Abstract
Purpose
This study aims to describe the variation and characteristics of vessel density (VD) of the macula and optic disc in the normal eyes of children.
Methods
This was a retrospective study where subjects aged 5–18 years with normal eyes were enrolled. The macula and optic disc were scanned by optical coherence tomography angiography (OCTA). The influences of age, gender, and axial length (AL) on VD were analyzed.
Results
A total of 71 normal eyes from 71 subjects were enrolled. For the macula, the mean VD of fovea, parafovea, and perifovea at superficial retina and deep retina were 20.1%, 50.2%, 49.4%, 36.1%, 53.9%, and 48.1%, respectively. The mean foveal avascular zone (FAZ) was 0.277 mm2. For optic disc, the mean VD of radial peripapillary capillary (RPC) and inside-disc areas were 51.8% and 51.7%, respectively. Significant differences were found between the superior-hemi and inferior-hemi VD of the superficial retinal parafovea, deep retinal perifovea, and perifovea. The fovea VD of the superficial and deep retina and FAZ areas were different between genders. The inside-disc VD was positively correlated with AL, while other VDs had no significant correlation with age and AL.
Conclusions
The parafovea VD of the superficial retina, parafovea, and perifovea of the deep retina had superior-hemi VD; boys had a higher fovea VD and smaller FAZ area than those of girls, the macular VD and peripapillary RPC density were steady for 5–18 year-olds. This study provided useful information for furthering the understanding of the development mode of vessel in children and the OCTA clinical applications in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The normal retinal vascular system is vital for visual function and the potential role of the microvasculature and blood flow in the pathophysiology of vascular retinopathies like retinal vein occlusion [1, 2], diabetic retinopathy [3, 4], optic neuropathies like glaucoma [5,6,7,8], macular disorders [8], and some system disorders [9, 10] have been extensively investigated. Previous studies have suggested that there are abnormalities in ocular blood flow in many ocular disorders and system disorders [11]. However, the lack of a reproducible and relevant in vivo quantitative assessment method has limited the study of both ocular perfusion and their microvascular networks.
Conventionally, fluorescein angiography (FA) has been the gold standard examination for identifying and evaluating the retinal capillary system [12, 13], which has been used in clinical practice for over 50 years. Unfortunately, FA cannot distinguish several important layers of blood vessels in the eye; essentially, only the superficial retina can be seen, as the deep capillary system is poorly visualized with a dye-based angiography system. It also cannot quantify the vessel density and is an invasive examination, which all limit its clinical application and research potential. Compared with FA, optical coherence tomography angiography (OCTA), a recently developed means, can produce images of blood flow that have unprecedented resolution of all the vascular layers of the retina with a rapid, non-invasive fashion [14]. For the macula [8], OCTA is capable of revealing details in the superficial and deep retinal layers and also the choriocapillaris. It allows us to measure quantitatively the vessel density (VD) of the superficial retina, which is defined from inner limiting membrane (ILM) to the inner plexiform layer (IPL), and deep retina, which is defined from the IPL to outer plexiform layer (OPL), as well as the foveal avascular zone (FAZ). For the optic disc [15, 16], VD the of vitreous/retina layer (defined as the layer above the OPL), radial peripapillary capillary (RPC) layer (defined from the ILM to the retinal nerve fiber layer (RNFL)), and choriocapillaris can also be measured quantitatively.
In this way, OCTA offers the possibility of quantifying the vessel perfusion density of different retinal layers. This capability provides new ways for disease description and quantification, revealing the role of vessel perfusion in pathogenesis of disease and development and evaluation of new treatments [14]. Although the clinical benefit of OCTA has yet to be fully elucidated, it has already become evident that there can be preferential ischemia in various retinal vascular diseases such as diabetic retinopathy and retinopathy of prematurity [17, 18]. Therefore, to determine the variation between normal retina VD and disorder VD, it is important to understand the variation and characters in vessel perfusion density in normal eyes in order to validate the abnormal OCTA findings in retinal vascular disorders. Most research has reported the features and characters of microvasculature in adult eyes [19, 20], but few studies have focused on the normal eyes of children. Therefore, there is a need for a study which examines the features and characteristics of microvasculature and the potential factors to influence the vessel perfusion density in normal children’s eyes.
