Abstract
We investigated the effect of 4 week of inspiratory (IMT) or expiratory muscle training (EMT), as well as the effect of a subsequent 6 week period of combined IMT/EMT on rowing performance in club-level oarsmen. Seventeen male rowers were allocated to either an IMT (n = 10) or EMT (n = 7) group. The groups underwent a 4 week IMT or EMT program; after interim testing, both groups subsequently performed a 6 week program of combined IMT/EMT. Exercise performance and physiological responses to exercise were measured at 4 and 10 week during an incremental rowing ergometer ‘step-test’ and a 6 min all-out (6MAO) effort. Pressure threshold respiratory muscle training was undertaken at the 30 repetition maximum load (∼50% of the peak inspiratory and expiratory mouth pressure, P Imax or P Emax, respectively). P Imax increased during the IMT phase of the training in the IMT group (26%, P < 0.001) and was accompanied by an improvement in mean power during the 6MAO (2.7%, P = 0.015). Despite an increase in P Emax by the end of the intervention (31%, P = 0.03), the EMT group showed no significant changes in any performance parameters during either the ‘step-test’ or 6MAO. There were no significant changes in breathing pattern or the metabolic response to the 6MAO test in either group, but the IMT group showed a small decrease in HR (2–5%, P = 0.001). We conclude that there were no significant additional changes following combined IMT/EMT. IMT improved rowing performance, but EMT and subsequent combined IMT/EMT did not.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Respiratory muscle training (RMT) yields improvements in exercise performance in both healthy young adults (McConnell and Romer 2004) and in patients with chronic obstructive pulmonary disease (COPD) (Lotters et al. 2002). In studies of healthy young people, two different forms of respiratory training have been employed: (a) voluntary isocapnic hyperpnoea (VIH) (Boutellier et al. 1992; Boutellier and Piwko 1992; Spengler et al. 1999; McMahon et al. 2002) and, (b) inspiratory muscle resistance training (IMT) (Volianitis et al. 2001b; Romer et al. 2002a, b; Edwards and Cooke 2004; Gething et al. 2004a; Gething et al. 2004b). The former is an endurance training approach that involves both the inspiratory and expiratory muscles, whilst the latter employs resistance training principles and is confined primarily to the inspiratory muscles. Both techniques apparently result in a similar pattern of physiological changes post-RMT (McConnell and Romer 2004), which suggests that the mechanism(s) for improved performance following RMT is independent of the training stimulus employed. However, it is unclear whether the expiratory muscle training (EMT), as occurs during VIH, provides any additional benefit to IMT alone.
A potential mechanism for the improved exercise performance that follows RMT centers around the notion that fatiguing respiratory muscles elicit a sympathetically mediated reflex vasoconstriction in locomotor muscles (Harms et al. 2000), thereby limiting limb blood flow. Prior fatigue of the inspiratory muscles accelerates the development of fatigue in the plantar flexors via a reflex change in limb blood flow (McConnell and Lomax 2006). Further, a 4 week period of IMT increases the intensity of inspiratory muscle work required to elicit changes in limb blood flow and plantar flexor fatigue. This was apparent from the observation that after IMT, an identical bout of prior inspiratory muscle work failed to induce any change in the fatigue profile of the plantar flexors. These data suggest that IMT acts to improve exercise performance by preserving limb blood flow during exercise.
The metaboreflex has been demonstrated in both expiratory and inspiratory muscles (Derchak et al. 2002; Sheel et al. 2002). If a mechanism based on the ablation of the respiratory muscle metaboreflex makes an important contribution to the improvements in exercise performance that follow RMT, we would predict that both specific IMT and specific EMT would improve performance. Further, we would predict that a combination of IMT and EMT would provide superior benefits compared with IMT or EMT alone.
Such a comparison has been made in patients with COPD. Weiner et al. (2003b) demonstrated that 12 week of specific EMT improved expiratory muscle strength and walking endurance, but did not decrease dyspnoea compared to a control group. However, in a subsequent study comparing IMT, EMT and a combined program of IMT/EMT, the authors reported no additional benefit of EMT, or a combined program of IMT/EMT compared to the benefits of IMT alone (Weiner et al. 2003a). The purpose of the present study was to compare the effects of 4 week of IMT or EMT upon ergometer rowing performance over 6 min (6MAO) in club-level oarsmen, as well as the effect of a subsequent 6 week period of combined IMT/EMT.
