness. That is, during the course of the endurance training program, there were increases in musculotendinous stiffness and decreases in the EMD whereas the plyometric training program elicited decreases in musculotendinous stiffness along with increases in EMD (Grosset et al. 2009). These previous findings (Grosset et al. 2009) were consistent with a study by Wilson et al. (1994) that reported strong positive correlations between musculotendinous stiffness and isometric and concentric performance. Furthermore, our recent study reported strong positive relationships between musculotendinous stiffness and muscle cross-sectional area (Ryan et al. 2009). The results of the present study also supported these previous findings (Ryan et al. 2009) in that 20 min of passive stretching increased the EMD (Fig. 2a), which suggested that the stretching may have elongated the SEC resulting in a “less stiff” transfer of force from the contractile component to the bone. Since previous studies have demonstrated transient decreases in musculotendinous stiffness after a bout of stretching (Kubo et al. 2001; Magnusson et al. 1996; Morse et al. 2008; Ryan et al. 2008a), it is possible that the stretching may have created more “slack” in the musculotendinous unit that may have diminished the SEC requiring more time (increased EMD) to take up that slack.
In addition to the 28.4% increases in EMD, the stretching protocol in the present study also caused a 9.3% decrease in PTF when evoked with a single square-wave pulse (Fig. 2b). Previous studies have also suggested that stretching may affect twitch force (Avela et al. 2004; Behm et al. 2001; Cè et al. 2008; Fowles et al. 2000; Ryan et al. 2008b). For example, stretching-induced decreases in PTF of 6–18% have been reported (Avela et al. 2004; Behm et al. 2001; Cè et al. 2008; Fowles et al. 2000; Ryan et al. 2008b). However, Herda et al. (2008b) found no changes in PTF evoked with a doublet following 20 min of passive stretching. In addition, Behm et al. (2001) found decreases in PTF when evoked with a single stimulus, but reported no changes in twitch force when summated with a tetanic train of stimuli after a bout of passive stretching. The authors suggested that the force summation caused by the high-frequency tetanic stimuli was sufficient to overcome the stretching-induced increase in laxity of the musculotendinous unit (Behm et al. 2001). Consequently, it was concluded that the causes of the stretching-induced decreases in force were neural in origin (Behm et al. 2001). Avela et al. (2004) also suggested that their findings of reduced twitch amplitudes could have been explained by a greater time required to elongate the slack in the SEC. Thus, overall, the present study found a stretching-induced force deficit that was consistent with previous studies strength (Behm et al. 2001; Cramer et al. 2004, 2005, 2007; Evetovich et al. 2003; Fowles et al. 2000; Kokkonen et al. 1998; Nelson et al. 2001a, b; Power et al. 2004), but the concomitant changes in EMD and RFD suggested that mechanical factors related to increased musculotendinous laxity may be partially responsible.
The RFD is commonly defined as the maximal rate of rise in muscle force and reflects the force generated during the early phase of a muscle action (Aagaard et al. 2002). The RFD is thought to be directly related to success in sport performances involving explosive types of muscle actions (Aagaard et al. 2002; Andersen and Aagaard 2006; Behm and Sale 1993; Haff et al. 2005; Kawamori et al. 2006; Mirkov et al. 2004; Moritani 2002) and is often used as an outcome measure associated with power-related exercises (Haff et al. 2005; Kawamori et al. 2006; Mirkov et al. 2004; Murphy et al. 1994; Stone et al. 2004; Viitasalo and Aura 1984). For example, Kawamori et al. (2006) reported that the RFD was correlated (r = 0.65–0.74) with explosive performance such that as dynamic RFD increased, vertical jump performance also increased, suggesting that athletes who exhibit greater RFD may be able to jump higher. Alternatively, Ryan et al. (2009) hypothesized that there may be an inverse relationship between muscle twitch properties and musculotendinous stiffness. Therefore, it is possible that a stiffer muscle–tendon unit may be able to generate force quicker (greater RFD) than a more compliant muscle. The results of the present study supported this hypothesis and indicated that the passive stretching elicited a 12.7% decrease in the RFD of the evoked twitches (Fig. 1c). These findings were also consistent with those of Cè et al. (2008) who showed a 24% decrease in the RFD as a result of stretching the plantar flexors. Although the precise mechanisms underlying the stretching-induced decrease in RFD are unknown, it may have been related to the decreases in muscle–tendon stiffness through changes in the viscoelastic properties of the connective tissue sheaths surrounding the muscle (Ryan et al. 2008a). Such changes in the perimysium (Morse et al. 2008), for example, may not allow for a rapid transfer of force from the sarcomeres to the bone. However, further studies are needed to test this hypothesis.
