Abstract
The purpose of this study was to observe the effect of high intermittent exercise training on children’s heart rate variability (HRV). Thirty-eight children (age 9.6 ± 1.2 years) were divided into an intermittent (IT, n = 22) and a control group (CON, n = 16). At baseline and after a 7-week training period, HRV parameters, peak oxygen consumption \( (\dot{V}{\text{O}}_{{2{\text{peak}}}} ) \) and maximal aerobic velocity (MAV) were assessed. Training consisted of three 30-min sessions composed by short maximal and supramaximal runs at velocities ranging from 100 up to 190% of MAV. HRV was computed in time and frequency domains. Training resulted in a significant increase in MAV and \( \dot{V}{\text{O}}_{{2{\text{peak}}}} \) in IT (P < 0.05) only without any significant change in HRV parameters for the two groups. Thus, 7 weeks of high intermittent exercise training allows to improve aerobic fitness. However, this modality of training was not sufficient enough to underline a possible effect on the heart rate autonomic regulation in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The measurement of the heart rate variability (HRV) is a useful tool to quantifying the activity of the autonomic nervous system on the cardiovascular function in adults as well as in children. In adults a decrease in HRV is often associated with both physiological (Molgaard et al. 1991) and psychological (Dishman et al. 2000) disorders. On the contrary a large HRV is a favourable prognostic in the decrease of disorder incidence for apparently healthy men (Molgaard et al. 1991) or in the advancement of disease for patients (Hayano et al. 1991). Likewise, low HRV in childhood is associated with several paediatric issues such as congenital heart diseases (Massin and von Bernuth 1998), obesity (Gutin et al. 2000) or diabetes (Javorka et al. 2005). Moreover, the decrease of the HRV is coupled with the worsening of the disease (Gutin et al. 2000; Javorka et al. 2005).
Adapted endurance training is widely accepted as non-pharmacological means to increase HRV and autonomic nervous control on heart (Billman 2002). In adults, cardiovascular autonomic adaptations increase with physical fitness improvement and particularly with the peak oxygen consumption \( (\dot{V}{\text{O}}_{{2{\text{peak}}}} ) \) (Iwasaki et al. 2003). However, a sufficient quantity of training seems necessary to induced both aerobic and cardiovascular autonomic adaptations, with exercise intensity playing a major role in this phenomenon as the majority of studies that highlighted an improvement in HRV used moderate or high intensity exercises (Aubert et al. 2003).
In children, autonomic nervous activity is dependant of the maturation state with in particular a greater vagal tone than adults (Lenard et al. 2004; Silvetti et al. 2001). These differences are not clear and may be related to both mechanical and neural alterations with age (Lenard et al. 2004) that could lead to different autonomic nervous adaptations after an aerobic training. Nevertheless, the prepubescent children studies on autonomic adaptation induced by exercise training are poor and lead to inconsistent conclusions (Franks and Boutcher 2003; Mandigout et al. 2002; Nagai et al. 2004; Triposkiadis et al. 2002; Vinet et al. 2005). In 1 year longitudinal study, Nagai et al. (2004) reported minor change in HRV parameters after submaximal exercise training in children with normal HRV whereas Mandigout et al. (2002) observed an enhancement of the majority of HRV components after 13 weeks of intermittent and continuous exercise training with an intensity higher than Nagai’s study (Nagai et al. 2004).
Thus in children, as in adults, the used of high intensity training could affect the cardiac adaptation and probably the heart rate regulation. One way to elicit or maintain different physiological parameters at a high level of activation is the used of high-intensity short intermittent exercise (Dupont et al. 2003). Besides, this type of training is also efficient as submaximal continuous training to induce beneficial adaptations in healthy (Helgerud et al. 2007), pathological (Wisloff et al. 2007) or paediatrics (Baquet et al. 2003) populations. Moreover in the paediatric population, this type of training might be an alternative to continuous exercises as it is linked to children’s spontaneous activity (Baquet et al. 2002). However to our knowledge, there are no available data dealing with the effect of training intensity on the autonomic nervous system adaptations at the heart level in children.
