Abstract
Aims
Keratan sulphate (KS) is the predominant glycosaminoglycan (GAG) present in the corneal stroma where it is thought to regulate collagen fibril diameter. In this study we investigated the distribution of KS in normal and keratoconic corneas.
Methods
Four normal, one mild, and four severe keratoconic corneas were used for the study. Distribution of keratan sulphate proteoglycans (KS-PG) was investigated using a primary monoclonal antibody (5-D-4) that recognizes disulphated disaccharides in the poly-N-acetyllactosamine repeats of KS. The immuno-reactivity of 5-D-4 was analyzed by immunohistochemistry and immuno-electron microscopy.
Results
Immuno-histochemistry showed diffuse 5-D-4 staining in keratoconic cornea compared to the punctuate staining in normal corneas. In the single cornea with mild keratoconus, immunogold microscopy revealed a very high density of KS-PG staining, especially in the posterior stroma, compared to severe keratoconic and normal cornea. The amount of KS-PG in the stroma in severe keratoconus was slightly less compared to the normal cornea. In the mild keratoconic cornea, a higher quantity of KS-PG was present around the keratocytes. In severe keratoconic corneas, a higher quantity of KS-PG was present within the keratocytes compared to normal cornea.
Conclusions
The finding of an altered expression of KS in our keratoconic corneas, in particular the strong expression of KS in keratocytes, is in keeping with reports of an altered expression of proteoglycan metabolism in keratoconus. KS-PG plays an important role in stromal collagen fibril assembly and a dysregulation of KS-PG synthesis or catabolism could explain changes in collagen fibril spacing and diameter, which we have reported elsewhere.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keratoconus is a disease that causes thinning, ectasia, and scarring of the central cornea, which leads to visual impairment [1]. The role of keratan sulphate proteoglycans (KS-PG) and other proteoglycans and proteins in its etiology has been investigated in previous studies. In normal cornea, KS-PG is the major proteoglycan, while dermatan sulphate proteoglycan makes up the remainder [2–4]. Yue et al. (1984) [5] reported a decrease in total protein and an increase in the non-proteinaceous (uronic acid) component in keratoconic corneas and cultured keratoconic stromal cells. It was suggested that the stromal cells have a reduced ability to synthesize proteins [5]. Later histochemical studies by Yue et al. (1984) [6], using safranin O, showed an enhancement of staining for glycosaminoglycan polyanions, indicating an accumulation of proteoglycan molecules in keratoconic corneas.
It has been suggested that keratan sulphate, dermatan sulphate, and its associated core proteins are important for the organization of collagen fibrils and lamellar adhesion in corneal stroma [7, 8]. Keratan sulphate is also concerned in maintaining a level of tissue hydration critical for corneal transparency. At hydration levels characteristic of normal corneal stroma, dermatan sulphate is fully hydrated whereas keratan sulphate is only partially hydrated, suggesting that it could have a regulatory role in corneal hydration [9].
Keratan sulphate consists of a linear, poly-N-acetyllactosamine chain that carries sulphate residues on C-6 of GlcNAc and Gal. Because sulphation of carbohydrates affects their biochemical characteristics, such as water solubility and electrical charge, this modification appears to be important for the function of keratan sulphate proteoglycans in the cornea. The importance of keratan sulphate sulphation in the cornea is also suggested by the finding that a lack of keratan sulphate sulphation is responsible for diffuse stromal clouding in the congenital hereditary eye disorder, macular corneal dystrophy (MCD1) [10–13].
Funderburgh et al. 1990 [14] found decreased antigenicity of keratan sulphate in keratoconic cornea, reduced in the central, thinned region of the corneal buttons and near normal at their periphery. Further studies by solid-phase immunoassay also showed a modified structure of keratan sulphate [14]. In those studies, the KS-PG contained fewer, or shorter, sulphated KS chains, but the amount of KS core protein remained unaltered. Sawaguchi et al. (1991) [15] studied proteoglycans using immunohistochemical and electron microscopic histochemical methods. They reported that KS-PG staining was reduced and dermatan sulphate staining was increased in keratoconic corneas. Electron microscopic histochemical studies using cuprolinic dye also showed the presence of large dermatan sulphate filaments and less abundant KS-PG filaments compared to normal cornea [8].
