Abstract
The mechanism that alters the pulmonary \(\dot{V}\hbox{O}_{2}\) response to heavy-intensity exercise following prior heavy exercise has been frequently ascribed to an improvement in pre-exercise blood flow (BF) or O2 delivery. Interventions to improve O2 delivery have rarely resulted in a similar enhancement of \(\dot{V}\hbox{O}_{2}.\) However, the actual limb blood flow and \(\dot{V}\hbox{O}_{2}\) dynamics in the second bout of repeated exercise remain equivocal. Seven healthy female subjects (21–32 years) performed consecutive 6-min (separated by 6 min of 10 W exercise) bilateral knee extension (KE) exercise in a semisupine position at a work rate halfway between the lactate threshold (LT) and \(\dot{V}\hbox{O}_{2}\)peak. Femoral artery blood flow (FBF) was measured by Doppler ultrasound simultaneously with breath-by-breath \(\dot{V}\hbox{O}_{2};\) each protocol being repeated at least four times for precise kinetic characterization. The effective time-constant (τ′) of the \(\dot{V}\hbox{O}_{2}\) response was reduced following prior exercise (bout 1: 61.0 ±10.5 vs. bout 2: 51.6±9.0 s; mean ± SD; P<0.05), which was a result of a reduced slow component (bout 1: 16.0±8.0 vs. bout 2: 12.5±6.7 %; P<0.05) and an unchanged ‘primary’ τ. FBF was consistently faster than \(\dot{V}\hbox{O}_{2}.\) However, there was no bout-effect on τ′ FBF (bout 1: 28.2±12.0 vs. bout 2: 34.2±8.5 s). The relationship between the exercise-associated \(\dot{V}\hbox{O}_{2}\) (i.e., \(\Delta \dot{V}\hbox{O}_{2}\)) and Δ FBF was similar between bouts, with a tendency (N.S: P>0.05) for \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF}\) to be increased during the transition to bout 2 rather than decreased, as hypothesized. The return of \(\dot{V}\hbox{O}_{2}\) kinetics toward first order, therefore, was associated with an ‘appropriate’, not enhanced, BF to the working muscles. Whether a relative prior-hyperemia in bout 2 enables a more homogeneous intramuscular distribution of BF and/or metabolic response is unclear, however, these data are consistent with events more proximal to the exercise muscle in mediating the \(\dot{V}\hbox{O}_{2}\) response during repeated heavy-intensity KE exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During heavy-intensity cycle ergometry (i.e., work rates that result in prolonged increases in circulating blood lactate, above the lactate threshold; LT) the determinants of muscular O2 consumption (QO2) and pulmonary O2 uptake \(\left(\dot{V}\hbox{O}_{2}\right)\) are poorly understood. The determinants of QO2 in this region have been attributed to such mechanisms as: O2 delivery (Hughson et al. 2001; MacDonald et al. 1997, 2001; Perrey et al. 2001); inertia of O2 utilization linked to intramuscular phosphate metabolism (Chance et al. 1986; Mahler 1985; Rossiter et al. 1999); or a substrate delivery limitation (in the form of reducing equivalents; Timmons et al. 1998). During cycle ergometry the dynamics of \(\dot{V}\hbox{O}_{2},\) subsequent to ‘phase I’ (Whipp et al. 1982), have been shown to closely reflect both QO2 (Grassi et al. 1996; Poole et al. 1991) and intramuscular phosphocreatine metabolism (Rossiter et al. 2001) and, therefore, the determination of \(\dot{V}\hbox{O}_{2}\) kinetics allows insights into the control of QO2.
During heavy-intensity exercise the expected first-order response dynamics of \(\dot{V}\hbox{O}_{2}\) (expected from first order intramuscular enzymatic processes; Mahler 1985) are supplemented by an additional delayed component yielding a slowly developing rise in \(\dot{V}\hbox{O}_{2}\) (i.e., the \(\dot{V}\hbox{O}_{2}\) ‘slow’ component) (Poole et al. 1994) that, if the exercise is sustained, can lead to the attainment of \(\dot{V}\hbox{O}_{2}\hbox{max}\) and fatigue. Following the studies of Gerbino et al. (1996), MacDonald et al. (2001) and Burnley et al. (2000), it was further demonstrated that \(\dot{V}\hbox{O}_{2}\) kinetics will return close to first-order, if the exercise is preceded by a ‘priming’ bout of sufficiently high intensity (Endo et al. 2004).
The functional ‘trimming-out’ of the slow component following ‘priming’ exercise (Burnley et al. 2002; Gerbino et al. 1996; MacDonald et al. 2001; Rossiter et al. 2002; Tordi et al. 2003) is commonly ascribed to improved muscle blood flow, and/or, O2 delivery (Gerbino et al. 1996; Hughson et al. 2001; MacDonald et al. 2001) resulting from such mechanisms as vasodilatation (from residual action of vasoactive substances consequent to prior exercise) or the Bohr effect, although, this is not consistently the case (Paterson et al. 2005; Walsh et al. 2002). As such, the mechanism(s) of \(\dot{V}\hbox{O}_{2}\) kinetic adaptation during such repeated heavy-intensity exercise remain(s) equivocal.
Three studies of particular interest, where attempts have been made to determine the kinetics of muscle blood flow and the fundamental and slow components of \(\dot{V}\hbox{O}_{2}\) during repeated heavy-intensity exercise, are those of MacDonald et al. (2001), Fukuba et al. (2004) and Paterson et al. (2005). All of these investigations (using either handgrip or knee-extension (KE) exercise) have shown an increased muscle blood flow (BF) prior to the second exercise bout. However, they have shown a range of responses during the second bout of repeated exercise, with both Fukuba et al. (2004) and Paterson et al. (2005) demonstrating a reduced phase II \(\tau \dot{V}\hbox{O}_{2},\) only Fukuba et al. (2004) showing a reduction of the \(\dot{V}\hbox{O}_{2}\) slow component, but neither of them modulating BF response kinetics. It is to be noted, therefore, that both these studies manifest a large post exercise hyperemia, which reflects a ‘blunting’ of the exercise BF response, possibly due to high intramuscular forces during contractions (see Hoelting et al. 2001; Shoemaker et al. 1994; Wilkerson et al. 2004). In the present study, therefore, a relatively large muscle mass was utilized for exercising, during ‘low-force’ but high-intensity dynamic exercise (that was more akin to cycle ergometry than ‘weight-lifting’ style KE exercise; see details in methods) that would allow a confident estimation of the kinetics of \(\dot{V}\hbox{O}_{2}\) and exercising muscle BF. Furthermore, as discussed by Yoshida and Whipp (1995), adequate tissue oxygenation is crucially dependent on tissue QO2/BF ratio. Therefore, we also wished to make a non-invasive estimate of QO2/BF (rather than their time constants (τ) alone) during bilateral KE exercise requiring coordinated leg movement in a fashion similar to cycle ergometry. We hypothesized that the facilitation of \(\dot{V}\hbox{O}_{2}\) kinetics (e.g., a reduction in τ and/or the \(\dot{V}\hbox{O}_{2}\) slow component) seen during exercise following a priming bout would be reflected in the faster adaptation of BF to the working muscles (as suggested by Gerbino et al. 1996; MacDonald et al. 2001), and that this would result in a better maintenance of QO2/BF during the transient.
Methods
Subjects
Seven healthy Japanese female subjects volunteered for the study (mean ± SD; age: 24±4 years, height: 160±3 cm, weight: 52±3 kg) and gave written informed consent approved by the ethics committees of the institutions involved (in accordance with the Declaration of Helsinki).