Therefore, the aim of this study was design to investigate the effects of high-intensity short intermittent training, on the autonomic cardiovascular control in prepubescent children, as measured by HRV.
Methods
Subjects
Fifty-two healthy children with no clinical or historical evidence of cardiovascular disease or hypertension participated in this study. All of them were nonobese and were Tanner stage 1 (Tanner 1962) before and after the training period (boys: pubic hair and genital organ development; girls: pubic hair and breast development). If children exhibited any overt signs of pubertal onset, they were excluded from taking part in the study. None of them was taking medication that would affect aerobic performance or autonomic nervous system. They were recruited from two different primary schools, selected from the same community environment. All of the children were submitted to a non-inclusion protocol before the start of the study. This consisted of an information session about the nature, the potential risks involved, the inclusion and non inclusion criteria and the benefits of the study. Children and their parents gave a written informed consent to participate in the study. The protocol has been reviewed and approved by the local Ethics Committee before the start of the study.
Experimental design
Subjects were randomly assigned to one of the two following groups: intermittent training (IT, n = 26; 15 boys and 11 girls), and control (CON, n = 26; 14 boys and 12 girls). During the protocol, 14 children were excluded for the study for different reasons. The main causes were a low grade heart rate recording or children that failed to reach criteria to confirm that test was maximal. At the end of the protocol, it remained respectively in, IT and CON: 12 boys and 10 girls; 7 boys and 9 girls. Their characteristics are described in Table 1. They performed an autonomic test and a graded running test before and after a 7 weeks training period with three 30-min sessions each week.
Maximal continuous graded exercise test
The graded test was performed on a motorized treadmill (Pulsar 4.0, HP-Cosmos, Nussdorf, Germany) with a slope set at 0°. Initial velocity was set at 6 km h−1 and was increased by steps of 0.5 km h−1 every minute until exhaustion. Strong verbal encouragements were given throughout the test. Oxygen uptake \( (\dot{V}{\text{O}}_{2} ), \) minute ventilation \( (\dot{V}{\text{E),}} \) and carbon dioxide production \( (\dot{V}{\text{CO}}_{2} ) \) were determined continuously using an automated portable cardiopulmonary exercise system (Cosmed, K4B2, Rome, Italy). Before each test, the O2 and CO2 analysis systems were calibrated using ambient air and a gas of know O2 (16%) and CO2 (5%) concentrations. The calibration of the turbine flowmeter of the K4B2 was performed using a 3 syringe (Quinton Instruments, Seattle, WA, USA) before its installation on the mask allowing gas collection. Heart rate was monitored every 5 s during the test with a heart rate monitor (S810, Polar Electo Oy, Kempele, Finland).
Autonomic and cardiovascular testing
Children entered a quiet laboratory room, installed in the school’s dormitory, with constant temperature (20–23°C) and dimmed light between 8:30 and 11:30 a.m. They rested comfortably for 10 min in a supine position before a 5-min supine recording. No attempt was made to control breathing frequency or tidal volume. intervals R–R were measured continuously using a heart rate monitor (S810, Polar Electo Oy, Kempele, Finland) with a sampling frequency of 1000 Hz from the ECG signal providing an accuracy of 1 ms for each intervals (Ruha et al. 1997). This kind of device has been previously validated to assess R–R interval both in adults (Kingsley et al. 2005; Gamelin et al. 2006) and in children (Gamelin et al. 2008). Even the heart rate monitor do not allow to check the QRS complex, the measurement error of this device is largely acceptable when compared with the different effect sizes (ESs) reported in a meta-analysis by Sandercock et al. (2005) for HRV parameters after training in sedentary men.
Training
During 7 weeks, children of IT groups followed three 30-min sessions per week. Theses trainings were built according to intermittent modality found in the paediatrics literature and to fit into the scholar schedule. The training intensity was determined for each child based on his own maximal aerobic velocity (MAV). The sessions were composed of short intermittent runs with exercise/recovery sequences lasting 5/15, 10/10, 15/10, 20/20 and 30/30 s. Intensities were set from 100 up to 190% of MAV (Table 2). Only the two-first sessions consisted in continuous runs. Each session was carefully supervised by a physical education teacher.
