Abstract
It was already established that exposure to hyperbaric conditions induces vagal-depended bradycardia but field study on autonomic nervous system (ANS) activity during self-contained underwater breathing apparatus (SCUBA) diving is lacking. The aim of the present study was to evaluate ANS modifications during real recreational SCUBA diving using heart rate variability analysis (timedomain, frequency-domain and Poincaré plot) in 10 experienced and volunteers recreational divers. Mean RR, root mean square of successive differences of interval (rMSSD), high frequency of spectral analysis and standard deviation 1 of Poincaré Plot increased (P < 0.05) during dive. Low frequency/high frequency ratio decreased during dive (P < 0.05) but increased after (P < 0.05). Recreational SCUBA diving induced a rise in vagal activity and a decrease in cardiac sympathetic activity. Conversely, sympathetic activity increases (P < 0.05) during the recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-contained underwater breathing apparatus (SCUBA) diving involves important cardio-pulmonary constraints. Laboratory studies have demonstrated that various stimuli in diving could be implicated in these cardiovascular adaptations and particularly in the modulation of autonomic nervous system (ANS) activity. First, it is well established that immersion induces an increase in central blood volume (Gabrielsen 1993; Norsk 1985) due to a redistribution of regional blood flow to the central circulation. It causes an increase in heart volume, stroke volume and cardiac output (Shiraishi et al. 2002; Miwa et al. 1996a; Norsk 1992). These phenomena are accompanied by bradycardia, resulting from vagal activation and a decrease in sympathetic activity (Miwa et al. 1997). Conversely, the cold water induces peripheral vasoconstriction and a rise in intra-thoracic blood volume (Bonde-Petersen et al. 1992) with an increase in sympathetic activity (Mourot et al. 2008). Secondly, both the absolute and partial oxygen pressures increase during SCUBA diving. Such hyperbaric conditions contribute to bradycardia and arteriolar vasoconstriction while the cardiac and stroke volumes decrease in SCUBA diving (Lafay et al. 1997; Neubauer et al. 2001; Molénat et al. 2004) and apnea (Marabotti et al. 2008). Lund et al. (1999, 2000) showed that an increase in parasympathetic activity is associated with a decrease in sympathetic activity in hyperbaric conditions.
Other factors could modulate the magnitude of these adaptations of the ANS. Emotional factors (Ross and Periodtoe 1980; Periodtoe and Sawada 1989), the level of physical training or the degree of diving proficiency could also contribute to cardiac and vascular autonomic functions.
Data concerning ANS responses to real SCUBA diving are only available from one study in a swimming pool (Schipke and Pelzer 2001) and there are little data available from studies in hyperbaric chambers (Lund et al. 1999, 2000). ANS responses could be modified by a number of factors during diving and ANS dysfunction could even be implicated in some diving accidents (Pelliccia et al. 2005, Mitchell et al. 2005). To our knowledge there has been no evaluation of ANS response in healthy volunteers during real SCUBA diving and this evaluation could be used to identify potentially at-risk subjects as suggested by Schipke and Pelzer (2001).
Frequency-domain analysis of heart rate variability (HRV) represents a widely recognized non-invasive method to quantify cardiac autonomic function (Task Force of the European Society of Cardiology, the North American Society of Pacing, Electrophysiology 1996; Akselrod et al. 1981). Use of the Fast Fourier Transform enabled us to obtain the power spectral density for RR interval variability reflecting the overall ANS (total power, Ptot), parasympathetic (high frequency, HF) and sympathetic activity (low frequency/high frequency ratio, LF/HF ratio). Other mathematical methods were also used, such as time-domain (Katona and Jih 1975) and Poincaré plot analysis (Tulppo et al. 1996).
The aim of this study was to assess ANS responses in real recreational SCUBA diving conditions. From previous studies (Schipke and Pelzer 2001), we hypothesized that there would be a dominance in cardiac parasympathetic activity during real SCUBA diving in healthy volunteers.
