Abstract
Hard tissue homeostasis is regulated by the balance between bone formation by osteoblasts and bone resorption by osteoclasts. This physiologic process allows adaptation to mechanical loading and calcium homeostasis. Under pathologic conditions, however, this process is ill-balanced resulting in either over-resorption or over-formation of hard tissue. Local over-resorption by osteoclasts is typically observed in osteolytic metastases of malignancies, autoimmune arthritis, and giant cell tumor of bone (GCTB). In tumor-related local osteolysis, tumor-derived osteoclast-activating factors induce bone resorption not by directly acting on osteoclasts but by indirectly upregulating receptor activator of NFκB ligand (RANKL) on osteoblastic cells. Similarly, synovial tissue in the autoimmune arthritis model does overexpress RANKL and contains numerous osteoclast precursors, and like a landing craft, when it comes in contact with eroded bone surfaces, osteoclast precursors are immediately polarized to become mature osteoclasts, inducing rapidly progressive bone destruction at a late stage of the disease. GCTB, on the other hand, is a common primary bone tumor, usually arising at the metaphysis of the long bone in young adults. After the discovery of RANKL, the concept of GCTB as a tumor of RANKL-expressing stromal cells was established, and comprehensive exosome studies finally disclosed the causative single-point mutation at histone H3.3 (H3F3A) in stromal cells. Thus, osteolytic lesions under various pathological conditions are ultimately attributable to the overexpression of RANKL, which opens up a common, practical and useful therapeutic target for diverse osteolytic conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hard tissue homeostasis is regulated by the equilibrium between bone formation by osteoblasts and bone resorption by osteoclasts (Martin and Ng 1994; Matsuo and Irie 2008; Chen et al. 2017; Katagiri and Takahashi 2002; Abdelgawad et al. 2016). In this process called remodeling, the group of cells responsible for remodeling is termed the basic multicellular unit (BMU) (Sims and Martin 2014; Buenzli et al. 2012). Currently, the concept of BMU has been expanded to include not only osteoblasts and osteoclasts, but also newly identified members such as T-lymphocytes, macrophages, osteocytes, and precursor populations of osteoblasts and osteoclasts (Sims and Martin 2014; Piemontese et al. 2017). Physiologic signaling pathways identified among BMU members ultimately influence two types of cells: osteoblasts and osteoclasts (Gyoja 2017; Chen et al. 2017; Tsuboi et al. 2016). Pathologic conditions of hard tissue alter these microenvironments, and the remodeling process is ill-balanced to either overproduce or overresorb hard tissue (Frost 1992). Because most of the pathologic conditions of hard tissue result in ‘lytic’ change by over-resorption (Mbalaviele et al. 2017; Johnson and Suva 2017), discussed in this review, principally, are conceptual outlines on how osteoclasts are recruited at disease sites.
Important note on handling archived histopathological specimens
For routine histopathological diagnosis, fixation and decalcification of hard tissue, two requisite and essential steps in tissue processing, various fixative and decalcifying agents have been used in the past (Gonzalez-Chavez et al. 2013). These commonly and commercially available agents can, however, occasionally cause unexpected artifacts that may lead to the misinterpretation of histochemical results (Wallington 1979). Therefore, in this review, before going into the details of the pathologic conditions of hard tissue, first discussed are some important points on processing routine histopathological specimens archived in the laboratory.
Decalcification agents, especially those with low pH value, occasionally cause the so-called ‘diffusion artifact’
This phenomenon was encountered when accessing tumor-derived parathyroid hormone-related protein (PTHrP) by immunohistochemistry. As shown in Fig. 1, while positive immunoreactions were almost exclusively observed among bone-infiltrating breast cancer cells, they showed nuclear localization. Because this peculiar subcellular localization of a peptide hormone was observed solely among autopsied specimens from hard tissue archived for a limited period of time when decalcification was done by the method based on formic acid, but not among those decalcified by the ethylenediaminetetraacetic acid (EDTA)-mediated method, we concluded that this apparent nuclear localization of PTHrP was induced by diffusion artifacts (Fahimi 1973). Thus, although evaluation of simple positivity or negativity of the immunoreaction may still be possible, care must be exercised when documenting subcellular localization of specific antigens with the use of specific decalcification agents.
Diffusion artifact in decalcified bone tissue. Diffusion artifacts attributed to decalcifying hard tissue with agents of low pH value. Histology section from an autopsied case of breast cancer with bone metastasis (a, HE, hematoxylin–eosin). By immunohistochemical analysis of PTHrP on osteolytic bone metastasis from breast cancer, decalcified specimens yield nuclear localization of the protein (b, PTHrP immunostaining). This apparent nuclear localization of PTHrP is induced by diffusion artifacts, because such subcellular localization is observed solely among autopsied specimens decalcified by the method based on formic acid. Each scale bar indicates 100 µm
Optimal conditions may vary and must be adjusted for individual histopathological sample often with a history of unclear tissue fixation (kind of fixative agent) and fixation period
Formalin fixation and paraffin embedding (FFPE) of specimens has become the standard preservation procedure for diagnostic surgical pathology. Pathology departments routinely archive vast numbers of FFPE blocks at ambient temperature, considered the most cost-effective and space-saving plan. Unlike experimental samples, while this archived resource of an enormous repository of tissues with long-term and detailed clinical data provides a valuable resource of DNA, RNA and protein for translational clinical research, some specimens can be ruined by under-fixation with poor quality or reused formalin or by over-fixation attributed to being kept in formalin over a weekend. This drawback is partially overcome by the antigen retrieval method developed for immunohistochemistry (IHC) on FFPE samples (Lopez et al. 2016; von Wasielewski et al. 1994; Bukari et al. 2017); thus, presently a wide range of archived FFPE blocks can be subjected to IHC not only for diagnostic pathology but also for experimental procedures. For in situ hybridization (ISH) studies, however, handling specimens, especially of hard tissues, requires strict pre-experimental optimization of proteinase-K treatment (Kitazawa et al. 1999). As shown in Fig. 2, the treatment of fixed hard tissue specimens with serial concentrations (0–5 µg/ml) of proteinase-K at 37 C for 10 min results in markedly different ISH results; too low concentration (0 or 0.5 µg/ml, Fig. a, b) results in low sensitivity, and too high (5 µg/ml, Fig. d) in low specificity (optimal condition in this case is 2 µg/ml, Fig. c). This optimization process although essential, is sometimes very difficult with long-term formalin-fixed samples. Keeping these drawbacks and limitations in mind, data from surgical pathology specimens should be interpreted rationally.
