Abstract
The cornea represents the external part of the eye and consists of an epithelium, a stroma and an endothelium. Due to its curvature and transparency this structure makes up approximately 70 % of the total refractive power of the eye. This function is partly made possible by the particular organization of the collagen extracellular matrix contained in the corneal stroma that allows a constant refractive power. The maintenance of such an organization involves other molecules such as type V collagen, FACITs (fibril-associated collagens with interrupted triple helices) and SLRPs (small leucine-rich proteoglycans). These components play crucial roles in the preservation of the correct organization and function of the cornea since their absence or modification leads to abnormalities such as corneal opacities. Thus, the aim of this review is to describe the different corneal collagens and proteoglycans by highlighting their importance in corneal transparency as well as their implication in corneal visual disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vision is important for environmental perception for most animal species. This is made possible in part by the cornea which is the most external part of the eye, defined by its curved shape and transparency. The cornea consists of 3 structures: an epithelium, a stroma which represents approximately 90 % of the total corneal thickness, and an endothelium. The stroma contains mesenchymal cells called keratocytes that secrete an extracellular matrix (ECM) composed mainly of collagen fibrils consisting mostly of type I collagen. The uniform narrow diameter (approximately 30 nm) and the regular organization of these fibrils are necessary for the conservation of the corneal transparency. Such an organization is the result of multiple interactions involving other ECM molecules such as type V collagen, FACITs (fibril-associated collagens with interrupted triple helices) and SLRPs (small leucine-rich proteoglycans). Type V collagen is a quantitatively minor component which is found in tissues where type I collagen is expressed and is involved in the regulation of type I collagen fibril assembly (Sun et al. 2011). FACITs are non-fibrillar collagens that are localized to the surface of collagen fibrils (Gordon and Hahn 2010). They are associated with striated fibrils assembled from fibrillar collagens such as type I collagen (Izu et al. 2011). The localization to the surface of the fibrillar collagens gives FACITs the potential to influence the stability of those collagen fibrils as well as their diameters (Tzortzaki et al. 2003). SLRPs are a family of proteoglycans/glycoproteins that are structurally related but genetically distinct (Zhang et al. 2006). Interactions between fibrillar collagens and SLRPs have been implicated as important regulators of collagen fibrillogenesis. SLRPs play regulatory roles in collagen fibril growth, fibril organization and ECM assembly (Chen and Birk 2013). Physical, chemical and inflammatory corneal injuries or even genetic modifications can result in corneal scarring that is represented by an alteration in corneal structure with loss of visual function. The scarring process involves not only modifications in corneal molecular composition but also in their organization. The principal causes of corneal scarring seem to lie largely in the loss of the perfect organization of the type I collagen fibrils and the increase in the expression of other molecules such as type III collagen, a marker of fibrosis. In fact, type III collagen is highly expressed in wounded cornea and seems to play an important role in corneal scarring (Galiacy et al. 2011).
Thus, in this review, we aim to summarize the different types of collagens and proteoglycans within the corneal structure by highlighting the importance of those molecules in the maintenance of corneal transparency as well as their involvement in corneal dysfunction.
The cornea
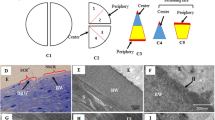
The cornea represents the outermost structure of the eye. Although it is an avascular and transparent tissue, this structure is highly innervated and plays a major role in ocular refraction, contributing to approximately 70 % of the eye’s total refractive power (Hatami-Marbini and Etebu 2013). The cornea is composed of 3 layers: an epithelium, separated from a stroma by a basement membrane (BM). In some species, there is also the presence of a Bowman’s layer between the BM and the stroma. The stroma is separated from the third layer, the endothelium, by the Descemet’s membrane (DM) (Fig. 1).
Corneal epithelium
The epithelium constitutes the most external layer of the cornea. It is immediately in contact with the tear film and the external environment. It represents approximately 8 % of the overall corneal thickness (Alberto and Garello 2013) and is a stratified squamous epithelium. It is composed of three cell layers: the basal (columnar) cell layer, the intermediate (wing/polyhedral) cell layer, and the superficial (squamous) cell layer. The columnar cell layer is a monostratified layer composed of large cells which undergo frequent mitosis. These cells are supported by a thin basal lamina. The wing cells consists of 2–3 layers of polyhedral cells, or 4–5 layers at the corneal periphery, containing tight desmosome junctions that connect them to the basal cells. The squamous cell layer consists of 2 long and flattened cell layers. The more superficial these cells, the flatter they become. They are characterized by the presence of microvilli on their surface, thereby increasing the exchange surface with the tear film. These cells desquamate continuously and are replaced by new cells.