Exercise protocols
All exercise was performed using (bilateral KE exercise) on a specially designed ergometer. For this, each foot was placed in an Achilles-bracing heel-cup attached, by a long steel-rod, to the pedal arm of an electromagnetically braked cycle ergometer (232c-XL, Combi) positioned behind the seated subject. One complete turn of the pedal arm required the knee to extend from 90° to ∼135°. The alternate movement of both legs required smoothly coordinated and continuous movement in a very similar manner to that of standard cycle ergometer exercise. The exercise model in this study was, therefore, different from the usual lateral knee-kicking exercise using a Krogh-type resistance-load cycle ergometer (e.g. Andersen et al. 1985) or bilateral knee-kicking exercise in which a weight is lifted by each leg independently (e.g., Fukuba et al. 2004). The exercise frequency was kept at 60 times per min per leg alternatively (directed by an audible signal 120 times per min). The ergometer had an adjustable seated-backrest allowing the subjects to be positioned semisupine i.e., with a hip angle of 150°.
The subjects initially performed a ramp-incremental exercise test (4 W.min−1) to the limit of tolerance using bilateral KE exercise. Ventilatory and gas exchange parameters were measured breath-by-breath allowing estimation of the LT and \(\dot{V}\hbox{O}_{2}\hbox{peak}.\) Capillary blood was sampled every 2 min for enzymatic determination of blood lactate (HEK-30L, Toyobo, Japan). The LT was estimated using the V-slope method (Beaver et al. 1986) and gas exchange criteria using corroboration from the point at which there was a systematic increase in the ventilatory equivalent for \(\dot{V}\hbox{O}_{2} \left(\dot{V}\hbox{E}/\dot{V}\hbox{O}_{2}\right)\) and end-tidal PO2, with no concomitant increase in the ventilatory equivalent for CO2 output (\(\dot{V}\)E/\(\dot{V}\)CO2) or decrease in end-tidal PCO2 (Whipp 1994); these were corroborated in the profile of blood lactate in every case.
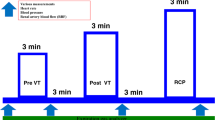
Following this, each subject completed repeated bouts (randomized throughout the subjects’ menstrual cycle) of high-intensity square-wave exercise on the KE apparatus with the seat and bicycle in the same position for each subject as the previous incremental test. The exercise intensity for the repeated bout was set at Δ 50% (based on the linear extrapolation of the \(\dot{V}\hbox{O}_{2}\)–work rate relationship below LT to \(\dot{V}\hbox{O}_{2}\hbox{peak}\) while accounting for the delay time between the work rate and \(\dot{V}\hbox{O}_{2}\) response observed during ramp-incremental exercise test (Whipp 1982); Δ is the work rate difference between the LT and \(\dot{V}\hbox{O}_{2}\hbox{peak}\)). This resulted in an average work rate of 52±7 W. The protocol consisted of a 4-min baseline KE exercise at 10 W followed by two consecutive 6-min work bouts at Δ 50% separated by 6 min of baseline KE exercise at 10 W. The subjects performed a total of 4–12 repetitions of the repeated bout exercise. The number of repetitions required for each subject was governed by signal-to-noise characteristics of averaged \(\dot{V}\hbox{O}_{2}\) and femoral artery blood flow (FBF) responses, allowing appropriate convergence of the confidence limits for the subsequent parameter estimation procedures. The repeated bout exercise was performed at the same time on separate days.
Measurements
Ventilatory and gas exchange responses were determined breath-by-breath by a computerized metabolic measuring system (RM-300, Minato Medical Co.,Japan) as previously described (Endo et al. 2003, 2004; Fukuba et al. 2004). Briefly, prior to each exercise test, a hot-wire flow-sensor and gas analyzers were calibrated using a known volume of air at several mean flow rates, and gas mixtures of known concentration, respectively. The heart rate (HR) was monitored continuously via a three-lead electrocardiotachogram (ECG) (BP-306, Colin). A second-by-second time course was calculated for each gas exchange variable by interpolation of the breath-by-breath data. Data were stored on disk for further analysis. Mean arterial pressure (MAP) was measured by using a photoplethysmograph finger blood pressure cuff (Omeda 2300, Finapres) on the middle finger at the level of femoral artery. The photoplethysmograph was calibrated by mercury manometer measurement with an arm cuff on the left arm before onset of exercise.
The FBF in the right femoral artery was obtained using simultaneous pulsed and echo Doppler ultrasound to measure mean blood velocity (MBV) and femoral artery diameter at a site ∼2–3 cm distal to the inguinal ligament. The FBF was obtained on a beat-by-beat basis with the pulsed Doppler system (Logiq 400, GE-Yokogawa Medical Systems, Japan) using a linear-array 4-MHz probe with the angle of insonation of 50–60°. During the practice sessions both the experimenter and the subjects determined the optimal positions of the sample volume location, which was recorded on videotape for future reference (i.e., ∼2–3 cm above the common femoral artery superficial and profundus branch bifurcation and ∼2 cm depth from the skin surface). The subject then held the probe and practiced with the experimenter to learn the pattern of arterial movement during the repeated bout exercise. The procedure with the subject holding the probe with continuous monitoring by the experimenter contrasted previous KE studies where the experimenter held the probe (e.g., MacDonald et al. 1998, 2001). However, after several practice sessions, the subjects were accustomed to obtaining reliable images and blood velocity profiles of the femoral artery by using both auditory and visual feedback of the Doppler signals, and we found this to be a more reliable method (the subject was better able to consistently track the vessel movement) than the method previously employed. To avoid failure in Doppler insonation (i.e., improper alignment of the ultrasound beam with the artery) due to blood vessel movement during KE exercise, a sample volume was occasionally repositioned at the optimal location in the femoral artery by moving a trackball, guided by the longitudinal image and rotatable flow-directional axis. The audio-range signals for antegrade and retrograde flow reflected from the moving blood cells, and the ECG signal were digitally sampled online at 20 kHz, and then analyzed offline by our Doppler signal processing software [Fast Fourier transfer analysis (FFT) by 256 point Hamming window (i.e., each 12.8 ms)], to yield instantaneous MBV. The calculated velocity signals were recorded at every 10 ms on a computer together with the B-mode echo images of the right femoral artery, which were obtained with a transmission frequency of 6.6-MHz using the same linear-array probe as the pulsed Doppler system. The cross-sectional area of the artery vessel was recorded on SVHS videotape and analyzed for artery diameter with on-screen calipers. Femoral artery diameter was measured at rest and during exercise; that is, five times at rest, each 10 s during the first 2 min of exercise, and then at 1-min intervals till the end of exercise, similar to the methods previously utilized (e.g., MacDonald et al. 1998, 2001). As the vessel diameters at rest and during exercise did not show any systematic changes, we used the vessel diameter at rest to calculate FBF. Room air was kept at 25±1°C by a thermal feedback device.