The purposes of the present study were to (1) evaluate and quantify the VD of both the macula and optic disc in normal eyes of children and (2) examine the relative contributions of age, gender, and axial length (AL) to macular and peripapillary vessel perfusion density.
Methods
This research was designed as a retrospective study and was conducted with adherence to the tenets of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Local ethical approval was obtained from the Ethics Committee of Sun Yat-sen Memorial Hospital at Sun Yat-sen University, Guangzhou, China. The inclusion criteria were as follows: (1) individuals aged from 5 to 18 years; (2) a spherical equivalent (SE) within ± 6.00 D; and (3) a best-corrected visual acuity (BCVA) of 20/20 or better. The exclusion criteria were as follows: (1) AL to be less than 22 mm (mm) or longer than 26 mm; (2) intraocular pressure (IOP) higher than 24 mmHg; (3) a history of ocular diseases or previous intraocular surgery; and (4) a history of prematurity, neurologic disease, or systemic disorders that may influence the microvasculature, including diabetes, hypertension, hyperlipidemia, cardiovascular disease, and renal disease.
All ALs were measured by partial coherence interferometry (IOLMaster, Software V5.4 and later, Carl Zeiss Meditec, Inc., Dublin, USA). One random eye was enrolled from all subjects. The patients’ demographic information and ALs were collected and further analyzed. The macula and optic disc VD were obtained by OCTA (RTVue XR Avanti; AngioVue software V2018.0.0.18; Optovue, Inc.) and macular 6 × 6 mm scans, as well as optic disc 4.5 × 4.5 mm scans, were performed in every subject. The characteristics of VD were documented. The difference between superior-hemi and inferior-hemi VD of the macula and peripapillary were analyzed. The potential correlation between vessel perfusion density and age, AL, and gender was also analyzed.
Statistical analysis
The outcomes included the FAZ area, the fovea, parafovea, and perifovea of superficial retina and the deep retina; the RPC density of inside-disc area and peripapillary; and the age, gender, and ALs of study participants. The mean ± standard deviation (SD) was calculated for quantitative variables. The Kolmogorov–Smirnov test was used to evaluate the normality of distribution for all variables. The Kruskal–Wallis test was applied for the comparison of variance for non-normally distributed data. The student t test was applied for the comparison of variance for normally distributed data. Scatter plots were constructed to explore the relationships between VD, age, and AL. Linear regression was used to explore the influence of age and AL on VD. Multiple linear regression modeling was fitted using the stepwise approach with the significance level set at 0.05. A P value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (version 23.0, SPSS, Inc.; Chicago, IL, USA). Figures were drawn using GraphPad Prism software (version 7.0e, GraphPad Software; San Diego, CA, USA).
Results
This study enrolled 71 eyes of 71 subjects, including 32 boys (45.07%) and 39 girls (54.93%). The mean age was 127.19 ± 4.61 months, range 53 to 243 months, the mean AL was 23.52 ± 0.13 mm, range from 21.19 to 25.91 mm. Table 1 summarizes the mean macular vessel density of the enrolled eyes, including fovea, parafovea, and perifovea of the superficial retina and deep retina, and the FAZ area. Meanwhile, Table 2 summarizes the RPC density of inside-disc and peripapillary.
