Abstract
Purpose
To present the long-term results of ab externo trabeculotomy in the management of glaucoma secondary to chronic uveitis.
Methods
In this retrospective single-centre case series, medical records of patients with glaucoma secondary to chronic uveitis, who underwent ab externo trabeculotomy, were evaluated. Two definitions of success were used: intraocular pressure (IOP) 6 ≤ IOP ≤ 21 mmHg (success 1) or 6 ≤ IOP ≤ 21 mmHg and at least 25 % reduction from baseline (success 2). Success was complete when no additional medication was required or qualified when additional medication or cycloablative procedures were required to achieve the specific IOP definition.
Results
Twenty-two eyes of 18 patients were included. After 3 years, median IOP decreased from 27 mmHg [range 17–43 mmHg, mean 27.5 mmHg, 95 % confidence interval of the mean (CI) 24.5–30.5 mmHg] to 15 mmHg (range 9–19 mmHg, mean 14.5 mmHg, CI 13–16.1 mmHg). Complete and qualified success 1 was 23 and 45 % after 3 years, respectively. For success 2, the rates were 23 and 32 %, respectively. Hyphema was the most common complication, which resolved completely within 1 month after surgery without further intervention.
Conclusion
Trabeculotomy ab externo was moderately successful in glaucoma secondary to chronic uveitis after 3 years. No sight-threatening complications were observed during the follow-up period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Secondary glaucoma is a common and potentially devastating complication in chronic forms of uveitis [1–3]. In uveitis, a breakdown of the blood-ocular barrier leads to influx of proteins as well as inflammatory and immunocompetent cells, cytokines and chemokines, leading to alteration in the aqueous humor composition [4, 5]. Several mechanisms are involved in the pathogenesis of uveitic glaucoma (UG), including obstruction of the trabecular meshwork (TM) by inflammatory cells and proteins, direct TM tissue damage, formation of anterior synechia, steroid-induced alteration of the TM function, and neovascularization [6]. Management of UG is challenging. Considering the limitations of the medical antiglaucoma therapy, surgery is often required to achieve a significant and sustained lowering of the intraocular pressure (IOP) [7]. Different approaches have been proposed in the surgical treatment of refractory UG, such as transscleral diode laser cyclophotocoagulation (TDLC), trabeculectomy with and without antimetabolites, deep sclerectomy and glaucoma drainage devices [8–22]. To our knowledge, the role of trabeculotomy ab externo in UG has not yet been described. A major advantage of the procedure is that it improves outflow facility without the need of external fistulation with its bleb-related complications. In the present study, the efficacy and safety of ab externo trabeculotomy in the treatment of glaucoma secondary to chronic uveitis were investigated.
Patients and methods
In this study, all medical records of consecutive patients with UG who underwent ab externo trabeculotomy between June 2004 and May 2011 in the Centre for Ophthalmology at the University Hospital Tübingen, were reviewed. Glaucoma was defined as the presence of either glaucomatous optic disc damage and/or glaucomatous visual field defect according to the guidelines of the European Glaucoma Society. In all patients, surgery was required because of uncontrolled IOP on maximal tolerated glaucoma medications. If cycloablative procedures had been performed first, trabeculotomy was performed after at least 4 weeks. We documented age at surgery, gender, preoperative and postoperative best corrected visual acuity (BCVA), IOP, number of glaucoma medications and postoperative complications for each patient. Two definitions of success were used: 6 mmHg ≤ IOP ≤ 21 mmHg (success 1) and 6 mmHg ≤ IOP ≤ 21 mmHg and at least 25 % reduction from baseline (success 2). If after glaucoma surgery further glaucoma medication was required, the outcome was described as a qualified success, and when the patient was free of glaucoma medication after the surgery, the outcome was considered a complete success. If cycloablative procedures were needed to control the IOP postoperatively, this was considered as qualified success. Failure of the procedure was defined as IOP > 21 mmHg at 2 consecutive visits despite re-introduction of glaucoma medications, which required further surgical interventions such as filtering surgery or the implantation of an Ahmed glaucoma valve. In these eyes, the examination before the reoperation was considered as the final follow-up examination for the patient.
This work adhered to the tenets of the Declaration of Helsinki. According to German legislation and the requirements of the local institutional review board (IRB), completely anonymized data was used for this study.
Operative technique
Uveitis was inactive for at least 3 months in all eyes before surgery. All patients received systemic body weight-adjusted oral steroid therapy starting with 1 mg per kg 5 days prior to surgery. Steroids were tapered over 10–12 weeks after surgery.