Analyses
The kinetics of \(\dot{V}\hbox{O}_{2},\) FBF, HR and O2-pulse (calculated from \(\dot{V}\hbox{O}_{2}/\hbox{HR}\)) during the repeated bout exercise were time-interpolated second by second, and averaged across each transition for each subject. Response parameters were obtained from the following range of analyses. Initially, the mean response time of \(\dot{V}\hbox{O}_{2}\) and O2-pulse kinetics was estimated by the “effective” time constant (τ′) using a monoexponential fit to the entire response (but excluding the first 20 s after the onset of exercise: phase I; e.g., Endo et al. 2004; Fukuba et al. 2004; Whipp et al. 1982). For HR and FBF the entire response was considered (although for HR, to avoid negative time delays (Td), the Td was fixed at exercise onset; 0 s). The monoexponential model was used to broadly describe the response kinetics and was fitted to the responses expressed as:
where f (t) represents variable value at time t ; BL is the baseline value of each variable at 10 W averaged from the last min prior to exercise, and A, Td, and τ′ are the amplitude, time delay and effective time constant parameters of the exponential response, respectively. However, there is known to be a bias in the \(\dot{V}\hbox{O}_{2}\) residual using mono exponential modeling when a delayed slow component of \(\dot{V}\hbox{O}_{2}\) is expressed during supra-LT exercise (e.g., Barstow and Molé 1991; Casaburi et al. 1989), therefore, where eqn 1 did not adequately describe the response kinetics, the \(\dot{V}\hbox{O}_{2},\) FBF and O2-pulse responses were also fitted to an exponential model (Eq. 1) that was limited to the primary phase (e.g., Rossiter et al. 2002) and beginning after at least 20 s, excluding the phase I duration (e.g., \(\hbox{f (t)} = \hbox{BL} + \hbox{A}_{\rm p} \cdot \left[1 - e^{{-({\rm t} - {\rm Tdp})/\tau {\rm p}}}\right];\) where the subscript ‘p’ denotes parameters of the primary component). Here, the fitting window was iteratively reduced (from end exercise toward the onset) until the residuals failed to demonstrate a consistent bias. The fitting was performed using a nonlinear regression technique (i.e., Marquardt-Levenberg Algorithm in Sigma Plot 2000, Jandel Scientific). The amplitude of slow component was calculated by the difference between the extrapolated Ap and the actual end-exercise amplitude (Δ EE)—the latter being calculated from the difference between BL and the average of the last 30s of each exercise bout. The primary component (Ap) was expressed as the relative gain (Ap/Δ W). The ratio of the slow component to the primary amplitude [(Δ EE−Ap)/Ap*100] was defined as the index of slow component. Femoral vascular conductance (FVC) was calculated from FBF/MAP throughout the repeated exercise bouts.
Statistical treatments
Values are expressed as mean ± SD. Since the estimated parameters and variables were found to be of normal distribution, the differences between first and second bouts were examined by the Student’s paired-comparison t test. Pearson product–moment correlation coefficients were used to evaluate relationships between two variables or parameters. The time-serial change of variables (every 20-s average) was tested with respect to the differences between first and second bout by repeated measures ANOVA with time (SPSS for Windows, SPSS Inc). When a significant difference was detected, this was further examined by Tukey’s post-hoc test. Statistical significance was accepted at P<0.05.
Results
The mean value of \(\dot{V}\hbox{O}_{2}\hbox{peak}\) during incremental exercise to the limit of tolerance was 1097±239 ml.min−1 and the LT was estimated at 657±98 ml.min−1 or 61±7% of \(\dot{V}\hbox{O}_{2}\hbox{peak}.\)
During heavy-intensity bilateral KE exercise the \(\dot{V}\hbox{O}_{2}\) response was found to be better characterized by limiting the fit to the primary phase (phase II) than by a monoexponential fit to the entire response (Fig. 1a, 2a). However, this approach did not improve the ‘goodness of fit’ for the FBF response of all subjects. Subsequently, the FBF was fitted to the same region of time (less the approximate limb-to-lung transit delay) as the phase II \(\dot{V}\hbox{O}_{2}.\) In this way we were able to discern a FBF ‘slow component’, however, its magnitude was consistently less than that for \(\dot{V}\hbox{O}_{2}\) (Table 1).
The time course of pulmonary oxygen uptake (a), femoral arterial blood flow (b) and O2-pulse (c) responses during repeated bout heavy knee extensor exercise in a representative subject. The right-hand panels show the superimposition of the average of multiple repetitions of each variable. Solid curves (left-hand panels) indicate the model estimation for \(\dot{V}\hbox{O}_{2}\) and FBF (primary parameters with extrapolation to end exercise) or O2 pulse (monoexponential). The residuals between the model and response are shown at the bottom of each panel. For (a and b) the residuals (solid circles) indicate the residuals to the phase II fit, whereas the open circles are residuals to the extrapolated exponential. They demonstrate a systematic bias in bout 1 that is reduced in bout 2
The superimposition of the pulmonary oxygen uptake (a) and femoral arterial blood flow (b) responses to repeated bouts of heavy-intensity exercise of the entire group (n=7). Values are averaged every 20 s. Error bars are mean ± SD. bout 1; closed circle, bout 2; open circle. +Significant difference between bout 1 and bout 2 (P<0.05)
Temporal profile and kinetics of \(\dot{V}\hbox{O}_{2}\) and FBF responses
An example of the \(\dot{V}\hbox{O}_{2}\) and FBF response profiles to the repeated heavy intensity square-wave protocol in a representative subject is shown in Fig. 1a and 1b. The effective \(\dot{V}\hbox{O}_{2} \tau^{\prime}\) was significantly reduced by prior heavy KE exercise (bout 1: 61.0±10.5 vs. bout 2: 51.6±9.0 s; Table 1). In contrast, while the FBF manifest a lower τ′ (P<0.05) compared to \(\dot{V}\hbox{O}_{2}\) in both bouts, the FBF τ′ was the same between bouts; indeed, FBF τ′ did not show a decrease during bout 2, as hypothesized (bout 1: 28.2±12.0 vs. bout 2: 34.2±8.5 s; P>0.05; Table 1). The primary \(\dot{V}\hbox{O}_{2} \tau_{p}\) was not significantly different between bouts (\(\dot{V}\hbox{O}_{2}\): bout 1: 38.2±11.7, bout 2: 36.4±8.0 S; Table 1). Moreover, the FBF τ p was similar between bouts (FBF: bout 1: 19.8±8.1, bout 2: 23.8±5.1 s; Table 1) and was consistently lower than \(\dot{V}\hbox{O}_{2} \tau_{p}\) (the same as for τ′). Figure 2 shows the group mean \(\dot{V}\hbox{O}_{2}\) and FBF responses superposed for bouts 1 and 2. The only difference in FBF between bouts was a relative hyperemia prior to bout 2 [FBF being increased ∼17% (from 1578±308 to 1844±306 ml·min−1), during the 10W-baseline], the absolute FBF remaining identical during the transient of both bouts. Consistent with this, femoral vascular conductance (FVC) prior to bout 2 was also increased. However, again similar to FBF, during exercise there were no statistical differences in FVC between the repeated bouts (the group means are shown in Fig. 3).
The relative pre-exercise hyperemia in bout 2 (compared to bout 1) was not associated with an alteration in the primary\(\dot{V}\hbox{O}_{2} \tau_{p},\) which was not significantly different between bouts (Table 1); the predominant reduction in effective τ′ being a result of a significantly (P<0.05) reduced slow component (bout 1: 16.0±8.0, bout 2: 12.5±6.7 %; Table 1). The FBF slow component, however, was unchanged between bouts (bout 1: 6.7±5.7, bout 2: 7.4±6.3 %; Table 1). Furthermore, the magnitude of the FBF slow component was significantly smaller than \(\dot{V}\hbox{O}_{2}\) in every case (P<0.05). The \(\dot{V}\hbox{O}_{2}\) response was manifest from a small (∼4.5%) but significantly increased pre-exercise baseline (305±23 vs. 319±25 ml.min−1 ; Table 1): The interplay between the baseline and kinetic phases of \(\dot{V}\hbox{O}_{2}\) resulted in a similar end-exercise value in both bouts (Table 1).