The present study was designed to examine the acute effects of stretching on involuntary, evoked muscle twitch properties. To ensure that the stimulation intensities remained consistent, the M-waves that evoked the twitches were measured, and the results indicated that the stretching protocol did not change the M-wave amplitude values for either the SOL or MG muscles (Fig. 3). These findings confirmed that the stimulation intensities were unaltered from pre- to post-stretching. Consequently, the stretching induced changes in EMD, PTF, and RFD were probably not related to any neural factors that were controlled in this study. These findings were in agreement with previous studies that found significant decreases in PTF and RFD following passive stretching, but no changes in EMG amplitude (Cè et al. 2008; Ryan et al. 2008b). For instance, Cè et al. (2008) stated that the lack of change in EMG parameters observed in their investigation implied a preservation of neuromuscular synaptic efficiency and maintenance of action potentials, suggesting that changes in viscoelastic and contraction properties were likely responsible for the deficit in force following passive stretching. Conversely, Weir et al. (2005) reported decreases in p-p M-wave amplitude, but no changes in PTF after 10 min of plantar flexor passive stretching. However, because the authors reported decreases in MVC and passive torque, but no changes in EMG amplitude during the MVCs, they suggested that the decreases in MVC force following stretching may have been attributed to alterations in the mechanical properties of the plantar flexors rather than a decrease in muscle activation. Although we cannot rule out a neural impairment as a possible mechanism underlying the stretching-induced force deficits observed in previous studies (Avela et al. 1999; Behm et al. 2001, 2004; Cramer et al. 2004; 2005; Evetovich et al. 2003; Fowles et al. 2000; Kokkonen et al. 1998; Nelson et al. 2001a, b; Nelson and Kokkonen 2001; Power et al. 2004), the present findings suggested that stretching-induced force deficits measured by evoked twitches may be related to transient decreases in musculotendinous stiffness (Ryan et al. 2008a, b).
Nelson et al. (2001a, b) have shown that stretching caused joint angle-specific decreases in isometric force at the shortest muscle lengths, but not at the longer muscle lengths. These findings suggested that passive stretching may alter the length-tension relationship. Other studies have reported similar findings for the hamstrings muscles, such that the stretching-induced force deficit was observed at short, but not long, muscle lengths (Herda et al. 2008a; McHugh and Nesse 2008). It is possible that the stretching-induced changes in twitch properties observed in the present study may have been more pronounced at shorter muscle lengths and less pronounced at longer muscle lengths. Nevertheless, this observation further validates our hypothesis and conclusion that the mechanism underlying the stretching-induced force deficit in the present study was mechanical in origin. Thus, future studies should examine the acute effects of passive stretching on the EMD and other twitch properties at several different ankle joint angles.
In summary, the results of the present study were consistent with previous findings that have shown acute decrease in PTF and RFD after a bout of stretching (Cè et al. 2008; Ryan et al. 2008b). However, to our knowledge, this study was the first to report acute stretching-induced increases in the EMD. Due to the hypothesized direct relationship between the EMD and musculotendinous stiffness (Grosset et al. 2009), our findings suggested that mechanical factors related to the stiffness of the muscle–tendon unit may contribute to the explanation for why stretching causes acute deficits in the force producing capabilities of evoked twitches. Furthermore, we found no changes in p-p M-wave amplitude from pre- to post-stretching, suggesting that the activation of the plantar flexor muscles was controlled in this study. Thus, the stretching-induced increases in EMD and decreases in PTF and RFD during the evoked muscle actions in this investigation may have been unrelated to muscle activation (i.e., neural factors). Future studies are needed to elaborate on the acute stretching-induced changes in the viscoelastic properties of the connective tissues surrounding the muscles and how these changes affect the relationship between the EMD and force production.