We further analyzed the difference between superior-hemi and inferior-hemi VD of the macula and peripapillary (Table 3), results suggested that the superficial retina parafovea VD and deep retina parafovea and perifovea VD had statistically significant differences between the superior-hemi and inferior-hemi, and the superior-hemi had a higher VD than the inferior-hemi. A comparison of the VD between boys and girls showed that the superficial retina fovea, deep retina fovea, and FAZ area had statistically significant differences between genders, while no difference was found in the parafovea VD and perifovea VD of the superficial retina, parafovea VD, and perifovea VD of deep retina, as well as the RPC density of inside-disc, and peripapillary (Table 4).
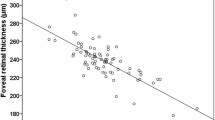
Linear regression analysis revealed that the RPC density of the inside-disc was significantly positively correlated with age and AL (Fig. 1, Table 5), while VD of other areas found no statistically significant correlation with age and AL (Figs. 1 and 2). Stepwise multiple regression analyses were conducted to eliminate collinearity. The model (which included age and AL) accounted for 20% of vessel perfusion density variations of the inside-disc and the AL significantly correlated with the RPC density of inside-disc (Table 5).
Discussion
In recent years, there has been an increasing interest in OCTA as an investigative instrument to study vascular abnormalities in posterior segment eye conditions or ocular signs of system disorders [21,22,23]. However, despite its potential usefulness, the lack of VD data in the normal eyes of children has limited its clinical applications in children. In this study, we evaluated the vessel density of the macula and optic disc by OCTA in the normal eyes of children aged from 5 to 18 years old. We compared the VD between superior-hemi and inferior-hemi of RPC, parafovea, perifovea in the superficial and deep retinas. Moreover, we assessed the correlation between VD of the macula and optic nerve head. In addition, the influence of gender, age, and AL on VD was also assessed.
The macula is one of the most metabolically active tissues; it derives its oxygen supply from multiple retinal capillary plexuses and choriocapillaris [24]. Due to the lack of data in the literature for normal children, we reviewed the previous study of unhealthy eyes of children. Magdalena Niestrata-Ortiz et al. examined 112 diabetic children without DR aged 6–18 years and 30 age-matched controls by measuring FAZ in superficial and deep capillary plexus and they concluded that the FAZ in normal children was significantly smaller than that of diabetic children. The mean FAZ surface area in the deep capillary plexus was 409.8 μm2 in the control group and the mean FAZ surface area in the superficial capillary plexus was 286.4 μm2 in the control group [25]; however, due to the different devices and software used in their study, their results cannot directly compare with this study. The normal eyes of adults have been well studied in previous studies. In Wang Q et al. study [26], they measured the VD of the macula and size of the FAZ in the superficial retinal layer in 105 normal eyes of 105 healthy participants (age 35.9 ± 13.8 years; range from 17 to 64 years); mean FAZ measured 0.35 ± 0.12 mm2, and mean density of superficial retinal small vessel network, superficial retinal capillary network, deep retinal capillary network, and choriocapillaris was 8.54% ± 0.92%, 31.8% ± 2.6%, 45.8% ± 3.3%, 44.4% ± 3.3%, and 44.5% ± 2.7%, respectively. Their results suggested that the density of the macular vascular networks was negatively correlated with age but was independent with AL or subfoveal choroidal thickness. In another study [27], Abtin Shahlaee et al. reported on 163 eyes of 122 subjects (age 41.1 ± 16.46 years, range from 12 to 78 years) and showed that in the parafoveal region, the superficial vascular density was 46% ± 2.2% and the deep vascular density was 52% ± 2.4%. In addition, the vascular density measurements were similar between two eyes and there was no sex difference. They also reported a negative correlation between all retinal regions VD and age after adjusting for signal strength. In Nauman Hashmani et al. [28], 209 eyes of 209 healthy subjects (age 39.6 ± 13.2 years, range from 20 to 75 years) were enrolled, the VD of fovea was the least dense area (32.5% ± 5.9%), and the temporal area was the densest (52.4% ± 4.4%). In their study, a correlation was found between the fovea VD and retinal thickness (r = 0.541, P < 0.001) and males had a greater density at the fovea (P = 0.002). Similarly, to the other study, they also reported that in all retinal regions, the VD was negatively correlated with age after adjusting for AL. Moreover, the mean VD showed steep decline after the age of 50 years. However, in the present study, we found that macular VD had no significant correlation with age or AL, which suggested that age and AL might not be key factors affecting the macular VD in children aged from 5 to 18 years old. Furthermore, in the current study, we found no statistical difference between males and females in the parafovea VD and perifovea VD of superficial or deep retinas, but found statistical difference in the FAZ area, superficial retinal fovea VD, and deep retinal fovea VD. The mean superficial retinal fovea VD and deep retinal fovea VD of boys were greater than those of girls. As expected, the mean FAZ area of boys was less than that of girls. These inconsistencies with previous studies may be explained by differences in instruments, methods of measurement, age range or the number of samples per age group, and ethnicities of the target subjects.