Optimization of proteinase-K concentration. Treatment of fixed and decalcified hard tissue specimens with serial concentrations (0–5 µg/ml) of proteinase-K at 37C for 10 min results in markedly different ISH results; too low concentration (0–0.5 µg/ml, a, b) shows low sensitivity, and too high (5 µg/ml, d) shows low specificity. Concentration of 2 µg/ml is regarded as optimal in this case (c). Each scale bar indicates 50 µm
Cancer-associated local osteolytic change: triangle of cancer cells, osteoblasts and osteoclasts
Metastatic malignancy frequently affects hard tissues. Breast cancer, for example, is frequently associated with osteolytic bone lesions either through hematogenous metastasis or by direct invasion to the bone (Ottewell et al. 2015; Liu et al. 2014), where osteoclasts play a major role in bone destruction (Singh et al. 2015; Kitazawa and Kitazawa 2002). Recently, the osteoclast differentiation factor, namely, receptor activator of NFκB (RANK) ligand (RANKL), has been identified as a prerequisite to the formation and maintenance of osteoclasts from hematopoietic precursors (Lacey et al. 1998; Yasuda et al. 1998). To elucidate the mechanism of osteoclastogenesis and bone destruction in bone-residing breast cancer, we and others have estimated in situ expression of RANKL with the use of a mouse bone-invasion model (Kitazawa and Kitazawa 2002) and autopsied samples: human breast cancer cell line, MCF-7, mixed with matrigel was subcutaneously injected into the forehead of nude mice maintained without an estrogen supplement. One, 2 and 3 weeks thereafter, the calvariae were removed and the expression of RANKL and PTHrP mRNA and osteoclastogenesis was analyzed by in situ hybridization and tartrate-resistant acid phosphatase (TRACP) activity. At early stages, spindle shaped mesenchymal cells and osteoblasts proliferated on the bone surface expressing RANKL. Three weeks after the transplantation, cancer cells formed a nest and partially invaded the eroded bone surface, where they survived without apoptosis or necrosis (Fig. 3a, HE). Numerous osteoclasts settled on the periosteal bone surface (Fig. 3b, TRACP) adjacent to the tumor nest. At all stages, PTHrP was confined to the MCF-7 breast cancer cells (Fig. 3c, PTHrP), whereas RANKL expression was confined to the osteoblastic linage (Fig. 3d, RANKL). Thus, cancer cells per se, while aggressive and destructive to surrounding tissue, are not capable of eroding and resorbing the hard tissue. In turn, cancer cells override the preexisting physiological BMU system that maintains bone volume (by balancing between bone formation and resorption) and induce local osteolytic lesions by accelerating the bone resorption axis by upregulating RANKL through interaction with osteoblastic cells (Kitazawa and Kitazawa 2002; Le Pape et al. 2016; Wu et al. 2017). Thus, cancer cells get access to growth factors stored in the bone matrix (Yoneda et al. 2013) by manipulating osteoblasts and osteoclasts, as summarized in Fig. 4. Then, can this triangular relation among cancer cells, osteoblasts and osteoclasts in experimental animals be translated to the clinical aspects of bone metastasis? To address this issue, a series of osteolytic bone metastatic lesions from autopsied materials was analyzed by IHC and ISH. At metastatic sites, RANKL expression was almost exclusively observed on osteoblastic cells located close to metastasizing cancer cells, where osteoclasts were induced by RANKL-positive osteoblastic cells (unpublished data). Similarly, with the use of autopsied cases of multiple myeloma, where neoplastic plasmacytic cells form typical osteolytic change called ‘punched-out lesion’ in hard tissue (Fig. 5a, HE), the expression of RANKL was investigated by IHC and ISH. As shown in Fig. 5b, c, RANKL-ISH (b) and -IHC (c), RANKL expression was also demonstrated mainly on osteoblastic cells but less so on typical multiple myeloma cells. Likewise, while we and some investigators attributed the major source of RANKL expression to osteoblastic cell types in the bone marrow of patients with multiple myeloma (Roux et al. 2002; Terpos et al. 2017), others have reported that primary multiple myeloma cells per se do express RANKL (Yuan et al. 2014). Thus, although direct induction and activation of osteoclasts by tumor-derived RANKL may in part contribute to the formation of osteolytic lesions, eventually almost all the osteolytic change induced by tumor cells, irrespective of their origin, can be attributed to the trilateral relation among cancer cells, osteoblasts and osteoclasts.