Temporal profile and kinetics of HR and O2-pulse
Notably unlike FBF, HR kinetics (τ′) tended to be slowed by prior exercise (bout 1: 56.3±8.9, bout 2: 73.3±17.6 s; Table 2), although this did not reach statistical significance (P=0.06). And, while both the baseline and end-exercise HR values were significantly higher for bout 2, the amplitude of the HR response was unaltered (Table 2). Despite the increased HR τ′, prior heavy KE exercise significantly speeded the O2-pulse response. A typical example of the O2-pulse profile during repeated heavy intensity exercise is shown in Fig. 1 C and group mean HR and O2-pulse responses for bout 1 and 2 are superimposed in Fig. 4a, 4b. Both estimates of the kinetics of O2-pulse (τ′ and τ p ) were significantly lower during the second bout compared with the first (bout 1: 38.0±11.6 and 31.7±14.0 s, bout 2: 30.6±10.8 and 29.6±14.7 s for τ′ and τ p , respectively; Table 2), with a small (0.1 ml.min−1 .beat−1, on average) but statistically significant increase in amplitude (Table 2).
The superimposition of the heart rate (a) and O2-pulse (b) responses to repeated bouts of heavy-intensity exercise of the entire group (n=7). Values are averaged every 20 s. Error bars are mean ± SD. bout 1; closed circle, bout 2; open circle. +Significant difference between bout 1 and bout 2 (P<0.05)
Kinetic association of \(\dot{V}\hbox{O}_{2}\) and FBF
Figure 5 shows the association of \(\dot{V}\hbox{O}_{2}\) arising from the exercising musculature (\(\Delta \dot{V}\hbox{O}_{2};\) after correction for the phase II delay time between variables) and the limb blood flow (Δ FBF; expressed here as the group mean of twice the ‘one-leg’ FBF). The dynamic profiles of \(\dot{V}\hbox{O}_{2}\) and FBF manifest relative differences depending on the bout number, whereas the \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) between the two exercise bouts were not significantly different, despite a tendency for \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) to be higher in the primary phase of bout 2.
Superimposed responses of \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF}\) during repeated heavy-intensity exercise in seven subjects. \(\Delta \dot{V}\hbox{O}_{2}\) is measured from the increment of \(\dot{V}\hbox{O}_{2}\) above the baseline (10 W exercise) value. \(\Delta \dot{V}\hbox{O}_{2}\) is expressed relative to the increment in FBF (Δ FBF; expressed here as twice the ‘one-leg’ FBF) after correction for the phase II delay time. \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF},\) therefore, is reflective of exercising muscle (a–v) O2 difference (see discussion) . Values are averaged every 20 s. Error bars are mean ± SD. bout 1; closed circle, bout 2; open circle
Discussion
The salient features of the present study were that: (1) the mean response time of the \(\dot{V}\hbox{O}_{2}\) response (reflecting the overall rate of \(\dot{V}\hbox{O}_{2}\) adaptation) was reduced following prior heavy-intensity exercise; (2) this was due to a significant reduction in the slow component amplitude and not a result of a reduced \(\dot{V}\hbox{O}_{2} \tau_{p},\) (3) pre-exercise FBF was increased prior to bout 2, however, the kinetics of the FBF response were identical during both bouts of heavy-intensity dynamic KE exercise (Table 1). These findings suggest that a residual hyperemia, consequent to prior high-intensity exercise, did not lead to either a faster adaptation of FBF or \(\dot{V}\hbox{O}_{2}\) during subsequent heavy intensity-exercise. The reduced \(\dot{V}\hbox{O}_{2}\) slow component during bout 2, which has been suggested to result from reduced acidosis and/or fatigue during bout 2 (Rossiter et al. 2001), however, was not a result of improved bulk BF or O2-delivery to the exercising muscles. If an improvement in FBF was required to bring about an alteration in \(\dot{V}\hbox{O}_{2}\) kinetics then the FBF response dynamics in bout 2 would be expected to be altered to allow better maintenance of \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF}\)—an event that was not observed in the present study (Fig. 5).
Baseline FBF
It has previously been suggested (Gerbino et al. 1996; MacDonald et al. 1998, 2001) that the speeded \(\dot{V}\hbox{O}_{2}\) dynamics during bout 2 of repeated heavy-intensity exercise may be due to improved muscle blood flow (and, therefore, O2 delivery) consequent to residual vasodilatory effects of the metabolic acidaemia. MacDonald et al. (2001) demonstrated that the muscle blood flow was elevated at exercise onset by a prior heavy-intensity hand grip exercise, consistent with the notion of improved O2-delivery during bout 2 and removal of a putative bulk O2 limitation to the kinetic \(\dot{V}\hbox{O}_{2}\) response. This was also the case in the present study, with both the pre-exercise FBF baseline and FVC being significantly raised prior to exercise onset. However, while the baseline FBF following heavy-intensity exercise was increased, this did not result in an alteration of the FBF kinetics. The FBF in the initial seconds after exercise onset was the same in both exercise bouts. The raised baseline FBF, therefore, may be beneficial (and necessary) in removing metabolic waste products following exercise, but FBF was both: (1) appropriate, considering the slightly raised \(\dot{V}\hbox{O}_{2}\) baseline, and (2) not augmented in the subsequent exercise bout. It has previously been demonstrated that prior severe-intensity KE exercise (i.e., a greater intensity than that used in the present study; Bangsbo et al. 2001; Krustrup et al. 2001) can lead to increases in baseline FBF that are sustained during the subsequent transient, and that this is associated with a reduced QO2 τ′. The present data differ, however, in that they suggest that increased blood flow prior to exercise does not, by necessity, lead to improved exercise blood flow.
The ‘phase II’ response
In the present study the phase II \(\dot{V}\hbox{O}_{2} \tau_{p}\) response (i.e., the portion of the \(\dot{V}\hbox{O}_{2}\) response which correlates well with QO2 kinetics; Grassi et al. 1996) was, unexpectedly unaltered by prior heavy-intensity exercise. Previous studies using prior-exercise and the KE modality have frequently led to a reduction in \(\dot{V}\hbox{O}_{2} \tau_{p}\) (Yoshida et al. 1995; Hughson et al. 2003; Fukuba et al. 2004; Rossiter et al. 2001; Paterson et al. 2005), whereas typically investigations using cycle ergoemetry find prior-exercise-induced changes are limited to the slow component region (e.g., Burnley et al. 2000, 2002; Endo et al. 2003, 2004; Gerbino et al. 1996; Koppo and Bouckaert 2000; Wilkerson et al. 2004). The distinction between KE and cycle erogometry, therefore, may be of paramount importance in this regard, as suggested by Shoemaker et al. (1994) and Hoelting et al. (2001) among others (Wilkerson et al. 2004).
