Abstract
Background
Diabetic retinopathy (DR) is a major cause of blindness in the working-age populations of developed countries, and effective treatments and prevention measures have long been the foci of study. Patients with DR invariably demonstrate impairments of the retinal microvascular endothelium. Many observational and preclinical studies have shown that angiogenesis and apoptosis play crucial roles in the pathogenesis of DR. Increasing evidence suggests that in DR, the small guanosine-5′-triphosphate-binding protein RhoA activates its downstream targets mammalian Diaphanous homolog 1 (mDia-1) and profilin-1, thus affecting important cellular functions, including cell morphology, motility, secretion, proliferation, and gene expression. However, the specific underlying mechanism of disease remains unclear.
Conclusion
This review focuses on the RhoA/mDia-1/profilin-1 signaling pathway that specifically triggers endothelial dysfunction in diabetic patients. Recently, RhoA and profilin-1 signaling has attracted a great deal of attention in the context of diabetes-related research. However, the precise molecular mechanism by which the RhoA/mDia-1/profilin-1 pathway is involved in progression of microvascular endothelial dysfunction (MVED) during DR has not been determined. This review briefly describes each feature of the cascade before exploring the most recent findings on how the pathway may trigger endothelial dysfunction in DR. When the underlying mechanisms are understood, novel therapies seeking to restore the endothelial homeostasis comprised in DR will become possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
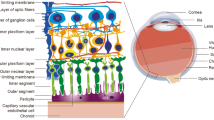
Diabetic retinopathy (DR), a common complication of diabetes, is a leading cause of vision loss [1, 2]. The early non-proliferative stages of DR are characterized by retinal microvascular damage triggering vascular hyperpermeability [2]. The retinal endothelium, which is the intimal lining of blood vessels, forms a barrier between the blood and the interstitium, regulating extravasation of plasma proteins, fluid, and leukocytes [3, 4]. Advances made in recent decades have revealed the complex nature of this semi-permeable membrane, and the key role played by the membrane in the maintenance of vascular homeostasis [5–7]. Appropriate retinal microvascular endothelial function is important in terms of eye homeostasis, and its dysfunction is associated with several pathophysiological conditions, including DR [8–10].
The end-stage of microvascular endothelial dysfunction (MVED) caused by hyperglycemia involves angiogenesis and apoptosis of endothelial cells [11–13]. Angiogenesis, which is the formation of new blood vessels from preexisting vessels, is important in terms of wound healing and in the pathology of many diseases, including tumor development and DR [14]. Angiogenesis is regulated by vascular-specific growth factors that trigger complex intracellular signaling cascades culminating in activation of endothelial cells. The relevant growth factors include vascular endothelial growth factor (VEGF), pigment epithelium-derived factor (PEDF), and RhoA/mammalian Diaphanous homolog 1 (mDia-1)/profilin-1 [15–19].
Recently, an important role of profilin-1 in wound-induced endothelial cell motility has been discovered [20–22]. In mammals, four profilin genes (profilin 1 – 4) have been described to date [23]. Profilin-1 was the first-known family member and is ubiquitously expressed by fungi, plants, certain viruses, and most animal cells except those of skeletal muscle [24, 25]. The roles played by Rho guanosine triphosphatases (GTPases) have been extensively studied in various types of mammalian cells, with the aid of (principally) dominant-negative and constitutively active mutants. The RhoA protein is conserved in evolutionary terms in everything from plants and yeasts to mammals; it acts by binding to and stimulating various downstream targets, including actin nucleators, protein kinases, and phospholipases, (especially mDia-1 and profilin-1) [26]. Although profilin-1 plays important roles in actin polymerization, and RhoA/mDia-1 signaling is involved in endothelial protection, profilin-1 has not yet been clearly shown to engage in angiogenic regulation.
In this review, we summarize the details of the RhoA/mDia-1/profilin-1 signaling involved in MVED caused by hyperglycemia. Our aim is to explore the relationship between DR microvascular endothelial function/dysfunction and the actions of the RhoA/mDia-1/profilin-1 cascade, with a principal focus on cellular and molecular mechanisms as opposed to clinical manifestations.
RhoA
RhoA is the prototypical member of the mammalian Rho subfamily, which has 20 members. The Rho GTPases are 20 to 24 kDa proteins that are essential for appropriate regulation of many cellular functions. The Rho GTPases have been extensively researched, as have Cdc42, Rac1 and other isoforms of G proteins [27–29]. RhoA is a molecular switch that responds to messages from G-protein-coupled receptors and cell surface receptors that bind cytokines, growth factors, and adhesion molecules. The Rho GTPases cycle between inactive guanosine diphosphate (GDP)-bound forms and active guanosine triphosphate (GTP)-bound forms, and their intrinsic hydrolytic activities are affected by various regulators (Fig. 1) [30–33]. Cycling of Rho GTPases between the two states is regulated by three sets of proteins; these are the guanine nucleotide-exchange factors (GEFs), the GTPase-activating proteins (GAPs), and the guanine nucleotide-dissociation inhibitors (GDIs) (Fig. 1) [26].
Focus on the cascade of RhoA/mDia-1/profilin-1 pathway. (1) An inactive RhoA-GDP form switching to an active RhoA-GTP form is regulated by GEF, GAP and GDI, etc. (2) RhoA-GTP binds to the DID part and sequence N-terminal to DID of mDia-1, while profilin-1 binds to the FH1 part of mDia-1. After forming a 1:1 complex with G-actin, profilin-1 modulates actin stress fibers via promoting or preventing actin polymerization. (3) RhoA/ROCK I/II could mediate actin polymerization by regulating profilin-1. Abbreviations: GDP guanosine diphosphate, GTP guanosine triphosphate, GEF guanine nucleotide-exchange factor, GAP GTPase-activating protein, GDI guanine nucleotide-dissociation inhibitor, mDia-1 mammalian Diaphanous homolog 1, DAD diaphanous auto-regulatory domain, FH1/2 formin homology 1/2, CC coil-coiled region, DID Dia-inhibitory domain, ROCK I/II Rho-associated coiled-coil containing protein kinase I/II
Much work performed over the past few decades has suggested that five classical pathways may be closely associated with DR; these are the advanced glycation end products (AGEs), oxidative stress, protein kinase C (PKC), hexosamine, and polyol pathways. In diabetes, RhoA and the receptor for AGEs (RAGE) can form a complex termed RhoA/RAGE, which has been suggested to activate Rho-associated coiled-coil-containing protein kinase (ROCK), resulting in reorganization of the actin cytoskeleton, in turn triggering endothelial cell hyperpermeability [34–36]. A recent study showed that RhoA activity was markedly increased, and endothelial nitric oxide synthase (eNOS) phosphorylation was downregulated by 57 % in retinas of diabetic rats 2 weeks after the onset of diabetes [2, 37]. Interestingly, in other studies, diabetes caused a ROCK-mediated increase in endothelial arginase activity, contributing in part to the impaired nitric oxide (NO) bioavailability characteristic of the disease (Fig. 2) [38, 39].
The crosstalk between RhoA/mDia-1/profilin-1 cascade and five classic pathways that might be closely associated with DR. (1) In diabetic condition, hyperglycemia activates RhoA signaling to interact with a multitude of pathways, e.g., AGEs, PKC, ROS, hexosamine and polyol pathways. (2) RhoA could lead to MVED via junction complexes, such as ZO-1, occludin and claudins, etc. (3) ROCK acts downstream of RhoA to regulate MVED. (4) Some indispensable molecules also participate in the crosstalk, including NF-κB, RAGE, MAPKs, NO, BSA and NADPH, etc. Abbreviations: mDia-1 mammalian Diaphanous homolog 1, ROS reactive oxygen species, AGEs advanced glycation end products, RAGE receptor for AGEs, PKC protein kinase C, ROCK Rho-associated coiled-coil containing protein kinase, NO nitric oxide, phos- phosphorylation, GEF guanine nucleotide-exchange factor, BSA bovine serum albumin, NADPH nicotinamide adenine dinucleotide phosphate, NF-κB nuclear factor-kappa B, MAPKs mitogen-activated protein kinases, MVED microvascular endothelial dysfunction
RhoA is involved in other cellular signaling pathways and in a variety of physiological and pathological processes, because it regulates many such processes, including cytoskeletal dynamics, cell polarity, membrane transport, and gene expression [40]. Glucosamine, a product of glucose influx via the hexosamine biosynthesis pathway (HBP) in diabetes, has recently been shown to increase vascular contraction, at least in part via activation of the RhoA/ROCK pathway [41]. Hyperglycemia increases endothelial cell RhoA/ROCK activity in a PKC and reactive oxygen species (ROS)-dependent manner, and activated ROCK mediates glucose-induced expression of the plasminogen activator inhibitor-1 (PAI-1) [37, 42–44]. Furthermore, the polyol pathway is also activated when microvascular permeability increases under hyperglycemic conditions, and the immediate cellular changes observed can be abrogated by inhibiting ROCK [45]. These studies have revealed the critical role played by the RhoA pathway in retinal MVED associated with diabetes (Fig. 2).