We hypothesize that an alteration in KS distribution disturbs the organization of collagen fibrils and lamellae in keratoconic cornea. In the present study we investigated the distribution of KS in normal and keratoconic corneas using the antibody 5-D-4, which recognizes linear, disulphated N-acetyl lactosamine disaccharide-containing moieties in KS [16–20]. For ultrastructural studies, KS distribution was studied in scar-free regions of the stroma where the overlying Bowman’s layer was intact. We report here the data from four normal cornea and five keratoconic corneas of differing age, with and without scarring.
Materials and methods
Four normal (24–75 years old) and five keratoconic (24–52 years old) corneal buttons, obtained at keratoplasty, were used in the present study. In one cornea there was no preoperative biomicroscopic evidence of scarring and we refer to this as ‘mild’ keratoconus. The mild keratoconic cornea in our study was obtained from a builder who elected to have surgery because he was unhappy about wearing contact lenses in a dusty environment. The diagnosis of keratoconus was based on corneal topography, apical corneal thinning, and the presence of a partial Fleischer ring. No breaks in Bowman’s membrane or corneal scars were observed biomicroscopically. The other four keratoconic buttons all showed visible scarring and are referred to here as ‘severe’. All keratoconus donors had given permission to use their tissue for research. Tissue procurement and use was in accordance with the Declaration of Helsinki and local regulations. It has been ethically approved by the local ethical committee; Pontypridd & Rhondda NHS Trust Ethical Committee. The normal donor eyes were obtained from the US National Disease Research Interchange. Each of the buttons was divided into two parts, one part was fixed in 10% formalin for immuno-histochemistry and the other in 4% paraformaldehyde, for immunoelectron microscopy.
The distribution of KS-PGs was investigated using a primary monoclonal antibody 5-D-4 that recognizes linear, disulphated N-acetyl lactosamine disaccharide-containing moieties in KS [16–20]. The immuno-reactivity of 5-D-4 was analyzed by immuno-histochemistry and immuno-electron microscopy. The antibody does not discriminate between different KS-types. The specificity of the antibody for human antigens was tested and confirmed by immunoassay.
Immunohistochemistry
Human corneal samples were fixed in 4% paraformaldehyde, and embedded in paraffin wax. The wax blocks were cross-sectioned at 10 μm. Wax sections were immersed in xylene and a graded series of ethanol to remove wax from the sections and then were washed briefly in PBS (pH 7.4) prior to immuno-fluorescent labeling. The sections were washed in PBS containing 0.001% Tween for 10 min before blocking with normal goat serum (Dako; X0907) at 1:20 dilution for 30 min at room temperature. Adjacent tissue sections were then incubated overnight at 4°C with monoclonal antibodies 5-D-4 at 1:50 dilution. To check for non-specific labeling, the primary antibody was replaced with native mouse immunoglobulin (Dako; X0931). We did not explore specificity further either by digesting KS in sections or preincubating antibody with an excess of KS [14]. After overnight incubation with primary antibody, the sections were washed in buffer for 10 min and incubated with a goat anti-mouse FITC-conjugated secondary antibody (Dako; F0479) at 1:50 dilution for 1 h at room temperature. The sections were washed for 10 min before counterstaining with 0.5 μg/ml propidium iodide (Sigma; P-4170) for 5 min at room temperature. The sections were again washed before mounting under coverslips with Vectashield mountant (Vector Labs; H-1000). Representative regions of cornea were scanned on an Olympus fluorescence microscope. Optical sections were presented as green/red anaglyph images.
Immuno-electron Microscopy
All corneal tissues were fixed in freshly prepared 4% paraformaldehyde (PFA) + 0.5% glutaraldehyde in 0.1 M phosphate for 2 h at 4°C within 30 min after removal from the eye. Tissue for immuno-electron microscopy was obtained from the central region of the hemi-buttons and was embedded and polymerized in LR White [20]. Ultrathin sections were cut (Reichert Ultracut Microtome) from the blocks and collected on 200 mesh formvar-carbon nickel grids.
As scarring itself induces changes in CF and PG structure and organization, we compared normal corneal stroma with scar-free regions of the corneas with severe keratoconic. In order to achieve this, we selected regions from the severe keratoconic blocks, adjacent to scar-free regions that had been assessed by semi-thin sectioning and toluidine blue staining. Bowman’s membrane was intact in these regions in both the mild and severe keratoconic corneas.
