Abstract
Salivary calcium plays a vital role in bio-mineralization of dental enamel and exposed dentin. In order to elucidate the yet unknown cellular and molecular mechanisms of calcium secretion in human salivary glands the presence of various relevant plasma membrane transport systems for calcium were investigated. Using an RT-PCR approach, expression of the epithelial calcium channel (CaT-Like), the calcium binding protein (calbindin-2), the endoplasmic reticulum pumps (SERCA-2 and -3), and the plasma membrane calcium ATPases (PMCA-1, -2, and -4), were found in parotid and submandibular glands. Immunohistochemistry revealed that CaT-Like is located in the basolateral plasma membrane of acinar cells; while calbindin-2, SERCA-2 and SERCA-3 were found inside the acinar cells; and PMCA-2 was found in the apical membrane and in the secretory canaliculi between the cells. Based on these findings, we propose the following model of calcium secretion in human salivary glands: (1) calcium enters the acinar cell at the basolateral side via calcium channel CaT-Like (calcium influx); (2) intracellular calcium is taken up into the endoplasmic reticulum by SERCA-2 and possibly SERCA3 or bound to calbindin-2 (intracellular calcium pool); and (3) calcium is secreted by PMCAs at the apical plasma membrane (calcium efflux).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental enamel, the hardest and densest material in the body, is composed of hydroxyapatite, a complex mineral containing calcium and phosphate. This unique biomineralization structure is constantly renewed by remineralization, which involves the deposition of calcium and phosphate ions from saliva into the enamel subsurface areas and onto the enamel surface (Edgar and Higham 1995). Under acidic conditions apatite crystallites of the subsurface enamel dissolve into the surrounding fluid. This demineralization is one of the first steps in dental caries development (Pearce 1998). The availability of calcium and phosphate is therefore of major importance for the remineralization of initial caries lesions after acid challenge (Tanaka and Kadoma 2000). Furthermore, a low caries rate is thought to be associated with high salivary calcium concentration in children (Mass et al. 2002) and adults (Sewon and Makela 1990). Finally, superficial erosions of teeth due to acid stress are also remineralized by calcium and phosphate present in saliva (Hoyer et al. 1984).
Several studies have been performed to analyze the mechanism of calcium transport through epithelial cells. In general, two modes of transepithelial calcium transport can be distinguished, namely transcellular or paracellular. In transcellular transport calcium entry across the membrane is mediated by epithelial calcium channels such as CaT1 in small intestine (Peng et al. 1999, 2000, 2003) or CaT2 in the distal renal tubule (Hoenderop et al. 2000). Intracellular calcium is then buffered either by calcium binding proteins such as calbindin-1 in kidney and small intestine (Hoenderop et al. 2000) or taken up into the endoplasmic reticulum by active calcium pumps such a SERCA in pancreas (Petersen 2003). Efflux of calcium from the cell is achieved by primary active mechanisms such as the plasma membrane calcium ATPase (PMCAs-1) and/or by the secondary active sodium–calcium exchanger (NCX1) in kidney and small intestine (Hoenderop et al. 2002). In paracellular transport paracellin, a tight junction protein forming Mg2+ and Ca2+ pores, appears to be involved (Simon et al. 1999).
Despite several studies addressing calcium transport in salivary glands the mechanism of calcium secretion into saliva is not well characterized (Peng et al. 2003). Therefore, the aim of this study is using molecular biology and immunohistochemistry techniques to elucidate the cellular and molecular mechanisms of transepithelial calcium transport for human salivary parotid and submandibular glands and to propose a model for calcium secretion into saliva.
Materials and methods
Tissue samples
Samples of human salivary gland were obtained from resection material of adult patients undergoing surgery for various primary maxillofacial interventions. Samples were not bigger than 3 mm3 and immediately after resection conserved in liquid nitrogen or in RNAlater (Qiagen, Hilden, Germany). For immunohistochemical analysis; samples were fixed in 4% paraformaldehyde in PBS for 24 h at 4°C, cryoprotected in 2.8 M sucrose, and then frozen in liquid nitrogen and stored at −70°C. Small pieces were embedded in TissueTek (Sakura, Torrance, CA, USA) and stored at −80°C. For RNA analysis, tissue samples were homogenized using the Mixer Mill MM 301 for 2 min and 200 Hz. Total RNA was isolated using the RNeasy Mini Kit (Qiagen).