References
Aagaard P, Simonsen EB, Andersen JL, Magnusson P, Dyhre-Poulsen P (2002) Increased rate of force development and neural drive of human skeletal muscle following resistance training. J Appl Physiol 93:1318–1326
Andersen LL, Aagaard P (2006) Influence of maximal muscle strength and intrinsic muscle contractile properties on contractile rate of force development. Eur J Appl Physiol 96:46–52
Avela J, Kyrolainen H, Komi PV (1999) Altered reflex sensitivity after repeated and prolonged passive muscle stretching. J Appl Physiol 86:1283–1291
Avela J, Finni T, Liikavainio T, Niemela E, Komi PV (2004) Neural and mechanical responses of the triceps surae muscle group after 1 h of repeated fast passive stretches. J Appl Physiol 96:2325–2332
Behm DG, Sale DG (1993) Intended rather than actual movement velocity determines velocity-specific training response. J Appl Physiol 74:359–368
Behm DG, Button DC, Butt JC (2001) Factors affecting force loss with prolonged stretching. Can J Appl Physiol 26:261–272
Behm DG, Bambury A, Cahill F, Power K (2004) Effect of acute static stretching on force, balance, reaction time, and movement time. Med Sci Sports Exerc 36:1397–1402
Blanpied P, Oksendahl H (2006) Reaction times and electromechanical delay in reactions of increasing and decreasing force. Percept Mot Skills 103:743–754
Cavanagh PR, Komi PV (1979) Electromechanical delay in human skeletal muscle under concentric and eccentric contractions. Eur J Appl Physiol Occup Physiol 42:159–163
Cè E, Paracchino E, Esposito F (2008) Electrical and mechanical response of skeletal muscle to electrical stimulation after acute passive stretching in humans: a combined electromyographic and mechanomyographic approach. J Sports Sci 26:1567–1577
Conforto S, Mathieu P, Schmid M, Bibbo D, Florestal J, D’Alessio T (2006) How much can we trust the electromechanical delay estimated by using electromyography? pp 1256–1259
Cornwell A, Nelson AG, Sidaway B (2002) Acute effects of stretching on the neuromechanical properties of the triceps surae muscle complex. Eur J Appl Physiol 86:428–434
Costa PB, Ryan ED, Herda TJ, DeFreitas JM, Beck TW, Cramer JT (2009a) Effects of stretching on peak torque and the H:Q ratio. Int J Sports Med 30:60–65
Costa PB, Ryan ED, Herda TJ, DeFreitas JM, Beck TW, Cramer JT (2009b) Effects of static stretching on the hamstrings-to-quadriceps ratio and electromyographic amplitude in men. J Sports Med Phys Fitness (in press)
Cramer JT, Housh TJ, Evetovich TK, Johnson GO, Ebersole KT, Perry SR, Bull AJ (2002) The relationships among peak torque, mean power output, mechanomyography, and electromyography in men and women during maximal, eccentric isokinetic muscle actions. Eur J Appl Physiol 86:226–232
Cramer JT, Housh TJ, Johnson GO, Miller JM, Coburn JW, Beck TW (2004) Acute effects of static stretching on peak torque in women. J Strength Cond Res 18:236–241
Cramer JT, Housh TJ, Weir JP, Johnson GO, Coburn JW, Beck TW (2005) The acute effects of static stretching on peak torque, mean power output, electromyography, and mechanomyography. Eur J Appl Physiol 93:530–539
Cramer JT, Beck TW, Housh TJ, Massey LL, Marek SM, Danglemeier S, Purkayastha S, Culbertson JY, Fitz KA, Egan AD (2007) Acute effects of static stretching on characteristics of the isokinetic angle - torque relationship, surface electromyography, and mechanomyography. J Sports Sci 25:687–698
Evetovich TK, Nauman NJ, Conley DS, Todd JB (2003) Effect of static stretching of the biceps brachii on torque, electromyography, and mechanomyography during concentric isokinetic muscle actions. J Strength Cond Res 17:484–488
Fowles JR, Sale DG, MacDougall JD (2000) Reduced strength after passive stretch of the human plantarflexors. J Appl Physiol 89:1179–1188
Gabriel DA, Boucher JP (1998) Effects of repetitive dynamic contractions upon electromechanical delay. Eur J Appl Physiol Occup Physiol 79:37–40
Grosset JF, Mora I, Lambertz D, Perot C (2005) Age-related changes in twitch properties of plantar flexor muscles in prepubertal children. Pediatr Res 58:966–970