Corneal epithelial basement membrane (CEBM)
The corneal epithelial basal cells secrete CEBM components. These components include type IV collagen, type VII collagen, laminin 332, nidogens and heparan sulfate proteoglycans (Ebihara et al. 2000). The type IV collagen is one of the major components of BMs. Currently, six α (α1-α6) (IV) chains have been identified. The trimer (α1) 2α2 is found in most BMs including the developing CEBM. In adults however, the CEBM expresses the α3, α4 and α5 chains of the type IV collagen and the trimer (α1) 2α2 is expressed only in the presence of CEBM injury (Ljubimov et al. 1995; Maguen et al. 1997; Ljubimov et al. 1998). The anchoring filaments (laminin 332) and “anchoring fibrils” (containing collagen VII) that are associated with this structure ensure the adhesion of the epithelium to the underlying structures. Unlike the skin epithelium, the corneal epithelium rests on a flat, non-corrugated BM allowing constant refractive power.
Bowman’s layer
The Bowman’s layer is an acellular structure and corresponds to a condensation of collagen fibrils (predominantly types I and V; Linsenmayer et al. 1983) and keratan sulfate proteoglycans (Akhtar et al. 2008). It has a thickness of around 17 μm in human (Alberto and Garello 2013). This structure does not regenerate after injury. Its precise role is still unknown. It could play a barrier function to protect against epithelio-stromal interactions and/or protect the stroma from injury (Alberto and Garello 2013).
Corneal stroma
The corneal stroma corresponds to the intermediate layer of the corneal structure and represents about 86 % of the overall corneal thickness (Alberto and Garello 2013). It is a connective tissue mainly composed of a collagen matrix in which mesenchymal cells, the keratocytes, are embedded. The molecular composition of the corneal stroma, as well as the architecture of certain elements contained therein, particularly the type I collagen, plays an important role in the maintenance of the corneal transparency. Indeed, corneal transparency greatly depends on the organization of the type I collagen fibrils, especially their diameter and regular lamellae organization. Such an arrangement is maintained by the association of type I collagen with other ECM molecules such as type V collagen, FACITs and SLRPs. Although, while this aspect of the corneal transparency will not be discussed in this review, it is also important to note that other cellular components such as the crystallins are also indispensable to the corneal transparency since they confer transparency to the keratocytes.
Descemet’s membrane
The Descemet’s membrane (DM) is the BM of the endothelium. This structure is composed of type IV collagen, type VIII collagen, laminin 332, laminin 411, laminin 511 as well as perlecan and nidogens (Kabosova et al. 2007). Its thickness increases with age. For example, in human, the corneal DM thickness goes from 3 μm at birth to 8–10 μm in adulthood. This increase of thickness is also accompanied by modifications in the composition and the distribution of the DM components. For instance, the infant DM contains the α1–α6 chains of type IV collagen on the stromal and endothelial sides, whereas the adult DM contains the α1 and α2 only on the stromal side and α3–α6 exclusively on the endothelial side (Ljubimov et al. 1995; Kabosova et al. 2007). The type VIII collagen also undergoes modifications. Those changes are characterized by a shift of its α1 chain from the endothelial face of the infant DM to the stromal face of the adult’s (Kabosova et al. 2007).
Corneal endothelium
The corneal endothelium consists of a thin cell monolayer that ensures corneal hydric homeostasis. The term endothelium is “consecrated” by usage. It is actually a single layer of flattened epithelium that does not regenerate. The essential function of the endothelium is to regulate corneal hydration and maintain the 78 % water content in the stroma. The endothelium also ensures uptake of nutrients and waste release in the cornea; exchanges that occur with the aqueous humor and that are necessary for the corneal metabolism (Noske et al. 1994; Bonanno 2003).