Methods
Volunteers
Ten adult (one-woman) volunteers took part in this protocol. All were experienced SCUBA divers (227.7 ± 590 dives). The mean age was 27.3 ± 9.7 years, the mean body mass was 73.7 ± 15.7 kg and the mean height was 178.9 ± 5.31 cm. All the subjects were free of any known cardiac abnormalities, and none of them was on any cardioactive medication. All were volunteers and were asked to refrain from taking any form of medication and not to drink any beverages containing alcohol or caffeine during the day of the SCUBA dive. Informed consent was obtained from each subject. We did not interfere in any way with the subject’s usual diving preparations and the advice of a diving instructor.
Material
Measurements were made using a POLAR® recorder (POLAR® S810, Polar Electro, Oulu, Finland). The validity of this device for measurement of heart rate and HRV has already been demonstrated (Radespiel-Tröger et al. 2003). It comprises a belt (with two electrodes) and a watch. The system allows measurement of RR intervals without recording the usual electrocardiographic activity. The sampling rate used was 1,000 Hz. The depth, duration of the dive, and water temperature were recorded with a Digital Depth Gauge (Digital, SCUBAPRO-UWATEC®, Hallwil, Switzerland).
Measurements
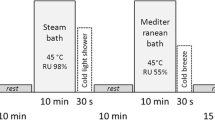
Between January 2006 and March 2007, all the subjects (n = 10) made a recreational dive in the Mediterranean Sea, off the coast of France. The average maximal depth was 19.7 ± 4.1 m, the mean water temperature was 16 ± 3°C and the mean dive duration was 39.5 ± 13.7 min.
The POLAR belts were set while the volunteers put on their neoprene wetsuits (one or two piece wetsuits, 5–7 mm, such as the Pacific suit (SCUBAPRO-UWATEC®, Hallwil, Switzerland) or the Iceberg suit (BEUCHAT® Marseille, France) with hood, gloves and flippers. The POLAR watches were strapped to their right forearm. This system enabled us to measure the RR interval (RRI). Recording began immediately the participants were dressed, i.e., 21.0 ± 5.0 min before the dive and finished 30 minutes after the dive. During each “non-diving” period (which are the periods before and after the dive), the subjects sat quietly on the boat and were asked neither to talk nor to stand up.
During each dive, three periods of 256 beats were chosen for analysis. The first occurred just after submersion (2.2 ± 3.2 min) at the start of the dive (Diving 1: D1), the second was 11.6 ± 4.06 min after submersion (Diving 2: D2) and the third (Diving 3: D3) 27.6 ± 10.6 min after submersion.
All the recordings presented were made during recreational dives. The dive sites were chosen as known to be free of current. However, if it became evident that currents were present, the dive and its subsequent recordings were canceled (one time) as underwater activity would no longer be representative of normal diving conditions. The descent and ascent phases of the dive were carried out by deflation and inflation of stabilizing jackets. For these reasons, we assumed that the workload was constant during the dives.
Data analysis
Polar precision performance 3.0 software was used for the time sampling of the different periods of each dive. MathLab software (Mathworks Inc®, Natick, MA, USA) was used for recognition of ectopic QRS beats or artifacts and a linear interpolation process was applied.
Time- and frequency-domain and geometrical HRV analysis was done using software from the Biomedical Signal Analysis Group Department of Applied Physics, University of Kuopio, Finland (Niskanen et al. 2004). The Fast Fourier Transform enabled us to obtain the power spectral density (Niskanen et al. 2004). It is well known that spontaneous breathing frequency decreases during SCUBA diving (Schipke and Pelzer 2001). Brown and collaborators (1993) demonstrated that breathing parameters strongly influence spectral analysis without altering the level of autonomic traffic: when breathing frequency decreased, the authors noticed a shift in the respiratory peak from the HF to the LF band. The frequency limits were adapted with reference to the well-recognized decrease in breathing frequency during SCUBA diving: total spectral power (Ptot: 0–0.4 Hz), high frequency (HF: 0.1–0.4 Hz) and low frequency (LF: 0.04–0.10 Hz) power spectral density of HRV were calculated as a function of these limits. To assess overall autonomic activity, total power spectral density (Ptot) was used; to assess parasympathetic activity, power spectral density of high frequencies (HF) and normalized high frequency (HFnu: HF/(LF + HF)) were also used and finally, to assess sympathetic activity, the low frequency/high frequency ratio (LF/HF ratio) and normalized low frequency (LFnu: LF/(LF + HF)) were used. The HF peak was determined for each selected time-period.