PTHrP production, RANKL expression and osteolytic change in experimental model. HE staining (a, HE, bar indicates 1000 µm) shows that MCF-7 cells form a nest at the periosteal site with a space between cancer cells and the surface of the bone. TRACP staining (b, bar indicates 1000 µm) shows numerous TRACP-positive osteoclasts (arrows) on bone surface nearby transplanted MCF-7 cells. Lower panels are magnified view of the boxed area in HE staining. PTHrP expression (c, bar indicates 100 µm) is observed on cancer cells, especially in the peripheral area of the nest. While apoptotic and necrotic changes are seen predominantly at the initially transplanted tumor nest, strong RANKL signals (d, bar indicates 100 µm) are observed on the proliferating mesenchymal cells around cancer cells.
Schematic view of the relation among osteoblasts, osteoclasts and tumor cells. The cancer cells override the preexisting physiological BMU system that maintains bone volume by balancing between bone formation and resorption, and induces local osteolytic lesions by accelerating the bone resorption axis by upregulating RANKL through the interaction with osteoblastic cells. Thus, cancer cells get granted growth factors stored in the bone matrix by orchestrating osteoblasts and osteoclasts. BMM bone marrow macrophages
HE staining of bone specimen from an autopsied case of multiple myeloma (a, HE). Osteoclasts are induced at eroded bone surface. By ISH (b), RANKL expression is mainly demonstrated on osteoblastic cells, and very weakly on typical multiple myeloma cells. By IHC (c), RANKL expression is also mainly demonstrated on osteoblastic cells, and very weakly on typical multiple myeloma cells. Each bar indicates 50 µm
Among tumor-derived osteoclast-activating factors, PTHrP most commonly observed in tumor cells of various origins was first isolated from lung cancer cell line established from a patient who had squamous cell carcinoma of the lung with humoral hypercalcemia of malignancy (HHM) (Suva et al. 1987). This protein has 8 of 13 N-terminal amino acid residues identical to those present in parathyroid hormone (PTH) and is thought to mimic most of the actions of PTH through a common PTH/ PTHrP receptor (Martin and Suva 1988). In addition to its being the major factor responsible for HHM, PTHrP has now drawn attention to the high incidence of its production in breast cancer with a potential for skeletal metastases and recurrence (Kohno et al. 1994). Since the discovery of the new RANKL–RANK signaling system, most of the bone resorptive factors have been shown to promote bone resorption by upregulating RANKL gene expression on osteoblastic cells (Dougall et al. 2014). As mentioned above, growth factors released from hard tissue by osteoclasts, in turn, favor the growth and survival of cancer cells in a hard tissue milieu; the interrelation among tumor cells, osteoclasts and osteoblasts at local osteolytic lesions plays a central role in developing invasion of and metastasis to the bone as well as in a systemic effect resulting in HHM (Theriault and Theriault 2012). Interestingly, PTHrP production is also observed in some cases of multiple myeloma with HHM (Cafforio et al. 2014). Two such autopsied cases demonstrating high serum PTHrP values have been described (Kitazawa et al. 2002; Kinomura et al. 2015) where PTHrP mRNA expression was confined to tumor cells. Since PTHrP is a soluble and diffusive peptide hormone, its production and secretion by tumor cells alone cannot fully explain the formation of local steep-edged or precipitous osteolytic change termed ‘punched-out lesion’. Although still controversial, whether RANKL is the sole factor responsible for the formation of osteolytic punched-out lesions in multiple myeloma, and whether other additional local factors including cell-to-cell interactions are assumably involved in the formation of localized round and sharp-edged osteolytic lesion (Xu et al. 2016), the role of PTHrP released from tumor cells has broader repertories in both local and systemic osteolytic lesions than has been speculated. Inclusively, osteoclasts induced by tumor-derived PTHrP may play a central role in cancer-mediated bone destruction and may offer a hospitable microenvironment for the survival of cancer cells in bone.