Corneal wound healing
Disruption of the BM following corneal injury leads to epithelial–stromal interactions that trigger the corneal wound healing process. Such injuries can be traumatic, chemical, inflammatory or infectious, all of which induce corneal matrix remodeling. This involves synthesis and degradation mechanisms that are closely controlled to preserve the transparency of the cornea and take place in normal circumstances without neovascularization. However, this process can also be dysregulated leading to alterations in corneal structure and associated loss of function by scar formation. This involves modifications in corneal molecular composition and organization.
The corneal wound healing process involves modification of the phenotype of keratocytes as well as their matrix environment (Hassell and Birk 2010; Wilson and Kim 1998). The corneal wound healing response starts when an injury affecting the corneal epithelium and stroma occurs. The keratocytes belonging to the wounded area die by apoptosis (Helena et al. 1998; Wilson et al. 1996). The epithelial cells around the wound bed lose their hemidesmosomes and migrate through the stromal injured area. Some of the stromal keratocytes that are still alive become active and proliferate (Del Pero et al. 1990; Hanna et al. 1989; Zieske et al. 2001). This process gives rise to a hypercellular area because of the poor ECM production. However, the low amount of ECM produced by these cells contains keratocan and lumican (Sundarraj et al. 1998). The cytoplasm of these cells contains α-smooth muscle actin (α-SMA) (Jester et al. 1995), a protein implicated in wound contraction and considered as a myofibroblast marker. According to these observations, it has been suggested that these “hypercellular cells” observed earlier during wound healing are in fact “hypercellular myofibroblasts” (Hassell and Birk 2010), a kind of myofibroblasts that produce a low amount of ECM. During the progression of the corneal wound healing process, these “hypercellular myofibroblasts” can then become myofibroblasts that still contain α-SMA but produce large amounts of collagens, hyaluronan and biglycan with low amounts of keratan sulfate proteoglycans to form a disorganized and opaque ECM. These “hypercellular myofibroblasts” can also become “wound fibroblasts” which produce large amounts of collagens as well as keratocan and lumican with keratan sulfate chains to form the normal highly organized ECM that restores transparency (Cintron and Kublin 1977; Cintron et al. 1978; Hassell et al. 1983; Maguen et al. 1997; Funderburgh et al. 1998; Ljubimov et al. 1998; Sundarraj et al. 1998; Dawson et al. 2005). The corneal transparency can also be reestablished in the disorganized and opaque ECM produced by the myofibroblasts by turnover and by the production of an organized ECM (Cintron et al. 1978; Hassell et al. 1983). In this case, the myofibroblasts would have to be substituted or to become “wound fibroblasts”.
Thus, according to the extent of cellular proliferation and ECM production, corneal stromal wound healing can be separated into an initial hypercellulari stage mainly marked by cellular proliferation, followed by a stratification stage which consists mostly of collagen and proteoglycan synthesis (Hassell and Birk 2010).
Crucial components of the cornea and their implication in corneal dysfunction
Type I collagen
Type I collagen, the most abundant of the collagens, is associated with other types of collagen in almost all body tissues. In some tissues, such as bone and tendon, type I represents more than 99 % of total collagen (Bateman et al. 1986). In other tissues, such as blood vessels, skin and cornea, it remains the major collagen where it represents 60, 85 and 75 % of the collagenous component, respectively (Borel and Bellon 1985; Smith et al. 1986; Michelacci 2003). In general, type I collagen is present in all interstitial connective tissues. However, there are a few exceptions such as the brain and the ocular vitreous body (Gelse et al. 2003).
Type I collagen exists as different isoforms. The most common isoform, which is found in cornea, has the chain composition α1 (I)2 α2 (I). Type I collagen can also exist as a homotrimer α1 (I)3 which is resistant to collagenases. Homotrimers occur in fetal tissues, fibrosis, and cancer, where their collagenase resistance may play an important physiological (and pathophysiological) role (Han et al. 2010).
In the corneal stroma, type I collagen, in the form of heterotypic fibrils with type V collagen, ensures the regular organisation lamellae as well as the thin diameter of each fibril (due to type V collagen) that are crucial for corneal transparency (Fournié et al. 2008; Knupp et al. 2009). These fibrils are arranged in 250–300 stacked lamellae each about 2 μm in thickness. Each lamella crosses the entire width of cornea lying parallel to the ocular surface. Disruption of this stromal type I collagen organization can lead to corneal transparency complications such as corneal scarring.