The surgical procedure followed the technique described previously [23]. Briefly, after conjunctival incision, a 4 × 4-mm scleral flap at four-fifths thickness was created at the corneal limbus. The Schlemm’s canal was identified and de-roofed. U-shaped probes were then inserted into both ends of the opened canal and rotated 90 degrees against the trabecular meshwork. Rotation of the probes achieved at least a 120-degree opening of the trabecular meshwork. The scleral flap was then closed watertight. Postoperative treatment comprised topical administration of combined antibiotic corticosteroid medication for 2 weeks. Pilocarpine 1 % was given postoperatively for 4 weeks to avoid formation of peripheral anterior synechia.
Statistical analysis
For statistical analysis, chi-squared tests, Fisher’s exact test, and rank-sum tests were performed using JMP software (version 11.0, SAS Institute Inc., Cary, NC, USA). Values of p less than 0.05 were considered to reflect statistically significant differences.
Results
Demographics
Twenty-two eyes of 18 patients were included in the study. Demographic characteristics of the patients are summarized in Table 1. Systemic immunosuppressive medication included prednisolone, methotrexate, mycophenolate mofetil and mycophenolate sodium, adalimumab, and azathioprine.
Ocular pressure and antiglaucoma medications
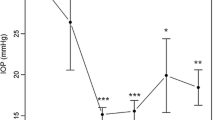
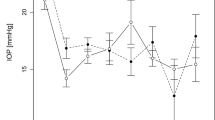
Median IOP decreased significantly from 27 mmHg (range 17–43 mmHg, mean 27.5 mmHg, 95%CI 24.5–30.5 mmHg) at baseline to 15.0 mmHg (range 9–19 mmHg, mean 14.5 mmHg, CI 13–16.1 mmHg) after 3 years (p < 0.001, Fig. 1). Figure 2 shows the median IOP at different time points.
Median IOP at different time points. The decrease in median IOP was statistically significant for all time points compared to the baseline value. The whiskers represent the range of IOP. One eye with an IOP of 31 mmHg at one visit at the 1-year follow up was treated with a cycloablative procedure, which was able to control IOP during further follow up. Similarly, one eye had an IOP of 24 mmHg at one visit at the 2-year follow up. The IOP could be controlled with additional anti-glaucoma medication. Eyes with failure were not included
The median number of antiglaucoma medications decreased from 5 (range 3–5, CI 4.2–5.0) at baseline to 1 (range 0–3, CI 0.5–1.7) after 3 years (p < 0.001). Combination glaucoma medications were enumerated as individual medications. Thirteen patients (13 eyes) received systemic acetazolamide prior to surgery. In these cases, acetazolamide was enumerated as an individual medication. No patient received acetazolamide after surgery.
Success
Table 2 shows the success results. Interestingly, if complete success was achieved, it fulfilled the stricter criteria (success 2) in all cases. Three eyes required one cycloablative procedure within 6 months after surgery. One eye required two cycloablative procedures after 6 and 12 months. IOP was controlled in all of these eyes. They were considered as qualified successes.
Seven eyes were considered as failures. Failure occurred within the first 3 months in six eyes and after 7 months in one eye. In all these eyes, an Ahmed glaucoma valve was implanted. The uveitis remained inactive and the immunosuppressive therapy did not need to be intensified during the study period in all patients.
Complications
Complications are presented in Table 3. We did not observe any sight-threatening complications after 3 years of follow-up.
Discussion
Glaucoma is a common, potentially sight-threatening complication of chronic uveitis. The reported incidence of UG is between 6.5 and 46 % [1, 2, 24, 25]. It increases in the course of chronic uveitis from 6.5 % after 1 year to 22.3 % after 10 years [25]. Surgical treatment is often required to control IOP in UG. Transscleral diode cyclophotocoagulation, deep sclerectomy, trabeculectomy with and without antimetabolites, and glaucoma drainage devices have been used with variable success.
Schlote et al. reported a success rate of 77.2 % after 1 year for TDLC in the treatment of UG. Similar results were reported for patients with Fuchs uveitis syndrome (FUS) [20, 22]. However, more than one TDLC treatment was necessary to achieve success in the majority of eyes. Also, the efficacy of TDLC seems to depend on the type of uveitis. Heinz et al. reported a failure rate of 68 % for TDLC in a series of 21 eyes with glaucoma secondary to juvenile idiopathic arthritis. Interestingly, in the present study, failure was more common in patients with FUS (four of five eyes) and granulomatous uveitis (two of two eyes). However, while different treatment approaches might produce different results depending on the type of uveitis, the small number of eyes in the various uveitis subgroups in our study does not allow for further statistical analysis.