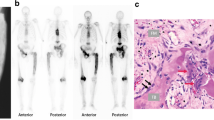
Rapidly progressive osteolytic change in late-stage autoimmune arthritis
Rheumatoid arthritis (RA) is a systemic disorder characterized by synovial inflammation and subsequent destruction and deformation of synovial joints (Orr et al. 2017). The articular lesions start with synovitis, focal erosion of unmineralized cartilage, and then culminate in the rapidly progressive destruction of subarticular bone by pannus at late stages of the disease (Ludwig et al. 2017). Osteoclasts, specialized cells that resorb bone, also play a central role in developing those osteolytic lesions (Udagawa et al. 2002). To elucidate the mechanism of osteoclastogenesis and bone destruction in autoimmune arthritis, the expression of RANKL, RANK and osteoprotegerin (OPG) (a decoy receptor for RANKL) mRNA in a mouse type II collagen-induced arthritis (CIA) model was investigated with the use of ISH (Mori et al. 2002). The results indicated that the inflamed and proliferating synovium formed a typical pannus (Fig. 6a, HE) with numerous TRAP-positive mononuclear cells (Fig. 6b, TRACP). Those osteoclast precursors were RANK-positive (Fig. 6c, RANK). In the inflamed synovium, synovial fibroblastic cells around these RANK-positive cells were strongly positive for RANKL (Fig. 6d, RANKL). These data indicated that the RANKL–RANK system also plays an important role in the recruitment of osteoclast precursor populations in autoimmune arthritis (Mori et al. 2002; Udagawa et al. 2002), and the inflamed synovium is, therefore, a suitable pool for osteoclast precursors. The articular lesions of autoimmune arthritis start with persistent synovitis, progress to articular cartilage destruction by matrix metalloproteinase released from macrophages and fibroblastic cells, and then destruction proceeds to subchondral bone (Teitelbaum 2006). Because the precursors immediately differentiate into polarized, functioning multinucleated mature osteoclasts on the bone surface only after they adhere to bone matrix proteins (Teitelbaum et al. 1995), once the synovium abundant in osteoclast precursors reaches the eroded articular bone surface, numerous mature osteoclasts are rapidly recruited to the eroded sites. Thus, like numerous skilled soldiers released from landing craft invading the coast, the abundant mature and activated osteoclasts are released from the inflamed synovium, resulting in the formation of the so-called pannus. Subsequent to the local destruction of the articular cartilage in autoimmune arthritis, direct contact between mononuclear osteoclast precursors in inflamed synovial tissue and denuded subchondral bone triggers rapid induction of mature and activated osteoclasts, provoking formation of the pannus at late stages of autoimmune arthritis. These findings demonstrate that RANKL expression in the inflamed synovium plays a central role in developing osteolytic lesions in local subarticular bone (Mori et al. 2002), suggesting that again the RANKL–RANK system can be a good target for therapeutic intervention in autoimmune arthritis.

[Modified from Fig. 5 of previous our publication in HCB (Mori et al. 2002)] Each scale bar indicates 100 µm
Mouse type II collagen-induced arthritis model shows typical severe arthritis with inflamed and proliferating synovium forming a typical pannus (a, HE) with numerous TRAP-positive mononuclear cells (b, TRACP). Those osteoclast precursors are RANK-positive (c, RANK). In the inflamed synovium, synovial fibroblastic cells around these RANK-positive cells are strongly positive for RANKL (d, RANKL).
Giant cell tumor of bone
Giant cell tumor of the bone (GCTB), a common bone tumor accounting for 5–10% of primary bone tumors and 15–20% of benign bone tumors, usually arises at the metaphysis of the long bone of young adults aged 20–40, when the epiphysial plate has matured. It commonly affects the distal portion of the femur, the proximal portion of the tibia, and less frequently, spinal bones. When progressing, GCTB often degrades surrounding bones, causes pain, limits articular motion, induces pathological fractures, and very rarely metastasizes to the lung. Plain X-ray examination of GCTB typically demonstrates localized cystic translucent lesions with thinning cortical bone at the metaphysis resulting in the so-called ‘soap bubble appearance’ (Sobti et al. 2016). By histopathological examination, numerous multinucleated giant cells, at first recognized as tumor cells, are termed GCTB (Yamada et al. 2017). Consequently, longstanding debates have been held between two groups: one claiming that GCTB is a tumor of the macrophage–monocyte cell lineage that is a precursor of osteoclastic giant cells; the other stating that stromal cells themselves are the tumor cells, and that giant cells are formed secondarily to the tumorous stromal cells (McCarthy 1980). The latter concept of the origin of stromal cells prevailed in that while osteoclastic giant cells gradually disappear, only the stromal cell element survives after passaging the primary cultured samples of surgically resected GCTB (Ghert et al. 2007). Two questions (1) why such numerous non-tumorous giant cells are induced, and (2) what underlies the genetic alteration of the development of GCTB, unresolved, however, for a long time. Although after the discovery of RANKL, the concept of GCTB as a stromal cell tumor overexpressing RANKL had been established (Werner 2006), genetic alterations causing GCTB remained unknown for as long as 15 years. During this period, while comprehensive exosome studies with the use of a next generation sequencer disclosed trunk or driver mutation of many tumors one after another, dealing with mRNAs extracted from surgically removed GCTB samples had been yielding uncertain and inconsistent results because of the peculiarity that GCTB is composed of a majority of non-tumorous