RhoA and the endothelium
The endothelium forms the inner lining of blood vessels and is metabolically active [46]. Apart from functioning as a barrier, it senses and responds to environmental factors and has important autocrine and paracrine functions that regulate the contractile state of blood vessels, the hemostatic balance, and other cellular functions [46, 47]. Recently, RhoA has received much attention as a key regulator of cell shape, movement, and proliferation [48].
RhoA and its downstream effector ROCK I/II modulate cell adhesion, migration, proliferation and apoptosis by controlling arrangement of the actin skeleton as well as cell shrinkage [33, 49, 50]. It has been shown both in vivo and in vitro that the Rho pathway plays a critical role in diabetic retinal microvascular pathology, and that hyperglycemia triggers retinal hypertonicity by activating Rho signaling and subsequently increasing RhoA/ROCK activity [2, 37, 51]. The calcium channel blocker fasudil and the lipid-lowering agents ezetimibe and simvastatin protect the retinal microvascular endothelium by inhibiting RhoA/ROCK activity, thus ameliorating endothelial proliferation and hypertonicity in diabetic patients [2, 46, 52, 53].
The evidence that RhoA is ubiquitously expressed in various types of endothelial cells is overwhelming, and it is clear that RhoA activation induces the breakdown of the endothelial barriers of microvascular mesenteric endothelial cells, human dermal microvascular endothelial cells, and macrovascular pulmonary artery endothelial cells, but not microvascular myocardial endothelial cells [54]. The primary negative regulator of Rho, RhoGDI-1, represses RhoA activity in the lung microvessel endothelium, and thus preserves endothelial barrier function in vivo. Inhibition of the RhoA pathway by GDIs can reverse the increase in microvascular permeability induced by acute stimulation with the PAR1 peptide or prolonged stimulation of RhoGDI-1-/- mice [55].
RhoA is also involved in the induction of endothelial hyperpermeability by certain agents, including thrombin, VEGF, angiopoietin-2 (Ang-2), and lysophosphatidic acid (LPA) [56–58]. RhoA and PI3 kinase mediate certain processes, and specific inhibitors prevent ROS-induced monocyte migration across an in vitro model of the blood brain barrier (BBB). Interestingly, such processes are also mediated by protein kinase B (PKB/Akt), previously unrecognized as a player in cytoskeleton and tight junction (TJ) dynamics; PKB acts downstream of both RhoA and PI3 kinase [59].
RhoA also regulates the activities of inter-endothelial junctions, affecting cell motility, proliferation, survival, and permeability [60–63]. In both DR and macular edema (ME), the TJ proteins occludin and zonula occluden-1 (ZO-1), and the adherens junction protein cadherin-5, are critical for maintenance of the endothelial barrier and for modulating the paracellular transport of large vessel endothelia [64–67]. Recently, many in vivo and in vitro studies have shown that RhoA/ROCK signaling affects the activities of junction complexes [51, 68–70]. Rho inhibition reduces localization of ZO-1 and occludin to cell junctions. Notably, constitutive Rho signaling conversely causes ZO-1 and occludin to accumulate at cell junctions [71].
The observed improvement in endothelial function upon inhibition of Rho-kinase activity by ezetimibe, an inhibitor of intestinal cholesterol absorption, suggests that the agent might have novel anti-atherogenic effects in humans [53]. In addition, inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, such as statins, may improve endothelial function and decrease vascular inflammation and atherosclerosis by inhibiting the Rho/ROCK pathway [46].
RhoA and angiogenesis
RhoA coupled to Gα13 modulates cell migration [72, 73]; this is accomplished by the direct interaction of activated Gα13 with a family of GEFs binding to RhoA. This family is termed the “regulator of G-protein signaling (RGS)-homology domain (RH)-containing GEFs” (RH-RhoGEFs) [73–75]. Disruption of the Gα13 gene in mice impaires the ability of endothelial cells to develop into an organized vascular system, resulting in intrauterine death [76–78]. The biological functions of RhoA depend principally on the associated RhoGEFs, which both control the RhoA GDP/GTP binding state and directly influence the development of angiogenesis [79, 80].
Rho signaling is also involved in sphingosine-1-phosphate (SPP)-induced angiogenesis, which is greatly inhibited by C3 transferase, a type of RhoA inhibitor [81]. A great deal of in vivo and in vitro work has shown that RhoA is required for angiogenesis [82–85]. Conversely, angiogenesis progression is restrained by blocking Rho or RhoA/ROCK signaling [86–88].
In terms of pharmacology, cerivastatin, a cholesterol-lowering agent, has been shown to inhibit in vitro microvascular endothelial cell proliferation induced by growth factors; this is reversed by treatment with geranylgeranyl pyrophosphate (GGPP). This mechanism is associated with the transition of RhoA from the cell membrane to the cytoplasm and depolymerization of actin fibers (which is also prevented by GGPP treatment). RhoA-dependent inhibition of cell proliferation is mediated by inhibition of focal adhesion kinase and Akt activation [89]. In addition, it has been proposed that the HMG-CoA reductase inhibitor simvastatin may interfere with angiogenesis by inhibiting the geranylgeranylation and membrane localization of RhoA. Furthermore, tube formation is inhibited by GGTI (a specific inhibitor of Rho geranylgeranylation), C3 exotoxin (which inactivates Rho), and adenovirus-mediated expression of a dominant-negative form of RhoA (which reverses the effect of simvastatin on tube formation). Finally, inhibitors of HMG-CoA reductase also inhibit signaling by VEGF, Akt, and focal adhesion kinase (three RhoA-dependent pathways involved in angiogenesis) [90].
To the best of our knowledge, vascular angiogenesis is regulated by several cytokines, of which VEGF-A and its receptor, VEGF receptor 2 (VEGFR-2), play indisputably important roles [91–94]. VEGF induces RhoA activation and its recruitment to the membrane of human endothelial cells. ROCK inhibition prevents VEGF-enhanced endothelial cell migration that follows mechanical wounding, but has no effect on basal endothelial cell migration. These findings indicate that the VEGF-induced cytoskeletal changes in endothelial cells require both RhoA and Rho kinase, and activation of signaling by these materials is involved in the VEGF-induced in vitro migration and angiogenesis of endothelial cells [95]. Furthermore, transient overexpression of the dominant-active RhoA mutant also increases tyrosine phosphorylation of VEGFR-2, whereas overexpression of a dominant-inactive form of the protein has no such effect. Together, these results indicate that the Rho proteins play important roles in angiogenesis by modulating the tyrosine phosphorylation status of VEGFR-2 [96].
Controversially, loss-of-function experiments with endothelial cells have revealed that inhibition of ROCK I/II by the pharmacological inhibitor H-1152 and ROCK I/II-specific small-interfering RNAs (siRNAs) increases VEGF-driven retinal neovascularization and sprouting angiogenesis [97].
Recently, a regulatory role for VEGF-C in initiation and potentiation of angiogenesis has been described [98–100]. VEGF-C knockdown decreases RhoA expression. Furthermore, RhoA knockdown, even upon supplementation with VEGF-C or VEGF-A, decreases endothelial cell proliferation and stress fiber formation, indicating that VEGF-C promotes angiogenesis via a RhoA-mediated pathway [101].
RhoA and apoptosis
RhoA was first described as an inhibitor of endothelial cell death [102]. An earlier study suggested that inhibition of the RhoA/ROCK pathway by a ROCK inhibitor, Y27632, attenuates glucose-induced apoptosis to an extreme degree [103]. More recently, RhoA signaling has been shown to trigger mitochondrial proximal tubule cell apoptosis in response to mechanical stretching, which is inhibited by phosphorylation of Erk1/2 and p38 MAPK [104].
On the other hand, inhibition of RhoA/ROCK1 signaling promotes apoptosis of leukemia cells by enhancing phosphorylation of Erk1/2 in an Mek1/2-independent manner [105]. Intriguingly, it had recently been shown that inhibition of RhoA and ROCK I activation by the C3 exoenzyme and Y27632, respectively, attenuates apoptosis of human leukemia cells [106].
RhoA involvement in cancer cell apoptosis is a major field of research. RhoA activation, induced by CNFy, triggers intrinsic apoptosis of the prostate cancer cell line LNCaP [107], and inhibition of RhoA/ROCK signaling promotes apoptosis of gastric cancer cells [108]. These data reveal a novel RhoA activity, which may aid in a comprehensive understanding of DR, but which currently remains enigmatic.
mDia-1
mDia-1 is an isoform of the formin family, which contains potent dynamic regulators. The formin family is defined by the presence of the formin homology 2 (FH2) domain [109], and is further classified in terms of the presence and arrangement of additional domains [110, 111]. Most eukaryocytic cells contain proteins with a great diversity of FH2 domains. Each such domain consists of approximately 400 amino acids that directly control how actin is modified by the formin; the FH1 domain affects the function of the FH2 domain by binding to profilin [109, 112, 113]. Thus, the FH1 domain binds profilin, which is required for actin chain elongation by diaphanous (Dia) (Fig. 1) [114–116].