RT-PCR analysis
To evaluate the mRNA expression of genes related to calcium transport in human salivary glands RT-PCR was performed using specific primers designed by Primer Express 2.0 Software (Applied Biosystems, Darmstadt, Germany) and obtained from MWG-Biotech AG (Ebersberg, Germany) (for sequences see Table 1). RNA (5 μg) was reverse-transcribed with Superscript II RT (Invitrogen) at 42°C for 50 min using oligo dT primers (Promega, Mannheim, Germany), control reactions did not contain RT. Hundred nanogram of cDNA or non-reverse-transcribed RNA were amplified for 35 cycles in 50 μl total volume of PCR buffer 5x-PCR (Qiagen) containing 10 μM dNTP, 1 unit Taq polymerase, 20 pmol of each primer. The thermal cycling program (94°C for 30 s, 55–62°C for 30 s, and 72°C for 90 s) was performed in an Eppendorf Mastercycler gradient. Amplified products were separated on a 1.2% agarose gel, all PCR-fragments were verified by sequencing. Intensities of bands from the agarose gels were quantified using the Scion Image software (National Institutes of Health, Bethesda, MD, USA), results were normalized to GAPDH.
Western blotting
To confirm the presence of proteins at the membrane level, western blot analysis from all significantly expressed genes from calcium channel and transporters expressed in human salivary gland samples was performed. Briefly, human salivary gland samples were homogenized with the Dounce tissue homogenizer (Bellco Glass Inc., Vineland, NJ, USA) in 1 ml homogenization buffer (20 mM HEPES, 1 mM EDTA, 250 mM sucrose) containing protease inhibitor cocktail (Roche Diagnostics GmbH, Mannheim, Germany). Total protein concentration was determined using the Lowry method. Protein (30 μg) were separated by electrophoresis through a 12% SDS-polyacrylamide gel, and transferred to nitrocellulose membrane (Millipore Corp., Bedford, MA). Antibodies against CaT-Like, Calbindin, SERCA and PCMA were used in a 1:2000 dilution, detected with anti-rabbit-IgG conjugated with horseradish peroxidase, and visualized using the ECL Western Blot Detection Kit (PerkinElmer, Boston, MA). All antibodies recognized the target proteins at the expected molecular weight. The Cat-Like immunoreaction could be blocked in the presence of the specific antigenic peptide (IINRGLEDGESWEYQI).
Immunohistochemistry
Immunohistochemistry was used to determine the localization of the proteins involved in calcium transport. This was performed on 8 μm thick sections of fixed frozen parotid and submandibular gland samples. Briefly, sections were washed in PBS, permeabilized with 0.1% BSA+0.3% Triton-X 100 in PBS and blocked for 30 min in 3% milk powder (0.5% fat) in PBS. Then they were incubated with the primary antibody in PBS+1% BSA overnight at 4°C. Primary antibodies were used against PMCA-1,-2 and -4, SERCA-2, SERCA-3, Na+/K+-ATPase β-subunit (Affinity BioReagents, Golden, CO, USA); CaT-Like (kindly provided by V. Flockerzi); and calbindin-2 (Sigma, St. Louis, MS). After permeabilizing, the sections were incubated once again with the secondary antibody for 90 min at 25°C in the dark. Secondary anti-IgG and IgM antibodies (goat-anti-rabbit, donkey-anti-rabbit, and goat-anti-mouse) were conjugated with Alexa488 or Alexa555 (Molecular Probes, Eugene, OR, USA) or Cy3 (Jackson Immuno Research, West Grove, PA, USA). Nuclei were stained with DAPI. Images were made using an Axiophot fluorescence microscope (Zeiss, Jena, Germany) equipped with a digital photo camera AxiCam (Zeiss).
Statistical analysis
Data are expressed as means ± SD. Statistical analysis was performed using Student’s unpaired t-test. P values less than 5% were considered statistically significant. All analyses were performed using Origin 6.0 software (Microcal Software Inc., Northhampton, MA, USA).