osteoclastic giant cells and a minority of tumorous stromal cells (Wang et al. 2012). From 2010, our group started the project of identifying causative genetic alteration in GCTB with the use of primary cultured samples of surgically resected GCTB. To overcome the deviant heterogeneity of GCTB, the primarily cultured samples were passaged twice to enrich the tumor cell population without reducing the character of the tumor cells. This somewhat complicated procedure required considerable time and effort for examining each GCTB case, and while in the process of collecting a sufficient number of cases to satisfy the recurrence of genetic alterations, to our regret, another comprehensive and cooperative exosome study among multicentric groups identified the causative genetic alteration as a single-point mutation at histone H3.3 (H3F3A) of the gene in 2013 (Lindroth and Plass 2013). The authors also demonstrated that the same GGG to TGG point mutation at codon 34 of the H3F3A gene resulting in p.G34W is recurrently observed in 50% (monoallelic mutation) of mRNA in all the cases examined by us (Fig. 7, upper panel). Interestingly, not only chondroblastoma (Behjati et al. 2013) showing similar histologic features as GCTB, but also high-grade glioma (GBM) in childhood (Schwartzentruber et al. 2012) and pediatric diffuse intrinsic pontine glioma (DIPG) (Wu et al. 2012) share similar H3.3 mutations as illustrated in lower panel of Fig. 7. Because these H3.3 mutations are disease-specific, and because giant cell reparative granuloma (GCRG), a reactive condition often difficult for differentiating from GCTB on histopathological examination, does not carry any H3.3 mutation, types of H3.3 mutation can be useful markers for molecular pathological diagnosis (Nohr et al. 2017; Yamamoto et al. 2017). Thus, assumptions of tumor-specific driver mutation revealed by comprehensive genomic and exosome analyses have influenced classification, pathological diagnosis and treatment of the disease, allowing the pathologist to conduct companion diagnosis for molecular-targeting therapy. Recently, in addition to conventional surgical curettage and the filling of defects with artificial bony materials, anti-RANKL antibody (denosumab) therapy introduced in the treatment of GCTB with successful outcome (Branstetter et al. 2012). It apparently does not directly target the tumor cells but reduces the formation of secondarily induced osteoclastic giant cells. By diminishing the number of those cells, the therapy is assumably effective for GCTB by the reduction of the enlargement of the tumor mass, the risk of pathological fracture, and the growth factors from hard tissue released by bone resorption (van der Heijden et al. 2017). Recently, we had an opportunity to compare histopathological features of a GCTB case before and after anti-RANKL antibody therapy. While biopsy specimens before the therapy revealed typical GCTB features of abundant giant osteoclastic cells (Fig. 8a), surgically resected specimens after treatment showed bone-forming tumors with abundant osteoid formation (Fig. 8b). Genetic analysis of microdissected samples from the two histopathological specimens revealed that both samples with apparently different phenotypes shared typical GGG to TGG point mutation at codon 34 of the H3F3A gene, resulting in p.G34W (data not shown), confirming that the peculiar bone-forming tumor secondary to anti-RANKL antibody treatment was directly transformed from the preceding GCTB (unpublished data). Because RANKL is a membrane-bound ligand, upon antibody binding, this peculiar phenomenon let us imagine the existence of RANKL-dependent reverse intracellular signaling that accelerates osteoblastic differentiation. These newly observed therapy-related consequences may lead to the development of another therapeutic strategy.
A GGG to TGG point mutation at codon 34 of the H3F3A gene resulting in p.G34W is recurrently observed in 50% (monoallelic mutation) of mRNA in all the cases we examined (upper panel). The portion and pattern of typical mutations seen in high-grade glioma (GBM) in childhood, chondroblastoma and GCTB are illustrated (lower panel)
Histopathological features of GCTB before (a, HE) and after (b, HE) anti-RANKL antibody therapy. While biopsy specimens before the therapy reveal typical GCTB features of abundant osteoclastic giant cells, surgically resected specimens after the treatment show bone-forming tumors with abundant osteoid formation. Each scale bar indicates 100 µm
Conclusions
Osteoclasts derive from hematopoietic cells of the monocyte/macrophage lineage. Since cell-to-cell interaction between cells of the osteoblast/stromal lineage and the monocyte/macrophage lineage has been regarded as a prerequisite to the formation of osteoclasts, a membrane-bound molecule expressed on osteoblasts/stromal cells has been postulated as a crucial factor for osteoclast differentiation. Recently, this membrane-bound molecule has been identified as identical to RANKL. To date, two types of receptors for RANKL are known: RANK and OPG. RANK expressed on osteoclast precursors and on mature osteoclasts transduces RANKL signaling. On the other hand, OPG is a secreted member of the TNF receptor superfamily that functions as a decoy receptor of the RANKL–RANK signaling system to inhibit osteoclastogenesis. Thus, RANKL, RANK and OPG constitute a critical system that controls bone resorption by regulating the number and activity of osteoclasts. Various pathologic conditions of hard tissue usually result in osteolytic lesions by osteoclasts, which are induced by unbalanced or altered signaling pathways among BMU members. Because the axis of RANKL and its decoy receptor OPG is one of the ultimate targets of signaling among BMU members, it is a major therapeutic target of osteolytic bone lesions irrespective of the pathogenesis of the disease.