Type III collagen
Type III collagen is a homotrimer composed of three α chains synthesized by the same gene. This collagen is less abundant than type I collagen but is present at different levels of expression in tissues that contain type I collagen with the exception of bone and tendon (Gelse et al. 2003). Type III collagen forms heterotypic fibers by associating with the type I collagen (Cameron et al. 2002). This molecule constitutes an important component of the interstitial tissue reticular fibers of the lung, liver, dermis, spleen and blood vessels. Type III collagen can also be abundant in elastic tissues (Gelse et al. 2003). The molecule is found among the corneal stroma fibrillar collagens but is weakly expressed in the physiological state. However, its expression greatly increases during various corneal pathological processes including wound healing and inflammation (Michelacci 2003). Type III collagen is considered as one of the principal markers of the stromal matrix remodeling observed after corneal injury. Moreover, rabbit corneal inflammation and neovascularisation studies have shown an important increase in this collagen after wounding. Interestingly, this augmentation was only localized in the caustic burn area (Saika et al. 1996). This molecule could be involved in the corneal scarring process observed after injury since its expression is greatly enhanced in the corneal scar (Galiacy et al. 2011). It is thus possible that the modification of the amount of type III collagen and therefore the disruption of the type I/type III collagen ratio might be responsible for the formation of a “haze” in the cornea (Chen et al. 2005).
Type IV collagen
Type IV collagen is the principal structural component of basement membranes (BMs) including the CEBM and the DM. This collagen is important in maintaining the structure and the function of the BMs (Poschl et al. 2004). Currently, six α (α1–α6) (IV) chains have been identified. The trimers (α1)3 and (α1)2 α2 are ubiquitous and form the major components of BMs whereas the α3 (IV), α4 (IV), α5 (IV) and α6 (IV) chains are minor BM components and are tissue-specific (Merjava et al. 2009). The CEBM expresses the trimer (α1)2 α2 of the type IV collagen during the corneal development. However, the adult CEBM predominantly expresses the α3, α4 and α5 chains of the type IV collagen in normal conditions and abundantly expresses the trimer (α1)2 α2 in the presence of CEBM injury (Ljubimov et al. 1995; Maguen et al. 1997; Ljubimov et al. 1998). The corneal DM expresses the six α (α1–α6) (IV) chains. Those six chains are present in the stromal and the endothelial sides of the DM during childhood (Kabosova et al. 2007). The adult DM, however, seems to present in the endothelial side only the α3–α6 chains and the α1 and α2 chains exclusively in the stromal side with a shift of the expression of both the chains from the stromal side to the endothelial side in pathological situations (Merjava et al. 2009).
Disruption of type IV collagen has been shown to lead to several physiological abnormalities including corneal visual impairments in humans. Mutations in the α1 chain of type IV collagen seem to induce severe ocular dysgenesis including anterior segment dysgenesis (ASD), a set of disorders characterized by several ocular clinical abnormalities involving corneal opacification (Van Agtmael et al. 2005; Rodahl et al. 2013). The implication of the type IV collagen in ASD including corneal opacities has also been confirmed by knocking out this gene in mouse (Gould et al. 2007). This collagen also seems to play a role in the posterior polymorphous corneal dystrophy (PPCD), which is a bilateral, autosomal dominant disease that affects, in the first place, the endothelium and the DM. Type IV collagen shows changes in terms of its level of expression but also in its localization in the corneas affected by PPCD (Merjava et al. 2009). Proteolysis of type IV collagen also leads to the release of tumstatin, which is a potent endogenous anti-angiogenic fragment (Esipov et al. 2012).
Type V collagen
Type V collagen is a quantitatively minor fibrillar collagen which is found in tissues where type I collagen is expressed. Several studies have shown that type I collagen may be associated with type V collagen by forming fibrils with a very small diameter. These interactions between type I collagen and type V collagen seem to be different from one corneal structure to another. In fact, this association in the corneal Bowman’s layer appears to expose epitopes of the triple helical domain of the type V collagen while in the corneal stroma those epitopes are not available for antibody detection without disruption to the structure of the heterotypic fibrils (Gordon et al. 1994). The best understood form of this collagen is found in striated fibrils of the corneal stroma where at least a portion of the N-terminal domain could be exposed on the fibril surface, whereas the triple-helical epitopes are masked by the fibril structure in which they are mostly buried (Linsenmayer et al. 1993; Birk 2001). There are several type V collagen isoforms which differ in their α chain composition (Fichard et al. 1995). The most common isoform is α1 (V)2 α2 (V) which is also found in the cornea (Birk et al. 1988; Gordon et al. 1994). The corneal stroma contains only one population of heterotypic collagen I/collagen V fibrils (Birk et al. 1988; Birk 2001).