For time-domain, standard deviation of normal-to-normal intervals (SDNN), standard deviation of the root mean square of successive difference (rMSSD) and mean RR were analyzed. SDNN was chosen as it represents overall ANS and rMSSD is a recognized index of parasympathetic activity (Task Force of the European Society of Cardiology, the North American Society of Pacing, Electrophysiology 1996).
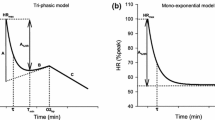
For the Poincaré plot analysis, only the standard deviation 1 (SD1) of the instantaneous beat-to-beat variability (Fig. 1) was used to evaluated parasympathetic activity as standard deviation 2 (SD2: standard deviation of continuous long-term variability) is much more complex to analyze (Tulppo et al. 1996).
During diving, the periods to be analyzed were selected depending on the recording quality, the time lapse between each analysis period, the lack of artifacts and the relative stability of RR trends. Excessive artifact numbers were presented during the recovery period of one subject and this was excluded from the analysis.
Statistical analysis
StatView 5.0 software (SAS Institute Inc® Cary, NC, USA) was used to perform the statistical analyses. Normal Gaussian distribution of the data was verified using z score histograms and then, analyses of variance (ANOVA) of repeated measurements were performed. To determine differences in HRV values between the different diving periods, data were analyzed using the Fisher post hoc test. P value <0.05 was considered significant. Values are presented as means ± SD.
Results
Figure 2 shows (a) RR interval changes and (b) the frequency-domain HRV analysis of basal, Diving 2 and recovery time-periods from one representative subject. Figure 3 shows the diving profile during a real recreational SCUBA dive.
a Original recording of RR intervals from one representative volunteer: each periods basal, diving 1 (D1), diving 2 (D2), diving 3 (D3) and recovery without artifacts and shown steady state. Thick lines represent the beginning and end of the dive and solid vertical lines represent each period of the analysis. b Spectral analysis of RR intervals of basal, diving 2 and recovery periods from the same data. Dotted lines represent frequency peak at very low frequency (0.00–0.04 Hz), at low frequency (0.04–0.10 Hz) and at high frequency (0.10–0.40 Hz) selected by an autoregressive model (in the case of Diving 2, this model does not show any low frequency peaks). The area in gray is the time in which volunteers where immersed in the sea. The first analyzed period D1 could be interpreted as a non-stationary RR interval analysis
Time domain analysis
Analysis of variance for mean RR (P < 0.05) and SDNN (P < 0.05) revealed an increase as shown in Table 1. rMSSD was also altered (P < 0.05) and pairwise comparisons indicated that rMSSD was greater (P < 0.05) in Diving 2 and Diving 3 compared to basal level (Table 1).
Spectral analysis
HF power spectral density increased during Diving 1, Diving 2 and Diving 3 in comparison with basal level (P < 0.05). HF power decreased after diving (Fig. 4b and Table 1) and this decrease was only significant when compared to Diving 2 (P < 0.05). The alteration in the HF peak from 0.139 ± 0.028 Hz at basal level to 0.129 ± 0.011 Hz for Diving 2 was not significant (Table 1).
The LF/HF ratio decreased (P < 0.05): it decreased during both in Diving 1 and Diving 2 in comparison with basal level (Fig. 4c and Table 1). During recovery, the LF/HF ratio increased in comparison with Diving 1, Diving 2 and Diving 3 and with basal level (P < 0.05). A tendency to increase was observed for Ptot (P = 0.07), although this did not reach a level of significance (Fig. 4a, Table 1).
Normalized indexes showed significant changes between recovery and all the diving periods: LFnu increased whereas HFnu decreased (P < 0.05) during recovery compared to Diving 1, 2 and 3 (Table 1).
Poincaré plot analysis
The SD1 increased (P < 0.05) during diving (Table 1). Pairwise analysis revealed an increase in SD1 during Diving 2 and Diving 3 in comparison to basal level (P < 0.05). However, the modifications of SD1 demonstrated by Poincaré plot analysis during Diving 1 did not appear significant.