Results
RNA expression of calcium transport genes
The expression of genes coding for calcium entry channel (CaT family), intracellular calcium binding (calbindin family), calcium sequestration (SERCA family), and calcium efflux (PMCA and NCX family) was investigated in human parotid and submandibular gland. Fragments obtained were characterized by their molecular weight and by sequence homology with the expected product. As shown in Table 2, CaT-Like was expressed in 91% of the parotid samples and 78% of the submandibular samples, while CaT2 mRNA was not detected. From the members of the calcium binding protein family only calbindin-2 was detected in the parotid as well as in the submandibular gland, with comparable high frequencies (94% vs. 83%, respectively). Expression of endoplasmic reticulum Ca2+-ATPase (SERCA) was found in both, parotid and submandibular glands. SERCA-2 expression was found in parotid (89%) and submandibular (86%) glands, while SERCA-3 expression in these salivary glands was 68 and 81%, respectively. None of the samples expressed SERCA-1. PMCA-1, PMCA-2 and PMCA-4 were expressed in most tissue samples. The frequency varied between 97 and 67%. No significant difference was observed between parotid and submandibular glands. Interestingly, in none of the salivary gland samples mRNA for members of the sodium/calcium exchanger (NCX) family was found. Relative expression of all transport channels and transporters did also not show any difference between parotid gland and submandibular gland.
Immunohistochemical localization of epithelial calcium transport proteins
Figure 1 shows the immunoreactions observed with a specific antibody against CaT-Like isoform. Immunhistochemistry using antibodies directed against other CaT1 isoforms did not show any reaction. As shown in Fig. 1a and d, the specific antibody against CaT-Like stains the basolateral membrane of parotid and submandibular acini. The specificity of the antibody used was confirmed by competition analyses with the antigenic peptide (Fig. 1b, e) in which CaT-Like staining was completely abolished. Figure 2 shows colocalization studies with the marker for basolateral membranes, Na+/K+-ATPase. The overlay in Fig. 2c clearly shows identical localization within the cell. The localization of calbindin-2 is shown in Fig. 3. A rather strong fluorescence is seen in parotid and submandibular glands, it fills the whole cell in a cloudlike pattern. Figure 4 illustrates the reaction of acini with an antibody against SERCA-2. The fluorescence signal observed is arranged in dense clusters in the cytosol of the basal cell pole. Preliminary results using a SERCA-3 antibody revealed colocalization of the staining with SERCA-2 distribution (data not shown). PMCA-1, -2 and -4 are located on the apical membrane. PMCA-2 shows a starfish like structure in the centre of the acini, the “arms” reaching deep between the cells (Fig. 5). To confirm the apical localization of PCMA-2, staining with an antibody against Na+/K+-ATPase, a marker of basolateral membranes, was used. As shown in Fig. 6, PMCA-2 is located in the apical membranes and the secretory canaliculi between the acinar cells and does not colocalize with the Na+/K+-ATPase, which as expected is observed on the basolateral membrane.
PMCA-2 staining in human parotid (a, b) and submandibular (c, d) salivary glands. Labeling of the apical membrane and secretory canaliculi is present in the acini. Secondary antibody labeled with AlexaFluor488 (green) or Alexa Fluor555 (red). b and d show controls without primary antibody. Magnifications: ×400. Scale bar 20 μm
Costaining of PMCA-2 and Na+/K+-ATPase β-subunit in human salivary glands. a and b parotid gland and c and d submandibular gland. Labeling of Na+/K+-ATPase β-subunit is seen in basolateral membrane in both glands (green), PMCA2 staining is shown in the apical membrane and secretory canaliculi (red). b and d show controls incubated without primary antibody. Magnification: 630×. Scale bar 20 μm
Proposed model of calcium secretion in human salivary glands
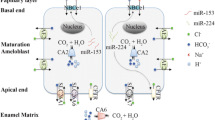
Figure 7 summarizes the distribution of the calcium channels and transport systems obtained in the present study. Since no significant differences in expression or cellular location were found between parotid and submandibular glands, the scheme presented here for the transepithelial transport of calcium applies to both of them. The proposed model can be summarized as follows: (1) calcium enters the acinar cell at the basolateral site via calcium channel CaT-Like (calcium influx); (2) intracellular calcium is taken up into the endoplasmic reticulum by SERCA-2 and possibly SERCA3 or bound to calbindin-2 (intracellular calcium pool); and (3) calcium is secreted by PMCAs on the apical plasma membrane (calcium efflux).