Compared to other tissues, the cornea is relatively rich in type V collagen (15–20 % of total fibrillar collagens) where it plays a central role in the initiation of fibril assembly (Hassell and Birk 2010), more precisely in the regulation of collagen fibril diameter. In vitro fibrillar interaction studies between types I and V collagens that mimic in vivo interactions have shown that these interactions are largely responsible for controlling type I collagen fibril diameters (Adachi and Hayashi 1986; Birk et al. 1990) and that the type V collagen N-terminal domain is responsible for the “regulator” effects of this collagen on fibril diameter (Birk 2001). Reducing the amount of type V collagen increases fibril diameter. Marchant et al. (1996) have also demonstrated the involvement of type V collagen in the regulation of type I collagen fibril diameter using a dominant negative approach designed to reduce endogenous levels of type V collagen. The crucial role of type V collagen in regulating collagen fibril assembly was confirmed by inactivation of this gene in a mouse model (col5a1 conditional KO mice) where the corneal collagen diameter was increased and the fibril lamellae structure was disorganized which resulted in corneal opacification and therefore a loss of its function (Sun et al. 2011).
Type VII collagen
Type VII collagen, a homotrimer of α1 chains (Canty and Kadler 2005) is a major component of anchoring fibrils and plays an indispensable role in the epithelial–stromal adhesion. This molecule represents one of the most important BM components, as anchoring fibrils insert into the BM and then splay out laterally in the stroma (Gipson et al. 1987). Type VII collagen is also important during corneal wound healing as it is expressed in the adhesion structures alongside wound closure (Gipson et al. 1989). It seems to be involved in corneal diseases such as recurrent corneal erosion. This abnormality is characterized by repeated periods of breakdown of corneal epithelium caused by a dysfunction in adhesion to the BM and could be secondary to a CEBM dystrophy (Chen et al. 2006). The type VII collagen could also be implicated in other corneal abnormalities such as keratoconus (a corneal dystrophy characterized by a thinning and a curvature of the central cornea) where a decrease of its expression has been observed in the CEBM (Tuori et al. 1997).
Type VIII collagen
Type VIII is a non-fibrillar collagen which is considered to be the major protein of the mammalian DM. It consists of α1 (VIII) and α2 (VIII) chains which form two distinct homotrimeric or heterotrimeric proteins, although the formation of the α1 (2) α2 (VIII) and α1 α2 (2) (VIII) has been shown based on in vitro translation system (Illidge et al. 2001). The Descemet’s membrane, similar to other tissues, seems to contain the α1 (VIII) and α2 (VIII) chains that exist under two distinct homotrimeric molecules (Greenhill et al. 2000). The gene encoding the α2 (VIII) collagen chain seems to be implicated in various corneal endotheliopathies including Fuchs’ endothelial corneal dystrophy (FECD), one of the commonest indications for corneal transplantation where the principal defect is a reduction in the number of corneal endothelial cells (Igo et al. 2012). The implication of the α2 (VIII) collagen chain in FECD has been demonstrated by the generation of a transgenic knock-in mouse model that carries a genetic defect on the Col8a2. These mice show similar symptoms to human disease, including progressive alterations in endothelial cell morphology, cell death and excrescences (Jun et al. 2012). This gene seems also to be involved in posterior polymorphous corneal dystrophy (PPCD) (Merjava et al. 2009).
Type XII collagen
Several types of non fibrillar collagen are often associated with the surface of the collagen fibrils. Among them, the FACITs are characterized by the alternation in their structure of typical collagen triple-helical domains and non-collagen domains, the latter including known matrix protein motifs (Akimoto et al. 2002). These collagens are not able to form collagen fibrils by themselves. However, they can interact and associate laterally with collagen fibrils through their triple helical domains (van der Rest et al. 1990; Shaw and Olsen 1991; Walchli et al. 1994; Gerecke et al. 2003; Fig. 2a). FACITs are localized at the surface of collagen fibrils and could therefore induce changes in the interaction properties as well as the organization of fibrils through the interactions between their collagenous domains and fibrillar collagens (Nishiyama et al. 1994; Young et al. 2000, 2002; Tzortzaki et al. 2003).