Phylogenetic analyses of the FH2 domain have shown that mouse formins can be divided into seven subfamilies, as follows [109]: Dia, dishevelled-associated activator of morphogenesis (DAAM), formin-related gene in leukocytes (FRL), formin homology domain-containing protein (FHOD), inverted formin (INF), formin (FMN), and delphilin.
The mDia subfamily contains three isoforms termed mDia-1 (also known as Diap-1), mDia-2 and mDia-3 (also known as Diap-2) [111, 117]. mDia proteins contain an RBD/FH3 sequence in their N-terminal regions, which in turn contain a Rho-binding domain (RBD), four Arm repeats (also termed the Dia-inhibitory domain, DID), a dimerization domain (DD), and a putative coil-coiled region (CC) [117, 118]. mDia-1 can be activated only by Rho (RhoA-C), whereas mDia-2 and mDia-3 can be also activated by Rac and Cdc42 [119, 120]. Members of the Dia protein family are key regulators of fundamental actin-driven cellular processes, which are conserved from yeast to humans [111]. Cellular studies have suggested that RhoA competes with the diaphanous auto-regulatory domain (DAD) to bind to the mDia-1 N-terminus, relieving the auto-inhibitory interaction, and thus enabling mDia-1 to influence actin dynamics [121–123].
Many studies have shown that mDia-1 is an Rho-regulated actin nucleator that acts downstream of RhoA [117, 118, 124]. It is a multimodular protein that interacts with numerous actin regulators, adapters and signaling components such as profilin-1 [111]. To date, at least 12 formins have been shown to interact with Rho family GTPases, the best-studied interaction is that between mDia-1 and RhoA [113, 125–127].
mDia-1 and angiogenesis
As emphasized above, VEGF and Ang-1 play essential (complementary) roles in vascular development during embryogenesis. VEGF is required for the formation of the initial vascular plexus early in development, and Ang-1 is necessary for subsequent vascular remodeling into mature blood vessels [128–130].
Gavard et al. [128] showed that Ang-1 counteracted VEGF-induced endothelial permeability by triggering the RhoA pathway and the consequent association of mDia with Src, thereby preventing activation of Src by VEGFR-2. Knockdown of endothelial RhoA by siRNA restored the VEGF-induced S665 VE-cadherin phosphorylation blocked by Ang-1, and knockdown of either mDia-1 or mDia-2 removed that protein from the heterocomplex and eliminated the ability of Ang-1 to counteract the VEGF-induced endothelial permeability of mouse endothelial cells. This proved that mDia was required downstream of Ang-1 to block VEGF-dependent permeability. Once activated, mDia-1 played a key role when Ang-1 controlled endothelial barrier function; expression of active mutant mDia-1 blocked VEGF-induced permeability. Thus, by limiting the access of Src to VEGFR-2, mDia-1 may restrict activation of the SFK-initiated pathway; ultimately controlling the interplay between Ang-1 and VEGF, and the biological outcome of this interaction.
mDia-1 and apoptosis
Kamasani et al. [131] showed that the Rho effector mDia-1 is a critical downstream player in farnesyl transferase inhibitor (FTI)-induced apoptosis. Dominant inhibition of mDia-1 action ablated FTI-induced apoptosis, but not actin reorganization or growth inhibition, the latter of which may be associated with a Rho effector kinase pathway interaction that downregulates c-Myc. In nude mice, dominant inhibition of mDia-1 promoted tumor formation and ablated the anti-tumor action of FTI. These findings suggest that the Rho/mDia-1 pathway plays a critical role in the cell death mechanism engaged by FTI, and that mDia-1 may be important in terms of the Rho-dependent survival of oncogenically transformed cells, perhaps influenced by oncogenic RhoGEF AKAP13/Lbc.
Profilin-1
To the best of our knowledge, actin is a highly dynamic protein network containing many actin-associated proteins [132, 133]. Of these, one key regulatory protein, profilin-1, binds to actin monomers in the skeletal body (at the barbed ends), and contributes to many biological activities by assembling and disassembling actin filaments [134–136]. Profilin-1 consists of 140 amino acids, and has a molecular weight of 12 – 15 kDa. It is a ubiquitously expressed protein that binds to G-actin [137–139] and is associated with many cellular activities ranging from control of actin polymerization to gene transcription [23].
Traditionally, profilin-1 has been considered an essential control element for actin polymerization and cell migration. Originally identified as an actin-sequestering protein that formed a 1:1 complex with G-actin, it was thought to prevent actin polymerization (Fig. 1) [140]. However, subsequent studies showed that it promotes actin polymerization by catalyzing the exchange of actin-bound ADP for ATP and transporting ATP-G-actin to the barbed end of actin [141, 142]. In addition, it liberates actin monomers from the sequestering protein thymosin-β4 [24], thus contributing indispensably to both physiological and pathological cell proliferation and migration [143]. In summary, profilin-1 has a dual effect on actin polymerization, depending on its concentration relative to those of G-actin and the free barbed ends of actin filaments [23].
In general, profilin-1 binds strongly to three major classes of ligands; in order of strength, these are: actin monomers [144], phosphatidylinositol 4, 5-bisphosphate (PIP2) [145] and proteins containing poly L-proline (PLP) (including vasodilator-stimulated phosphoprotein, or VASP; Wiskott-Aldrich Syndrome Protein, or WASP; and Dia) [116, 146, 147]. Notably, profilin-1 binds to (and regulates the action of) retinal cadherin (R-cadherin), downstream of the Rho GTPases [148].
Based on in vivo experiments with transgenic mice overexpression of profilin-1 in smooth muscle cells increases actin polymerization and subsequently activates the Rho/ROCK pathway [149]. In another work, ROCK and Dia-1 together mediated actin polymerization by regulating the activity of profilin-1 [150]. RhoA controls the actions of R-cadherin, a member of the classical cadherin family, through the Dia-1/profilin-1 signaling pathway [148].
Profilin-1 and the endothelium
Romeo et al. [151] showed that profilin-1 acted downstream of low-density lipoprotein (LDL) to mediate diabetic MVED. Profilin-1 overexpressed in rat aortic endothelial cells triggered three indicators of endothelial dysfunction: an increase in apoptosis, elevated expression of intracellular adhesion molecule 1 (ICAM-1), and decreased phosphorylation of VASP (a marker for NO signaling). In addition, loss of profilin-1 was associated with reduced cell-cell adhesion and inhibition of cell migration. Furthermore, such loss inhibited cell growth without compromising cell survival, at least in the short term, thus suggesting that profilin-1 plays an important role in endothelial proliferation. In another study, silencing of profilin-1 expression suppressed the matrigel-induced early cord morphogenesis of endothelial cells [20].
Profilin-1 and angiogenesis
Fan et al. [22] recently showed that VEGF-A-inducible phosphorylation of profilin-1 at Tyr 129 was critical in terms of endothelial cell migration and angiogenesis. Chemotactic activation of VEGFR-2 and Src induced profilin-1 phosphorylation at the leading edge of the cell, promoting the binding of profilin-1 to actin and actin polymerization. Subsequently, use of a conditional endothelial knockin of phosphorylation-deficient profilin-1Y129F in mice revealed that profilin-1 phosphorylation was critical to allow angiogenesis after wounding and ischemic injury, but not developmental angiogenesis. Thus, the VEGFR-2/Src-mediated phosphorylation of profilin-1 bypasses canonical, multistep, intracellular signaling events to initiate endothelial cell migration and angiogenesis in some other manner, and may serve as a highly selective and nontoxic target of therapeutic interventions seeking to minimize pathological angiogenesis.
Profilin-1 and apoptosis
Of all conditions in which profilin-1 affects apoptosis, breast cancer has received the most attention. Yao et al. [152] found that stable expression of ectopic profilin-1 sensitized the breast cancer cell line MDA-MB-468 to apoptosis. Thus, profilin-1, which functions primarily to promote the formation of local superstructures from actin filaments and integrin, may contribute to the promotion of apoptosis. A previously unknown activity of profilin-1 was discovered; the protein mediates staurosporine (STS)-induced apoptosis in breast cancer cells by upregulating integrin α5β1 synthesis, presenting a new target for breast cancer therapy. A subsequent study [153] showed that profilin-1 overexpression sensitized cancer cells to apoptosis of the typical intrinsic mitochondrial pathway triggered by STS. Again, this revealed a new function/action of profilin-1: it combines synergistically with apoptotic agents to increase apoptosis.