Proposed model of calcium secretion in human salivary gland acinar cells. Expression of calcium channels and transport proteins were analyzed by RT-PCR. Its localization was assessed by immunohistochemistry. CaT-Like, calcium channel 1; CALB-2, calbindin-2; SERCA-2, sarcoplasmic reticulum calcium pump; PMCA, plasma membrane calcium ATPase
Discussion
The present study delineates for the first time a mechanism of transepithelial calcium transport in human salivary parotid and submandibular glands using immunohistochemistry techniques and molecular biology. Comparable RT-PCR data expression of all genes investigated has already been reported in rat salivary glands (Melvin et al. 2005), we confirm their presence for human salivary glands. The experiments performed here faced several obstacles. First of all, saliva contains a high concentration of RNAses, which, if not the necessary precautions are taken, can destroy mRNA very rapidly. Thus, several glands gave no result at all due to the fact that the time span between resection, mincing and immersion in the appropriate RNAse inhibitor containing solutions was too long. Another point of concern was the state of the tissue adjacent to the diseased tissue. In some cases, although the tissue looked macroscopically normal, the expression pattern for the transport systems was changed dramatically, whereas the expression of the housekeeping genes GAPDH, β-actin and Na+/K+-ATPase was very reproducible. Such alterations may be the reason for the scatter observed for the amount of RT-PCR products generated and that the frequency of positive results was less than 100%.
One of the most striking findings in the immunohistochemical investigations is the basolateral localization of CaT-Like. CaT-Like is specifically expressed in placenta, pancreatic acinar cells, prostate and salivary glands (Peng et al. 2000; Wissenbach et al. 2001; Zhuang et al. 2002). Until now the role of CaT-Like in salivary glands has not yet been studied. Basolateral calcium influx in rat salivary glands has been functionally characterized as store-operated calcium entry (Ambudkar 2000). However, the molecular basis of this channel was not identified. Later the molecule was proposed to be member of the transient receptor potential (TRP) gene family (Petersen et al. 1999; Petersen and Fedirko 2001; Hoenderop et al. 2003; Nijenhuis et al. 2003). CaT-Like belongs to the same family (Hirnet et al. 2003). It codes for a calcium-selective channel (TRPV6_Human, GenBank NM_018646). Interestingly, CaT-Like is abundantly expressed in tissues with exocrine functions but not in absorptive tissues, such as intestine and kidney (Wissenbach et al. 2001). This study shows that in human salivary gland this protein is localized on the basolateral membrane, suggesting an important physiological role for calcium influx into the acinar cells.
The sarcoplasmic reticulum calcium pump (SERCA) has been found to be expressed in salivary gland cells (Lee et al. 1997; Meehan et al. 1997). The primary function of SERCA appears to maintain an intracellular calcium pool. In addition, it is assumed that SERCA-2 mediates a kind of transcellular tunneling of calcium (Petersen 2003). This evidence has been derived from the functional data obtained in pancreatic acini and in isolated salivary glands (Ambudkar 2000). In the salivary gland, however, calbindin also appears to assume a role in intracellular calcium shuttling. The calbindin pathway has been reported in small intestine and kidney (Hoenderop et al. 2005). These data are in concordance with the results obtained in the present study, suggesting an important role of SERCA and calbindin in the regulation of the intracellular calcium pool in human salivary glands.
Another important finding of this study is the localization of PMCA-1, -2 and -4 in salivary glands. The localization of PMCA on the apical plasma membranes of the acini, but not on the basolateral membranes, leads to the asymmetry of transport properties of the two membrane areas required for transepithelial transport (Kinne 1991). Our data demonstrate that PMCA constitutes the major calcium efflux pathway in human parotid and submandibular salivary glands. The absence of NCX expression correlates with the findings of other authors (Ambudkar 2000; Melvin et al. 2005). In addition, apical membrane localization of PMCA-2 has also been reported in other exocrine cells, such as the mammary gland (Reinhardt and Horst 1999; Reinhardt et al. 2000) and pancreas (Lee et al. 1997). Our results suggest that calcium transport across human salivary gland acinar cells is an active transcellular process that plays an important role in salivary calcium secretion.