We further examined the VD properties of the optic disc. Analysis showed there was no difference between superior-hemi and inferior-hemi peripapillary RPC. Further analysis showed that the age and AL accounted for 15% and 20% of VD variation of inside-disc RPC density, respectively, while no statistical significance was found with peripapillary RPC density. Stepwise multiple regression analyses were conducted to eliminate collinearity. Model (which included the age and AL) accounted for 20% of the VD variation of inside-disc RPC density. The AL significantly correlated with the inside-disc RPC density. This finding is different to previous studies on adults, which reported that RPC density decreased with the age of the adult [29, 30]. An explanation for this might be that our subjects were aged from 5 to 18 years, and in previous reports, retinal nerve fiber layer (RNFL) thickness was positively correlated with age and axial length in subjects < 15 years old while negatively correlated with age in adult subjects [31, 32]. RNFL is formed by the expansion of the fibers of the optic nerve which form the optic disc. As the RPC networks are nourish peripapillary RNFL, when the RNFL becomes thickened and the areas of RNFL become larger due to AL growth [33], the inside-disc RPC density might become consistently higher [34].
Our study is not without its limitations. First, in this study, we only recruited subjects aged from 5 to 18 years old, because in subjects younger than 5 years old, it was usually hard to acquire good enough quality scans due to poor cooperation, which could impact the accuracy of the acquired VD value calculated from the scanned image. Furthermore, subjects younger than 5 years old with poor cooperation were also not recommend for examination by OCTA in clinical practice. Second, image magnification has been shown to significantly influence the foveal VD [35]. This study did not correct the magnification according to the AL and this may have induced subtle errors and therefore, the data within the superficial retina and fovea must be looked at with caution. It must be noted, however, that most of the enrolled eyes (63 eyes; 80.8%) were within an AL range of 22.02–24.90 mm, which does not seem to be significantly affected by image magnification. Third, the intrasession reproducibility of OCT was reported in some studies [36, 37]. This retrospective study did not test the intrasession reproducibility of measurements, but since the reported intrasession reproducibility was good, the influence of intrasession reproducibility to results may be limited; however, further well-designed studies are warranted to clarify the influence of intrasession reproducibility of OCTA test in childhood. Other limitations of this study include a cross-sectional study design with people of limited ethnic backgrounds, the relatively small samples in age or AL subgroups. Therefore, further well-designed multicenter cohort studies with large samples and different ethnic backgrounds are warranted to further assess normal retinal microvasculature development and determine the physiological factors which can influence retinal VD in different ethnic backgrounds.
Conclusion
This study demonstrated the reference value and characteristics of macular VD and optic disc VD of normal eyes in children. This study found that superficial retinal parafovea VD, deep retinal parafovea VD, and deep retinal perifovea VD had higher superior-hemi density than inferior-hemi, greater fovea VD, and smaller FAZ area in boys than girls, and macular VD or peripapillary RPC density had no significant correlation with age and AL while the inside-disc RPC density was positively correlated with AL. Therefore, the macular VD and peripapillary VD were steady in 5–18-year-olds, and AL should be considered when assessing the inside-disc VD in children. This study provided useful information for further understanding the development mode of vessel in children and the OCTA clinical applications in children.