References
Abdelgawad ME, Delaisse JM, Hinge M, Jensen PR, Alnaimi RW, Rolighed L, Engelholm LH, Marcussen N, Andersen TL (2016) Early reversal cells in adult human bone remodeling: osteoblastic nature, catabolic functions and interactions with osteoclasts. Histochem Cell Biol 145(6):603–615. https://doi.org/10.1007/s00418-016-1414-y
Behjati S, Tarpey PS, Presneau N, Scheipl S, Pillay N, Van Loo P, Wedge DC, Cooke SL, Gundem G, Davies H, Nik-Zainal S, Martin S, McLaren S, Goodie V, Robinson B, Butler A, Teague JW, Halai D, Khatri B, Myklebost O, Baumhoer D, Jundt G, Hamoudi R, Tirabosco R, Amary MF, Futreal PA, Stratton MR, Campbell PJ, Flanagan AM (2013) Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nat Genet 45(12):1479–1482. https://doi.org/10.1038/ng.2814
Branstetter DG, Nelson SD, Manivel JC, Blay JY, Chawla S, Thomas DM, Jun S, Jacobs I (2012) Denosumab induces tumor reduction and bone formation in patients with giant-cell tumor of bone. Clin Cancer Res 18(16):4415–4424. https://doi.org/10.1158/1078-0432.CCR-12-0578
Buenzli PR, Jeon J, Pivonka P, Smith DW, Cummings PT (2012) Investigation of bone resorption within a cortical basic multicellular unit using a lattice-based computational model. Bone 50(1):378–389. https://doi.org/10.1016/j.bone.2011.10.021
Bukari BA, Citartan M, Ch’ng ES, Bilibana MP, Rozhdestvensky T, Tang TH (2017) Aptahistochemistry in diagnostic pathology: technical scrutiny and feasibility. Histochem Cell Biol 147(5):545–553. https://doi.org/10.1007/s00418-017-1561-9
Cafforio P, Savonarola A, Stucci S, De Matteo M, Tucci M, Brunetti AE, Vecchio VM, Silvestris F (2014) PTHrP produced by myeloma plasma cells regulates their survival and pro-osteoclast activity for bone disease progression. J Bone Miner Res 29(1):55–66. https://doi.org/10.1002/jbmr.2022
Chen X, Wang Z, Duan N, Zhu G, Schwarz EM, Xie C (2017) Osteoblast–osteoclast interactions. Connect Tissue Res. https://doi.org/10.1080/03008207.2017.1290085
Dougall WC, Holen I, Gonzalez Suarez E (2014) Targeting RANKL in metastasis. Bonekey Rep 3:519. https://doi.org/10.1038/bonekey.2014.14
Fahimi HD (1973) Diffusion artifacts in cytochemistry of catalase. J Histochem Cytochem 21(11):999–1009. https://doi.org/10.1177/21.11.999
Frost HM (1992) Perspectives: bone’s mechanical usage windows. Bone Miner 19(3):257–271
Ghert M, Simunovic N, Cowan RW, Colterjohn N, Singh G (2007) Properties of the stromal cell in giant cell tumor of bone. Clin Orthop Relat Res 459:8–13. https://doi.org/10.1097/BLO.0b013e31804856a1
Gonzalez-Chavez SA, Pacheco-Tena C, Macias-Vazquez CE, Luevano-Flores E (2013) Assessment of different decalcifying protocols on osteopontin and osteocalcin immunostaining in whole bone specimens of arthritis rat model by confocal immunofluorescence. Int J Clin Exp Pathol 6(10):1972–1983
Gyoja F (2017) Basic helix-loop-helix transcription factors in evolution: roles in development of mesoderm and neural tissues. Genesis. https://doi.org/10.1002/dvg.23051
Johnson RW, Suva LJ (2017) Hallmarks of bone metastasis. Calcif Tissue Int. https://doi.org/10.1007/s00223-017-0362-4
Katagiri T, Takahashi N (2002) Regulatory mechanisms of osteoblast and osteoclast differentiation. Oral Dis 8(3):147–159
Kinomura M, Shimada N, Nishikawa M, Omori K, Jo T, Ueda Y, Notohara K, Kitazawa R, Kitazawa S, Fukushima M, Asano K (2015) Parathyroid hormone-related peptide-producing multiple myeloma and renal impairment. Intern Med 54(23):3029–3033. https://doi.org/10.2169/internalmedicine.54.5085
Kitazawa S, Kitazawa R (2002) RANK ligand is a prerequisite for cancer-associated osteolytic lesions. J Pathol 198(2):228–236. https://doi.org/10.1002/path.1199
Kitazawa S, Kitazawa R, Maeda S (1999) In situ hybridization with polymerase chain reaction-derived single-stranded DNA probe and S1 nuclease. Histochem Cell Biol 111(1):7–12
Kitazawa R, Kitazawa S, Kajimoto K, Sowa H, Sugimoto T, Matsui T, Chihara K, Maeda S (2002) Expression of parathyroid hormone-related protein (PTHrP) in multiple myeloma. Pathol Int 52(1):63–68
Kohno N, Kitazawa S, Sakoda Y, Kanbara Y, Furuya Y, Ohashi O, Kitazawa R (1994) Parathyroid hormone-related protein in breast cancer tissues: relationship between primary and metastatic sites. Breast Cancer 1(1):43–49
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ (1998) Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93(2):165–176
Le Pape F, Vargas G, Clezardin P (2016) The role of osteoclasts in breast cancer bone metastasis. J Bone Oncol 5(3):93–95. https://doi.org/10.1016/j.jbo.2016.02.008
Lindroth AM, Plass C (2013) Recurrent H3.3 alterations in childhood tumors. Nat Genet 45(12):1413–1414. https://doi.org/10.1038/ng.2832