It is likely that high intramuscular forces required during such a weight-lifting style KE exercise (or exercise requiring high contraction frequencies) result in a significant blood flow limitation during the exercise itself. Previous observations from our laboratory (Fukuba et al. 2004) have shown a reduction in the \(\dot{V}\hbox{O}_{2} \tau_{p}\) using a weight-lifting style model. However, this approach was associated with both: (1) high kinetic parameters ( \(\dot{V}\hbox{O}_{2} \tau_{p} \sim 50\,\hbox{s};\) and functional gain \((\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{W}) \sim 20\,\hbox{ml}.\min^{-1}.\hbox{W}^{-1})\) compared to those typically seen during cycle ergometry in healthy subjects (e.g., ∼25–35 s; ∼10±1 ml.min−1 .W−1), and (2) a dramatic hyperemia on the cessation of exercise; FBF increasing by almost twofold immediately on cessation of muscle contractions (see Fig.1 in Fukuba et al. 2004), which was not the case in the present study (Fig. 1b). More recently, Paterson et al. (2005) have also investigated FBF and \(\dot{V}\hbox{O}_{2}\) kinetics during single leg KE exercise using a cycle ergometer to achieve the work rate, although they found that prior exercise did indeed induce a reduction in \(\dot{V}\hbox{O}_{2} \tau_{p}.\) In their study the exercise was associated with a functional gain of ∼15 ml.min−1 .W−1 and a large post-exercise hyperemia, whereas in the present study these values (τ p ∼36 s and primary gain ∼12 ml.min−1 .W−1) were more similar to those associated with cycle ergometry, and the end-exercise hyperemic response was only ∼5% greater (3825±526 vs. 4025±676 ml.min−1 ; average of 5 s preceding and following exercise cessation in bout 1) than the end-exercise value (see Figure 1). We believe that these subtle, but potentially important, differences may partly explain the divergence of the results found, and support the notion that exercise resulting in lower intramuscular forces than those seen during weight-lifting style KE (and, therefore, closer to those seen in cycle ergometry; see Hoelting et al. 2001; Radegran and Saltin 1998; Shoemaker et al. 1994 for discussion), may allow blood flow responses to be less-impeded by mechanical constraints, and the physiological determinants to predominate.
We hypothesized that prior heavy-intensity KE exercise would lead to a reduction in \(\dot{V}\hbox{O}_{2} \tau_{p},\) as is typically the case for KE exercise (Yoshida et al. 1995; Rossiter et al. 2001; Hughson et al. 2003; Paterson et al. 2005), and that this reduction may be a result of ‘improved’ FBF kinetics. However, as this ‘cycle-like’ exercise mode did not alter \(\dot{V}\hbox{O}_{2} \tau_{p}\) between bouts, we cannot accept or reject the hypothesis that FBF limits O2 availability during the phase II response during heavy-intensity KE exercise. The data do suggest, however, that if a blood flow limitation were to manifest during bout 1, it does not appear to be relieved by prior heavy-intensity exercise, as was previously suggested Gerbino et al. (1996), and is in agreement with the results of Paterson et al. (2005). The absence of an alteration in any phase of the FBF kinetics, however, does have important implications for the \(\dot{V}\hbox{O}_{2}\) slow component.
The ‘slow’ component
Alleviation of the \(\dot{V}\hbox{O}_{2}\) slow component during bout 2 of repeated heavy-intensity exercise was a characteristic of the present study (similar to previous observations during cycle ergometry e.g., Burnley et al. 2000; Gerbino et al. 1996; Koppo and Bouckaert 2000; MacDonald et al. 1998). However, contrary to our hypothesis, the reduced slow component was not associated with an alteration of the kinetics of FBF during KE exercise. While FBF did show evidence of a ‘slow’ component (Fig. 1b), it was consistently less than the magnitude of the \(\dot{V}\hbox{O}_{2}\) slow component, by about 50%. This suggests that FBF rises rapidly at exercise onset (compared to \(\dot{V}\hbox{O}_{2}\)) and attains a level that allows adequate bulk O2-delivery—this being supplemented, on some occasions, by a small FBF slow component. The bulk FBF is unlikely to be limiting to \(\dot{V}\hbox{O}_{2}\) during this region, otherwise the \(\dot{V}\hbox{O}_{2}\) slow component would not be expressed. The studies of Bangsbo et al. (2001) and Krustrup et al. (2001) clearly show that both FBF, (as well as O2-extraction and QO2) can be increased by prior severe-intensity exercise, however, the present data differ as they show that increases in FBF are not obligatory to reduce the \(\dot{V}\hbox{O}_{2}\) response magnitude during this phase. Thus, the degree of reduction in the \(\dot{V}\hbox{O}_{2}\) slow component by prior exercise may be intensity-dependent (a greater ‘priming’ intensity leading to a greater reduction in the \(\dot{V}\hbox{O}_{2}\) slow component; Bangsbo et al. 2001; Endo et al. 2004; Krustrup et al. 2001) and it does not seem to be exclusively mediated via a bulk blood flow-related mechanism.
Determinants of \(\dot{V}\hbox{O}_{2}\) kinetics during repeated heavy-intensity exercise
The present findings, therefore, are consistent with the notion that the reduction in the \(\dot{V}\hbox{O}_{2}\) slow component during heavy-intensity exercise following prior heavy exercise is due to factors more proximal to the exercising muscle than those measured here. Reductions in both the \(\dot{V}\hbox{O}_{2} \tau_{p}\) and the magnitude of the \(\dot{V}\hbox{O}_{2}\) slow component are manifested during KE exercise (Fukuba et al. 2004; Rossiter et al. 2003; Paterson et al. 2005), whereas cycle ergometry (Burnley et al. 2000; Gerbino et al. 1996; MacDonald et al. 1997) typically expresses a more limited facilitation, and therefore, it was surprising that \(\dot{V}\hbox{O}_{2} \tau_{p}\) was not reduced in the present study. The ratio of BF to QO2 is thought to be higher in KE than cycling (Radegran and Saltin 1998) and, therefore, KE exercise might be expected to less likely result in any modulation of the \(\dot{V}\hbox{O}_{2}\) response if a limiting BF was the cause of this modulation (as long as the exercise mode or intensity did in itself not limit BF). However, the opposite is more typically the case, which suggests that a mechanism other than BF is likely to be operating to reduce \(\dot{V}\hbox{O}_{2} \tau_{p}\) or the \(\dot{V}\hbox{O}_{2}\) slow component, during KE exercise at least. There is now a considerable amount of work suggesting that experimental impositions to increase or limit muscle blood flow (or O2 delivery) do not lead to alterations in the \(\dot{V}\hbox{O}_{2}\) response kinetics (e.g., Grassi et al. 2000; Williamson et al. 1996; MacDonald et al. 1997; Endo et al. 2003; Koga et al. 1997). It would seem, therefore, that alterations in \(\dot{V}\hbox{O}_{2}\) kinetics at this intensity may result from alterations more proximal to skeletal muscle metabolism (e.g., Rossiter et al. 2001; Rossiter et al. 2003; Howlett and Hogan 2003). While O2 delivery clearly has the potential to limit \(\dot{V}\hbox{O}_{2}\) kinetics (MacDonald et al. 1998; Perrey et al. 2001) it seems that this is typically not the case, at least during moderate or heavy-intensity exercise (present data; Paterson et al. 2005).