Discussion
Various methods including spectral-domain analysis (Fast Fourier Transform), time-domain and Poincaré plot analysis have been used to evaluate ANS activity during and after SCUBA diving. We will comment on these, discuss the ANS responses and finally sum up their clinical implications for SCUBA diving.
Time-frequency domain and Poincaré plot analysis
The HF spectral power of RRI increased during all the dive periods whereas rMSSD and SD1 from the Poincaré plot analysis showed an increase only during Diving 2 and 3 as compared to the basal level. Moreover, the HF component of Diving 2 is significantly higher than the one during recovery; this is confirmed by the decrease in HFnu. Taken together with the increase in the RR mean, these results point to an increase in parasympathetic activity and a decrease in sympathetic activity as shown by the decrease in the LF/HF ratio and LFnu during the dive, regardless of the period under consideration.
The respiratory frequency peak, strongly correlated to breathing frequency, was situated within the HF band of the spectral analysis during all the periods of the present protocol (Table 1) as expected (Task Force of the European Society of Cardiology, the North American Society of Pacing, Electrophysiology 1996). Lund et al. (2000) set breathing frequency during their study in a dry hyperbaric chamber, but this is impossible under real diving conditions. The classic HF frequency band limits of Fast Fourier Transform analysis seem unsuitable for studying a real dive: the decrease in ventilatory frequency would lead to a shift of the respiratory frequency peak from the HF to the LF band as was the case in a previous study published by Schipke and Pelzer in 2001. However, the HF limits chosen seem to have been judicious for the evolution of the respiratory frequency peak and the other HRV indexes, e.g., time domain and Poincaré plot results.
Finally, several authors (Brown et al. 1993; Kollai and Mizsei 1990) have shown the importance of both tidal volume and breathing frequency control when evaluating parasympathetic activity using HRV analysis but the control of ventilation parameters is a major difficulty in real diving conditions. Using these slightly modified limits for HRV means that this widely recognized, non-invasive method can be used to quantify cardiac autonomic function during a real dive.
ANS activity in SCUBA diving
The present study shows that all recognized parasympathetic HRV indexes increase and those of sympathetic activity decrease during real recreational SCUBA diving in healthy subjects. Even under recording conditions where the real life factors of stress and emotion are present, parasympathetic activity clearly dominates in these experienced recreational divers. These results corroborate a preceding indoor swimming-pool study (Schipke and Pelzer 2001) as well as hyperbaric chamber experiments (Lund et al. 1999, 2000). Furthermore, sympathetic activity radically increases during the diving recovery period.
The increase in overall ANS activity is less clear: Ptot only showed a tendency to increase after diving (P = 0.07) without reaching significance levels and the SDNN increase during the protocol (P < 0.01) was not shown to be statistically significant using pairwise comparisons.
Several stimuli could play a part in the increase in parasympathetic activity, e.g., water immersion, and exposure to hyperbaric conditions and the cold. Water density induces redistribution of blood volume from peripheral blood flow to central circulation and so central venous pressure increases (Gabrielsen et al. 1993; Norsk et al. 1985). During thermoneutral head-out immersion (Bonde-Petersen et al. 1992), this blood redistribution has also been linked to bradycardia and a decrease in peripheral vascular resistance. ANS responses also seem to be altered as is shown by muscular sympathetic nerve activity (Miwa et al. 1996b), HRV (Miwa et al. 1996a) and systolic blood pressure variability (Miwa et al. 1996a). A possible mechanism could be increased baroreceptor sensitivity, with an ensuing increase in parasympathetic activity (Ueno et al. 2005). Moreover, temperature, in our study between 12 and 20°C, may be an additional factor of blood redistribution because of cold-induced peripheral vasoconstriction (Bonde-Petersen et al. 1992). This phenomenon may also increase the cardiopulmonary and arterial baroreceptor load. Likewise, breathing through a regulator and restrictions on breathing through the nose during SCUBA diving may lead to breathing resistance which could participate in ANS modification.