The potential clinical relevance of the data shown in the present study is worth considering in more detail. It is evident that in other organs the transport systems found in the acinar cells are subjected to hormonal regulation. Such control is clearly established for vitamin D in intestine (Wood et al. 2001) and kidney (van Baal et al. 1999; Hoenderop et al. 2001), and for prolactin in the mammary gland (Shennan and Peaker 2000) to give a few examples. If the appropriate receptors were present in the salivary gland a variation in salivary calcium secretion depending on the hormonal status might be expected. Furthermore, local factors—such as presence of diseased tissue in the neighborhood—appear to influence the expression of the transporters and thus might also affect calcium secretion into saliva.
In conclusion, we propose a model of calcium transport and calcium secretion in human salivary glands. This model can be summarized as follows: (1) calcium enters the acinar cell at the basolateral site via calcium channel CaT-Like (calcium influx); (2) intracellular calcium is taken up into the endoplasmatic reticulum by SERCA-2 and possibly SERCA3 or bound to calbindin-2 (intracellular calcium pool); and (3) calcium is secreted by PMCA on the apical plasma membrane (calcium efflux). In closing, a detailed analysis of the various gene expressions described here, regarding calcium secretion into saliva and the development of dental caries should be pursued further. Similarly, physiological investigations on intact salivary glands are required to confirm the proposed model in vivo.
References
Ambudkar IS (2000) Regulation of calcium in salivary gland secretion. Crit Rev Oral Biol Med 11:4–25
van Baal J, Hoenderop JGJ, Groenendijk M, van Os CH, Bindels RJM, Willems PH (1999) Hormone-stimulated Ca2+ transport in rabbit kidney: multiple sites of inhibition by exogenous ATP. Am J Physiol Renal Physiol 277:F899–F906
Edgar WM, Higham SM (1995) Role of saliva in caries models. Adv Dent Res 9:235–238
Hirnet D, Olausson J, Fecher-Trost C, Bodding M, Nastainczyk W, Wissenbach U, Flockerzi V, Freichel M (2003) The TRPV6 gene, cDNA and protein. Cell Calcium 33:509–518
Hoenderop JG, Willems PH, Bindels RJ (2000) Toward a comprehensive molecular model of active calcium reabsorption. Am J Physiol 278:F352–F360
Hoenderop JG, Muller D, Van Der Kemp AW, Hartog A, Suzuki M, Ishibashi K, Imai M, Sweep F, Willems PH, Van Os CH, Bindels RJ (2001) Calcitriol controls the epithelial calcium channel in kidney. J Am Soc Nephrol 12:1342–1349
Hoenderop JG, Nilius B, Bindels RJ (2002) ECaC: the gatekeeper of transepithelial Ca2+ transport. Biochim Biophys Acta 1600:6–11
Hoenderop JG, Nilius B, Bindels RJM (2003) Epithelial calcium channels: from identification to function and regulation. Eur J Physiol 446:304–308
Hoenderop JG, Nilius B, Bindels RJ (2005) Calcium absorption across epithelia. Physiol Rev 85:373–422
Hoyer I, Gaengler P, Bimberg R (1984) In vivo remineralization of human enamel and dental calculus formation. J Dent Res 63:1136–1139
Kinne RKH (1991) Selectivity and direction: plasma membranes in renal transport. Am J Physiol 260:F153–F162
Lee MG, Xu X, Zeng W, Diaz J, Kuo TH, Wuytack F, Racymaekers L, Muallem S (1997) Polarized expression of Ca2+ pumps in pancreatic and salivary gland cells. J Biol Chem 272:15771–15776
Mass E, Gadoth N, Harell D, Wolff A (2002) Can salivary composition and high flow rate explain the low caries rate in children with familial dysautonomia? Pediatr Dent 24:581–586
Meehan S, Wu AJ, Kang EC, Sakai T, Ambudkar IS (1997) Interferon-gamma induces a decrease in the intracellular calcium pump in a human salivary gland cell line. Am J Physiol 273:C2030–C2036
Melvin JE, Yule D, Shuttleworth T, Begenisich T (2005) Regulation of fluid and electrolyte secretion in salivary gland acinar cells. Annu Rev Physiol 67:445–469