Monoclonal antibody 5-D-4 (1:100 to 1:500) was used as the primary antibody to localize keratan sulphate in the normal and keratoconic human cornea. The antibody was visualized with 10-nm goat anti-mouse immunogold conjugate (1:25). The immunogold conjugates, goat serum, bovine serum and Tween-20 were supplied by Biocell, Cardiff, UK. Immunostaining of the sections was performed as described in Akhtar et al. 2001 [20].
Sections were stained with 2% aqueous uranyl acetate and lead citrate. Sections were examined in a JEOL 1010 transmission electron microscope and gold particles were counted in anterior, middle, and posterior zones of the stroma. The center of the ‘anterior’ zone was within 20 μm posterior to the posterior edge of Bowman’s layer, the center of the posterior zone was within 20 μm anterior to the anterior edge of Descemet’s membrane, and the ‘middle’ zone was estimated to be roughly in the middle of the width of the particular section which was under examination. Five images were taken from each zone and gold counted from these images. Gold particles were analyzed overall by using the Soft Imaging System (AnalySIS, Soft Imaging System GmbH, Münster, Germany) analysis program.
Results
Immuno-histochemistry
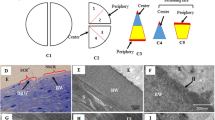
Negative controls showed no non-specific labeling of the corneal tissue (Fig. 1a). Comparison of immuno-fluorescent labeling patterns with monoclonal antibodies 5-D-4 in the normal corneas and the mild keratoconic and severe keratoconic corneas, showed different distributions of keratan sulphate. The staining pattern in normal corneas was clearly defined (Fig. 1b) whereas in keratoconic it was diffuse and aggregated in places (Fig. 1c). In normal corneas, immunolabeled KS was observed as elongated streaks adjacent to collagen bundles (arrow) whereas in keratoconic corneas this defined pattern of streaks was not observed. There were aggregated spots of immunofluorescence in keratoconic stroma, suggesting the aggregation of KS-PG in some parts of the stroma (arrowhead) (Fig. 1c).
Immuno-fluorescent localization of keratan sulphate with monoclonal antibody 5-D-4 in normal human and severe keratoconic cornea. a Control of immuno-fluorescent. b In normal cornea, keratan sulphate is immuno-localized throughout the stroma and gives a clearly defined staining pattern. Elongate, fibrillar streaks and rows of punctuate KS immunolabel interposed between adjacent collagen fiber bundles (arrowheads). c In keratoconus cornea, keratan sulphate was also detectable throughout the stroma but its organization was markedly different to that of control corneas. Instead of it being highly organized at the surface of collagen fibril bundles as elongated streaks of immunolabel (arrowheads), it was diffusely distributed throughout the stroma, occurring as punctate foci of fluorescent label (arrowheads)
Ultrastructural localization in normal and keratoconic cornea
In normal corneas, the 5-D-4 KS-PG labeling was very low or absent in the epithelial basement membrane (Fig. 2a) but well distributed in the epithelium, Bowman’s layer throughout the stroma, and Descemet’s membrane (not shown). Moderate labeling of KS-PG was also observed within keratocytes (Fig. 2b) and endothelial cells. Within normal cornea, the highest KS-PG was observed in Descemet’s membrane and the posterior stroma compared to other parts.
Immuno-gold localization of KS with monoclonal antibody 5-D-4. a Low labeling in basement in normal cornea. b Moderate labeling in and around the keratocytes and stroma of normal cornea. c Strong labeling in thick basement below degenerate hemidesmosomes in mild keratoconic cornea. d Labeling in Bowman’s layer of mild keratoconic cornea. e Degenerate hemidesmosomes, thick basement membrane, and Bowman’s layer in severe keratoconic cornea. f Immuno-gold localization of keratan sulphate with monoclonal antibodies 5-D-4 in basement material and on microfibrils present in basement membrane of severe keratoconic cornea (B Bowman’s layer, BM Basement membrane, E Epithelial cells, H Hemidesmosomes, KR Keratocytes, MF Microfibrils, S Stroma)
In mildly keratoconic cornea, large amounts of KS-PG were observed in the epithelial basement membrane, Bowman’s layer, stroma, and Descemet’s membrane. A large aggregation of gold particles localizing KS-PG was observed below the hemidesmosomes in the thickened, electron-dense basement membrane (Fig. 2c) and in the Bowman’s layer (Fig. 2d). In severe keratoconic corneas, the basement membrane was very thick and contained numerous, embedded microfibrils (Fig. 2e) and hemidesmosomes were arc-shaped (Fig. 2e). There was a moderate amount of KS-PG present in the basement membrane (Fig. 2e). Gold particles, localizing KS-PG, were observed around the micro-fibrils and in the basement membrane material (Fig. 2f). The basement membrane and Bowman’s layer of keratoconic cornea had higher amounts of KS-PG compared to normal cornea.