Temperature sensitive facial receptors seem to be especially sensitive to cold immersion and lead to direct vagal stimulation and subsequent bradycardia (Hayashi et al. 1997; Kinoshita et al. 2006). During SCUBA diving, facial temperature receptors may have contributed to vagal activation. In the present study, the exposure time to the cold water may have contributed to the increase in parasympathetic activity, the decrease in cardiac sympathetic activity and finally, to an increase in mean RR (Srámek et al. 2000).
Previous hyperbaric chamber experiments have demonstrated an enhancement of parasympathetic activity, this autonomic disequilibrium appearing independently of modifications in respiratory frequency (Lund et al. 2000). In our study, hyperbaric conditions up to 3 ATA contributed to these alterations in HRV.
SCUBA diving recovery
Without being significant compared to basal level and with a large scattering, the recovery period shows high Ptot and the SDNN values reach a level equivalent to that observed during diving (Figs. 3a, 4a). Overall, ANS activity shows a continuously high level after diving while a significant decrease of parasympathetic indexes, particularly HF components, is observed compared to the diving period. We noticed that cardiac sympathetic activity radically increased. Hirayanagi et al. 2003 showed that during a 7-day recovery period, consecutive to severe hyperbaric exposure (30 days with a pressure of up to 41 ATA), cardiac sympathetic activity was associated with an increase in plasmatic catecholamines. This long-term hyperbaric exhibition is far more important than that encountered in recreational SCUBA diving, but this result suggests altered cardiac ANS activity after SCUBA diving, indicative of sympathetic activity. Other results have shown that after immersion in cold water, there is a considerable increase in the concentration of plasma norepinephrine (Johnson et al. 1977).
Limitations
Our field study did not allow us to evaluate separately the role of depth or cold for each analyzed time-period of the dive. This limitation prevents us from understanding the role of different stimuli in parasympathetic activity supremacy; further distinction among these factors was not possible. Activities such as swimming underwater were not checked although such underwater activities could modify heart balance. However, in these recreational dives, workload was minimal.
Furthermore, in the Diving periods, the hyperbaric exposure was not stationary. This could have affected the spectral results, but the time-domain and Poincaré plot analysis corroborate the spectral results for these periods.
Finally, the increase in the LF/HF ratio while on the boat could have contributed to the significant difference between the dive, recovery and basal period. However, Portier and Guézennec 2007 showed that an increase in LF/HF ratio is significant only when the subject is standing. Seating the subjects during the basal and recovery periods attenuated this limitation.
Clinical implications
The abrupt increase in parasympathetic activity suggests a potential risk of vagally mediated syncope (Lafay 2006; Pelliccia et al. 2005; Mitchell et al. 2005) in recreational SCUBA diving as for instance in free diving (Lemaitre et al. 2005). With the same clinical perceptive, Eckenhoff and Knight (1984) described asymptomatic supraventricular arrhythmia in 10% of 81 healthy subjects during dives, certainly related to an increase in parasympathetic activity. Moreover, sympathetic activity could play a major role in cardiac arrhythmia during recovery and this increase in sympathetic activity during diving deserves further investigation. HRV analysis could be used to prevent such incidents by screening the diver population as suggested by Schipke and Pelzer (2001). Studies including larger populations should also be performed to assess the potential usefulness of such screening.
Conclusions
Time-domain, frequency-domain analysis, and Poincaré plot analysis of HRV highlight a dominance in parasympathetic activity during real recreational SCUBA diving associated with an increase in sympathetic activity during the recovery period. These autonomic responses could be the consequence of numerous stimuli such as mechanoreceptors sensitive to pulmonary distension, cold sensitive receptors and hemodynamic changes induced by hyperbaric exposure and immersion. The clinical implications of such findings in vagally mediated syncope or cardiac arrhythmia should be kept in mind.