Methods
Seventeen competitive male rowers gave written informed consent to participate in the study, which was approved by Brunel University Research Ethics Committee. All participants were recruited from a local rowing club, and whilst they were at different stages of their rowing careers (competing >6 months) they trained under the same coach, and participated in an identical cardiovascular and resistance-training program during the study.
All seventeen participants were non-smokers and were free from upper respiratory tract infections. Two participants (one in the IMT group and one in the EMT group) were diagnosed with mild asthma. Only the subject in the IMT group demonstrated mild obstruction at rest. Neither participant suffered regularly from episodes of bronchoconstriction, and stated that symptoms were only brought on by upper respiratory tract infections or specific allergies. None of the participants were taking medication during the course of the study. Participants were requested to maintain their normal diet for 2 days prior to testing and to refrain from vigorous exercise and alcohol 2 days preceding the testing and to avoid caffeinated beverages the day of the test.
Design
Participants made at least three visits to the laboratory, but eight participants made four visits. The additional visit by these participants was at baseline, and was used to assess the within-subject variation (reliability) of the testing procedures. Following the baseline visit(s) participants were ranked according to their 6MAO rowing ergometer performance time and then divided into two groups. One group undertook 4 week of IMT (n = 10; age, 24.9 ± 5.6 year; stature, 1.9 ± 4.8 m; body mass, 83.7 ± 4.8 kg), whilst the other undertook 4 week of EMT (n = 7; age, 28.7 ± 9.1 year; stature, 1.9 ± 5.3 m; body mass, 82.6 ± 13.5 kg). Immediately at the end of this phase, the first post-intervention visit took place (Post-intervention 1). Thereafter two of the IMT group stopped training due to illness and difficulty with maintaining their rowing training program for personal reasons. The remaining participants (n = 15) undertook a 6 week period of combined IMT (n = 8) and EMT (n = 7). At the end of this combined phase of training a second post-intervention test took place (Post-intervention 2). This phase was extended to 6 week due to events in their rowing program.
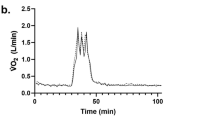
During their baseline visit to the laboratory, participants were familiarized with all procedures and each participant performed the entire protocol. Pre- and post-exercise respiratory mouth pressures and spirometry, including maximal flow volume loops (MFVLs) were recorded. A progressive incremental rowing exercise test was used to evaluate physiological variables and rowing ergometer performance expressed as mean power and distance covered. The final stage of the step test was a 6MAO to compare rowing performance between conditions. Physiological variables measured included: peak heart rate (HR) in the last 30 s of each stage; oxygen uptake ( \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \)); earlobe blood lactate concentration [La−]B and ratings of respiratory effort (RRE) at the end of each stage.
Procedures
Respiratory muscle strength
The P Imax and P Emax were assessed as expressions of inspiratory and expiratory muscle strength using a hand-held mouth pressure meter (MPM, Micro Medical Ltd, Kent, UK) in the standing position. The P Imax and P Emax manoeuvres were initiated at residual volume (RV) and total lung capacity (TLC), respectively. The assessment of maximal pressures required a sharp, forceful effort maintained for a minimum of ∼2 s. The pressure meter incorporated a 1 mm leak to prevent glottic closure during the P Imax manoeuvre and to reduce buccal muscle contribution during the P Emax manoeuvre (Black and Hyatt 1969). Participants were given prior instruction and were verbally coached throughout the manoeuvre. A minimum of five satisfactory inspiratory and expiratory efforts were conducted with the highest measurement within 0.5 kPa being defined as maximal (Volianitis et al. 2001a). Measurements were performed before and 2 min after completion of the 6MAO to determine improvements in maximal pressures due to training and to assess the extent of exercise-induced respiratory muscle fatigue (RMF), respectively.
Breathing pattern and oxygen uptake
Minute ventilation, MFVLs and pulmonary gas exchange indices were assessed during exercise using an online turbine ergospirometry system (Oxycon, Jaeger-Toennies, Hoechberg, Germany). Resting MFVLs were assessed using the same online system according to European Respiratory Society guidelines (Quanjer et al. 1993). The MFVLs were performed and the following measures were recorded: peak inspiratory flow (PIF), peak expiratory flow (PEF), forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1) and forced expiratory flow at 50% of FVC (FEF50%).