Data analysis
Determination of peak oxygen uptake \( \dot{V}{\text{O}}_{{2{\text{peak}}}} \) and maximal aerobic velocity
Cardiopulmonary parameters were averaged on 5 s periods during the maximal continuous graded exercise test. Peak \( \dot{V}{\text{O}}_{2} \) was determined as the mean of the two consecutive highest values. \( \dot{V}{\text{O}}_{2} \) was accepted as maximal index when three of the following criteria were met: a levelling off of \( \dot{V}{\text{O}}_{2} \) despite a further increase in velocity, a final heart rate above 195 beat per minute, a respiratory exchange ration (RER) >1, and a visible exhaustion (Berthoin et al. 2006).
The velocity of the last completed stage was considered as the MAV (i.e. the minimal velocity eliciting \( \dot{V}{\text{O}}_{{2{\text{peak}}}} \)during an incremental test (Berthoin et al. 1999).
Analysis of heart rate variability:
Raw R–R intervals were edited so that artefacts and non-sinus beats could be replaced by interpolation from adjacent normal R–R intervals. The signal was then considered to be normal, and to provide normal-to-normal (N–N) intervals. HRV was computed in the time and frequency domains, but also quantitatively from the Poincaré plot analysis.
Time domain analysis:
A segment of 256 s was selected within the 300 s of the supine recording. Mean N–N interval, the standard deviation of all N–N intervals (SDNN), root mean square of differences of successive N–N intervals (RMSSD) and proportion of differences between adjacent N–N intervals of more than 50 ms (pNN50) were computed.
Frequency domain analysis:
The same segments of 256 s were resampled at 2 Hz and detrended for subsequent analysis. Spectral analysis was performed with a fast Fourier transform (FFT) to quantify the power spectral density of the low frequency (LF; 0.04–0.15 Hz) and the high frequency (HF; 0.15–0.40 Hz) bands. Additional calculations included LF + HF, LF and HF expressed in normalized unit, which represent the relative value of each power component in proportion to the total power minus the power spectral density of very low frequency (VLF; ≤0.04 Hz) and the ratio LF/HF according the Task Force recommendation for short term recordings (Task 1996).
Quantitative beat-to-beat analysis:
The Poincaré plot is a scattergram in which each N–N interval is plotted as a function of the previous one. The Poincaré plot provides both a qualitative and a quantitative analysis of HRV. The shape of the plot can be used to classify the signal into one of various classes (Tulppo et al. 1996; Mourot et al. 2004), but also to fit an ellipse, which enables to quantify the parameters SD1 and SD2. SD1 represents the dispersion of the points perpendicular to the line of identity, and it is thought to be an index of the instantaneous beat-to-beat variability of the data. SD2 represents the dispersion of the points along the line of identity, and is supposed to represents the slow variability of heart rate (Tulppo et al. 1996; Brennan et al. 2001).
All analysis were perform with HRV analysis Software v1.1 (Biosignal Laboratory, University of Kuopio, Finland).
Statistical analysis
Standard statistical methods were used for the calculation of means and standard deviations. Normal Gaussian distribution of the data was verified by the Shapiro–Wilk’s test, and homoscedasctivity by a modified Levene test. A logarithmic transformation was performed before the analysis when data were skewed or exhibited heteroscedasticity. A two-way analysis of variance (group by time) was used to evaluate the effect of training on HRV and other relevant parameters. The compound symmetry, or sphericity, was checked by the Mauchley test. When the assumption of sphericity was not met, the significance of F-ratios was adjusted according to the Greenhouse–Geisser’s procedure when the epsilon correction factor was <0.75, or according to the Huyn–Feld’s procedure when the epsilon correction factor was >0.75. Multiple comparisons were made with the Bonferroni post-hoc test. The magnitude of the difference was assessed by the adjusted effect size (aES). The ES (Eq. 1) and adjusted ESa (Eq. 2) formula is listed just below:
where b before, a after, m group mean, SD standard deviation, n group subject size, r correlation coefficient between before and after data.