Non-penetrating deep sclerectomy (NPDS) is another option in the treatment of UG. It has been introduced to avoid bleb-related postoperative complications of filtration surgery. Dupas et al. reported in a prospective comparative study similar success rates for NPDS and trabeculectomy in UG after 1 year. However, deep sclerectomy patients required significantly more postoperative adjustments in the form of goniopuncture or needling to achieve success compared to the trabeculectomy group [12]. Similar results were reported by others as well [8, 26]. However, there are no sufficient long-term data of deep sclerectomy in the treatment of UG. One study reported a success rate of 18.9 % after 30 months, which is lower than the success rates for trabeculotomy ab externo in the current study [27].
Trabeculectomy with or without antimetabolites has also been studied in patients with UG. Promising results with success rates of 90 and 79 % after 1 and 2 years, respectively, have been reported for trabeculectomy with mitomycin C [9, 18]. Stavrou et al. reported a qualified success rate of 78 % (IOP ≤ 21 mmHg) in a case series of 32 eyes with UG after 5 years [21]. However, patients with UG more often develop a cystic bleb and require significantly more postoperative procedures compared to patients with primary open-angle glaucoma [18]. Also, the incidence of potentially sight-threatening complications like persistent postoperative hypotony and hypotony maculopathy is considerably higher in uveitic patients [16].
Glaucoma drainage devices (GDDs) are an alternative approach in the treatment of uncontrolled UG. Ceballos et al. reported a success rate of 91.7 % with the Baerveldt glaucoma drainage device after 2 years [10]. Very promising results have been reported for the Molteno implant with a success rate of 75 % after 10 years [17]. Papadaki et al. showed good results for the Ahmed glaucoma valve in UG with success rates of 77 and 50 % after 1 and 4 years, respectively [19]. However, high success rates of GDD go along with possible serious postoperative complications like postoperative hypotony, hypotony maculopathy, choroidal effusion and corneal endothelium dysfunction [10, 17, 28]. Also, the postoperative Tenon cyst formation is considered a rate-limiting step in the success of glaucoma implant surgery [29–32]. The reported incidence of the encapsulated bleb formation ranges between 23 and 42.8 % [30, 32]. Gil-Carrasco et al. reported that encapsulated blebs tend to occur in young patients (range 22–44 years), which corresponds to the typical age of patients with UG [30].
In a recent study, Anton et al. showed that trabeculectomy ab interno with the Trabectome® can be used in patients with UG. The short-term results showed an IOP reduction of approximately 40 % and a medication reduction from 2 to 0.67. These results are similar to the efficacy of the current study. However, comparison is difficult because of heterogenic study populations and somewhat different success criteria [33].
Compared to the above surgical techniques, trabeculotomy ab externo was moderately successful as a stand-alone procedure in our case series. However, the use of glaucoma medications or cycloablative procedures improved the success rates considerably. The majority of treatment failures in the current study occurred within the first 3 months after surgery. Most of these patients were under the age of 30 years (4/7, range 15–43 years), and had either FUS (four eyes) or granulomatous uveitis (two eyes). A possible explanation for early failure in these cases might be secondary structural abnormalities in the Schlemm’s canal and the collecting channels associated with longstanding uveitis. Younger age is also a possible reason for failure, considering that an age below 30 years is a well-known risk factor for failure in glaucoma surgery [34, 35]. It should also be considered that FUS differs from other uveitic forms in its unilaterality, absence of acute symptoms and the mild anterior chamber inflammation which is irresponsive to steroids [36]. It is, therefore, possible that the specific features of FUS lead to different results of glaucoma treatment in these patients compared to glaucoma secondary to other uveitis entities.
The high safety profile of trabeculotomy ab externo is a major advantage of the procedure compared to filtration surgery. The most common complication in our study was the postoperative hyphema, which resolved completely within 1 month without any further intervention in all cases. Actually, one could argue if hyphema is a complication of the procedure at all since it could be interpreted as a sign of patency of the Schlemm’s canal and the collector channels. Postoperative hypotony is a feared complication of filtration surgery. In the current study, one eye (5 %) developed early postoperative hypotony which was controlled and resolved after a single injection of sodium hyaluronate in the anterior chamber.