Incremental rowing ergometer test
The ergometer (Concept IIC, Vermont, USA) rowing protocol included four submaximal stages of 4 min duration, followed by one 6MAO effort at drag factor set to 138 (damper setting ∼4). Starting power was determined by calculating the power corresponding to each participant’s typical light aerobic training intensity, and subtracting 50 W. All participants perform both incremental and maximal exercise ergometer rowing as part of their routine training and monitoring. A light aerobic training intensity was defined as 55–70% of maximal HR at 18–20 strokes per minute. Subsequent stages were incremented by 25 W. There was a 1 min interval between each stage to allow for blood lactate and perceptual measurements. The participants selected the power and pace during the 6MAO effort and instructed to achieve the greatest distance possible (using the ergometer distance meter) in 6 min. The ergometer also displayed mean power for each stage.
Heart rate, blood lactate concentration and ratings of respiratory effort
The HR was assessed using a short-range telemetry system (Polar Sport Tester, Polar Electro, Finland) to the peak value during the final 30 s of each stage of the exercise. Blood lactate concentration [La−]B was sampled from the earlobe using a portable lactate analyser (Lactate Pro Portable Lactate Analyzer, Arkray, Japan) at the completion of each exercise stage. The Borg category-ratio scale (CR-10; Borg 1998) was used to profile respiratory effort during exercise. Each participant was provided with verbal and written instructions (Borg 1998) on the use of the scale prior to testing.
Inspiratory and expiratory muscle training
Participants were instructed on usage of the inspiratory (POWERbreathe®, Gaiam, UK) or expiratory (Powerlung®, Powerlung, USA) pressure threshold-loading devices for respiratory muscle training. The Powerlung® provides a threshold load during both inspiration and expiration. To isolate the expiratory load for the EMT group, the inspiratory load was disabled by removing the valve tensioning spring. Both groups were instructed to perform 30 inspiratory or expiratory efforts twice daily for 4 week against a pressure load equivalent to their individual 30 repetition maximum (30RM, equivalent to ∼50% of P Imax or P Emax), a protocol that is effective for IMT (Volianitis et al. 2001b; Romer et al. 2002a, b; Romer and McConnell 2003). Participants in both groups were instructed to breathe rapidly and with maximal effort against the training load. The IMT group was instructed to initiate each breath from RV and to sustain the effort until their lungs felt full. The EMT group was instructed to initiate each breath from TLC and to sustain the effort until their lungs were empty. Participants were instructed to increase the training load in order to maintain it at the 30RM (Romer et al. 2002a), which increased throughout the training period. Following the first 4 week of either IMT or EMT, all participants undertook 6 week of combined IMT/EMT using the respiratory muscle trainer that had been used by the EMT group. For this phase of the study, the device applied both an inspiratory and expiratory load. Participants were directed to perform both maximal inspirations and expirations for 30RM, twice daily and to increase resistance when necessary to maintain the intensity at the 30RM load. Participants completed respiratory training diaries while they continued their scheduled whole body exercise training throughout the intervention.
Statistical analyses
Ratio limits of agreement were calculated to determine the within-subject variation according to the procedures of Bland and Altman (1986). Thus, the 95% ratio limits of agreements were used to estimate sample sizes for a range of treatment effects (including those measured post-intervention) for a repeated-measures design, given a statistical power of 0.9 and an alpha level of 0.05. These estimates were performed using a bespoke Excel spreadsheet, based upon the calculations of Zar (1998).
A repeated measures analysis of variance (ANOVA) was used to evaluate ‘treatment’ (IMT and EMT) and ‘time’ on each of the dependent variables. Planned pairwise comparisons were made with repeated measures t tests to compare main effects; the Bonferroni adjustment was used to modify for per family type I error rate per comparison and probability values of ≤0.05 were considered significant. Pearson’s bivariate correlations were used to determine significant relationships between variables. Data were analysed using the statistical software package SPSS V10.0 for Windows (Chicago, IL, USA) and results are reported as the mean ± standard deviation (SD).