References
Seknazi D, Coscas F, Sellam A, Rouimi F, Coscas G, Souied EH, Glacet-Bernard A (2018) Optical coherence tomography angiography in retinal vein occlusion: correlations between macular vascular density, visual acuity, and peripheral nonperfusion area on fluorescein angiography. Retina 38(8):1562–1570. https://doi.org/10.1097/IAE.0000000000001737
Chung CY, Tang HHY, Li SH, Li KKW (2018) Differential microvascular assessment of retinal vein occlusion with coherence tomography angiography and fluorescein angiography: a blinded comparative study. Int Ophthalmol 38(3):1119–1128. https://doi.org/10.1007/s10792-017-0570-y
Nesper PL, Roberts PK, Onishi AC, Chai H, Liu L, Jampol LM, Fawzi AA (2017) Quantifying microvascular abnormalities with increasing severity of diabetic retinopathy using optical coherence tomography angiography. Invest Ophthalmol Vis Sci 58(6):BIO307–BIO315. https://doi.org/10.1167/iovs.17-21787
Krawitz BD, Mo S, Geyman LS, Agemy SA, Scripsema NK, Garcia PM, Chui TYP, Rosen RB (2017) A circularity index and axis ratio of the foveal avascular zone in diabetic eyes and healthy controls measured by optical coherence tomography angiography. Vis Res 139:177–186. https://doi.org/10.1016/j.visres.2016.09.019
Zhang S, Wu C, Liu L, Jia Y, Zhang Y, Zhang Y, Zhang H, Zhong Y, Huang D (2017) Optical coherence tomography angiography of the peripapillary retina in primary angle-closure glaucoma. Am J Ophthalmol 182(2):194–200. https://doi.org/10.1016/j.ajo.2017.07.024
Triolo G, Rabiolo A, Shemonski ND, Fard A, Di Matteo F, Sacconi R, Bettin P, Magazzeni S, Querques G, Vazquez LE, Barboni P, Bandello F (2017) Optical coherence tomography angiography macular and peripapillary vessel perfusion density in healthy subjects, glaucoma suspects, and glaucoma patients. Invest Ophthalmol Vis Sci 58(13):5713–5722. https://doi.org/10.1167/iovs.17-22865
Yarmohammadi A, Zangwill LM, Diniz-Filho A, Suh MH, Yousefi S, Saunders LJ, Belghith A, Manalastas PI, Medeiros FA, Weinreb RN (2016) Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in glaucoma. Ophthalmology 123(12):2498–2508. https://doi.org/10.1016/j.ophtha.2016.08.041
Eandi CM, Ciardella A, Parravano M, Missiroli F, Alovisi C, Veronese C, Morara MC, Grossi M, Virgili G, Ricci F (2017) Indocyanine green angiography and optical coherence tomography angiography of choroidal neovascularization in age-related macular degeneration. Invest Ophthalmol Vis Sci 58(9):3690–3696. https://doi.org/10.1167/iovs.17-21941
Bharadwaj AS, Appukuttan B, Wilmarth PA, Pan Y, Stempel AJ, Chipps TJ, Benedetti EE, Zamora DO, Choi D, David LL, Smith JR (2013) Role of the retinal vascular endothelial cell in ocular disease. Prog Retin Eye Res 32:102–180. https://doi.org/10.1016/j.preteyeres.2012.08.004
Amemiya T, Bhutto IA (2001) Retinal vascular changes and systemic diseases: corrosion cast demonstration. Ital J Anat Embryol 106(2 Suppl 1):237–244. https://doi.org/10.1016/j.preteyeres.2012.08.004 10.1159/000115864
Wylegala A (2018) Principles of OCTA and applications in clinical neurology. Curr Neurol Neurosci Rep 18(12):96. https://doi.org/10.1007/s11910-018-0911-x
Fluorescein angiography: insight and serendipity a half century ago. Arch Ophthalmol 129(7):943–948. https://doi.org/10.1001/archophthalmol.2011.160