References
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ (1981) Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 213(4504):220–222. doi:10.1126/science.6166045
Bonde-Petersen F, Schultz-Pedersen L, Dragsted N (1992) Peripheral and central blood flow in man during cold, thermoneutral, and hot water immersion. Aviat Space Environ Med 63(5):346–350
Brown TE, Beightol LA, Koh J, Eckberg DL (1993) Important influence of respiration on human R-R interval power spectra is largely ignored. J Appl Physiol 75(5):2310–2317
Eckenhoff RG, Knight DR (1984) Cardiac arrhythmias heart rate changes in prolonged hyperbaric air exposures. Undersea Biomed Res 11(4):355–367
Gabrielsen A, Johansen LB, Norsk P (1993) Central cardiovascular pressures during graded water immersion in humans. J Appl Physiol 75(2):581–585
Hayashi N, Ishihara M, Tanaka A, Osumi T, Yoshida T (1997) Face immersion increases vagal activity as assessed by heart rate variability. Eur J Appl Physiol Occup Physiol 76(5):394–399. doi:10.1007/s004210050267
Hirayanagi K, Nakabayashi K, Okonogi K, Ohiwa H (2003) Autonomic nervous activity and stress hormones induced by hyperbaric saturation diving. Undersea Hyperb Med 30(1):47–55
Johnson DG, Hayward JS, Jacobs TP, Collis ML, Eckerson JD, Williams RH (1977) Plasma norepinephrine responses of man in cold water. J Appl Physiol 43(2):216–220
Katona PG, Jih F (1975) Respiratory sinus arrhythmia: noninvasive measure of parasympathetic cardiac control. J Appl Physiol 39(5):801–805
Kinoshita T, Nagata S, Baba R, Kohmoto T, Iwagaki S (2006) Cold-water face immersion per se elicits cardiac parasympathetic activity. Circ J 70(6):773–776. doi:10.1253/circj.70.773
Kollai M, Mizsei G (1990) Respiratory sinus arrhythmia is a limited measure of cardiac parasympathetic control in man. J Physiol 424:329–342
Lafay V (2006) The heart and undersea diving. Arch Mal Coeur Vaiss 99(11):1115–1119
Lafay V, Boussuges A, Ambrosi P, Barthelemy P, Frances Y, Gardette B, Jammes Y (1997) Doppler-echocardiography study of cardiac function during a 36 atm (3, 650 kPa) human dive. Undersea Hyperb Med 24(2):67–71
Lemaitre F, Bernier F, Petit I, Renard N, Gardette B, Joulia F (2005) Heart rate responses during a breath-holding competition in well-trained divers. Int J Sports Med 26(6):409–413. doi:10.1055/s-2004-821159
Lund VE, Kentala E, Scheinin H, Klossner J, Helenius H, Sariola-Heinonen K, Jalonen J (1999) Heart rate variability in healthy volunteers during normobaric and hyperbaric hyperoxia. Acta Physiol Scand 167(1):29–35. doi:10.1046/j.1365-201x.1999.00581.x
Lund V, Kentala E, Scheinin H, Klossner J, Sariola-Heinonen K, Jalonen J (2000) Hyperbaric oxygen increases parasympathetic activity in professional divers. Acta Physiol Scand 170(1):39–44. doi:10.1046/j.1365-201x.2000.00761.x
Marabotti C, Belardinelli A, L’Abbate A, Scalzini A, Chiesa F, Cialoni D, Passera M, Bedini R (2008) Cardiac function during breath-hold diving in humans: an echocardiographic study. Undersea Hyperb Med 35(2):83–90
Mitchell JH, Haskell W, Snell P, Van Camp SP (2005) Task Force 8: classification of sports. J Am Coll Cardiol 45:1364–1367. doi:10.1016/j.jacc.2005.02.015
Miwa C, Sugiyama Y, Mano T, Iwase S, Matsukawa T (1996a) Spectral characteristics of heart rate and blood pressure variabilities during head-out water immersion. Environ Med 40(1):91–94
Miwa C, Mano T, Saito M, Iwase S, Matsukawa T, Sugiyama Y, Koga K (1996b) Ageing reduces sympatho-suppressive response to head-out water immersion in humans. Acta Physiol Scand 158(1):15–20. doi:10.1046/j.1365-201X.1996.527289000.x