Liu W, Vivian CJ, Brinker AE, Hampton KR, Lianidou E, Welch DR (2014) Microenvironmental influences on metastasis suppressor expression and function during a metastatic cell’s journey. Cancer Microenviron 7(3):117–131. https://doi.org/10.1007/s12307-014-0148-4
Lopez IA, Ishiyama G, Hosokawa S, Hosokawa K, Acuna D, Linthicum FH, Ishiyama A (2016) Immunohistochemical techniques for the human inner ear. Histochem Cell Biol 146(4):367–387. https://doi.org/10.1007/s00418-016-1471-2
Ludwig RJ, Vanhoorelbeke K, Leypoldt F, Kaya Z, Bieber K, McLachlan SM, Komorowski L, Luo J, Cabral-Marques O, Hammers CM, Lindstrom JM, Lamprecht P, Fischer A, Riemekasten G, Tersteeg C, Sondermann P, Rapoport B, Wandinger KP, Probst C, El Beidaq A, Schmidt E, Verkman A, Manz RA, Nimmerjahn F (2017) Mechanisms of autoantibody-induced pathology. Front Immunol 8:603. https://doi.org/10.3389/fimmu.2017.00603
Martin TJ, Ng KW (1994) Mechanisms by which cells of the osteoblast lineage control osteoclast formation and activity. J Cell Biochem 56(3):357–366. https://doi.org/10.1002/jcb.240560312
Martin TJ, Suva LJ (1988) Parathyroid hormone-related protein: a novel gene product. Baillieres Clin Endocrinol Metab 2(4):1003–1029
Matsuo K, Irie N (2008) Osteoclast–osteoblast communication. Arch Biochem Biophys 473(2):201–209. https://doi.org/10.1016/j.abb.2008.03.027
Mbalaviele G, Novack DV, Schett G, Teitelbaum SL (2017) Inflammatory osteolysis: a conspiracy against bone. J Clin Invest 127(6):2030–2039. https://doi.org/10.1172/JCI93356
McCarthy EF (1980) Giant-cell tumor of bone: an historical perspective. Clin Orthop Relat Res (153):14–25
Mori H, Kitazawa R, Mizuki S, Nose M, Maeda S, Kitazawa S (2002) RANK ligand, RANK, and OPG expression in type II collagen-induced arthritis mouse. Histochem Cell Biol 117(3):283–292. https://doi.org/10.1007/s00418-001-0376-9
Nohr E, Lee LH, Cates JM, Perizzolo M, Itani D (2017) Diagnostic value of histone 3 mutations in osteoclast-rich bone tumors. Hum Pathol 68:119–127. https://doi.org/10.1016/j.humpath.2017.08.030
Orr C, Vieira-Sousa E, Boyle DL, Buch MH, Buckley CD, Canete JD, Catrina AI, Choy EHS, Emery P, Fearon U, Filer A, Gerlag D, Humby F, Isaacs JD, Just SA, Lauwerys BR, Le Goff B, Manzo A, McGarry T, McInnes IB, Najm A, Pitzalis C, Pratt A, Smith M, Tak PP, Thurlings R, Fonseca JE, Veale DJ (2017) Synovial tissue research: a state-of-the-art review. Nat Rev Rheumatol 13(8):463–475. https://doi.org/10.1038/nrrheum.2017.115
Ottewell PD, O’Donnell L, Holen I (2015) Molecular alterations that drive breast cancer metastasis to bone. Bonekey Rep 4:643. https://doi.org/10.1038/bonekey.2015.10
Piemontese M, Almeida M, Robling AG, Kim HN, Xiong J, Thostenson JD, Weinstein RS, Manolagas SC, O’Brien CA, Jilka RL (2017) Old age causes de novo intracortical bone remodeling and porosity in mice. JCI Insight. https://doi.org/10.1172/jci.insight.93771
Roux S, Meignin V, Quillard J, Meduri G, Guiochon-Mantel A, Fermand JP, Milgrom E, Mariette X (2002) RANK (receptor activator of nuclear factor-kappaB) and RANKL expression in multiple myeloma. Br J Haematol 117(1):86–92
Schwartzentruber J, Korshunov A, Liu XY, Jones DT, Pfaff E, Jacob K, Sturm D, Fontebasso AM, Quang DA, Tonjes M, Hovestadt V, Albrecht S, Kool M, Nantel A, Konermann C, Lindroth A, Jager N, Rausch T, Ryzhova M, Korbel JO, Hielscher T, Hauser P, Garami M, Klekner A, Bognar L, Ebinger M, Schuhmann MU, Scheurlen W, Pekrun A, Fruhwald MC, Roggendorf W, Kramm C, Durken M, Atkinson J, Lepage P, Montpetit A, Zakrzewska M, Zakrzewski K, Liberski PP, Dong Z, Siegel P, Kulozik AE, Zapatka M, Guha A, Malkin D, Felsberg J, Reifenberger G, von Deimling A, Ichimura K, Collins VP, Witt H, Milde T, Witt O, Zhang C, Castelo-Branco P, Lichter P, Faury D, Tabori U, Plass C, Majewski J, Pfister SM, Jabado N (2012) Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482(7384):226–231. https://doi.org/10.1038/nature10833
Sims NA, Martin TJ (2014) Coupling the activities of bone formation and resorption: a multitude of signals within the basic multicellular unit. Bonekey Rep 3:481. https://doi.org/10.1038/bonekey.2013.215
Singh T, Kaur V, Kumar M, Kaur P, Murthy RS, Rawal RK (2015) The critical role of bisphosphonates to target bone cancer metastasis: an overview. J Drug Target 23(1):1–15. https://doi.org/10.3109/1061186X.2014.950668
Sobti A, Agrawal P, Agarwala S, Agarwal M (2016) Giant cell tumor of bone—an overview. Arch Bone Jt Surg 4(1):2–9
Suva LJ, Winslow GA, Wettenhall RE, Hammonds RG, Moseley JM, Diefenbach-Jagger H, Rodda CP, Kemp BE, Rodriguez H, Chen EY et al (1987) A parathyroid hormone-related protein implicated in malignant hypercalcemia: cloning and expression. Science 237(4817):893–896