Buttery RG, Haight JR, Bell K (1990) Vascular and avascular retinae in mammals. A funduscopic and fluorescein angiographic study. Brain Behav Evol 35(3):156–175. https://doi.org/10.1159/000115864
Rodríguez F, Staurenghi G, Gale R (2018) The role of OCT-A in retinal disease management. Graefes Arch Clin Exp Ophthalmol 256(11):2019–2026
Singh A, Agarwal A, Mahajan S, Karkhur S, Singh R, Bansal R, Dogra MR, Gupta V (2017) Morphological differences between optic disc collaterals and neovascularization on optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol 255(4):753–759. https://doi.org/10.1007/s00417-016-3565-x
Akil H, Falavarjani KG, Sadda SR, Sadun AA (2017) Optical coherence tomography angiography of the optic disc; an overview. J Ophthalmic Vis Res 12(1):98–105. https://doi.org/10.4103/2008-322X.200162
Campbell JP, Nudleman E, Yang J, Tan O, Chan RVP, Chiang MF, Huang D, Liu G (2017) Handheld optical coherence tomography angiography and ultra-wide-field optical coherence tomography in retinopathy of prematurity. JAMA Ophthalmol 135(9):977–981. https://doi.org/10.1001/jamaophthalmol.2017.2481
Vinekar A, Chidambara L, Jayadev C, Sivakumar M, Webers CA, Shetty B (2016) Monitoring neovascularization in aggressive posterior retinopathy of prematurity using optical coherence tomography angiography. J AAPOS 20(3):271–274. https://doi.org/10.1016/j.jaapos.2016.01.013
Yip VCH, Wong HT, Yong VKY, Lim BA, Hee OK, Cheng J, Fu H, Lim C, Tay ELT, Loo-Valdez RG, Teo HY, Lim Ph A, Yip LWL (2019) Optical coherence tomography angiography of optic disc and macula vessel density in glaucoma and healthy eyes. J Glaucoma 28(1):80–87. https://doi.org/10.1097/IJG.0000000000001125
Lim CW, Cheng J, Tay ELT, Teo HY, Wong EPY, Yong VKY, Lim BA, Hee OK, Wong HT, Yip LWL (2018) Optical coherence tomography angiography of the macula and optic nerve head: microvascular density and test-retest repeatability in normal subjects. BMC Ophthalmol 18(1):315. https://doi.org/10.1186/s12886-018-0976-y
Bojikian KD, Chen PP, Wen JC (2019) Optical coherence tomography angiography in glaucoma. Curr Opin Ophthalmol 30(2):110–116. https://doi.org/10.1097/ICU.0000000000000554
Gildea D (2018) The diagnostic value of optical coherence tomography angiography in diabetic retinopathy: a systematic review. Int Ophthalmol 67:30–55. https://doi.org/10.1007/s10792-018-1034-8
Borrelli E, Sarraf D, Freund KB, Sadda SR, Khadamy J, Abri Aghdam K, Falavarjani KG (2018) OCT angiography and evaluation of the choroid and choroidal vascular disorders. An update on optical coherence tomography angiography in diabetic retinopathy. Prog Retin Eye Res 67(4):30–55. https://doi.org/10.1016/j.preteyeres.2018.07.002
Provis J, Penfold P, Cornish E, Sandercoe T, Madigan M (2005) Anatomy and development of the macula: specialisation and the vulnerability to macular degeneration. Clin Exp Optom 88(5):269–281
Niestrata-Ortiz M, Fichna P, Stankiewicz W, Stopa M (2019) Enlargement of the foveal avascular zone detected by optical coherence tomography angiography in diabetic children without diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 257(4):689–697. https://doi.org/10.1007/s00417-019-04264-8