In the stroma of the mildly keratoconic cornea, the amount of KS-PG labeling was very intense (Fig. 3a) and a large amount aggregated on microfibrillar material distributed in the stroma. In the severely keratoconic corneas, there was strong labeling with antibody throughout the stroma, similar to that of the mildly keratoconic cornea. In severely keratoconic buttons, KS-PG was also observed within collagen fibrils (Fig. 3b). The labeling was in pairs on the longitudinal collagen fibrils (Fig. 3b). There were numerous microfibrils scattered in the stroma, which also labeled strongly with antibody (Fig. 3c). The mildly keratoconic stroma had higher amounts of KS-PG compared to both normal cornea and severe keratoconus. In severe keratoconus, the amount of labeling of KS-PG in anterior stroma was similar to that observed in the normal stroma, but in the middle and posterior stroma, KS-PG was less compared to normal cornea. The amount of labeling in Descemet’s membrane was intense in both mild and severe keratoconic corneas (Fig. 3d) and similar to that in the normal stroma.
Immuno-gold localization of KS with monoclonal antibody 5-D-4. a Strong labeling of 5-D-4 in stroma of mild keratoconic cornea. b Strong labeling in stroma; note that gold particles are present within collagen fibrils and some of them are in pairs (arrowhead), in severe keratoconic. c Labeling on microfibrils present in stroma of severe keratoconic cornea. d Strong labeling in Descemet’s membrane of mild keratoconic cornea. e Strong labeling around the keratocytes and moderate labeling in the keratocytes of mild keratoconic. f Strong labeling in the keratocytes of severe keratoconic (CF Collagen fibrils, DM Descemet’s membrane, F Fibrils, FL microfibrils, KR Keratocytes, S Stroma)
Degenerate keratocytes were observed in both mild and severe keratoconic corneas. The labeling of KS-PG was low within keratocytes of the mild keratoconic cornea but was strong in the aggregates of microfibrillar material around the keratocytes in most parts of the stroma (Fig. 3e). In severely keratoconic corneas, some of the keratocytes were without cell organelles and appeared empty on electron microscopy but were strongly labeled with gold particles localizing the KS-PG (Fig. 3f). The KS-PG was also packed in vacuoles and lysosomes in the keratocytes of the posterior stroma. The distribution of KS-PG around the keratocytes was higher in the mildly keratoconic cornea compared to the normal and severely keratoconic corneas whereas within the keratocytes, KS-PG was higher in severely keratoconic compared to the mildly keratoconic and normal corneas (Fig. 3c).
The labeling of 5D4 was analyzed from the digital images processed (AnalySIS; Soft Imaging System GmbH). Table 1 shows the quantitative analysis of the antibody labeling in Bowman’s layer and at different depths in the normal and keratoconic cornea. The mild keratoconus cornea had higher density of KS-PGs compared to normal cornea and severe keratoconus. The severe keratoconus had less density of KS-PGs compared to normal cornea, especially in the middle and posterior stroma. The total amount of KS-PG was highest in mild keratoconic cornea and lowest in normal cornea.
Discussion
The present study demonstrates the distribution of keratan sulphate in keratoconic and normal corneas with the use of antibody 5-D-4. In cornea, the candidates for proteoglycan 5-D-4 labeling are the so-called ‘small leucine-rich proteoglycans’ lumican, keratocan, and mimecan. They each possess keratan sulphate chains and are concerned with the regulation of the formation of the stromal extracellular matrix [21]. Labeling with the monoclonal antibody 5-D-4 therefore identifies the presence of one or all of these PGs. The antibody 5-D-4 localizes all the KS-PG sulphate groups without discriminating between sulphate groups from newly formed KS-PG or sulphate groups released from degraded KS-PG.