Grosset JF, Piscione J, Lambertz D, Perot C (2009) Paired changes in electromechanical delay and musculo-tendinous stiffness after endurance or plyometric training. Eur J Appl Physiol 105:131–139
Haff GG, Carlock JM, Hartman MJ, Kilgore JL, Kawamori N, Jackson JR, Morris RT, Sands WA, Stone MH (2005) Force–time curve characteristics of dynamic and isometric muscle actions of elite women olympic weightlifters. J Strength Cond Res 19:741–748
Herda TJ, Cramer JT, Ryan ED, McHugh MP, Stout JR (2008a) Acute effects of static versus dynamic stretching on isometric peak torque, electromyography, and mechanomyography of the biceps femoris muscle. J Strength Cond Res 22:809–817
Herda TJ, Ryan ED, Smith AE, Walter AA, Bemben MG, Stout JR, Cramer JT (2008b) Acute effects of passive stretching vs vibration on the neuromuscular function of the plantar flexors. Scand J Med Sci Sports [Epub ahead of print]
Hermens HJ, Frekis B, Merletti R, Stegman D, Blok J, Rau G, Klug CD, Hägg G (1999) SENIAM—European recommendations for surface electromyography. Results of the SENIAM project. Roessingh Research and Development, Enschede
Hopkins JT, Feland JB, Hunter I (2007) A comparison of voluntary and involuntary measures of electromechanical delay. Int J Neurosci 117:597–604
Kawamori N, Rossi SJ, Justice BD, Haff EE, Pistilli EE, O’Bryant HS, Stone MH, Haff GG (2006) Peak force and rate of force development during isometric and dynamic mid-thigh clean pulls performed at various intensities. J Strength Cond Res 20:483–491
Kokkonen J, Nelson AG, Cornwell A (1998) Acute muscle stretching inhibits maximal strength performance. Res Q Exerc Sport 69:411–415
Kubo K, Kanehisa H, Kawakami Y, Fukunaga T (2001) Influence of static stretching on viscoelastic properties of human tendon structures in vivo. J Appl Physiol 90:520–527
Linford CW, Hopkins JT, Schulthies SS, Freland B, Draper DO, Hunter I (2006) Effects of neuromuscular training on the reaction time and electromechanical delay of the peroneus longus muscle. Arch Phys Med Rehabil 87:395–401
Magnusson SP, Simonsen EB, Aagaard P, Kjaer M (1996) Biomechanical responses to repeated stretches in human hamstring muscle in vivo. Am J Sports Med 24:622–628
Marek SM, Cramer JT, Fincher AL, Massey LL, Dangelmaier SM, Purkayastha S, Fitz KA, Culbertson JY (2005) Acute Effects of Static and Proprioceptive Neuromuscular Facilitation Stretching on Muscle Strength and Power Output. J Athl Train 40:94–103
McHugh MP, Nesse M (2008) Effect of stretching on strength loss and pain after eccentric exercise. Med Sci Sports Exerc 40:566–573
Minshull C, Gleeson N, Walters-Edwards M, Eston R, Rees D (2007) Effects of acute fatigue on the volitional and magnetically-evoked electromechanical delay of the knee flexors in males and females. Eur J Appl Physiol 100:469–478
Mirkov DM, Nedeljkovic A, Milanovic S, Jaric S (2004) Muscle strength testing: evaluation of tests of explosive force production. Eur J Appl Physiol 91:147–154
Moritani T (2002) Motor unit and motoneurone excitability during explosive movement. In: Komi PV (ed) Strength and power in sport. Blackwell, London, pp 27–49
Morse CI, Degens H, Seynnes OR, Maganaris CN, Jones DA (2008) The acute effect of stretching on the passive stiffness of the human gastrocnemius muscle tendon unit. J Physiol 586:97–106
Muro M, Nagata A (1985) The effects on electromechanical delay of muscle stretch of the human triceps surae. In: Winter D, Norman R, Wells R, Hayes K, Palta A (eds) Biomechanics IX-A. Human Kinetics, Champaign, pp 86–90
Murphy AJ, Wilson GJ, Pryor JF (1994) Use of the iso-inertial force mass relationship in the prediction of dynamic human performance. Eur J Appl Physiol Occup Physiol 69:250–257
Nelson AG, Kokkonen J (2001) Acute ballistic muscle stretching inhibits maximal strength performance. Res Q Exerc Sport 72:415–419
Nelson AG, Allen JD, Cornwell A, Kokkonen J (2001a) Inhibition of maximal voluntary isometric torque production by acute stretching is joint-angle specific. Res Q Exerc Sport 72:68–70
Nelson AG, Guillory IK, Cornwell C, Kokkonen J (2001b) Inhibition of maximal voluntary isokinetic torque production following stretching is velocity-specific. J Strength Cond Res 15:241–246