Wang Q, Chan S, Yang JY, You B, Wang YX, Jonas JB, Wei WB (2016) Vascular density in retina and choriocapillaris as measured by optical coherence tomography angiography. Am J Ophthalmol 168:95–109. https://doi.org/10.1016/j.ajo.2016.05.005
Shahlaee A, Samara WA, Hsu J, Say EA, Khan MA, Sridhar J, Hong BK, Shields CL, Ho AC (2016) In vivo assessment of macular vascular density in healthy human eyes using optical coherence tomography angiography. Am J Ophthalmol 165:39–46. https://doi.org/10.1016/j.ajo.2016.02.018
Hashmani N, Hashmani S, Murad A, Baig N (2019) Macular vascular density at the superficial capillary plexus using the optical coherence tomography angiography. Clin Ophthalmol 13:295–302. https://doi.org/10.2147/OPTH.S189515
Wang Q, Chan S, Yang J, You B, Wang Y, Jonas J, Wei W (2016) Vascular density in retina and choriocapillaris as measured by optical coherence tomography angiography. Am J Ophthalmol 168:95–109
Pinhas A, Linderman R, Mo S, Krawitz B, Geyman L, Carroll J, Rosen R, Chui T (2018) A method for age-matched OCT angiography deviation mapping in the assessment of disease- related changes to the radial peripapillary capillaries. PLoS One 13(5):e0197062
Hong SW, Ahn YJ, Kang NY (2017) Relationship between age and retinal nerve fiber layer thickness in normal children. Semin Ophthalmol 32(5):655–660. https://doi.org/10.3109/08820538.2016.1157613
Patel NB, Lim M, Gajjar A, Evans KB, Harwerth RS (2014) Age-associated changes in the retinal nerve fiber layer and optic nerve head. Invest Ophthalmol Vis Sci 55(8):5134–5143. https://doi.org/10.1167/iovs.14-14303
Hong S, Ahn Y, Kang N (2017) Relationship between age and retinal nerve fiber layer thickness in normal children. Semin Ophthalmol 32(5):655–660
She X, Guo J, Liu X, Zhu H, Li T, Zhou M, Wang F, Sun X (2018) Reliability of vessel density measurements in the peripapillary retina and correlation with retinal nerve fiber layer thickness in healthy subjects using optical coherence tomography angiography. Ophthalmologica 240(4):183–190
Sampson DM, Gong P, An D, Menghini M, Hansen A, Mackey DA, Sampson DD, Chen FK (2017) Axial length variation impacts on superficial retinal vessel density and foveal avascular zone area measurements using optical coherence tomography angiography. Invest Ophthalmol Vis Sci 58(7):3065–3072. https://doi.org/10.1167/iovs.17-21551
Reibaldi M, Uva M, Avitabile T, Toro M, Zagari M, Mariotti C, Cennamo G, Reibaldi A, Longo A (2012) Intrasession reproducibility of RNFL thickness measurements using SD-OCT in eyes with keratoconus. Ophthalmic Surg Lasers Imaging 43(6 Suppl):S83–S89
Venugopal J, Rao H, Weinreb R, Pradhan Z, Dasari S, Riyazuddin M, Puttiah N, Rao D, Devi S, Mansouri K, Webers C (2018) Repeatability of vessel density measurements of optical coherence tomography angiography in normal and glaucoma eyes. Br J Ophthalmol 102(3):352–357
Funding
This study was funded by the National Natural Science Foundation of China (Grant no.: 81700833).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhang, B., Fan, M. et al. The vascular densities of the macula and optic disc in normal eyes from children by optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol 258, 437–444 (2020). https://doi.org/10.1007/s00417-019-04466-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04466-0