Conclusion
In summary, we have explored the roles played by the RhoA/mDia-1/profilin-1 signaling pathway during MVED progression in DR. Many studies have shown that endothelial function is critical in terms of eye homeostasis, and its dysfunction is closely associated with DR. Angiogenesis and apoptosis are the most common end-stage symptoms of advanced retinal MVED caused by the hyperglycemia of DR. However, DR is much more than simple chronic hyperglycemia in one eye. The understanding and management of MVED is a major focus of research seeking to prevent microvascular complications associated with all stages of DR. Our review of angiogenesis and apoptosis during DR, together with previous studies, reinforces the concept that MVED predisposes toward DR.
References
Pastor JC, de la Rua ER, Martin F (2002) Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retin Eye Res 21:127–144
Arita R, Hata Y, Nakao S, Kita T, Miura M, Kawahara S, Zandi S, Almulki L, Tayyari F, Shimokawa H, Hafezi-Moghadam A, Ishibashi T (2009) Rho kinase inhibition by fasudil ameliorates diabetes-induced microvascular damage. Diabetes 58:215–226. doi:10.2337/db08-0762
Mehta D, Bhattacharya J, Matthay MA, Malik AB (2004) Integrated control of lung fluid balance. Am J Physiol Lung Cell Mol Physiol 287:L1081–L1090. doi:10.1152/ajplung.00268.2004
Lenna S, Han R, Trojanowska M (2014) Endoplasmic reticulum stress and endothelial dysfunction. IUBMB Life 66:530–537. doi:10.1002/iub.1292
Roberts AC, Porter KE (2013) Cellular and molecular mechanisms of endothelial dysfunction in diabetes. Diab Vasc Dis Res 10:472–482. doi:10.1177/1479164113500680
Michiels C (2003) Endothelial cell functions. J Cell Physiol 196:430–443. doi:10.1002/jcp.10333
Sena CM, Pereira AM, Seica R (2013) Endothelial dysfunction - a major mediator of diabetic vascular disease. Biochim Biophys Acta 1832:2216–2231. doi:10.1016/j.bbadis.2013.08.006
Basha B, Samuel SM, Triggle CR, Ding H (2012) Endothelial dysfunction in diabetes mellitus: possible involvement of endoplasmic reticulum stress? Exp Diabetes Res 2012:481840. doi:10.1155/2012/481840
Takeno K, Mita T, Nakayama S, Goto H, Komiya K, Abe H, Ikeda F, Shimizu T, Kanazawa A, Hirose T, Kawamori R, Watada H (2012) Masked hypertension, endothelial dysfunction, and arterial stiffness in type 2 diabetes mellitus: a pilot study. Am J Hypertens 25:165–170. doi:10.1038/ajh.2011.158
Ishida K, Taguchi K, Matsumoto T, Kobayashi T (2014) Activated platelets from diabetic rats cause endothelial dysfunction by decreasing Akt/endothelial NO synthase signaling pathway. PLoS One 9:e102310. doi:10.1371/journal.pone.0102310
Wojciak-Stothard B, Abdul-Salam VB, Lao KH, Tsang H, Irwin DC, Lisk C, Loomis Z, Stenmark KR, Edwards JC, Yuspa SH, Howard LS, Edwards RJ, Rhodes CJ, Gibbs JS, Wharton J, Zhao L, Wilkins MR (2014) Aberrant chloride intracellular channel 4 expression contributes to endothelial dysfunction in pulmonary arterial hypertension. Circulation 129:1770–1780. doi:10.1161/CIRCULATIONAHA.113.006797
Lovren F, Verma S (2013) Evolving role of microparticles in the pathophysiology of endothelial dysfunction. Clin Chem 59:1166–1174. doi:10.1373/clinchem.2012.199711
Wang J, Chen S, Ma X, Cheng C, Xiao X, Chen J, Liu S, Zhao B, Chen Y (2013) Effects of endothelial progenitor cell-derived microvesicles on hypoxia/reoxygenation-induced endothelial dysfunction and apoptosis. Oxidative Med Cell Longev 2013:572729. doi:10.1155/2013/572729
Michael IP, Westenskow PD, Hacibekiroglu S, Greenwald AC, Ballios BG, Kurihara T, Li Z, Warren CM, Zhang P, Aguilar E, Donaldson L, Marchetti V, Baba T, Hussein SM, Sung HK, Iruela-Arispe ML, Rini JM, van der Kooy D, Friedlander M, Nagy A (2014) Local acting Sticky-trap inhibits vascular endothelial growth factor dependent pathological angiogenesis in the eye. EMBO Mol Med 6:604–623. doi:10.1002/emmm.201303708
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9:669–676. doi:10.1038/nm0603-669
Lakeland TV, Borg ML, Matzaris M, Abdelkader A, Evans RG, Watt MJ (2014) Augmented expression and secretion of adipose-derived pigment epithelium-derived factor does not alter local angiogenesis or contribute to the development of systemic metabolic derangements. Am J Physiol Endocrinol Metab 306:E1367–E1377. doi:10.1152/ajpendo.00046.2014
Song JW, Daubriac J, Tse JM, Bazou D, Munn LL (2012) RhoA mediates flow-induced endothelial sprouting in a 3-D tissue analogue of angiogenesis. Lab Chip 12:5000–5006. doi:10.1039/c2lc40389g
Yang W, Ramachandran A, You S, Jeong H, Morley S, Mulone MD, Logvinenko T, Kim J, Hwang D, Freeman MR, Adam RM (2014) Integration of proteomic and transcriptomic profiles identifies a novel PDGF-MYC network in human smooth muscle cells. Cell Commun Signal 12:44. doi:10.1186/PREACCEPT-9184871921296322
Yakkundi A, McCallum L, O’Kane A, Dyer H, Worthington J, McKeen HD, McClements L, Elliott C, McCarthy HO, Hirst DG, Robson T (2013) The anti-migratory effects of FKBPL and its peptide derivative, AD-01: regulation of CD44 and the cytoskeletal pathway. PLoS One 8:e55075. doi:10.1371/journal.pone.0055075
Ding Z, Lambrechts A, Parepally M, Roy P (2006) Silencing profilin-1 inhibits endothelial cell proliferation, migration and cord morphogenesis. J Cell Sci 119:4127–4137. doi:10.1242/jcs.03178
Fan Y, Gong Y, Ghosh PK, Graham LM, Fox PL (2009) Spatial coordination of actin polymerization and ILK-Akt2 activity during endothelial cell migration. Dev Cell 16:661–674. doi:10.1016/j.devcel.2009.03.009
Fan Y, Arif A, Gong Y, Jia J, Eswarappa SM, Willard B, Horowitz A, Graham LM, Penn MS, Fox PL (2012) Stimulus-dependent phosphorylation of profilin-1 in angiogenesis. Nat Cell Biol 14:1046–1056. doi:10.1038/ncb2580
Ding Z, Bae YH, Roy P (2012) Molecular insights on context-specific role of profilin-1 in cell migration. Cell Adhes Migr 6:442–449. doi:10.4161/cam.21832
Witke W (2004) The role of profilin complexes in cell motility and other cellular processes. Trends Cell Biol 14:461–469. doi:10.1016/j.tcb.2004.07.003
Jockusch BM, Murk K, Rothkegel M (2007) The profile of profilins. Rev Physiol Biochem Pharmacol 159:131–149. doi:10.1007/112_2007_704
Heasman SJ, Ridley AJ (2008) Mammalian Rho GTPases: new insights into their functions from in vivo studies. Nat Rev Mol Cell Biol 9:690–701. doi:10.1038/nrm2476
Takayama N, Kai H, Kudo H, Yasuoka S, Mori T, Anegawa T, Koga M, Kajimoto H, Hirooka Y, Imaizumi T (2011) Simvastatin prevents large blood pressure variability induced aggravation of cardiac hypertrophy in hypertensive rats by inhibiting RhoA/Ras-ERK pathways. Hypertens Res 34:341–347. doi:10.1038/hr.2010.229
Chew TW, Liu XJ, Liu L, Spitsbergen JM, Gong Z, Low BC (2014) Crosstalk of Ras and Rho: activation of RhoA abates Kras-induced liver tumorigenesis in transgenic zebrafish models. Oncogene 33:2717–2727. doi:10.1038/onc.2013.240
Zhu Y, Casey PJ, Kumar AP, Pervaiz S (2013) Deciphering the signaling networks underlying simvastatin-induced apoptosis in human cancer cells: evidence for non-canonical activation of RhoA and Rac1 GTPases. Cell Death Dis 4:e568. doi:10.1038/cddis.2013.103