The scale proposed by Cohen (1988) was used for interpretation. The magnitude of the difference was considered either small (0.2), moderate (0.5), or large (0.8). Pearson product moment correlation was used to evaluate the association between the baseline status of body mass index (BMI), \( \dot{V}{\text{O}}_{{2{\text{peak}}}} , \) training response (delta \( \dot{V}{\text{O}}_{{2{\text{peak}}}} \) and delta MAV), and different HRV parameters. Statistical significance was set at P = 0.05 level for all analysis. All calculations were made with Statistica 6.0 (Statsoft, Tulsa, USA).
Results
Anthropometric characteristics, MAV and maximal heart rate (HRmax) measured before and after the training period are reported in Table 1. No significant group difference appeared at baseline for all parameters.
A large and significant increase was found for IT in \( \dot{V}{\text{O}}_{{2{\text{peak}}}} \) (P < 0.05, aES = 1.8) and MAV (P < 0.05, aES = 2.8), while it remained unchanged for CON (P > 0.05).
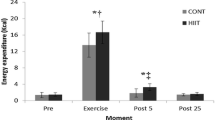
HRV parameters are reported in Table 3. No significant difference was found for time domain, frequency domain or quantitative parameters (P > 0.05), whatever the group (experimental or control). The magnitude of the difference (aES) of relevant parameters is shown in Fig. 1.
There was no association between any of the parameters measured in this study (P > 0.05).
Discussion
The primary finding from the present study was the non significant effect of 7 weeks of high intensity intermittent exercise training programs on the autonomic cardiovascular control of prepubescent children, as measured by HRV, despite a large increase in aerobic fitness.
Given the high interindividual variability of HRV in children (Winsley et al. 2003), great care was taken to standardize measurement conditions. The tests were realized at the same time of the day to avoid circadian variations of HRV parameters (Otsuka et al. 1997). Environmental factors known to influence HRV such as temperature, noise or strong luminosity were controlled during each test. Moreover, recommendations for the last 24 h were given to the parents, where children were asked to abstain from consuming caffeinated beverages and to refrain from excessive physical activity. All together, these precautions should have increased the signal-to-noise ratio, thus contributing to an improved confidence in the data.
The absences of training-induced modifications of HRV are not in accordance with Nagai et al. (2004), who reported an increase in LF without difference in total and HF power spectral density in healthy children with normally initial HRV values after 12 months of moderate continuous training. In the same way, Mandigout et al. (2002) observed an increase in HRV without alteration in autonomic balance after an intense combined (intermittent and continuous exercises) endurance training during 13 weeks.
In these studies, training load (i.e. intensity, duration and frequency of training) may account for this discrepancy. Aubert et al. (2003), Earnest et al. (2008) already highlighted the fact that training intensity may be an essential factor to take into account to involve autonomic adaptations. Although heart rate suffers some limitations to quantify training intensity during near maximal or maximal aerobic exercises (Achten and Jeukendrup 2003), data in our study (unpublished data) were close to or sometimes higher than the 80–90% of maximal heart rate reported by Mandigout et al. (2002). Since training frequency was similar to Mandigout et al. (2002) study (i.e. three sessions per week), the single difference with this work which could explain HRV differences between studies was the training duration. Seven weeks may be too short to involve significant HRV modifications. Although this point has never been studied specifically with prepubescent children, several adult data suggest it should not be the case. In fact, Lee et al. (2003) reported an increase in vagal modulation of heart rate after only eight training sessions performed over 2 weeks in young men. Moreover, Iwasaki et al. (2003) showed that the majority of the autonomic response was achieved after 12 weeks of moderate training in adults. These results suggest that significant adaptations should have been observed after 7 weeks of intense training in healthy adults. Nevertheless these adaptations seem to be also age-dependent as it was suggested by the studies of Earnest et al. (2008) and Verheyden et al. (2006) in older people. As for elderly, children could be less sensitive to training adaptations. In our study, the children maturation could restrain the autonomic adaptations induced by the training as observed for maximal oxygen consumption (Baquet et al. 2003).