A drawback of the current study is its retrospective design. The decision for a surgical intervention was purely at the individual surgeon’s discretion. Additionally, a variety of UG types and a broad spectrum of disease severity were treated. This precluded determination of prognostic indicators for success and failure. Also, both eyes were treated in four patients, which can be a confounder of results. Further, prospective studies are warranted to better evaluate the role of the procedure in the treatment paradigm for UG.
In conclusion, this study demonstrated a moderate success rate and a high safety profile of ab externo trabeculotomy in patients with UG after 3 years. A major advantage of ab externo trabeculotomy in the treatment of UG is that it improves outflow facility and restores the physiological pathway of the aqueous humor outflow without the need of external fistulation with its bleb-related complications. Success rates can be improved using glaucoma medication or cycloablative procedures.
References
Merayo-Lloves J, Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS (1999) Secondary glaucoma in patients with uveitis. Ophthalmologica 213:300–304
Panek WC, Holland GN, Lee DA, Christensen RE (1990) Glaucoma in patients with uveitis. Br J Ophthalmol 74:223–227
Takahashi T, Ohtani S, Miyata K, Miyata N, Shirato S, Mochizuki M (2002) A clinical evaluation of uveitis-associated secondary glaucoma. Jpn J Ophthalmol 46:556–562
Deuter CM, Klinik T, Muller M, Geerling G, Zierhut M (2010) Secondary glaucoma in uveitis. Ophthalmologe 107:427–434
Heinz C, Pleyer U, Ruokonnen P, Heiligenhaus A (2008) Secondary glaucoma in childhood uveitis. Ophthalmologe 105:438–444
Moorthy RS, Mermoud A, Baerveldt G, Minckler DS, Lee PP, Rao NA (1997) Glaucoma associated with uveitis. Surv Ophthalmol 41:361–394
Sung VC, Barton K (2004) Management of inflammatory glaucomas. Curr Opin Ophthalmol 15:136–140
Auer C, Mermoud A, Herbort CP (2004) Deep sclerectomy for the management of uncontrolled uveitic glaucoma: preliminary data. Klin Monatsbl Augenheilkd 221:339–342
Ceballos EM, Beck AD, Lynn MJ (2002) Trabeculectomy with antiproliferative agents in uveitic glaucoma. J Glaucoma 11:189–196
Ceballos EM, Parrish RK 2nd, Schiffman JC (2002) Outcome of Baerveldt glaucoma drainage implants for the treatment of uveitic glaucoma. Ophthalmology 109:2256–2260
Chawla A, Mercieca K, Fenerty C, Jones NP (2013) Outcomes and complications of trabeculectomy enhanced with 5-fluorouracil in adults with glaucoma secondary to uveitis. J Glaucoma 22:663–666
Dupas B, Fardeau C, Cassoux N, Bodaghi B, LeHoang P (2010) Deep sclerectomy and trabeculectomy in uveitic glaucoma. Eye (Lond) 24:310–314
Heinz C, Koch JM, Heiligenhaus A (2006) Transscleral diode laser cyclophotocoagulation as primary surgical treatment for secondary glaucoma in juvenile idiopathic arthritis: high failure rate after short term follow up. Br J Ophthalmol 90:737–740
Hill RA, Nguyen QH, Baerveldt G, Forster DJ, Minckler DS, Rao N, Lee M, Heuer DK (1993) Trabeculectomy and molteno implantation for glaucomas associated with uveitis. Ophthalmology 100:903–908
Iwao K, Inatani M, Seto T, Takihara Y, Ogata-Iwao M, Okinami S, Tanihara H (2014) Long-term outcomes and prognostic factors for trabeculectomy with mitomycin C in eyes with uveitic glaucoma: a retrospective cohort study. J Glaucoma 23:88–94
Kaburaki T, Koshino T, Kawashima H, Numaga J, Tomidokoro A, Shirato S, Araie M (2009) Initial trabeculectomy with mitomycin C in eyes with uveitic glaucoma with inactive uveitis. Eye (Lond) 23:1509–1517
Molteno AC, Sayawat N, Herbison P (2001) Otago glaucoma surgery outcome study: long-term results of uveitis with secondary glaucoma drained by molteno implants. Ophthalmology 108:605–613