Nelson AG, Driscoll NM, Landin DK, Young MA, Schexnayder IC (2005) Acute effects of passive muscle stretching on sprint performance. J Sports Sci 23:449–454
Norman RW, Komi PV (1979) Electromechanical delay in skeletal muscle under normal movement conditions. Acta Physiol Scand 106:241–248
Ogura Y, Miyahara Y, Naito H, Katamoto S, Aoki J (2007) Duration of static stretching influences muscle force production in hamstring muscles. J Strength Cond Res 21:788–792
Power K, Behm D, Cahill F, Carroll M, Young W (2004) An acute bout of static stretching: effects on force and jumping performance. Med Sci Sports Exerc 36:1389–1396
Rosenbaum D, Hennig EM (1995) The influence of stretching and warm-up exercises on Achilles tendon reflex activity. J Sports Sci 13:481–490
Rubini EC, Costa AL, Gomes PS (2007) The effects of stretching on strength performance. Sports Med 37:213–224
Ryan ED, Beck TW, Herda TJ, Hull HR, Hartman MJ, Costa PB, Defreitas JM, Stout JR, Cramer JT (2008a) The time course of musculotendinous stiffness responses following different durations of passive stretching. J Orthop Sports Phys Ther 38:632–639
Ryan ED, Beck TW, Herda TJ, Hull HR, Hartman MJ, Stout JR, Cramer JT (2008b) Do practical durations of stretching alter muscle strength? A dose–response study. Med Sci Sports Exerc 40:1529–1537
Ryan ED, Herda TJ, Costa PB, Defreitas JM, Beck TW, Stout JR, Cramer JT (2009) Passive properties of the muscle–tendon unit: the influence of muscle cross-sectional area. Muscle Nerve 39:227–229
Shrier I (2004) Does stretching improve performance? A systematic and critical review of the literature. Clin J Sport Med 14:267–273
Stone MH, Sands WA, Carlock J, Callan S, Dickie D, Daigle K, Cotton J, Smith SL, Hartman M (2004) The importance of isometric maximum strength and peak rate-of-force development in sprint cycling. J Strength Cond Res 18:878–884
Viitasalo JT, Aura O (1984) Seasonal fluctuations of force production in high jumpers. Can J Appl Sport Sci 9:209–213
Vint PF, McLean SP, Harron GM (2001) Electromechanical delay in isometric actions initiated from nonresting levels. Med Sci Sports Exerc 33:978–983
Weir DE, Tingley J, Elder GC (2005) Acute passive stretching alters the mechanical properties of human plantar flexors and the optimal angle for maximal voluntary contraction. Eur J Appl Physiol 93:614–623
Wilson GJ, Murphy AJ, Pryor JF (1994) Musculotendinous stiffness: its relationship to eccentric, isometric, and concentric performance. J Appl Physiol 76:2714–2719
Winter EM, Brookes FB (1991) Electromechanical response times and muscle elasticity in men and women. Eur J Appl Physiol Occup Physiol 63:124–128
Yamaguchi T, Ishii K (2005) Effects of static stretching for 30 seconds and dynamic stretching on leg extension power. J Strength Cond Res 19:677–683
Zhou S, Lawson DL, Morrison WE, Fairweather I (1995) Electromechanical delay in isometric muscle contractions evoked by voluntary, reflex and electrical stimulation. Eur J Appl Physiol Occup Physiol 70:138–145
Zhou S, McKenna MJ, Lawson DL, Morrison WE, Fairweather I (1996) Effects of fatigue and sprint training on electromechanical delay of knee extensor muscles. Eur J Appl Physiol Occup Physiol 72:410–416
Zhou S, Carey MF, Snow RJ, Lawson DL, Morrison WE (1998) Effects of muscle fatigue and temperature on electromechanical delay. Electromyogr Clin Neurophysiol 38:67–73
Acknowledgments
This study was funded in part by a research grant from the National Strength and Conditioning Association (NSCA) Foundation, Colorado Springs, CO.
This experiment complies with the current laws of the country in which they were performed.
Conflict of interest statement
The authors would like to declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Arnold de Haan.
Rights and permissions
About this article
Cite this article
Costa, P.B., Ryan, E.D., Herda, T.J. et al. Acute effects of passive stretching on the electromechanical delay and evoked twitch properties. Eur J Appl Physiol 108, 301–310 (2010). https://doi.org/10.1007/s00421-009-1214-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-009-1214-3