Inter-test precision
Parameters derived for the MFVL and mouth pressures showed the lowest reliability compared with the other variables measured (Table 1). The data suggested that the study had sufficient power to detect changes in most parameters with an effect size of >20% (assuming n = 7 per group). The exceptions were FVC and FEV1, which required effect sizes of >5 and 10%, respectively. In contrast mean power, distance, \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \,_{{6{\text{MAO}}}} \) and HR required effect sizes of >5%. The highest reliability was observed in the RRE which required an effect size of <5%.
Results
Adherence to respiratory training
Training adherence to the IMT-only and EMT-only phases was similar between groups. The IMT group completed a total of 42.7 ± 9.7 sessions (76 ± 17.3% of prescribed) and the EMT group a total of 43.4 ± 5.5 (78 ± 9.8%). During the combined program phase of the study, the IMT group adherence remained unchanged at 74.5 ± 33.4%, whilst the adherence in the EMT group fell to 60.3 ± 37.3% (P = 0.42) of the prescribed training sessions.
Respiratory muscle and pulmonary function
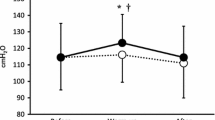
There was an interaction over time within groups (P = 0.00), as well as between the two groups over time (P = 0.008) in P Imax (Table 2). PreEx-P Imax in the IMT group was 26% higher compared to baseline after 4 week of IMT (P = 0.00) and improved by a further 3.3% after the combined IMT/EMT phase to 30% (P = 0.00 relative to baseline). The EMT group also showed a small improvement in P Imax after the combined IMT/EMT program to 13% (P = 0.03) (Fig. 1a).
Maximal inspiratory and expiratory pressure pre- and post-exercise compared to Baseline 2; Comparison of post-exercise inspiratory and expiratory muscle fatigue between groups. IMT light gray, EMT black; PreEx-P Imax pre-exercise maximal inspiratory pressure, PreEx-P Emax pre-exercise maximal inspiratory pressure, IMF inspiratory muscle fatigue, EMF expiratory muscle fatigue. *Different than baseline 2 (P ≤ 0.05); †Different than preceding time point (P ≤ 0.05)
Expiratory muscle strength
The IMT group showed no significant change in P Emax during the IMT-only phase of training (Table 2). During the combined IMT/EMT phase, the IMT group showed no statistically significant improvement in P Emax (to 23%) (P = 0.06). During the EMT-only phase, the P Emax did not increase significantly (18%). During the combined IMT/EMT phase, the EMT group showed a further (relative to baseline) improvement in P Emax (to 31%) (P = 0.03).
Exercise-induced inspiratory and expiratory muscle fatigue
Only the IMT group exhibited a change over time in the exercise-induced fall in P Imax (inspiratory muscle fatigue = IMF) following IMT and combined IMT/EMT (P = 0.03) (Table 2, Fig. 1). In the IMT group, IMF persisted following the IMT phase, but was abolished following the combined IMT/EMT phase. In contrast, the EMT group showed no significant change in the severity of IMF at any stage; the exercise-induced fall in P Emax (expiratory muscle fatigue = EMF) tended to decrease in the EMT group after 4 week of EMT-only training (from a fall of 13 to 8%). There was no further change after the combined IMT/EMT phase. In the IMT group, EMF showed no change during the IMT-only phase, but tended to be reduced following the combined IMT/EMT phase (from a fall of 15 to 5%).
In contrast to the percentage changes in P Imax and P Emax post-exercise, which largely persisted at the same magnitude following the interventions (Fig. 1c, d), the absolute values for post-exercise P Imax and P Emax showed consistent improvements in both groups (Table 2). There were no significant correlations between the changes in respiratory muscle fatigue and the changes in exercise performance in either group at any stage of the intervention.
Maximal flow volume loop
Baseline pulmonary function data were similar to baseline values (Table 2). The only changes in pulmonary function were an increase in PIFR in the IMT group following the IMT phase (P = 0.04), and a decrease in FVC following the combined IMT/EMT phase (P = 0.03).
Breathing pattern and physiological variables during rowing
No significant change was found in V T, MIFR, \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}_{{\text{E}}} \) and f R after IMT, EMT, or combined IMT/EMT in either group. However, for the IMT group, there was a correlation between the individual changes in P Imax and \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}_{{\text{E}}} \) (the value at stage 4 was selected for comparison) between baseline and post-intervention test 2 (r = 0.85, P = 0.02), as well as between post-intervention 1 and 2 (r = 0.90, P = 0.02).