Our ultrastructural studies showed a marked difference in the intensity of keratan sulphate (KS) labeling in certain regions of the normal and keratoconic corneas. Although we were only able to study a single corneal specimen from a patient with mild keratoconus, we believe that the findings may give insight into the evolution of the disease, which may be pursued in future studies. Interpretation of structural studies of keratoconus are potentially impaired by the examination of tissue at a stage when secondary events obscure the primary mechanism of the disease. We therefore use these observations cautiously, for hypothesis generation. In the stroma of the single cornea with mild keratoconus, there was a very high intensity of KS labeling, especially in the posterior stroma, compared to severe keratoconic and normal corneas. This could be due to a higher population of active cells in the posterior region of the mildly keratoconic cornea. In the stroma of the severely keratoconic corneas, the amount of KS labeling was slightly less compared to normal corneal stroma. These findings were consistent with the report of Funderburgh et al. (1989) [2] who found a reduction in KS-PG in keratoconic corneas compared to normal corneas, but with no significant difference in the amount of KS-PG core protein antigens in keratoconic and normal corneal extracts. They suggested that keratoconic cornea had a form of KS-PG that contained fewer keratan sulphate chains or in which the keratan sulphate had a modified structure [2, 7]. In the corneal buttons from keratoconus patients, the stroma of the mildly keratoconic cornea showed a higher KS labeling than that from the severely keratoconic corneas. Since only one mild keratoconus button was available for study, our interpretation must be cautious, but higher labeling could be due to unmasking of the 5-D-4 epitope in the mildly keratoconic cornea, which was later reduced by degradation in the more severe stage of the disease. In the basement membrane and Bowman’s layer the intensity of labeling for KS-PG was higher in both mild and severe keratoconic cornea compared to normal cornea. An important feature of the study was the presence of KS labeling in and around the keratocytes. There was a higher degree of KS labeling around keratocytes in mild keratoconic corneas and a larger quantity of KS labeling within the keratocytes of the severely keratoconic corneas. The accumulation of the 5-D-4 was mostly within and around degenerate keratocytes.
In the present study, degeneration of keratocytes was observed in both mild and severe keratoconic corneas. This could be due to an alteration in the activity of lysosomal enzymes. It has been reported that morphological changes occur in the early stages of keratoconus due to an increased activity of lysosomal enzymes, but these changes were masked (could not be detected) due to extensive damage in the cornea [22]. A marked increase in the lysosomal enzymes cathepsins B and G, in keratocytes was reported, not only in the anterior stroma but also deep in the posterior stroma of the central cornea [23, 24] as well as in the peripheral cornea [16, 24]. Cathepsin G is responsible for the degradation of type VI collagen [25], which is a major component of the extracellular matrix in human cornea [26, 27] and is thought to be involved in cell to matrix and matrix to matrix interactions. The destruction of keratocytes could also be caused by higher levels of H2O2 production [28].
Our study showed that in the early stages of keratoconus, Bowman’s layer was intact and no degeneration was observed in that area. However, there were high levels of the KS aggregation within and around the keratocytes in the anterior stroma as well as in the posterior stroma. We hypothesize that in the early stages of keratoconus, the over-sulphated domains of keratan sulphate (recognized by 5-D-4) accumulate inside the keratocytes, due to a lack of outward transport into the matrix. This could be due to degradation of type VI collagen by the lysosomal enzyme cathepsin G [25], which is thought to be involved in cell-to-matrix and matrix-to-matrix interactions [25]. In the more severely keratoconic corneas, the accumulation of over-sulphated domains was greater within keratocytes. This could be due to deficiency of the enzymes that are involved in removing sulphate groups from the GAGs that are endocytosed by the corneal cells over time, and due to inhibition of intercellular pathways by increase in the number of IL-1α receptors [29]. This disturbance in the synthesis of KS-PG and catalysis of waste products within the cell is thought to lead to dysregulation of KS-PG in the extracellular matrix. Labeling of 5-D4 was observed between collagen fibrils and within collagen fibrils, as shown in Fig. 3b. The presence of 5-D-4 inside the collagen fibril (Fig. 3b) is a novel finding that has not been previously observed in the cornea. The presence of PG within collagen fibrils has been shown by Akhtar et al. (2008) [30]. It suggests an abnormal fibrillogenesis in keratoconic corneas.