These data, as well as those of others, however, cannot account for the heterogeneity of microvascular QO2/BF matching. It is possible that, while bulk FBF is adequate, local QO2/BF (determining intracellular PO2) may be limiting in some areas of the exercising musculature. Recently, Krustrup et al. (2004) have shown that the \(\dot{V}\hbox{O}_{2}\) slow component is associated with a widening spread of glycogen utilization, suggesting an increasing contribution to force production from ‘O2-inefficient’ fibers and anaerobic glycolysis during the slow component region. This provides the potential for a progressive reduction in QO2/BF at least in some spatially dispersed muscle regions. It seems, therefore, that heterogeneous bioenergetic contributions to power production might indeed be the source of the \(\dot{V}\hbox{O}_{2}\) slow component, similar to suggestions by Poole and colleagues (1994). However, while the range of QO2/BF in the exercising muscle remains poorly understood, Mizuno et al (2003) have shown (using positron emission tomography) that regional QO2/BF appears to be well matched. This is, somewhat, contrary to measurements of deoxy-hemoglobin and/or myoglobin (using near-infra-red spectroscopy; e.g., DeLorey et al. 2004; Gurd et al. 2005) that suggest that QO2/BF may be better maintained during the second bout of repeated exercise, despite the suggestion that a greater portion of FBF is directed to the skin (Nielsen et al. 1988) during repeated exercise (which would be expected to further limit QO2/BF matching in bout 2). Together, this suggests that the distribution of BF may be a critical factor for understanding the determinants of the \(\dot{V}\hbox{O}_{2}\) slow component. It may be the case, for example, that a re-distribution of muscle blood flow in bout 2 compared to bout 1, could better protect the muscle from fatigue, by allowing more rapid clearance of fatigue inducing metabolites or better maintenance of local QO2/BF. It is important to note, therefore, that either intramuscular (such as muscle and fiber-type recruitment patterns, e.g., Barstow et al. 1996; Burnley et al. 2000; Pringle et al. 2003; Saunders et al. 2000) or BF-related events occurring during the primary phase, may yet have important consequences for the manifestation of the \(\dot{V}\hbox{O}_{2}\) slow component. These issues, however, remain to be resolved.
Indices of \(\dot{V}\hbox{O}_{2}\) to blood flow matching
Yoshida and Whipp (1995) have suggested that although \(\tau^{\prime} \dot{V}\hbox{O}_{2}/\tau^{\prime}\hbox{BF}\) may be greater than 1.0 (as was consistently the case in the present study), it is the absolute QO2/BF ratio (and, subsequently, QO2/microvascular flow) that determines adequate (or not) tissue oxygenation. For whole body exercise, the muscle \(\dot{V}\hbox{O}_{2}\)-to-blood-flow dynamic relationship can be used to estimate the arterio–venous O2 content difference (Yoshida and Whipp 1995); in the present study we used \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF}\) to estimate the (a–v)O2 manifest above the 10 W baseline exercise. During the first 20 s of the repeated exercise bouts the \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) averaged ∼0.075 and ∼0.08, for bout 1 and bout 2, respectively. Thus, the value of \(\Delta \dot{V}\hbox{O}_{2}/\Delta\hbox{ FBF}\) in this first 20-s period in the present study likely reflects only a small decrease or even maintenance of C v O2 during the initial seconds of both exercise bouts (consistent with previous studies; Bangsbo et al. 2000; Grassi et al. 1996). Similarly, Behnke et al. (2002) demonstrated the maintenance of microvascular PO2 (PO2m) early in the exercise transient of stimulated rat spinostrapezious muscle, suggesting adequate O2 availability during this period. Similar demonstrations by Hogan (2001) in the intracellular PO2 profile of the single frog myocyte and of the muscle oxygenation profile in humans (Grassi et al. 2003) also support this notion. These are all consistent with the present findings. In fact, in our study \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) did not surpass the 0.1 (a–v)O2 isopleth until ∼40 s after exercise onset (Fig. 5), e.g., only a moderate reduction in C V O2(Stringer et al. 1997).
The relatively slow kinetic response of HR during the second exercise bout was associated with a significantly faster increase in O2-pulse. At the whole-body level this suggests that either (a–v)O2 difference or stroke volume (or both) was ‘improved’ early during the second exercise transient. Assuming a negligible alteration in stroke volume during bout 2 in our semi-supine modality (De Cort et al. 1991; Yoshida et al. 1993; Gledhill et al. 1994), then the O2-pulse profile would suggest that (a–v)O2 difference increased more rapidly during bout 2. While there was a tendency (P>0.05) for the dynamics of \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) to be more rapid during bout 2, this was not a consistent finding. Therefore, the O2-pulse τ′ may reflect a reduced mean circulation time and/or be reflective of increased QO2 early in the second exercise transient (e.g., reduced QO2 τ). While this distinction could not be achieved within the precision of the current techniques (which are, by definition, estimates) the O2-pulse profile is, at least, not inconsistent with an improvement of O2-extraction during bout 2.
Limitations
The direct measurement of QO2 during exercise in human subjects is technically challenging (Bangsbo et al. 2000; Whipp et al. 1995), especially in our subject population of Japanese women where the overall amplitude of FBF and QO2 responses is expected to be small (with a maximal cardiac output of ∼14 l/min; unpublished observations). We were, therefore, unable to make direct QO2 measurements, but instead relied upon the relevant phases of pulmonary \(\dot{V}\hbox{O}_{2}\) dynamics (phases 2 and 3) to make inferences regarding the exercising muscle. Under normal conditions in healthy subjects primary \(\dot{V}\hbox{O}_{2}\) kinetics are likely to cohere to those of QO2 by +/-10% (Barstow et al. 1991), and these have been shown to be virtually indistinguishable during moderate cycle ergometry (Grassi et al. 1996). Similarly, Poole et al. (1991) demonstrated that ∼80–90 % of the magnitude of the \(\dot{V}\hbox{O}_{2}\) slow component response is reflected within the leg QO2. While, we cannot be certain that the \(\dot{V}\hbox{O}_{2}\) kinetics measured here adequately reflect intramuscular events, it seems likely that they provide a reasonable and reliable proxy from which to draw salient conclusions regarding the control and/or limitation of skeletal muscle oxidative phosphorylation. The present study is, therefore, in accordance with many previous suggestions that under normal conditions muscle QO2 responses are likely to be controlled by factor(s) within the exercising limbs rather than O2 delivery (e.g., Campbell-O’Sullivan et al. 2002; Chance et al. 1986; Howlett and Hogan 2003; Jones et al. 2004; Mahler 1985; Timmons et al. 1998). However, under more extreme conditions (such as hypoxia or possibly even during severe exercise) O2 delivery has the potential to be a limiting factor (Engelen et al. 1996; Grassi et al. 2000).
Conclusion
In summary, the unexpected finding that \(\dot{V}\hbox{O}_{2} \tau_{p}\) which was not altered by prior heavy-intensity KE exercise did not allow us to refute the suggestion that bulk O2-delivery is limiting factor to the primary \(\dot{V}\hbox{O}_{2}\) kinetic responses during repeated heavy-intensity exercise. However, the reduction in the \(\dot{V}\hbox{O}_{2}\) slow component following prior heavy-intensity exercise was not accompanied by an alteration in FBF kinetics during the transient, suggesting that although \(\tau^{\prime}\dot{V}\hbox{O}_{2}/ \tau^{\prime}\hbox{FBF}\) remained greater than 1.0 (Yoshida and Whipp 1995) throughout both exercise bouts, increases in FBF (and therefore O2-delivery) were not required to manifest a reduced \(\dot{V}\hbox{O}_{2}\) slow component during bout 2; the contour of \(\Delta \dot{V}\hbox{O}_{2}/\Delta \hbox{FBF}\) was maintained between bouts. Rather, these data implicate mechanisms that are more proximally related to the intramuscular event(s) within exercising muscles in mediating this phenomenon.