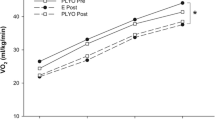
Oxygen uptake and heart rate
No significant differences in \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \) were evident after either phase of the intervention in either group (Table 3). Although there was no statistically significant change in end-exercise HR (6MAO) (P = 0.28), a paired t test was performed to interpret the average change in HR in both groups across all steps. There was an average decrease of 2–5% for the IMT group across all steps following the IMT phase of the intervention (P = 0.00) and during the sub-maximal steps following the combined IMT/EMT phase (P = 0.00). There was no change in the EMT group in HR at any stage after either phase of training.
Blood lactate
There was no significant interaction over time within groups (P = 0.08), or between the two groups over time (P = 0.38). However, there was a tendency for [La−]B to be lower in the IMT group after training (Table 3). Alterations to the [La−]B relationship in this group were greatest following the combined IMT/EMT phase (average decrease in [La−]B across all steps = 30%) and there was a lower [La−]B immediately after the 6MAO effort (14%, P = 0.05). We calculated that a sample size of >10 (per group) would be required in order to detect an effect of 30% during the sub-maximal stages. It is therefore possible that the lack of significance for the sub-maximal steps is a type 2 error. There was a weak correlation between the individual changes in P Imax and [La−]B between baseline and post-intervention test 1 (r = 0.62, P = 0.06). There was no change in mean [La−]B in the EMT group after either phase of training.
Ratings of respiratory effort sensation
A difference in the step and group interaction for the RRE was found between the IMT and EMT groups (P = 0.07) over the two intervention phases of the study (Table 3). Although effect sizes were >10% during the submaximal stages, a paired t test revealed no difference between the baseline and post-intervention phases. A reduction in the rating of RRE was evident in the IMT group following the 6MAO (P = 0.05). There was no correlation between the individual changes in P Imax and RRE (the rating at stage 4 was selected for comparison) between baseline and post-intervention test 1 or 2. No change was evident in the RRE of the EMT group at any stage, after either phase of training.
Rowing performance
The IMT group showed a 2.7% improvement in mean power after the IMT phase (P = 0.02), followed by a further non-significant improvement of 1.6% after the combined IMT/EMT phase (P = 0.08) (Fig. 2a). No significant change was evident in the EMT group after either phase of training.
The IMT group improved their overall distance completed in the 6MAO efforts by 0.92% (16.2 m) following the IMT phase (P = 0.02). There was no further increase following the IMT/EMT phase (Fig. 2b). No change was evident in the EMT group after either phase of training.
There was no significant correlation between the individual changes in P Imax and either index of rowing performance between baseline and post-intervention test 1 or 2. Similarly, there was no significant correlation between the change in rowing performance and the changes in \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \), HR, [La−]B, or RRE between baseline and post-intervention test 1 or 2.
Discussion
The aim of this study was to differentiate the effects of IMT, EMT and a combined IMT/EMT program upon rowing performance and the physiological responses to maximal and sub-maximal rowing. Following the first phase of training during which participants performed IMT or EMT, the IMT group showed an improvement in P Imax, but no change in P Emax. The EMT group showed no statistically significant improvement in P Emax or P Imax during this first phase. During the combined IMT/EMT phase, the IMT group showed a further small improvement in P Imax, and an improvement in P Emax. The EMT group showed a small improvement in P Imax, and a further improvement in P Emax. These changes were only associated with improvements in rowing performance in the IMT group. Furthermore, the addition of EMT to the IMT group’s training during the combined IMT/EMT phase resulted in only minor additional improvements in rowing performance, despite an improvement in P Emax. The temporal patterns of the changes in respiratory muscle strength and rowing performance lead us to concluded that IMT induced the greatest improvements in performance. However, we do not believe that the change in P Imax per se is the factor resulting in improved rowing performance. Rather, we propose that IMT induced improvements to the structure and function of the inspiratory muscles that elicited an increase in the intensity of inspiratory muscle work that was required to elicit the inspiratory muscle metaboreflex. Changes to expiratory muscle function failed to induce changes in performance and may indicate that, (1) the potency of the expiratory muscle metaboreflex is lower than that of the inspiratory muscles, and/or, (2) the threshold of the expiratory muscle metaboreflex is higher than that of the inspiratory muscles, and it is not activated by maximal rowing.