An other explanation of the lack of significant result concerns the training load that plays a key factor to induce autonomic adaptations. High training period can lead to an overload and an accumulation of fatigue. In adults there is either no change in autonomic activity (Pichot et al. 2002) or a shift of parasympathetic to sympathetic activity (Iellamo et al. 2002; Portier et al. 2001). In our study all intensities prescribed were maximal or supramaximal and could lead the children to a fatigue state. In this way, the fatigue did not allow to observe the beneficial effect of training on HRV parameters. This is in accordance with Vinet et al. (2005) who found no significant difference between highly trained and sedentary children in HRV. Nevertheless, to the best of our knowledge, no longitudinal study investigated the overreaching on heart rate variability in children. Thus, it seems that an optimal intensity have to be prescribed to induce favourable autonomic adaptation without fatigue.
Nevertheless, it is important to underline that the HRV measurement is a non invasive tool to estimate the activity of the autonomic nervous system and suffers from several limitations. It is necessary to keep in mind that variation in heart rate is not only due to the autonomic nervous system tone and is the result of some mechanisms as for example the baroreflex (Cevese et al. 2001) or the respiration (Rentero et al. 2002). Thus, some cautions should be taken during the result interpretation and the use of other indirect measures as the heart rate post-exercise could bring additional interesting information.
The aim of this study was to observe the effect of 7 weeks of supramaximal intermittent exercise training on the autonomic cardiovascular control of prepubescent children, as measured by HRV. The very large increase in MAV was not accompanied by significant autonomic gains. Additional data with longer training and different intensities are needed to confirm the effect of training intensity on HRV and the autonomic nervous system sensibility of children to physical training.
References
Achten J, Jeukendrup AE (2003) Heart rate monitoring: applications and limitations. Sports Med 33:517–538. doi:10.2165/00007256-200333070-00004
Aubert AE, Seps B, Beckers F (2003) Heart rate variability in athletes. Sports Med 33:889–919. doi:10.2165/00007256-200333120-00003
Baquet G, Berthoin S, Dupont G, Blondel N, Fabre C, van Praagh E (2002) Effects of high intensity intermittent training on peak VO(2) in prepubertal children. Int J Sports Med 23:439–444. doi:10.1055/s-2002-33742
Baquet G, van Praagh E, Berthoin S (2003) Endurance training and aerobic fitness in young people. Sports Med 33:1127–1143. doi:10.2165/00007256-200333150-00004
Berthoin S, Baquet G, Rabita J, Blondel N, Lensel-Corbeil G, Gerbeaux M (1999) Validity of the Universite de Montreal Track Test to assess the velocity associated with peak oxygen uptake for adolescents. J Sports Med Phys Fitness 39:107–112
Berthoin S, Baquet G, Dupont G, Van Praagh E (2006) Critical velocity during continuous and intermittent exercises in children. Eur J Appl Physiol 98:132–138. doi:10.1007/s00421-006-0253-2
Billman GE (2002) Aerobic exercise conditioning: a nonpharmacological antiarrhythmic intervention. J Appl Physiol 92:446–454
Brennan M, Palaniswami M, Kamen P (2001) Do existing measures of Poincare plot geometry reflect nonlinear features of heart rate variability? IEEE Trans Biomed Eng 48:1342–1347. doi:10.1109/10.959330
Cevese A, Gulli G, Polati E, Gottin L, Grasso R (2001) Baroreflex and oscillation of heart period at 0.1 Hz studied by alpha-blockade and cross-spectral analysis in healthy humans. J Physiol 531:235–244. doi:10.1111/j.1469-7793.2001.0235j.x