Nijenhuis T, Hoenderop JG, Nilius B, Bindels RJ (2003) (Patho)physiological implications of the novel epithelial Ca2+ channels TRPV5 and TRPV6. Pflugers Arch 446:401–409
Pearce E (1998) Plaque minerals and dental caries. New Zealand Dent J 94:12–15
Peng JB, Chen XZ, Berger UV, Vassilev PM, Tsukaguchi H, Brown EM, Hediger MA (1999) Molecular cloning and characterization of a channel-like transporter mediating intestinal calcium absorption. J Biol Chem 274:22739–22746
Peng JB, Chen XZ, Berger UV, Weremowicz S, Morton CC, Vassilev PM, Brown EM, Hediger MA (2000) Human calcium transport protein CaT1. Biochem Biophys Res Commun 278:326–332
Peng JB, Brown EM, Hediger MA (2003) Epithelial Ca2+ entry channels: transcellular Ca2+ transport and beyond. J Physiol 551:729–740
Petersen OH, Burdakov D, Tepikin AV (1999) Regulation of store-operated calcium entry: lessons from a polarized cell. Eur J Cell Biol 78:221–223
Petersen OH, Fedirko NV (2001) Calcium signalling: store-operated channel found at last. Curr Biol 11:R520–R523
Petersen OH (2003) Localization and regulation of Ca2+ entry and exit pathways in exocrine gland cells. Cell Calcium 33:337–344
Reinhardt TA, Horst RL (1999) Ca2+ -ATPases and their expression in the mammary gland of pregnant and lactating rats. Am J Physiol 276:C796–C802
Reinhardt TA, Filoteo AG, Penniston JT, Horst RL (2000) Ca(2+)-ATPase protein expression in mammary tissue. Am J Physiol 279:C1595–C1602
Sewon L, Makela M (1990) A study of the possible correlation of high salivary calcium levels with periodontal and dental conditions in young adults. Arch Oral Biol 35(Suppl):211S–212S
Shennan DB, Peaker M (2000) Transport of milk constituents by the mammary gland. Physiol Rev 80:925–951
Simon DB, Lu Y, Choate KA, Velazquez H, Al-Sabban E, Praga M, Casari G, Bettinelli A, Colussi G, Rodriguez-Soriano J, McCredie D, Milford D, Sanjad S, Lifton RP (1999) Paracellin-1, a renal tight junction protein required for paracellular Mg2+ resorption. Science 285:103–106
Tanaka M, Kadoma Y (2000) Comparative reduction of enamel demineralization by calcium and phosphate in vitro. Caries Res 34:241–245
Wissenbach U, Niemeyer BA, Fixemer T, Schneidewind A, Trost C, Cavalie A, Reus K, Meese E, Bonkhoff H, Flockerzi V (2001) Expression of CaT-like, a novel calcium-selective channel, correlates with the malignancy of prostate cancer. J Biol Chem 22:19461–19468
Wood RJ, Tchack L, Taparia S (2001) 1,25-Dihydroxyvitamin D3 increases the expression of the CaT1 epithelial calcium channel in the Caco-2 human intestinal cell line. BMC Physiol 1:11
Zhuang L, Peng JB, Tou L, Takanaga H, Adam RM, Hediger MA, Freeman MR (2002) Calcium selective calcium channel, CaT1, is localized in gastrointestinal tract epithelium and is aberrantly expressed in human malignancies. Lab Invest 82:1755–1764
Acknowledgements
We thank S. Rosin-Steiner and T. Stratmann for excellent technical assistance. Tissue samples were kindly provided by Prof. Dr. R. Maerker (Staedtische Kliniken Dortmund, Germany), Prof. Dr. K. Wolff and PD Dr. D. Nolte (Knappschaftskrankenhaus Bochum, Germany), Dr. H. Luckhaupt (St.-Johannes-Hospital Dortmund, Germany), Prof. Dr. T. Deitmer (HNO-Klinik, Klinikum Dortmund, Germany) and PD Dr. Dr. G. Nehse (Staedtische Kliniken Oldenburg, Germany). This work was supported by a Tandem Project of the Max-Planck-Society No. 271. Dr. F. Castañeda provided considerable help in finalizing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Evamaria Kinne-Saffran deceased on 6 December 2002
Rights and permissions
About this article
Cite this article
Homann, V., Kinne-Saffran, E., Arnold, W.H. et al. Calcium transport in human salivary glands: a proposed model of calcium secretion into saliva. Histochem Cell Biol 125, 583–591 (2006). https://doi.org/10.1007/s00418-005-0100-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-005-0100-2