Peng F, Wu D, Gao B, Ingram AJ, Zhang B, Chorneyko K, McKenzie R, Krepinsky JC (2008) RhoA/Rho-kinase contribute to the pathogenesis of diabetic renal disease. Diabetes 57:1683–1692. doi:10.2337/db07-1149
Bryan BA, Dennstedt E, Mitchell DC, Walshe TE, Noma K, Loureiro R, Saint-Geniez M, Campaigniac JP, Liao JK, D’Amore PA (2010) RhoA/ROCK signaling is essential for multiple aspects of VEGF-mediated angiogenesis. FASEB J 24:3186–3195. doi:10.1096/fj.09-145102
Margolis SS, Salogiannis J, Lipton DM, Mandel-Brehm C, Wills ZP, Mardinly AR, Hu L, Greer PL, Bikoff JB, Ho HY, Soskis MJ, Sahin M, Greenberg ME (2010) EphB-mediated degradation of the RhoA GEF Ephexin5 relieves a developmental brake on excitatory synapse formation. Cell 143:442–455. doi:10.1016/j.cell.2010.09.038
Hotulainen P, Hoogenraad CC (2010) Actin in dendritic spines: connecting dynamics to function. J Cell Biol 189:619–629. doi:10.1083/jcb.201003008
Goldin A, Beckman JA, Schmidt AM, Creager MA (2006) Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 114:597–605. doi:10.1161/CIRCULATIONAHA.106.621854
Hirose A, Tanikawa T, Mori H, Okada Y, Tanaka Y (2010) Advanced glycation end products increase endothelial permeability through the RAGE/Rho signaling pathway. FEBS Lett 584:61–66. doi:10.1016/j.febslet.2009.11.082
Niiya Y, Abumiya T, Yamagishi S, Takino J, Takeuchi M (2012) Advanced glycation end products increase permeability of brain microvascular endothelial cells through reactive oxygen species-induced vascular endothelial growth factor expression. J Stroke Cerebrovasc Dis 21:293–298. doi:10.1016/j.jstrokecerebrovasdis.2010.09.002
Zhou H, Li YJ (2010) RhoA/Rho kinase: a novel therapeutic target in diabetic complications. Chin Med J (Engl) 123:2461–2466
Romero MJ, Iddings JA, Platt DH, Ali MI, Cederbaum SD, Stepp DW, Caldwell RB, Caldwell RW (2012) Diabetes-induced vascular dysfunction involves arginase I. Am J Physiol Heart Circ Physiol 302:H159–H166. doi:10.1152/ajpheart.00774.2011
Romero MJ, Platt DH, Tawfik HE, Labazi M, El-Remessy AB, Bartoli M, Caldwell RB, Caldwell RW (2008) Diabetes-induced coronary vascular dysfunction involves increased arginase activity. Circ Res 102:95–102. doi:10.1161/CIRCRESAHA.107.155028
Jaffe AB, Hall A (2005) Rho GTPases: biochemistry and biology. Annu Rev Cell Dev Biol 21:247–269. doi:10.1146/annurev.cellbio.21.020604.150721
Kim do H, Seok YM, Kim IK, Lee IK, Jeong SY, Jeoung NH (2011) Glucosamine increases vascular contraction through activation of RhoA/Rho kinase pathway in isolated rat aorta. BMB Rep 44:415–420. doi:10.5483/BMBRep.2011.44.6.415
Rikitake Y, Liao JK (2005) Rho-kinase mediates hyperglycemia-induced plasminogen activator inhibitor-1 expression in vascular endothelial cells. Circulation 111:3261–3268. doi:10.1161/CIRCULATIONAHA.105.534024
Aveleira CA, Lin CM, Abcouwer SF, Ambrosio AF, Antonetti DA (2010) TNF-alpha signals through PKCzeta/NF-kappaB to alter the tight junction complex and increase retinal endothelial cell permeability. Diabetes 59:2872–2882. doi:10.2337/db09-1606
Kawamura H, Yokote K, Asaumi S, Kobayashi K, Fujimoto M, Maezawa Y, Saito Y, Mori S (2004) High glucose-induced upregulation of osteopontin is mediated via Rho/Rho kinase pathway in cultured rat aortic smooth muscle cells. Arterioscler Thromb Vasc Biol 24:276–281. doi:10.1161/01.ATV.0000112012.33770.2a
Sward P, Rippe B (2012) Acute and sustained actions of hyperglycaemia on endothelial and glomerular barrier permeability. Acta Physiol (Oxf) 204:294–307. doi:10.1111/j.1748-1716.2011.02343.x
Sawada N, Liao JK (2014) Rho/Rho-associated coiled-coil forming kinase pathway as therapeutic targets for statins in atherosclerosis. Antioxid Redox Signal 20:1251–1267. doi:10.1089/ars.2013.5524
Aird WC (2007) Phenotypic heterogeneity of the endothelium: I. Structure, function, and mechanisms. Circ Res 100:158–173. doi:10.1161/01.RES.0000255691.76142.4a
van Nieuw Amerongen GP, van Hinsbergh VW (2007) Endogenous RhoA inhibitor protects endothelial barrier. Circ Res 101:7–9. doi:10.1161/CIRCRESAHA.107.156513
Riou P, Kjaer S, Garg R, Purkiss A, George R, Cain RJ, Bineva G, Reymond N, McColl B, Thompson AJ, O’Reilly N, McDonald NQ, Parker PJ, Ridley AJ (2013) 14-3-3 proteins interact with a hybrid prenyl-phosphorylation motif to inhibit G proteins. Cell 153:640–653. doi:10.1016/j.cell.2013.03.044
Riento K, Ridley AJ (2003) Rocks: multifunctional kinases in cell behaviour. Nat Rev Mol Cell Biol 4:446–456. doi:10.1038/nrm1128
Lu QY, Chen W, Lu L, Zheng Z, Xu X (2014) Involvement of RhoA/ROCK1 signaling pathway in hyperglycemia-induced microvascular endothelial dysfunction in diabetic retinopathy. Int J Clin Exp Pathol 7:7268–7277
Takeda N, Kondo M, Ito S, Ito Y, Shimokata K, Kume H (2006) Role of RhoA inactivation in reduced cell proliferation of human airway smooth muscle by simvastatin. Am J Respir Cell Mol Biol 35:722–729. doi:10.1165/rcmb.2006-0034OC
Nochioka K, Tanaka S, Miura M, Zhulanqiqige do E, Fukumoto Y, Shiba N, Shimokawa H (2012) Ezetimibe improves endothelial function and inhibits Rho-kinase activity associated with inhibition of cholesterol absorption in humans. Circ J 76:2023–2030
Baumer Y, Burger S, Curry FE, Golenhofen N, Drenckhahn D, Waschke J (2008) Differential role of Rho GTPases in endothelial barrier regulation dependent on endothelial cell origin. Histochem Cell Biol 129:179–191. doi:10.1007/s00418-007-0358-7
Gorovoy M, Neamu R, Niu J, Vogel S, Predescu D, Miyoshi J, Takai Y, Kini V, Mehta D, Malik AB, Voyno-Yasenetskaya T (2007) RhoGDI-1 modulation of the activity of monomeric RhoGTPase RhoA regulates endothelial barrier function in mouse lungs. Circ Res 101:50–58. doi:10.1161/CIRCRESAHA.106.145847
Essler M, Amano M, Kruse HJ, Kaibuchi K, Weber PC, Aepfelbacher M (1998) Thrombin inactivates myosin light chain phosphatase via Rho and its target Rho kinase in human endothelial cells. J Biol Chem 273:21867–21874
van Nieuw Amerongen GP, Draijer R, Vermeer MA, van Hinsbergh VW (1998) Transient and prolonged increase in endothelial permeability induced by histamine and thrombin: role of protein kinases, calcium, and RhoA. Circ Res 83:1115–1123
Parikh SM, Mammoto T, Schultz A, Yuan HT, Christiani D, Karumanchi SA, Sukhatme VP (2006) Excess circulating angiopoietin-2 may contribute to pulmonary vascular leak in sepsis in humans. PLoS Med 3:e46. doi:10.1371/journal.pmed.0030046
Schreibelt G, Kooij G, Reijerkerk A, van Doorn R, Gringhuis SI, van der Pol S, Weksler BB, Romero IA, Couraud PO, Piontek J, Blasig IE, Dijkstra CD, Ronken E, de Vries HE (2007) Reactive oxygen species alter brain endothelial tight junction dynamics via RhoA, PI3 kinase, and PKB signaling. FASEB J 21:3666–3676. doi:10.1096/fj.07-8329com
Etienne-Manneville S, Hall A (2002) Rho GTPases in cell biology. Nature 420:629–635. doi:10.1038/nature01148
Ridley AJ (2001) Rho family proteins: coordinating cell responses. Trends Cell Biol 11:471–477
van Nieuw Amerongen GP, van Delft S, Vermeer MA, Collard JG, van Hinsbergh VW (2000) Activation of RhoA by thrombin in endothelial hyperpermeability: role of Rho kinase and protein tyrosine kinases. Circ Res 87:335–340