Teitelbaum SL (2006) Osteoclasts; culprits in inflammatory osteolysis. Arthritis Res Ther 8(1):201. https://doi.org/10.1186/ar1857
Teitelbaum SL, Abu-Amer Y, Ross FP (1995) Molecular mechanisms of bone resorption. J Cell Biochem 59(1):1–10. https://doi.org/10.1002/jcb.240590102
Terpos E, Christoulas D, Gavriatopoulou M, Dimopoulos MA (2017) Mechanisms of bone destruction in multiple myeloma. Eur J Cancer Care (Engl). https://doi.org/10.1111/ecc.12761
Theriault RL, Theriault RL (2012) Biology of bone metastases. Cancer Control 19(2):92–101. https://doi.org/10.1177/107327481201900203
Tsuboi K, Hasegawa T, Yamamoto T, Sasaki M, Hongo H, de Freitas PH, Shimizu T, Takahata M, Oda K, Michigami T, Li M, Kitagawa Y, Amizuka N (2016) Effects of drug discontinuation after short-term daily alendronate administration on osteoblasts and osteocytes in mice. Histochem Cell Biol 146(3):337–350. https://doi.org/10.1007/s00418-016-1450-7
Udagawa N, Kotake S, Kamatani N, Takahashi N, Suda T (2002) The molecular mechanism of osteoclastogenesis in rheumatoid arthritis. Arthritis Res 4(5):281–289. https://doi.org/10.1186/ar431
van der Heijden L, Dijkstra PDS, Blay JY, Gelderblom H (2017) Giant cell tumour of bone in the denosumab era. Eur J Cancer 77:75–83. https://doi.org/10.1016/j.ejca.2017.02.021
von Wasielewski R, Werner M, Nolte M, Wilkens L, Georgii A (1994) Effects of antigen retrieval by microwave heating in formalin-fixed tissue sections on a broad panel of antibodies. Histochemistry 102(3):165–172
Wallington EA (1979) Artifacts in tissue sections. Med Lab Sci 36(1):3–61
Wang H, Wan N, Hu Y (2012) Giant cell tumour of bone: a new evaluating system is necessary. Int Orthop 36(12):2521–2527. https://doi.org/10.1007/s00264-012-1664-9
Werner M (2006) Giant cell tumour of bone: morphological, biological and histogenetical aspects. Int Orthop 30(6):484–489. https://doi.org/10.1007/s00264-006-0215-7
Wu G, Broniscer A, McEachron TA, Lu C, Paugh BS, Becksfort J, Qu C, Ding L, Huether R, Parker M, Zhang J, Gajjar A, Dyer MA, Mullighan CG, Gilbertson RJ, Mardis ER, Wilson RK, Downing JR, Ellison DW, Zhang J, Baker SJ, St. Jude Children’s Research Hospital–Washington University Pediatric Cancer Genome P (2012) Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat Genet 44(3):251–253. https://doi.org/10.1038/ng.1102
Wu C, Sun Z, Guo B, Ye Y, Han X, Qin Y, Liu S (2017) Osthole inhibits bone metastasis of breast cancer. Oncotarget 8(35):58480–58493. https://doi.org/10.18632/oncotarget.17024
Xu L, Mohammad KS, Wu H, Crean C, Poteat B, Cheng Y, Cardoso AA, Machal C, Hanenberg H, Abonour R, Kacena MA, Chirgwin J, Suvannasankha A, Srour EF (2016) Cell adhesion molecule CD166 drives malignant progression and osteolytic disease in multiple myeloma. Cancer Res 76(23):6901–6910. https://doi.org/10.1158/0008-5472.CAN-16-0517
Yamada Y, Kinoshita I, Kenichi K, Yamamoto H, Iwasaki T, Otsuka H, Yoshimoto M, Ishihara S, Toda Y, Kuma Y, Setsu N, Koga Y, Honda Y, Inoue T, Yanai H, Yamashita K, Ito I, Takahashi M, Ohga S, Furue M, Nakashima Y, Oda Y (2017) Histopathological and genetic review of phosphaturic mesenchymal tumours, mixed connective tissue variant. Histopathology. https://doi.org/10.1111/his.13377
Yamamoto H, Iwasaki T, Yamada Y, Matsumoto Y, Otsuka H, Yoshimoto M, Kohashi K, Taguchi K, Yokoyama R, Nakashima Y, Oda Y (2017) Diagnostic utility of histone H3.3G34 W, G34R, and G34 V mutant-specific antibodies for giant cell tumors of bone. Hum Pathol. https://doi.org/10.1016/j.humpath.2017.11.020
Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, Tomoyasu A, Yano K, Goto M, Murakami A, Tsuda E, Morinaga T, Higashio K, Udagawa N, Takahashi N, Suda T (1998) Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci USA 95(7):3597–3602
Yoneda T, Tanaka S, Hata K (2013) Role of RANKL/RANK in primary and secondary breast cancer. World J Orthop 4(4):178–185. https://doi.org/10.5312/wjo.v4.i4.178
Yuan L, Chan GC, Fung KL, Chim CS (2014) RANKL expression in myeloma cells is regulated by a network involving RANKL promoter methylation, DNMT1, microRNA and TNFalpha in the microenvironment. Biochim Biophys Acta 1843(9):1834–1838. https://doi.org/10.1016/j.bbamcr.2014.05.010
Acknowledgements
This study was partially supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture, Japan (to RK, RH and SK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kitazawa, R., Haraguchi, R., Fukushima, M. et al. Pathologic conditions of hard tissue: role of osteoclasts in osteolytic lesion. Histochem Cell Biol 149, 405–415 (2018). https://doi.org/10.1007/s00418-018-1639-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-018-1639-z