References
Andersen P, Adams RP, Sjogaard G, Thorboe A, Saltin B (1985) Dynamic knee extension as model for study of isolated exercising muscle in humans. J Appl Physiol 59:1647–1653
Bangsbo J, Krustrup P, Gonzalez-Alonso J, Boushel R, Saltin B (2000) Muscle oxygen kinetics at onset of intense dynamic exercise in humans. Am J Physiol 279:R899–R906
Bangsbo J, Krustrup P, Gonzalez-Alonso J, Saltin B (2001) ATP production and efficiency of human skeletal muscle during intense exercise:effect of previous exercise. Am J Physiol 280:E956–E964
Barstow TJ and Molé PA (1991) Linear and non-linear characteristics of oxygen uptake kinetics during heavy exercise. J Appl Physiol 71:2099–2106
Barstow TJ, Jones AM, Nguyen PH, Casaburi R (1996) Influence of muscle fiber type and pedal frequency on oxygen uptake kinetics of heavy exercise. J Appl Physiol 81:1642–1650
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60:2020–2027
Behnke BJ, Kindig CA, Musch TI, Sexton WL, Poole DC (2002) Effects of prior contractions on muscle microvascular oxygen pressure at onset of subsequent contractions. J Physiol 539:927–934
Burnley M, Jones AM, Carter H, Doust JH (2000) Effects of prior heavy exercise on phase II pulmonary oxygen uptake kinetics and the slow component during heavy exercise. J Appl Physiol 89:1387–1396
Burnley M, Doust JH, Ball D, Jones AM (2002) Effects of prior heavy exercise on \(\dot{V}\hbox{O}_{2}\) kinetics during heavy exercise are related to changes in muscle activity. J Appl Physiol 93:167–174
Campbell-O’Sullivan SP, Constantin-Teodosiu D, Peirce N, Greenhaff PL (2002) Low intensity exercise in humans accelerates mitochondrial ATP production and pulmonary oxygen kinetics during subsequent more intense exercise. J Physiol 538:931–939
Casaburi R, Barstow TJ, Robinson T, Wasserman K (1989) Influence of work rate on ventilatory and gas exchange kinetics. J Appl Physiol 67:547–555
Chance B, Leigh JS Jr, Kent J, McCully K, Nioka S, Clark BJ, Maris JM, Graham T (1986) Multiple controls of oxidative metabolism in living tissues as studied by phosphorus magnetic resonance. Proc Natl Acad Sci USA: 83
De Cort SC, Innes JA, Barstow TJ, Guz A (1991) Cardiac output, oxygen consumption and arteriovenous oxygen difference following a sudden rise in exercise level in humans. J Physiol 441:501–512
DeLorey DS, Kowalchuk JM, Paterson DH (2004) Effects of prior heavy-intensity exercise on pulmonary O2 uptake and muscle deoxygenation kinetics in young and older adult humans. J Appl Physiol 97:998–1005
Endo M, Tauchi S, Hayashi N, Koga S, Rossiter HB, Fukuba Y (2003) Facial cooling-induced bradycardia does not slow pulmonary \(\dot{V}\hbox{O}_{2}\) kinetics at the onset of high-intensity exercise. J Appl Physiol 95:1623–31
Endo M, Usui S, Fukuoka Y, Miura A, Rossiter HB, Fukuba Y (2004) Effects of priming exercise intensity on the dynamic linearity of the pulmonary \(\dot{V}\hbox{O}_{2}\) response during heavy exercise. Eur J Appl Physiol 91:545–554
Engelen M, Porszasz J, Riley M, Wasserman K, Maehara K, Barstow TJ (1996) Effects of hypoxic hypoxia on O2 uptake and heart rate kinetics during heavy exercise. J Appl Physiol 81:2500–2508
Fukuba Y, Ohe Y, Miura A, Kitano A, Endo M, Sato H, Miyachi M, Koga S, Fukuda O (2004) Dissociation between the time courses of femoral artery blood flow and pulmonary \(\dot{V}\hbox{O}_{2}\) during repeated bouts of heavy knee extension exercise in humans. Exp Physiol 89:243–253
Gerbino A, Ward SA, Whipp BJ (1996) Effects of prior exercise on pulmonary gas-exchange kinetics during high-intensity exercise in humans. J Appl Physiol 80:99–107
Gledhill N, Cox D, Jamnik R (1994) Endurance athletes’ stroke volume does not plateau:major advantage is diastolic function. Med Sci Sports Exerc 26(9):1116–1121
Grassi B, Poole DC, Richardson RS, Knight DR, Erickson BK, Wagner PD (1996) Muscle O2 uptake kinetics in humans:implications for metabolic control. J Appl Physiol 80:988–998
Grassi B, Hogan MC, Kelley KM, Aschenbach WG, Hamann JJ, Evans RK, Patillo RE, Gladden LB (2000) Role of convective O2 delivery in determining \(\dot{V}\hbox{O}_{2}\) on-kinetics in canine muscle contracting at peak \(\dot{V}\hbox{O}_{2}.\) J Appl Physiol 89:1394–1301
Grassi B, Pogliaghi S, Rampichini S, Quaresima V, Ferrari M, Marconi C, Cerretelli P (2003) Muscle oxygenation and pulmonary gas exchange kinetics during cycling exercise on-transitions in humans. J Appl Physiol 95:149–158
Gurd JB, Scheuermann BW, Paterson DH, Kowalchuk JM (2005) Prior heavy-intensity exercise speeds \(\dot{V}\hbox{O}_{2}\) kinetics during moderate-intensity exercise in young adults. J Appl Physiol 98:1371–1378
Hoelting BD, Scheuermann BW, Barstow TJ (2001) Effect of contraction frequency on leg blood flow during knee extension exercise in humans. J Appl Physiol 91:671–679
Hogan MC (2001) Fall in intracellular PO2 at the onset of contractions in Xenopus single skeletal muscle fibers. J Appl Physiol 90:1871–1876
Howlett RA and Hogan MC (2003) Dichloroacetate accelerates the fall in intracellular PO2 at onset of contractions in Xenopus single muscle fibers. Am J Physiol 284:R481–R485
Hughson RL, Tschakovsky ME, Houston ME (2001) Regulation of oxygen consumption at the onset of exercise. Exerc Sport Sci Rev 29:129–133
Hughson RL, Schijvens H, Burrows S, Devitt D, Betik AC, Hopman MTE (2003) Blood flow and metabolic control at the onset of heavy exercise. Int J Sport and Health Science 1:1–10
Jones AM, Wilkerson DP, Wilmshurst S, Campbell IT (2004) Infuluence of L-NAME on pulmonary O2 uptake kinetics during heavy intensity cycle exercise. J Appl Physiol 96:1033–1038
Koga S, Shiojiri T, Kondo N, Barstow TJ (1997) Effect of increased muscle temperature on oxygen uptake kinetics during exercise. J Appl Physiol 83:1333–1338
Koppo K, Bouckaert J (2000) In human the oxygen uptake slow component is reduced by prior exercise of high as well as low intensity. Eur J Appl Physiol 83:559–565
Krustrup P, Gonzalez-Alonso J, Quistorff B and Bangsbo J (2001) Muscle heat production and anaerobic energy turnover during repeated intense dynamic exercise in humans. J Physiol 536:947–956
Krustrup P, Soderlund K, Mohr M, Bangsbo J (2004) The slow component of oxygen uptake during intense, sub-maximal exercise in man is associated with additional fibre recruitment. Pflugers Arch 447:855–866