Adherence to respiratory training
During the first 4 week, training adherence was comparable between the two groups; however, a decrease in training adherence was apparent in the EMT group during the combined training phase (from 77% of prescribed sessions to 60%) and most likely, contributed to the smaller improvement observed in P Imax. The decrease in mean adherence was partly due to two of the EMT participants contracting upper respiratory infections during the combined training phase.
Respiratory muscle function
Inspiratory muscle strength
The IMT group showed progressive improvement in P Imax at both post-intervention testing sessions; these results are similar to those studies using pressure-threshold training, which range from 25–45% (Volianitis et al. 2001b; Edwards and Cooke 2004). During the combined training phase, the IMT group displayed a ‘plateau’ of improvement consistent with previous studies (Volianitis et al. 2001b; Romer and McConnell 2003).
By the end of the 10 week intervention, the EMT group achieved an improvement of 13% in P Imax, with no associated change in rowing performance; Hart et al. (2001) also observed no change in incremental treadmill performance after a 6 week program of IMT that increased P Imax by 10%. This suggests that improvement in performance following IMT requires an intensity of training that increases P Imax by >25% (Volianitis et al. 2001b; Romer et al. 2002a, b; Edwards and Cooke 2004; Gething et al. 2004a, b). A further contributory factor to the poorer than anticipated strength improvements during the combined training phase may have been the training device. Participants found the combined IMT/EMT more challenging than training during only one phase of the breathing cycle. Thus, increased breathing effort during both phases of the respiratory cycle led to impairment of the intensity of training that could be tolerated in each. Combined IMT and EMT in young swimmers, using the same device as was used here, also yielded a modest change in both P Imax and P Emax, despite a 12 week training intervention and an increase in training intensity after 6 week, but no change in swimming performance (Wells et al. 2005).
Expiratory muscle strength
Maximal expiratory pressures (P Emax) increased in both groups, with the greatest overall improvement occurring in the EMT group. The improvement in P Emax observed in the IMT group during the combined phase of training was not significantly different from that observed in the EMT group during the EMT phase. Despite these improvements in P Emax there appeared to be no associated changes in rowing performance in either group.
Respiratory muscle fatigue
Inspiratory muscle fatigue has been attenuated post-IMT (Volianitis et al. 2001b; Romer et al. 2002c), which did not occur in the present study. The percentage fall in P Imax (IMF) post-exercise remained unchanged after the IMT, and there was an improvement in mean power during the 6MAO. Furthermore, the combined IMT/EMT phase resulted in attenuation of IMF, but a smaller further improvement in mean power compared to the IMT only phase. There are two potential explanations for this: (1) that the attenuation of IMF per se does not play a role in the improved performance that follows IMT, and/or, (2) that IMF was delayed, but not attenuated, thereby permitting limb blood flow to be maintained for longer during the 6MAO effort. Since the inspiratory muscle metaboreflex appears to exhibit ‘threshold’ qualities (Sheel et al. 2002), the threshold for stimulation of the metaboreflex may not have been exceeded after IMT, despite a fall in P Imax. We have recently shown that after IMT the same inspiratory loading task failed to elicit metaboreflex induced changes in limb blood flow, but still induced inspiratory muscle fatigue (McConnell and Lomax 2006).
Performance implications
After 4 week of RMT, only the IMT group demonstrated an improvement in indices of rowing performance, with only a slight further improvement in performance after the combined training phase. These results are consistent with the plateau in performance observed by Volianitis et al. (2001b) after 4 week of IMT. The increase of 16.2 m following IMT is greater than the average scull boat length (average 8.2–13.4 m) and comparable to the average length of a sweep-oar rowing boat (10.4–19.9 m, depending on the number of oarsmen).