Cohen J (1988) Statistical power analysis for the behavioral sciences. Hillsdale, New Jersey
Dishman RK, Nakamura Y, Garcia ME, Thompson RW, Dunn AL, Blair SN (2000) Heart rate variability, trait anxiety, and perceived stress among physically fit men and women. Int J Psychophysiol 37:121–133. doi:10.1016/S0167-8760(00)00085-4
Dupont G, Blondel N, Berthoin S (2003) Time spent at VO2max: a methodological issue. Int J Sports Med 24:291–297. doi:10.1055/s-2003-39503
Earnest CP, Lavie CJ, Blair SN, Church TS (2008) Heart rate variability characteristics in sedentary postmenopausal women following six months of exercise training: the DREW study. PLoS ONE 3:e2288. doi:10.1371/journal.pone.0002288
Franks PW, Boutcher SH (2003) Cardiovascular response of trained preadolescent boys to mental challenge. Med Sci Sports Exerc 35:1429–1435. doi:10.1249/01.MSS.0000078935.78895.8E
Gamelin FX, Berthoin S, Bosquet L (2006) Validity of the polar S810 heart rate monitor to measure R–R intervals at rest. Med Sci Sports Exerc 38:887–893. doi:10.1249/01.mss.0000218135.79476.9c
Gamelin FX, Baquet G, Berthoin S, Bosquet L (2008) Validity of the polar S810 to measure R–R intervals in children. Int J Sports Med 29:134–138. doi:10.1055/s-2007-964995
Gutin B, Barbeau P, Litaker MS, Ferguson M, Owens S (2000) Heart rate variability in obese children: relations to total body and visceral adiposity, and changes with physical training and detraining. Obes Res 8:12–19. doi:10.1038/oby.2000.3
Hayano J, Yamada A, Mukai S, Sakakibara Y, Yamada M, Ohte N, Hashimoto T, Fujinami T, Takata K (1991) Severity of coronary atherosclerosis correlates with the respiratory component of heart rate variability. Am Heart J 121:1070–1079. doi:10.1016/0002-8703(91)90664-4
Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, Simonsen T, Helgesen C, Hjorth N, Bach R, Hoff J (2007) Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc 39:665–671. doi:10.1249/mss.0b013e3180304570
Iellamo F, Legramante JM, Pigozzi F, Spataro A, Norbiato G, Lucini D, Pagani M (2002) Conversion from vagal to sympathetic predominance with strenuous training in high-performance world class athletes. Circulation 105:2719–2724. doi:10.1161/01.CIR.0000018124.01299.AE
Iwasaki K, Zhang R, Zuckerman JH, Levine BD (2003) Dose-response relationship of the cardiovascular adaptation to endurance training in healthy adults: how much training for what benefit? J Appl Physiol 95:1575–1583
Javorka M, Javorkova J, Tonhajzerova I, Calkovska A, Javorka K (2005) Heart rate variability in young patients with diabetes mellitus and healthy subjects explored by Poincare and sequence plots. Clin Physiol Funct Imaging 25:119–127. doi:10.1111/j.1475-097X.2004.00601.x
Kingsley M, Lewis MJ, Marson RE (2005) Comparison of polar 810 s and an ambulatory ECG system for R–R interval measurement during progressive exercise. Int J Sports Med 26:39–44. doi:10.1055/s-2004-817878
Lee CM, Wood RH, Welsch MA (2003) Influence of short-term endurance exercise training on heart rate variability. Med Sci Sports Exerc 35:961–969. doi:10.1249/01.MSS.0000069410.56710.DA
Lenard Z, Studinger P, Mersich B, Kocsis L, Kollai M (2004) Maturation of cardiovagal autonomic function from childhood to young adult age. Circulation 110:2307–2312. doi:10.1161/01.CIR.0000145157.07881.A3
Mandigout S, Melin A, Fauchier L, N’Guyen LD, Courteix D, Obert P (2002) Physical training increases heart rate variability in healthy prepubertal children. Eur J Clin Invest 32:479–487. doi:10.1046/j.1365-2362.2002.01017.x
Massin M, von Bernuth G (1998) Clinical and haemodynamic correlates of heart rate variability in children with congenital heart disease. Eur J Pediatr 157:967–971. doi:10.1007/s004310050979