In the normal cornea, keratan sulphate proteoglycans are located both between collagen fibrils, within lamellae and also between lamellae. Small interstitial proteoglycans (lumican, keratocan, and mimecan) [4, 31] are involved in collagen fibrillogenesis and maintain the architecture and biomechanical properties of the normal cornea. In keratoconic corneas, we suggest that a disturbance in the synthesis and catalysis of keratan sulphate (KS-PG) within cells may lead to dysregulation of proteoglycan turnover in the extracellular matrix. We propose that the KS-proteoglycan catabolism occurs between the collagen lamellae and leads to a loss of KS-proteoglycans and accumulation of proteoglycan degradation products. This could increase PG catabolism and compromise the adhesion of lamellae, leading to their slippage, and an alteration in inter-fibrillar spacing of collagen fibrils within lamellae and accumulation of intra-fibrillar proteoglycans (Fig. 3b). This dysregulation of large PGs might affect the leucine-rich PGs that could lead to the disturbance in fibrillogenesis. Simultaneous malfunctioning of keratocytes could affect the synthesis of collagen and PGs and lead to the formation of very small and very large collagen fibrils, and the accumulation of abnormal PGs in the cells and in the matrix.
Conclusions
The KS-PGs plays an important role in stromal collagen fibril assembly. We interpret the findings here to a dysregulation of KS-PG synthesis or catabolism and propose that it could explain the distribution of PGs in keratoconic corneas and changes in collagen fibrillogenesis and fibril spacing and diameter, which we have reported elsewhere [30].
References
Bron AJ (1988) Keratoconus. Cornea 7:163–169
Funderburgh JL, Panjwani N, Conrad GW, Baum J (1989) Altered keratan sulfate epitopes in keratoconus. Investig Ophthalmol Vis Sci 30:2278–2281
Gregory JD, Damle SP, Covington HI, Cintron C (1988) Developmental changes in proteoglycans of rabbit corneal stroma. Investig Ophthalmol Vis Sci 29:1413–1417
Hassell JR, Newsome DA, Hascall VC (1979) Characterization and biosynthesis of proteoglycans of corneal stroma from rhesus monkey. J Biol Chem 254:12346–12354
Yue BY, Sugar J, Benveniste K (1984) Heterogeneity in keratoconus possible biochemical basis. Proc Soc Exp Biol Med 175:336–341
Yue BY, Sugar J, Schrode K (1988) Histochemical studies of keratoconus. Curr Eye Res 7:81–86
Scott JE, Haigh M (1988) Identification of specific binding sites for keratan sulphate proteoglycans and chondroitin-dermatan sulphate proteoglycans on collagen fibrils in cornea by the use of cupromeronic blue in 'critical-electrolyte-concentration' techniques. Biochem J 253:607–610
Chakravarti S, Magnuson T, Lass JH, Jepsen KJ, LaMantia C, Carroll H (1998) Lumican regulates collagen fibril assembly: skin fragility and corneal opacity in the absence of lumican. J Cell Biol 141:1277–1286
Bettelheim FA, Goetz D (1976) Distribution of hexosamines in bovine cornea. Investig Ophthalmol Vis Sci 15:301–304
Hassell JR, Newsome DA, Krachmer JH, Rodrigues MM (1980) Macular corneal dystrophy: failure to synthesize a mature keratan sulfate proteoglycan. Proc Natl Acad Sci USA 77:3705–3709
Nakazawa K, Hassell JR, Hascall VC, Lohmander LS, Newsome DA, Krachmer J (1984) Defective processing of keratan sulfate in macular corneal dystrophy. J Biol Chem 259:13751–13757
Klintworth GK, Meyer R, Dennis R, Hewitt AT, Stock EL, Lenz ME, Hassell JR, Stark WJ Jr, Kuettner KE, Thonar EJ (1986) Macular corneal dystrophy. Lack of keratan sulfate in serum and cornea. Ophthalmic Paediatr Genet 7:139–143
Akama TO, Nakayama J, Nishida K, Hiraoka N, Suzuki M, McAuliffe J, Hindsgaul O, Fukuda M, Fukuda MN (2001) Human corneal GlcNac 6-O-sulfotransferase and mouse intestinal GlcNac 6-O-sulfotransferase both produce keratan sulfate. J Biol Chem 276:16271–16278
Funderburgh JL, Funderburgh ML, Rodrigues MM, Krachmer JH, Conrad GW (1990) Altered antigenicity of keratan sulfate proteoglycan in selected corneal diseases. Investig Ophthalmol Vis Sci 31:419–428