Noble J, Derzko-Dzulynsky L, Rabinovitch T, Birt C (2007) Outcome of trabeculectomy with intraoperative mitomycin C for uveitic glaucoma. Can J Ophthalmol 42:89–94
Papadaki TG, Zacharopoulos IP, Pasquale LR, Christen WB, Netland PA, Foster CS (2007) Long-term results of Ahmed glaucoma valve implantation for uveitic glaucoma. Am J Ophthalmol 144:62–69
Schlote T, Derse M, Zierhut M (2000) Transscleral diode laser cyclophotocoagulation for the treatment of refractory glaucoma secondary to inflammatory eye diseases. Br J Ophthalmol 84:999–1003
Stavrou P, Murray PI (1999) Long-term follow-up of trabeculectomy without antimetabolites in patients with uveitis. Am J Ophthalmol 128:434–439
Voykov B, Deuter C, Zierhut M, Leitritz MA, Guenova E, Doycheva D (2014) Is cyclophotocoagulation an option in the management of glaucoma secondary to Fuchs’ uveitis syndrome? Graefes Arch Clin Exp Ophthalmol 252:485–489
Tanihara H, Negi A, Akimoto M, Terauchi H, Okudaira A, Kozaki J, Takeuchi A, Nagata M (1993) Surgical effects of trabeculotomy ab externo on adult eyes with primary open angle glaucoma and pseudoexfoliation syndrome. Arch Ophthalmol 111:1653–1661
Heinz C, Koch JM, Zurek-Imhoff B, Heiligenhaus A (2009) Prevalence of uveitic secondary glaucoma and success of nonsurgical treatment in adults and children in a tertiary referral center. Ocul Immunol Inflamm 17:243–248
Neri P, Azuara-Blanco A, Forrester JV (2004) Incidence of glaucoma in patients with uveitis. J Glaucoma 13:461–465
Souissi K, El Afrit MA, Trojet S, Kraiem A (2006) Deep sclerectomy for the management of Uveitic glaucoma. J Fr Ophtalmol 29:265–268
Khairy HA, Green FD, Nassar MK, Azuara-Blanco A (2006) Control of intraocular pressure after deep sclerectomy. Eye (Lond) 20:336–340
Gedde SJ, Singh K, Schiffman JC, Feuer WJ, Tube Versus Trabeculectomy Study G (2012) The tube versus trabeculectomy study: interpretation of results and application to clinical practice. Curr Opin Ophthalmol 23:118–126
Eibschitz-Tsimhoni M, Schertzer RM, Musch DC, Moroi SE (2005) Incidence and management of encapsulated cysts following Ahmed glaucoma valve insertion. J Glaucoma 14:276–279
Gil-Carrasco F, Salinas-VanOrman E, Recillas-Gispert C, Paczka JA, Gilbert ME, Arellanes-Garcia L (1998) Ahmed valve implant for uncontrolled uveitic glaucoma. Ocul Immunol Inflamm 6:27–37
Lai JS, Poon AS, Chua JK, Tham CC, Leung AT, Lam DS (2000) Efficacy and safety of the Ahmed glaucoma valve implant in Chinese eyes with complicated glaucoma. Br J Ophthalmol 84:718–721
Ozdal PC, Vianna RN, Deschenes J (2006) Ahmed valve implantation in glaucoma secondary to chronic uveitis. Eye (Lond) 20:178–183
Anton A, Heinzelmann S, Ness T, Lubke J, Neuburger M, Jordan JF, Wecker T (2015) Trabeculectomy ab interno with the trabectome(R) as a therapeutic option for uveitic secondary glaucoma. Graefes Arch Clin Exp Ophthalmol 251:2753–2760
Costa VP, Katz LJ, Spaeth GL, Smith M, Gandham S (1993) Primary trabeculectomy in young adults. Ophthalmology 100:1071–1076
Investigators A (2002) The advanced glaucoma intervention study (AGIS): 11. Risk factors for failure of trabeculectomy and argon laser trabeculoplasty. Am J Ophthalmol 134:481–498
Bonfioli AA, Curi AL, Orefice F (2005) Fuchs’ heterochromic cyclitis. Semin Ophthalmol 20:143–146
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Voykov, B., Dimopoulos, S., Leitritz, M.A. et al. Long-term results of ab externo trabeculotomy for glaucoma secondary to chronic uveitis. Graefes Arch Clin Exp Ophthalmol 254, 355–360 (2016). https://doi.org/10.1007/s00417-015-3204-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3204-y