Russ PK, Kupperman AI, Presley SH, Haselton FR, Chang MS (2010) Inhibition of RhoA signaling with increased Bves in trabecular meshwork cells. Invest Ophthalmol Vis Sci 51:223–230. doi:10.1167/iovs. 09-3539
Russ PK, Davidson MK, Hoffman LH, Haselton FR (1998) Partial characterization of the human retinal endothelial cell tight and adherens junction complexes. Invest Ophthalmol Vis Sci 39:2479–2485
Peng H, Luo P, Li Y, Wang C, Liu X, Ye Z, Li C, Lou T (2013) Simvastatin alleviates hyperpermeability of glomerular endothelial cells in early-stage diabetic nephropathy by inhibition of RhoA/ROCK1. PLoS One 8:e80009. doi:10.1371/journal.pone.0080009
Gu YT, Xue YX, Wang YF, Wang JH, Chen X, ShangGuan QR, Lian Y, Zhong L, Meng YN (2013) Minoxidil sulfate induced the increase in blood–brain tumor barrier permeability through ROS/RhoA/PI3K/PKB signaling pathway. Neuropharmacology 75:407–415. doi:10.1016/j.neuropharm.2013.08.004
Srivastava K, Shao B, Bayraktutan U (2013) PKC-beta exacerbates in vitro brain barrier damage in hyperglycemic settings via regulation of RhoA/Rho-kinase/MLC2 pathway. J Cereb Blood Flow Metab 33:1928–1936. doi:10.1038/jcbfm.2013.151
Le Drean G, Haure-Mirande V, Ferrier L, Bonnet C, Hulin P, de Coppet P, Segain JP (2014) Visceral adipose tissue and leptin increase colonic epithelial tight junction permeability via a RhoA-ROCK-dependent pathway. FASEB J 28:1059–1070. doi:10.1096/fj.13-234203
Yang M, Chen XM, Du XG, Cao FF, Vijaya Luxmi S, Shen Q (2013) Continuous blood purification ameliorates endothelial hyperpermeability in SAP patients with MODS by regulating tight junction proteins via ROCK. Int J Artif Organs 36:700–709. doi:10.5301/ijao.5000216
Zhang K, Zhang H, Xiang H, Liu J, Liu Y, Zhang X, Wang J, Tang Y (2013) TGF-beta1 induces the dissolution of tight junctions in human renal proximal tubular cells: role of the RhoA/ROCK signaling pathway. Int J Mol Med 32:464–468. doi:10.3892/ijmm.2013.1396
Gopalakrishnan S, Raman N, Atkinson SJ, Marrs JA (1998) Rho GTPase signaling regulates tight junction assembly and protects tight junctions during ATP depletion. Am J Physiol 275:C798–C809
Wang Q, Liu M, Kozasa T, Rothstein JD, Sternweis PC, Neubig RR (2004) Thrombin and lysophosphatidic acid receptors utilize distinct rhoGEFs in prostate cancer cells. J Biol Chem 279:28831–28834. doi:10.1074/jbc.C400105200
Mikelis CM, Palmby TR, Simaan M, Li W, Szabo R, Lyons R, Martin D, Yagi H, Fukuhara S, Chikumi H, Galisteo R, Mukouyama YS, Bugge TH, Gutkind JS (2013) PDZ-RhoGEF and LARG are essential for embryonic development and provide a link between thrombin and LPA receptors and Rho activation. J Biol Chem 288:12232–12243. doi:10.1074/jbc.M112.428599
Hall A (1998) G proteins and small GTPases: distant relatives keep in touch. Science 280:2074–2075
Patel M, Kawano T, Suzuki N, Hamakubo T, Karginov AV, Kozasa T (2014) Galpha13/PDZ-RhoGEF/RhoA signaling is essential for gastrin-releasing peptide receptor-mediated colon cancer cell migration. Mol Pharmacol 86:252–262. doi:10.1124/mol.114.093914
Offermanns S, Mancino V, Revel JP, Simon MI (1997) Vascular system defects and impaired cell chemokinesis as a result of Galpha13 deficiency. Science 275:533–536
Ruppel KM, Willison D, Kataoka H, Wang A, Zheng YW, Cornelissen I, Yin L, Xu SM, Coughlin SR (2005) Essential role for Galpha13 in endothelial cells during embryonic development. Proc Natl Acad Sci U S A 102:8281–8286. doi:10.1073/pnas.0503326102
Ye D, Yang Q, Li Y, Huang X, Hu J, Qian S, Tan Z, Song P (2011) Galpha13 is closely related to hematopoiesis in zebrafish. Mol Biol Rep 38:2685–2694
Bar-Sagi D, Hall A (2000) Ras and Rho GTPases: a family reunion. Cell 103:227–238
Kather JN, Kroll J (2013) Rho guanine exchange factors in blood vessels: fine-tuners of angiogenesis and vascular function. Exp Cell Res 319:1289–1297. doi:10.1016/j.yexcr.2012.12.015
Lee MJ, Thangada S, Claffey KP, Ancellin N, Liu CH, Kluk M, Volpi M, Sha’afi RI, Hla T (1999) Vascular endothelial cell adherens junction assembly and morphogenesis induced by sphingosine-1-phosphate. Cell 99:301–312
Hou TC, Lin JJ, Wen HC, Chen LC, Hsu SP, Lee WS (2013) Folic acid inhibits endothelial cell migration through inhibiting the RhoA activity mediated by activating the folic acid receptor/cSrc/p190RhoGAP-signaling pathway. Biochem Pharmacol 85:376–384. doi:10.1016/j.bcp.2012.11.011
Lai Y, Shen Y, Liu XH, Zhang Y, Zeng Y, Liu YF (2011) Interleukin-8 induces the endothelial cell migration through the activation of phosphoinositide 3-kinase-Rac1/RhoA pathway. Int J Biol Sci 7:782–791
Oviedo PJ, Sobrino A, Laguna-Fernandez A, Novella S, Tarin JJ, Garcia-Perez MA, Sanchis J, Cano A, Hermenegildo C (2011) Estradiol induces endothelial cell migration and proliferation through estrogen receptor-enhanced RhoA/ROCK pathway. Mol Cell Endocrinol 335:96–103. doi:10.1016/j.mce.2010.06.020
Cascone I, Giraudo E, Caccavari F, Napione L, Bertotti E, Collard JG, Serini G, Bussolino F (2003) Temporal and spatial modulation of Rho GTPases during in vitro formation of capillary vascular network. Adherens junctions and myosin light chain as targets of Rac1 and RhoA. J Biol Chem 278:50702–50713. doi:10.1074/jbc.M307234200
Uchida S, Watanabe G, Shimada Y, Maeda M, Kawabe A, Mori A, Arii S, Uehata M, Kishimoto T, Oikawa T, Imamura M (2000) The suppression of small GTPase rho signal transduction pathway inhibits angiogenesis in vitro and in vivo. Biochem Biophys Res Commun 269:633–640. doi:10.1006/bbrc.2000.2315
Washida N, Wakino S, Tonozuka Y, Homma K, Tokuyama H, Hara Y, Hasegawa K, Minakuchi H, Fujimura K, Hosoya K, Hayashi K, Itoh H (2011) Rho-kinase inhibition ameliorates peritoneal fibrosis and angiogenesis in a rat model of peritoneal sclerosis. Nephrol Dial Transplant 26:2770–2779. doi:10.1093/ndt/gfr012
Hsu YL, Wu LY, Hou MF, Tsai EM, Lee JN, Liang HL, Jong YJ, Hung CH, Kuo PL (2011) Glabridin, an isoflavan from licorice root, inhibits migration, invasion and angiogenesis of MDA-MB-231 human breast adenocarcinoma cells by inhibiting focal adhesion kinase/Rho signaling pathway. Mol Nutr Food Res 55:318–327. doi:10.1002/mnfr.201000148
Vincent L, Soria C, Mirshahi F, Opolon P, Mishal Z, Vannier JP, Soria J, Hong L (2002) Cerivastatin, an inhibitor of 3-hydroxy-3-methylglutaryl coenzyme a reductase, inhibits endothelial cell proliferation induced by angiogenic factors in vitro and angiogenesis in in vivo models. Arterioscler Thromb Vasc Biol 22:623–629
Park HJ, Kong D, Iruela-Arispe L, Begley U, Tang D, Galper JB (2002) 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors interfere with angiogenesis by inhibiting the geranylgeranylation of RhoA. Circ Res 91:143–150
Baker GJ, Yadav VN, Motsch S, Koschmann C, Calinescu AA, Mineharu Y, Camelo-Piragua SI, Orringer D, Bannykh S, Nichols WS, deCarvalho AC, Mikkelsen T, Castro MG, Lowenstein PR (2014) Mechanisms of glioma formation: iterative perivascular glioma growth and invasion leads to tumor progression, VEGF-independent vascularization, and resistance to antiangiogenic therapy. Neoplasia 16:543–561. doi:10.1016/j.neo.2014.06.003