Physiological variables
IMT reduces HR at equivalent intensities of exercise (Haas and Haas 1981; Swanson 1998; Gething et al. 2004a), as well as reducing [La−]B , respiratory and/or whole body effort sensations (Volianitis et al. 2001b; Romer et al. 2002a, b). Gething et al. (2004a) observed a decrease in exercising HR of ∼6 bpm at the end of a 5 min bout of constant power cycling after their 6 week of IMT that increased P Imax by 29%. Haas and Haas (1981) also observed a lower HR and \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \) during submaximal exercise after a 16 d combined program of VIH and inspiratory resistance loading (IRL) in healthy adults. Similarly, Swanson (1998) reported a decrease in HR after 6 week of VIH. The mechanism by which HR might decrease following IMT can only be speculated upon, but one explanation for changes in cardiovascular response to exercise is an improvement in inspiratory muscle efficiency following IMT, thereby preserving blood flow to the working muscles, and/or a delay/attenuation of the metaboreflex-induced increase in sympathetic vasomotor outflow (Sheel et al. 2002). A decrease in HR and a slight, though non-significant, decrease in \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \) is consistent with these suggestions. Data from the present study, HR, RRE and \( \ifmmode\expandafter\dot\else\expandafter\.\fi{V}{\text{O}}_{2} \) all showed attenuation after IMT. In some instances, our failure to achieve statistical significance was due to type 2 error. However, it was striking that EMT induced no discernable changes, or trends in any of the parameters measured, either during the EMT-only phase, or the combined IMT/EMT phase, in either group (Table 3).
Our finding of an improvement in P Imax combined with a decreased in [La−]B is similar to that of Romer et al. (2002b), who observed an IMT-induced improvement of P Imax of 31% in their training group, with a 15.7% decrease in [La−]B. Spengler et al. (1999) and Romer et al. (2002b) also reported a correlation between the change in [La−]B and exercise performance. Spengler et al. (1999) suggested that the reason for this change in the lactate response was that trained respiratory muscles used more lactate as fuel to maintain work output. Since there was no further decrease after the EMT, or the combined IMT/EMT training, decreases in [La−]B are attributable only to IMT. McConnell and Sharpe (2005) showed that the IMT-induced reduction in [La−]B was not associated with a change in the exercise intensity equivalent to the maximal lactate steady state, which suggests that performance improvement after IMT cannot be ascribed to an increase in ‘lactate threshold’.
Conclusion
The present study systematically compared the effects of IMT and EMT in healthy young adults. We observed no apparent benefits of EMT, either alone, or in combination with IMT. However, the responses of our participants to IMT were largely consistent with those of previous studies, with an improvement in rowing performance being accompanied by improvements in factors such as HR, [La−]B and effort perception. In contrast, despite improvements in P Emax there were no discernable changes in any of the performance or physiological parameters measured. EMT does not appear to result in any improvements in rowing performance.
References
Black LF, Hyatt RE (1969) Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 99:696–702
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Borg G (1998) Borg’s perceived exertion and pain scales. Human Kinetics, Champaign
Boutellier U, Piwko P (1992) The respiratory system as an exercise limiting factor in normal sedentary subjects. Eur J Appl Physiol Occup Physiol 64:145–152
Boutellier U, Buchel R, Kundert A, Spengler C (1992) The respiratory system as an exercise limiting factor in normal trained subjects. Eur J Appl Physiol Occup Physiol 65:347–353
Derchak PA, Sheel AW, Morgan BJ, Dempsey JA (2002) Effects of expiratory muscle work on muscle sympathetic nerve activity. J Appl Physiol 92:1539–1552
Edwards AM, Cooke CB (2004) Oxygen uptake kinetics and maximal aerobic power are unaffected by inspiratory muscle training in healthy subjects where time to exhaustion is extended. Eur J Appl Physiol 93:139–144
Gething AD, Passfield L, Davies B (2004a) The effects of different inspiratory muscle training intensities on exercising heart rate and perceived exertion. Eur J Appl Physiol 92:50–55