Molgaard H, Sorensen KE, Bjerregaard P (1991) Attenuated 24-h heart rate variability in apparently healthy subjects, subsequently suffering sudden cardiac death. Clin Auton Res 1:233–237. doi:10.1007/BF01824992
Mourot L, Bouhaddi M, Perrey S, Rouillon JD, Regnard J (2004) Quantitative Poincare plot analysis of heart rate variability: effect of endurance training. Eur J Appl Physiol 91:79–87. doi:10.1007/s00421-003-0917-0
Nagai N, Hamada T, Kimura T, Moritani T (2004) Moderate physical exercise increases cardiac autonomic nervous system activity in children with low heart rate variability. Childs Nerv Syst 20:209–214. doi:10.1007/s00381-004-0915-5 discussion 215
Otsuka K, Cornelissen G, Halberg F (1997) Age, gender and fractal scaling in heart rate variability. Clin Sci (Lond) 93:299–308
Pichot V, Busso T, Roche F, Garet M, Costes F, Duverney D, Lacour JR, Barthelemy JC (2002) Autonomic adaptations to intensive and overload training periods: a laboratory study. Med Sci Sports Exerc 34:1660–1666. doi:10.1097/00005768-200210000-00019
Portier H, Louisy F, Laude D, Berthelot M, Guezennec CY (2001) Intense endurance training on heart rate and blood pressure variability in runners. Med Sci Sports Exerc 33:1120–1125. doi:10.1097/00005768-200107000-00009
Rentero N, Cividjian A, Trevaks D, Pequignot JM, Quintin L, McAllen RM (2002) Activity patterns of cardiac vagal motoneurons in rat nucleus ambiguus. Am J Physiol Regul Integr Comp Physiol 283:R1327–R1334
Ruha A, Sallinen S, Nissila S (1997) A real-time microprocessor QRS detector system with a 1-ms timing accuracy for the measurement of ambulatory HRV. IEEE Trans Biomed Eng 44:159–167. doi:10.1109/10.554762
Sandercock GR, Bromley PD, Brodie DA (2005) Effects of exercise on heart rate variability: inferences from meta-analysis. Med Sci Sports Exerc 37:433–439. doi:10.1249/01.MSS.0000155388.39002.9D
Silvetti MS, Drago F, Ragonese P (2001) Heart rate variability in healthy children and adolescents is partially related to age and gender. Int J Cardiol 81:169–174. doi:10.1016/S0167-5273(01)00537-X
Tanner JM (1962) Growth at adolescence. Blackwell, Oxford
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability, standards of measurement, physiological interpretation, and clinical use. Circulation 93:1043–1065
Triposkiadis F, Ghiokas S, Skoularigis I, Kotsakis A, Giannakoulis I, Thanopoulos V (2002) Cardiac adaptation to intensive training in prepubertal swimmers. Eur J Clin Invest 32:16–23. doi:10.1046/j.0014-2972.2001.00939.x
Tulppo MP, Makikallio TH, Takala TE, Seppanen T, Huikuri HV (1996) Quantitative beat-to-beat analysis of heart rate dynamics during exercise. Am J Physiol 271:H244–H252
Verheyden B, Eijnde BO, Beckers F, Vanhees L, Aubert AE (2006) Low-dose exercise training does not influence cardiac autonomic control in healthy sedentary men aged 55–75 years. J Sports Sci 24:1137–1147. doi:10.1080/02640410500497634
Vinet A, Beck L, Nottin S, Obert P (2005) Effect of intensive training on heart rate variability in prepubertal swimmers. Eur J Clin Invest 35:610–614. doi:10.1111/j.1365-2362.2005.01557.x
Winsley RJ, Armstrong N, Bywater K, Fawkner SG (2003) Reliability of heart rate variability measures at rest and during light exercise in children. Br J Sports Med 37:550–552. doi:10.1136/bjsm.37.6.550
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen O, Skjaerpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115:3086–3094. doi:10.1161/CIRCULATIONAHA.106.675041
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gamelin, FX., Baquet, G., Berthoin, S. et al. Effect of high intensity intermittent training on heart rate variability in prepubescent children. Eur J Appl Physiol 105, 731–738 (2009). https://doi.org/10.1007/s00421-008-0955-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-008-0955-8