Giannarelli C, Alique M, Rodriguez DT, Yang DK, Jeong D, Calcagno C, Hutter R, Millon A, Kovacic JC, Weber T, Faries PL, Soff GA, Fayad ZA, Hajjar RJ, Fuster V, Badimon JJ (2014) Alternatively spliced tissue factor promotes plaque angiogenesis through the activation of hypoxia-inducible factor-1alpha and vascular endothelial growth factor signaling. Circulation 130:1274–1286. doi:10.1161/CIRCULATIONAHA.114.006614
Kumar AH, Martin K, Doyle B, Huang CL, Pillai GK, Ali MT, Skelding KA, Wang S, Gleeson BM, Jahangeer S, Ritman EL, Russell SJ, Caplice NM (2014) Intravascular cell delivery device for therapeutic VEGF-induced angiogenesis in chronic vascular occlusion. Biomaterials 35:9012–9022. doi:10.1016/j.biomaterials.2014.07.016
Jorgens K, Stoll SJ, Pohl J, Fleming TH, Sticht C, Nawroth PP, Hammes HP, Kroll J (2015) High tissue glucose alters intersomitic blood vessels in zebrafish via methylglyoxal targeting the VEGF receptor signaling cascade. Diabetes 64:213–225. doi:10.2337/db14-0352
van Nieuw Amerongen GP, Koolwijk P, Versteilen A, van Hinsbergh VW (2003) Involvement of RhoA/Rho kinase signaling in VEGF-induced endothelial cell migration and angiogenesis in vitro. Arterioscler Thromb Vasc Biol 23:211–217
Gingras D, Lamy S, Beliveau R (2000) Tyrosine phosphorylation of the vascular endothelial-growth-factor receptor-2 (VEGFR-2) is modulated by Rho proteins. Biochem J 348(Pt 2):273–280
Kroll J, Epting D, Kern K, Dietz CT, Feng Y, Hammes HP, Wieland T, Augustin HG (2009) Inhibition of Rho-dependent kinases ROCK I/II activates VEGF-driven retinal neovascularization and sprouting angiogenesis. Am J Physiol Heart Circ Physiol 296:H893–H899. doi:10.1152/ajpheart.01038.2008
Li D, Xie K, Ding G, Li J, Chen K, Li H, Qian J, Jiang C, Fang J (2014) Tumor resistance to anti-VEGF therapy through up-regulation of VEGF-C expression. Cancer Lett 346:45–52. doi:10.1016/j.canlet.2013.12.004
Engelmann D, Mayoli-Nussle D, Mayrhofer C, Furst K, Alla V, Stoll A, Spitschak A, Abshagen K, Vollmar B, Ran S, Putzer BM (2013) E2F1 promotes angiogenesis through the VEGF-C/VEGFR-3 axis in a feedback loop for cooperative induction of PDGF-B. J Mol Cell Biol 5:391–403. doi:10.1093/jmcb/mjt035
Zhang D, Li B, Shi J, Zhao L, Zhang X, Wang C, Hou S, Qian W, Kou G, Wang H, Guo Y (2010) Suppression of tumor growth and metastasis by simultaneously blocking vascular endothelial growth factor (VEGF)-A and VEGF-C with a receptor-immunoglobulin fusion protein. Cancer Res 70:2495–2503. doi:10.1158/0008-5472.CAN-09-3488
Kumar B, Chile SA, Ray KB, Reddy GE, Addepalli MK, Kumar AS, Ramana V, Rajagopal V (2011) VEGF-C differentially regulates VEGF-A expression in ocular and cancer cells; promotes angiogenesis via RhoA mediated pathway. Angiogenesis 14:371–380. doi:10.1007/s10456-011-9221-5
Li X, Liu L, Tupper JC, Bannerman DD, Winn RK, Sebti SM, Hamilton AD, Harlan JM (2002) Inhibition of protein geranylgeranylation and RhoA/RhoA kinase pathway induces apoptosis in human endothelial cells. J Biol Chem 277:15309–15316. doi:10.1074/jbc.M201253200
Yang H, Zhao B, Liao C, Zhang R, Meng K, Xu J, Jiao J (2013) High glucose-induced apoptosis in cultured podocytes involves TRPC6-dependent calcium entry via the RhoA/ROCK pathway. Biochem Biophys Res Commun 434:394–400. doi:10.1016/j.bbrc.2013.03.087
Bocanegra V, Gil Lorenzo AF, Cacciamani V, Benardon ME, Costantino VV, Valles PG (2014) RhoA and MAPK signal transduction pathways regulate NHE1-dependent proximal tubule cell apoptosis after mechanical stretch. Am J Physiol Renal Physiol 307:F881–F889. doi:10.1152/ajprenal.00232.2014
Li F, Jiang Q, Shi KJ, Luo H, Yang Y, Xu CM (2013) RhoA modulates functional and physical interaction between ROCK1 and Erk1/2 in selenite-induced apoptosis of leukaemia cells. Cell Death Dis 4:e708. doi:10.1038/cddis.2013.243
Li G, Liu L, Shan C, Cheng Q, Budhraja A, Zhou T, Cui H, Gao N (2014) RhoA/ROCK/PTEN signaling is involved in AT-101-mediated apoptosis in human leukemia cells in vitro and in vivo. Cell Death Dis 5:e998. doi:10.1038/cddis.2013.519
Augspach A, List JH, Wolf P, Bielek H, Schwan C, Elsasser-Beile U, Aktories K, Schmidt G (2013) Activation of RhoA, B, C by Yersinia Cytotoxic Necrotizing Factor (CNFy) induces apoptosis in LNCaP prostate cancer cells. Toxins (Basel) 5:2241–2257. doi:10.3390/toxins5112241
Xu XT, Song QB, Yao Y, Ruan P, Tao ZZ (2012) Inhibition of RhoA/ROCK signaling pathway promotes the apoptosis of gastric cancer cells. Hepato-Gastroenterology 59:2523–2526. doi:10.5754/hge12147
Higgs HN, Peterson KJ (2005) Phylogenetic analysis of the formin homology 2 domain. Mol Biol Cell 16:1–13. doi:10.1091/mbc.E04-07-0565
Schonichen A, Geyer M (2010) Fifteen formins for an actin filament: a molecular view on the regulation of human formins. Biochim Biophys Acta 1803:152–163. doi:10.1016/j.bbamcr.2010.01.014
Bogdan S, Schultz J, Grosshans J (2013) Formin’ cellular structures: physiological roles of Diaphanous (Dia) in actin dynamics. Commun Integr Biol 6:e27634. doi:10.4161/cib.27634
Rivero F, Muramoto T, Meyer AK, Urushihara H, Uyeda TQ, Kitayama C (2005) A comparative sequence analysis reveals a common GBD/FH3-FH1-FH2-DAD architecture in formins from Dictyostelium, fungi and metazoa. BMC Genomics 6:28. doi:10.1186/1471-2164-6-28
Higgs HN (2005) Formin proteins: a domain-based approach. Trends Biochem Sci 30:342–353. doi:10.1016/j.tibs.2005.04.014
Kursula P, Kursula I, Massimi M, Song YH, Downer J, Stanley WA, Witke W, Wilmanns M (2008) High-resolution structural analysis of mammalian profilin 2a complex formation with two physiological ligands: the formin homology 1 domain of mDia1 and the proline-rich domain of VASP. J Mol Biol 375:270–290. doi:10.1016/j.jmb.2007.10.050
Chang F, Drubin D, Nurse P (1997) cdc12p, a protein required for cytokinesis in fission yeast, is a component of the cell division ring and interacts with profilin. J Cell Biol 137:169–182
Watanabe N, Madaule P, Reid T, Ishizaki T, Watanabe G, Kakizuka A, Saito Y, Nakao K, Jockusch BM, Narumiya S (1997) p140mDia, a mammalian homolog of Drosophila diaphanous, is a target protein for Rho small GTPase and is a ligand for profilin. EMBO J 16:3044–3056. doi:10.1093/emboj/16.11.3044
Shinohara R, Thumkeo D, Kamijo H, Kaneko N, Sawamoto K, Watanabe K, Takebayashi H, Kiyonari H, Ishizaki T, Furuyashiki T, Narumiya S (2012) A role for mDia, a Rho-regulated actin nucleator, in tangential migration of interneuron precursors. Nat Neurosci 15(373–380):S371–S372. doi:10.1038/nn.3020
Sakamoto S, Narumiya S, Ishizaki T (2012) A new role of multi scaffold protein Liprin-alpha: Liprin-alpha suppresses Rho-mDia mediated stress fiber formation. Bioarchitecture 2:43–49
Lammers M, Meyer S, Kuhlmann D, Wittinghofer A (2008) Specificity of interactions between mDia isoforms and Rho proteins. J Biol Chem 283:35236–35246. doi:10.1074/jbc.M805634200
DeWard AD, Leali K, West RA, Prendergast GC, Alberts AS (2009) Loss of RhoB expression enhances the myelodysplastic phenotype of mammalian diaphanous-related Formin mDia1 knockout mice. PLoS One 4:e7102. doi:10.1371/journal.pone.0007102