Gething AD, Williams M, Davies B (2004b) Inspiratory resistive loading improves cycling capacity: a placebo controlled trial. Br J Sports Med 38:730–736
Haas F, Haas A (1981) Effect of inspiratory muscle training in healthy subjects. FASEB 40:540
Harms CA, Wetter TJ, St Croix CM, Pegelow DF, Dempsey JA (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Hart N, Sylvester K, Ward S, Cramer D, Moxham J, Polkey MI (2001) Evaluation of an inspiratory muscle trainer in healthy humans. Respir Med 95:526–531
Lotters F, van Tol B, Kwakkel G, Gosselink R (2002) Effects of controlled inspiratory muscle training in patients with COPD: a meta-analysis. Eur Res J 20:570–577
McConnell AK, Lomax M (2006) The influence of inspiratory muscle work history and specific inspiratory muscle training upon human limb muscle fatigue. J Physiol
McConnell AK, Romer LM (2004) Respiratory muscle training in healthy humans: resolving the controversy. Int J Sports Med 25:284–293
McConnell AK, Sharpe GR (2005) The effect of inspiratory muscle training upon maximum lactate steady-state and blood lactate concentration. Eur J Appl Physiol 94:277–284
McMahon ME, Boutellier U, Smith RM, Spengler CM (2002) Hyperpnea training attenuates peripheral chemosensitivity and improves cycling endurance. J Exp Biol 205:3937–3943
Quanjer PH, Tammeling GJ, Cotes JE, Pederson OF, Peslin R, Yernault JC (1993) Lung volumes and forced ventilatory flows. Eur Res J 6:5–40
Romer LM, McConnell AK (2003) Specificity and reversibility of inspiratory muscle training. Med Sci Sports Exerc 35:237–244
Romer LM, McConnell AK, Jones DA (2002a) Effects of inspiratory muscle training on time-trial performance in trained cyclists. J Sports Sci 20:547–562
Romer LM, McConnell AK, Jones DA (2002b) Effects of inspiratory muscle training upon recovery time during high intensity, repetitive sprint activity. Int J Sports Med 23:353–360
Romer LM, McConnell AK, Jones DA (2002c) Inspiratory muscle fatigue in trained cyclists: effects of inspiratory muscle training. Med Sci Sports Exerc 34:785–792
Sheel AW, Derchak PA, Pegelow DF, Dempsey JA (2002) Threshold effects of respiratory muscle work on limb vascular resistance. Am J Physiol Heart Circ Physiol 282:H1732–H1738
Spengler CM, Roos M, Laube SM, Boutellier U (1999) Decreased exercise blood lactate concentrations after respiratory endurance training in humans. Eur J Appl Physiol Occup Physiol 79:299–305
Swanson GD. (1998) Pulmonary training may alter exertional dyspnea and fatigue via an exercise-like training effect of a lowered heart rate. In: Hughson RL, Cunningham DA, Duffin J (eds) Advances in modelling and control of ventilation. Plenum Press, New York, pp 231–236
Volianitis S, McConnell AK, Jones DA (2001a) Assessment of maximum inspiratory pressure. Prior submaximal respiratory muscle activity (‘warm-up’) enhances maximum inspiratory activity and attenuates the learning effect of repeated measurement. Respiration 68:22–27
Volianitis S, McConnell AK, Koutedakis Y, McNaughton L, Backx K, Jones DA (2001b) Inspiratory muscle training improves rowing performance. Med Sci Sports Exerc 33:803–809
Weiner P, Magadle R, Beckerman M, Weiner M, Berar-Yanay N (2003a) Comparison of specific expiratory, inspiratory, and combined muscle training programs in COPD. Chest 124:1357–1364
Weiner P, Magadle R, Beckerman M, Weiner M, Berar-Yanay N (2003b) Specific expiratory muscle training in COPD. Chest 124:468–473
Wells GD, Plyley M, Thomas S, Goodman L, Duffin J (2005) Effects of concurrent inspiratory and expiratory muscle training on respiratory and exercise performance in competitive swimmers. Eur J Appl Physiol 94:527–540
Zar JH (1998) Biostatistical analysis. Prentice Hall, New Jersey
Acknowledgments
We would like to thank the oarsmen of the Thames Tradesmen rowing club for their participation in this study. Conflicts of Interest: Alison McConnell has a beneficial interest in the POWERbreathe® Inspiratory Muscle Trainer in the form of a royalty share on license income to the University of Birmingham, UK. She also acts as a consultant to Gaiam Ltd. The authors are grateful to Gaiam Ltd. and MicroMedical Ltd. for donation of equipment for use in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Griffiths, L.A., McConnell, A.K. The influence of inspiratory and expiratory muscle training upon rowing performance. Eur J Appl Physiol 99, 457–466 (2007). https://doi.org/10.1007/s00421-006-0367-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-006-0367-6