MacDonald M, Pedersen PK, Hughson RL (1997) Acceleration of \(\dot{V}\hbox{O}_{2}\) kinetics in heavy submaximal exercise by hyperoxia and prior high-intensity exercise. J Appl Physiol 83:1318–1325
MacDonald MJ, Shoemaker JK, Tschakovsky ME, Hughson RL (1998) Alveolar oxygen uptake and femoral artery blood flow dynamics in upright and supine leg exercise in humans. J Appl Physiol 85:1622–1628
MacDonald MJ, Naylor HL, Tschakovsky ME, Hughson RL (2001) Peripheral circulatory factors limit rate of increase in muscle O2 uptake at onset of heavy exercise. J Appl Physiol 90:83–89
Mahler M (1985) First-order kinetics of muscle oxygen consumption, an equivalent proportionality between QO2 and phosphorylcreatine level. Implications for the control of respiration. J Gen Physiol 86:135–165
Mizuno M, Kimura Y, Iwakawa T, Oda K, Ishii K, Ishiwata K, Nakamura Y, Muraoka I (2003) Regional differences in blood flow and oxygen consumption in resting muscle and their relationship during recovery from exhaustive exercise. J Appl Physiol 95:2204–2210
Nielsen HV, Staberg B, Nielsen K, Sejrsen P (1988) Effects of dynamic leg exercise on subcutaneous blood flow rate in the lower limb of man. Acta Physiol Scand 134:513–518
Paterson ND, Kowalchuk JM, Paterson DH (2005) Effects of prior heavy-intensity exercise during single-leg knee-extension on \(\dot{V}\hbox{O}_{2}\) kinetics and limb blood flow. J Appl Physiol 99:683–690
Perrey S, Tschakovsky ME, Hughson RL (2001) Muscle chemoreflex elevates muscle blood flow and O2 uptake at exercise onset in nonischemic human forearm. J Appl Physiol 91:2010–2016
Poole DC, Schaffartzik W, Knight DR, Derion T, Kennedy B, Guy HJ, Prediletto R, Wagner PD (1991) Contribution of excising legs to the slow component of oxygen uptake kinetics in humans. J Appl Physiol 71:1245–1260
Poole DC, Barstow TJ, Gaesser GA, Willis WT, Whipp BJ (1994) \(\dot{V}\hbox{O}_{2}\) slow component:physiological and functional significance. Med Sci Sports Exerc 26:1354–1358
Pringle JS, Doust JH, Carter H, Tolfrey K, Campbell IT, Jones AM (2003) Oxygen uptake kinetics during moderate, heavy and severe intensity “submaximal” exercise in humans: the influence of muscle fibre type and capillarisation. Eur J Appl Physiol 89:289–300
Radegran G, Saltin B (1998) Muscle blood flow at onset of dynamic exercise in humans. Am J Physiol 274:H314–H322
Rossiter HB, Ward SA, Doyle VL, Howe FA, Griffths JR, Whipp BJ (1999) Inferences from pulmonary O2 uptake with respect to intramuscular [phosphocreatine] kinetics during moderate exercise in humans. J Physiol 518:921–932
Rossiter HB, Ward SA, Kowalchuk JM, Howe FA, Griffiths JR, Whipp BJ (2001) Effects of prior exercise on oxygen uptake and phosphocreatine kinetics during high-intensity knee-extension exercise in humans. J Physiol 537:291–303
Rossiter HB, Ward SA, Kowalchuk JM, Howe FA, Griffiths JR, Whipp BJ (2002) Dynamic asymmetry of phosphocreatine concentration and O2 uptake between the on- and off-transients of moderate- and high-intensity exercise in humans. J Physiol 541:991–1002
Rossiter HB, Ward SA, Howe FA, Wood DM, Kowalchuk JM, Griffiths JR, Whipp BJ (2003) Effects of dichloroacetate on VO2 and intramuscular 31P metabolite kinetics during high-intensity exercise in humans. J Appl Physiol 95:1105–1115
Saunders MJ, Evans EM, Arngrimsson SA, Allison JD, Warren GL, Cureton KJ (2000) Muscle activation and the slow component rise in oxygen uptake during cycling. Med Sci Sports Exerc 32:2040–2045
Shoemaker JK, Hodge L, Hughson RL (1994) Cardiorespiratory kinetics and femoral artery blood velocity during dynamic knee extension exercise. J Appl Physiol 77:2625–2632
Stringer WW, Hansen JE, Wasserman K (1997) Cardiac output estimated noninvasively from oxygen uptake during exercise. J Appl Physiol 82:908–912
Timmons JA, Gustafsson T, Sundberg CJ, Jansson E, Greenhaff PL (1998) Muscle acetyl group availability is a major determinant of oxygen deficit in humans during submaximal exercise. Am J Physiol 274:E377-E380
Tordi N, Perrey S, Harvey A, Hughson RL (2003) Oxygen uptake kinetics during two bouts of heavy cycling separated by fatiguing sprint exercise in humans. J Appl Physiol 94:533–41
Walsh ML, Takahashi A, Endo M, Miura A, Fukuba Y (2002) Effects of ischaemia on subsequent exercise-induced oxygen uptake kinetics in healthy adult humans. Exp Physiol 87:227–235
Whipp BJ (1994) The bioenergetic and gas exchange basis of exercise testing. Clin Chest Med 15:173–192
Whipp BJ, Ward SA, Lamarra N, Davis JA, Wasserman K (1982) Parameters of ventilatory and gas exchange dynamics during exercise. J Appl Physiol 52:1506–1513
Whipp BJ, Lamarra N, Ward SA (1995) Obligatory anaerobiosis resulting from oxygen uptake-to-blood flow ratio dispersion in skeletal muscle:a model. Eur J Appl Physiol 71:147–152
Wilkerson DP, Koppo K, Barstow TJ, Jones AM (2004) Effect of prior multiple-sprint exercise on pulmonary O2 uptake kinetics following the onset of perimaximal exercise. J Appl Physiol 97:1227–1236
Williamson JW, Raven PB, Whipp BJ (1996) Unaltered oxygen uptake kinetics at exercise onset with lower-body positive pressure in humans. Exp Physiol 81:695–705
Yoshida T, Whipp BJ (1995) Dynamics of the pulmonary O2 uptake to blood flow ratio \(\left(\dot{V}\hbox{O}_{2}/\hbox{Q}\right)\) during and following constant-load exercise. In: Semple SJG, Adams L, Whipp BJ (eds) Modeling and Control of Ventilation. Plenum, New York, pp 207–211
Yoshida T, Yamamoto K, Udo M (1993) Relationship between cardiac output and oxygen uptake at the onset of exercise. Eur J Appl Physiol 66:155–160
Yoshida T, Kamiya J, Hishimoto K (1995) Are oxygen uptake kinetics at the onset of exercise speeded up by local metabolic status in active muscles?. Eur J Appl Physiol 70:482–486
Acknowledgements
This study was supported in part by Grant-in-Aid for Scientific Research (C:#16500383 and #12680048) from JSPS and Grant-in-Aid for Young Scientists (B:#16700465) from MEXT. HBR is an International Fellow of the Wellcome Trust (UK) (#064898).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Endo, M., Okada, Y., Rossiter, H.B. et al. Kinetics of pulmonary \(\dot{V} \hbox{O}_{2}\) and femoral artery blood flow and their relationship during repeated bouts of heavy exercise. Eur J Appl Physiol 95, 418–430 (2005). https://doi.org/10.1007/s00421-005-0051-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-005-0051-2