Li F, Higgs HN (2005) Dissecting requirements for auto-inhibition of actin nucleation by the formin, mDia1. J Biol Chem 280:6986–6992. doi:10.1074/jbc.M411605200
Li F, Higgs HN (2003) The mouse Formin mDia1 is a potent actin nucleation factor regulated by autoinhibition. Curr Biol 13:1335–1340
Watanabe N, Kato T, Fujita A, Ishizaki T, Narumiya S (1999) Cooperation between mDia1 and ROCK in Rho-induced actin reorganization. Nat Cell Biol 1:136–143
Sakamoto S, Ishizaki T, Okawa K, Watanabe S, Arakawa T, Watanabe N, Narumiya S (2012) Liprin-alpha controls stress fiber formation by binding to mDia and regulating its membrane localization. J Cell Sci 125:108–120. doi:10.1242/jcs.087411
Li Z, Xu Y, Zhang C, Liu X, Jiang L, Chen F (2014) Mammalian diaphanous-related formin 1 is required for motility and invadopodia formation in human U87 glioblastoma cells. Int J Mol Med 33:383–391. doi:10.3892/ijmm.2013.1577
Dong B, Zhang SS, Gao W, Su H, Chen J, Jin F, Bhargava A, Chen X, Jorgensen L, Alberts AS, Zhang J, Siminovitch KA (2013) Mammalian diaphanous-related formin 1 regulates GSK3beta-dependent microtubule dynamics required for T cell migratory polarization. PLoS One 8:e80500. doi:10.1371/journal.pone.0080500
Carramusa L, Ballestrem C, Zilberman Y, Bershadsky AD (2007) Mammalian diaphanous-related formin Dia1 controls the organization of E-cadherin-mediated cell-cell junctions. J Cell Sci 120:3870–3882. doi:10.1242/jcs.014365
Gavard J, Patel V, Gutkind JS (2008) Angiopoietin-1 prevents VEGF-induced endothelial permeability by sequestering Src through mDia. Dev Cell 14:25–36. doi:10.1016/j.devcel.2007.10.019
Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, O’Shea KS, Powell-Braxton L, Hillan KJ, Moore MW (1996) Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature 380:439–442. doi:10.1038/380439a0
Suri C, Jones PF, Patan S, Bartunkova S, Maisonpierre PC, Davis S, Sato TN, Yancopoulos GD (1996) Requisite role of angiopoietin-1, a ligand for the TIE2 receptor, during embryonic angiogenesis. Cell 87:1171–1180
Kamasani U, Duhadaway JB, Alberts AS, Prendergast GC (2007) mDia function is critical for the cell suicide program triggered by farnesyl transferase inhibition. Cancer Biol Ther 6:1422–1427
Fan Y, Potdar AA, Gong Y, Eswarappa SM, Donnola S, Lathia JD, Hambardzumyan D, Rich JN, Fox PL (2014) Profilin-1 phosphorylation directs angiocrine expression and glioblastoma progression through HIF-1alpha accumulation. Nat Cell Biol 16:445–456. doi:10.1038/ncb2954
Wang R, Cleary RA, Wang T, Li J, Tang DD (2014) The association of cortactin with profilin-1 is critical for smooth muscle contraction. J Biol Chem 289:14157–14169. doi:10.1074/jbc.M114.548099
Yu LX, Parthasarathy MV (2014) Molecular and cellular characterization of the tomato pollen profilin, LePro1. PLoS One 9:e86505. doi:10.1371/journal.pone.0086505
Montani L, Buerki-Thurnherr T, de Faria JP, Pereira JA, Dias NG, Fernandes R, Goncalves AF, Braun A, Benninger Y, Bottcher RT, Costell M, Nave KA, Franklin RJ, Meijer D, Suter U, Relvas JB (2014) Profilin 1 is required for peripheral nervous system myelination. Development 141:1553–1561. doi:10.1242/dev.101840
Courtemanche N, Pollard TD (2013) Interaction of profilin with the barbed end of actin filaments. Biochemistry 52:6456–6466. doi:10.1021/bi400682n
Witke W, Sutherland JD, Sharpe A, Arai M, Kwiatkowski DJ (2001) Profilin I is essential for cell survival and cell division in early mouse development. Proc Natl Acad Sci U S A 98:3832–3836. doi:10.1073/pnas.051515498
Tseng PC, Runge MS, Cooper JA, Williams RC Jr, Pollard TD (1984) Physical, immunochemical, and functional properties of Acanthamoeba profilin. J Cell Biol 98:214–221
Schluter K, Jockusch BM, Rothkegel M (1997) Profilins as regulators of actin dynamics. Biochim Biophys Acta 1359:97–109
Carlsson L, Nystrom LE, Sundkvist I, Markey F, Lindberg U (1977) Actin polymerizability is influenced by profilin, a low molecular weight protein in non-muscle cells. J Mol Biol 115:465–483
Theriot JA, Mitchison TJ (1993) The three faces of profilin. Cell 75:835–838
Pantaloni D, Carlier MF (1993) How profilin promotes actin filament assembly in the presence of thymosin beta 4. Cell 75:1007–1014
Ding Z, Gau D, Deasy B, Wells A, Roy P (2009) Both actin and polyproline interactions of profilin-1 are required for migration, invasion and capillary morphogenesis of vascular endothelial cells. Exp Cell Res 315:2963–2973. doi:10.1016/j.yexcr.2009.07.004
Shields AR, Spence AC, Yamashita YM, Davies EL, Fuller MT (2014) The actin-binding protein profilin is required for germline stem cell maintenance and germ cell enclosure by somatic cyst cells. Development 141:73–82. doi:10.1242/dev.101931
Lassing I, Lindberg U (1985) Specific interaction between phosphatidylinositol 4,5-bisphosphate and profilactin. Nature 314:472–474
Reinhard M, Giehl K, Abel K, Haffner C, Jarchau T, Hoppe V, Jockusch BM, Walter U (1995) The proline-rich focal adhesion and microfilament protein VASP is a ligand for profilins. EMBO J 14:1583–1589
Suetsugu S, Miki H, Takenawa T (1998) The essential role of profilin in the assembly of actin for microspike formation. EMBO J 17:6516–6526. doi:10.1093/emboj/17.22.6516
Bonacci TM, Hirsch DS, Shen Y, Dokmanovic M, Wu WJ (2012) Small GTPase Rho regulates R-cadherin through Dia1/profilin-1. Cell Signal 24:2102–2110
Moustafa-Bayoumi M, Alhaj MA, El-Sayed O, Wisel S, Chotani MA, Abouelnaga ZA, Hassona MD, Rigatto K, Morris M, Nuovo G, Zweier JL, Goldschmidt-Clermont P, Hassanain H (2007) Vascular hypertrophy and hypertension caused by transgenic overexpression of profilin 1. J Biol Chem 282:37632–37639. doi:10.1074/jbc.M703227200
Da Silva JS, Medina M, Zuliani C, Di Nardo A, Witke W, Dotti CG (2003) RhoA/ROCK regulation of neuritogenesis via profilin IIa-mediated control of actin stability. J Cell Biol 162:1267–1279. doi:10.1083/jcb.200304021
Romeo G, Frangioni JV, Kazlauskas A (2004) Profilin acts downstream of LDL to mediate diabetic endothelial cell dysfunction. FASEB J 18:725–727. doi:10.1096/fj.03-0841fje
Yao W, Yu X, Fang Z, Yin P, Zhao C, Li N, Wang L, Li Z, Zha X (2012) Profilin1 facilitates staurosporine-triggered apoptosis by stabilizing the integrin beta1-actin complex in breast cancer cells. J Cell Mol Med 16:824–835. doi:10.1111/j.1582-4934.2011.01369.x
Yao W, Cai X, Liu C, Qin Y, Cheng H, Ji S, Xu W, Wu C, Chen T, Xu J, Long J, Fang Z, Qu B, Hoth M, Ni Q, Zha X, Yu X (2013) Profilin 1 potentiates apoptosis induced by staurosporine in cancer cells. Curr Mol Med 13:417–428
Acknowledgments
This work was supported by grants from the National Nature Science Foundation of China (81271032).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lu, Q., Lu, L., Chen, W. et al. RhoA/mDia-1/profilin-1 signaling targets microvascular endothelial dysfunction in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 253, 669–680 (2015). https://doi.org/10.1007/s00417-015-2985-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-2985-3