Sawaguchi S, Yue BY, Chang I, Sugar J, Robin J (1991) Proteoglycan molecules in keratoconus corneas. Investig Ophthalmol Vis Sci 32:1846–1853
Scudder P, Tang PW, Hounsell EF, Lawson AM, Mehmet H, Feizi T (1986) Isolation and characterization of sulphated oligosaccharides released from bovine corneal keratan sulphate by the action of endo-beta-galactosidase. Eur J Biochem 157:365–373
Hounsell EF, Feeney J, Scudder P, Tang PW, Feizi T (1986) 1H-NMR studies at 500 MHz of a neutral disaccharide and sulphated di-, tetra-, hexa- and larger oligosaccharides obtained by endo-beta-galactosidase treatment of keratan sulphate. Eur J Biochem 157:375–384
Mehmet H, Scudder P, Tang PW, Hounsell EF, Caterson B, Feizi T (1986) The antigenic determinants recognized by three monoclonal antibodies to keratan sulphate involve sulphated hepta- or larger oligosaccharides of the poly(N-acetyllactosamine) series. Eur J Biochem 157:385–391
Tang PW, Scudder P, Mehmet H, Hounsell EF, Feizi T (1986) Sulphate groups are involved in the antigenicity of keratan sulphate and mask i antigen expression on their poly-N-acetyllactosamine backbones. An immunochemical and chromatographic study of keratan sulphate oligosaccharides after desulphation or nitrosation. Eur J Biochem 160:537–545
Akhtar S, Bron AJ, Hawksworth NR, Bonshek RE, Meek KM (2001) Ultrastructural morphology and expression of proteoglycans, βig-h3, tenascin-C, fibrillin-1, and fibronectin in bullous keratopathy. Br J Ophthalmol 85:720–731
Kao WWY, Liu CY (2003) Role of lumican and keratocan on corneal transparency. Glycoconj J 19:275–285
Sherwin T, Brookes NH, Loh IP, Poole CA, Clover GM (2002) Cellular incursion into Bowman's membrane in the peripheral cone of the keratoconus cornea. Exp Eye Res 74:473–482
Whitelock RB, Fukuchi T, Zhou L, Twining SS, Sugar J, Feder RS, Yue BY (1997) Cathepsin G, acid phosphatase, and alpha 1-proteinase inhibitor messenger RNA levels in keratoconus corneas. Investig Ophthalmol Vis Sci 38:529–534
Zhou L, Sawaguchi S, Twining SS, Sugar J, Feder RS, Yue BY (1998) Expression of degradative enzymes and protease inhibitors in corneas with keratoconus. Investig Ophthalmol Vis Sci 39:1117–11124
Kielty CM, Lees M, Shuttleworth CA, Woolley D (1993) Catabolism of intact type VI collagen microfibrils: susceptibility to degradation by serine proteinases. Biochem Biophys Res Commun 191:1230–1236
Zimmermann DR, Fischer RW, Winterhalter KH, Witmer R, Vaughan L (1988) Comparative studies of collagens in normal and keratoconus corneas. Exp Eye Res 46:431–442
Reale E, Groos S, Luciano L, Eckardt C, Eckardt U (2001) In the mammalian eye type VI collagen tetramers form three morphologically different aggregates. Matrix Biol 20:37–51
Kenney MC, Chwa M, Atilano SR, Tran A, Carballo M, Saghizadeh M, Vasiliou V, Adachi W, Brown DJ (2005) Increased levels of catalase and cathepsin V/L2 but decreased TIMP-1 in keratoconus corneas: evidence that oxidative stress plays a role in this disorder. Investig Ophthalmol Vis Sci 46:823–832
Bureau J, Fabre EJ, Hecquet C, Pouliquen Y, Lorans G (1993) Modification of prostaglandin E2 and collagen synthesis in keratoconus fibroblasts, associated with an increase of interleukin 1 alpha receptor number. C R Acad Sci III 316:425–430
Akhtar S, Bron AJ, Salvi SM, Hawksworth NR, Tuft SJ, Meek KM (2008) Collagen fibrils and proteoglycans in keratoconus - a quantitative ultra-structural analysis. Acta Ophthalmol 86:764–772
Rada JA, Cornuet PK, Hassell JR (1993) Regulation of corneal collagen fibrillogenesis in vitro by corneal proteoglycan (lumican and decorin) core proteins. Exp Eye Res 56:635–648
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akhtar, S., Bron, A.J., Hayes, A.J. et al. Role of keratan sulphate (sulphated poly -N-acetyllactosamine repeats) in keratoconic cornea, histochemical, and ultrastructural analysis. Graefes Arch Clin Exp Ophthalmol 249, 413–420 (2011). https://doi.org/10.1007/s00417-010-1512-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-010-1512-9