Miwa C, Sugiyama Y, Mano T, Iwase S, Matsukawa T (1997) Sympatho-vagal responses in humans to thermoneutral head-out water immersion. Aviat Space Environ Med 68(12):1109–1114
Molénat F, Boussuges A, Grandfond A, Rostain JC, Sainty JM, Robinet C, Galland F, Meliet JL (2004) Haemodynamic effects of hyperbaric hyperoxia in healthy volunteers: an echocardiographic and Doppler study. Clin Sci (Lond) 106(4):389–395. doi:10.1042/CS20030293
Mourot L, Bouhaddi M, Gandelin E, Cappelle S, Dumoulin G, Wolf JP, Rouillon JD, Regnard J (2008) Cardiovascular autonomic control during short-term thermoneutral and cool head-out immersion. Aviat Space Environ Med 79(1):14–20. doi:10.3357/ASEM.2147.2008
Neubauer B, Tetzlaff K, Staschen CM, Bettinghausen E (2001) Cardiac output changes during hyperbaric hyperoxia. Int Arch Occup Environ Health 74(2):119–122. doi:10.1007/s004200000201
Niskanen JP, Tarvainen MP, Ranta-Aho PO, Karjalainen PA (2004) Software for advanced HRV analysis. Comput Methods Programs Biomed 76(1):73–81. doi:10.1016/j.cmpb.2004.03.004
Norsk P (1992) Gravitational stress and volume regulation. Clin Physiol 12(5):505–526. doi:10.1111/j.1475-097X.1992.tb00355.x
Norsk P, Bonde-Petersen F, Warberg J (1985) Central venous pressure and plasma arginine vasopressin during water immersion in man. Eur J Appl Physiol Occup Physiol 54(1):71–78. doi:10.1007/BF00426302
Pelliccia A, Fagard R, Bjornstad HH et al (2005) Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J 26:1422–1445. doi:10.1093/eurheartj/ehi325
Periodtoe A, Sawada Y (1989) Assessment of baroreceptor reflex function during mental stress and relaxation. Psychophysiology 26(2):140–147. doi:10.1111/j.1469-8986.1989.tb03145.x
Portier H, Guézennec CY (2007) Study of heart rate variability during offshore race with sleep deprivation. Sci Sports 22:163–165. doi:10.1016/j.scispo.2007.05.002
Radespiel-Tröger M, Rauh R, Mahlke C, Gottschalk T, Mück-Weymann M (2003) Agreement of two different methods for measurement of heart rate variability. Clin Auton Res 13(2):99–102. doi:10.1007/s10286-003-0085-7
Ross A, Periodtoe A (1980) Attenuation of the diving reflex in man by mental stimulation. J Physiol 302:387–393
Schipke JD, Pelzer M (2001) Effect of immersion, submersion, and scuba diving on heart rate variability. Br J Sports Med 35(3):174–180. doi:10.1136/bjsm.35.3.174
Shiraishi M, Schou M, Gybel M, Christensen NJ, Norsk P (2002) Comparison of acute cardiovascular responses to water immersion and head-down tilt in humans. J Appl Physiol 92(1):264–268
Srámek P, Simecková M, Janský L, Savlíková J, Vybíral S (2000) Human physiological responses to immersion into water of different temperatures. Eur J Appl Physiol 81(5):436–442. doi:10.1007/s004210050065
Task Force of the European Society of Cardiology, the North American Society of Pacing, Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93(5):1043–1065
Tulppo MP, Mäkikallio TH, Takala TE, Seppänen T, Huikuri HV (1996) Quantitative beat-to-beat analysis of heart rate dynamics during exercise. Am J Physiol 271(1 Pt 2):H244–H252
Ueno LM, Miyachi M, Matsui T, Takahashi K, Yamazaki K, Hayashi K, Onodera S, Moritani T (2005) Effect of aging on carotid artery stiffness and baroreflex sensitivity during head-out water immersion in man. Braz J Med Biol Res 38(4):629–637. doi:10.1590/S0100-879X2005000400018
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chouchou, F., Pichot, V., Garet, M. et al. Dominance in cardiac parasympathetic activity during real recreational SCUBA diving. Eur J Appl Physiol 106, 345–352 (2009). https://doi.org/10.1007/s00421-009-1010-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-009-1010-0