There are several FACITs, collagens IX, XII, XIV and FACIT-like molecules, collagens XVI, XIX, XX, XXI, XXII, XXVI (Zwolanek et al. 2014). In this review, we focus on the type XII collagen, the FACIT that seems to be involved in corneal wound healing (Massoudi et al. 2012). Type XII collagen is a homotrimer of α1 chains (Canty and Kadler 2005). It contains collagenous domains (COL1 and COL2) and non-collagenous domains (NC1, NC2 and NC3; Fig. 2a). The COL1 and COL2 domains are localized at the carboxy-terminal end and are able to form a collagen triple helix as for the fibrillar collagens. The NC1 and NC2 domains do not have a particular protein structure. However, the NC3 domain, localized to the N-terminal end of the molecule, contains several peptide domains. These domains include von Willebrand factor A (vWA), fibronectin type III (FN-III) and thrombospondin (Tsp) repeats (Fig. 2a) (Yamagata, et al. 1991; Kania et al. 1999). This N-terminal end is relatively large and reveals itself to be a complex modular structure with a high potential for functional interactions (Yamagata et al. 1991; Walchli et al. 1994). Type XII collagen could help to stabilize fibril organization by forming interfibrillar bridges with other ECM components (Keene et al. 1991).
Currently, four isoforms of type XII collagen, generated by alternative splicing, have been described (Kania et al. 1999; Massoudi et al. 2012): two in the NC1 domain and two in the NC3 domain (Fig. 2a). These isoforms have distinct histological and developmental distributions: the isoforms that contain the long form of the NC3 [(XII-NC3-L/NC1-L and XII-NC3-L/NC1-S),] are mainly expressed during the early stages of the embryonic development whereas those with the short form of NC3 are predominant in adult tissues (Bohme et al. 1995). In addition, these isoforms also have different biochemical properties because of their structural difference. For instance, the long forms of the protein (XII-NC3-L/NC1-L and XIINC3-L/NC1-S) contain a supplementary heparin binding site in the 7th type III fibronectin motif in addition to the GAG chains that are covalently linked (Koch et al. 1992, 1995). Alternative splicing in the NC1 domain leads also to a supplementary heparin binding site for the isoforms XII-NC3-L/NC1-L and XII-NC3-C/NC1-L. Type XII collagen can also interact with matrix components such as decorin (Font et al. 1998) or tenascin X (Veit et al. 2006).
In the cornea, type XII collagen is expressed in epithelial BM, DM, and along stromal collagen fibrils (Anderson et al. 2000; Gordon et al. 1996; Kabosova et al. 2007; Oh et al. 1993; Wessel et al. 1997; Young et al. 2002). In human, the NC3 long isoform is the most abundant (Kabosova et al. 2007; Wessel et al. 1997), whereas in mouse both NC3 isoforms are present (Oh et al. 1993; Izu et al. 2011).
In 2012, we showed that type XII collagen could be involved in the formation and maintenance of the corneal scar (Massoudi et al. 2012). During this study, we demonstrated that the expression of type XII collagen increases after corneal injury and is largely concentrated in the subepithelial region of the cornea, especially in and near the wound bed. This high expression is observed throughout the corneal wound healing process. Most interestingly, the overexpression of type XII collagen was found to be localized in scars established for several months not only in human but also in mouse corneas, right in the injured area which was also positive for α-SMA. In the mouse cornea, the overexpression of type XII collagen seems to involve the NC1L isoform (Massoudi et al. 2012).
Type XVIII collagen
Type XVIII collagen belongs to the subgroup of non-fibrillar collagens and is a heparan sulfate proteoglycan (Ylikarppa et al. 2003). This collagen has three variants. The longer variants are found especially in the liver whereas the shortest one is found in most epithelial and endothelial BMs including corneal BMs (Maatta et al. 2006; Seppinen and Pihlajaniemi 2011). These variants are encoded by 2 different promoters. The short variant is encoded by promoter 1 and has its own signal sequence. The middle and long variants, however, are both encoded by promoter 2 and therefore have the same signal sequence (Fig. 2b; Seppinen and Pihlajaniemi 2011). Type XVIII collagen variants differ in their N-terminal regions but share several triple-helical regions separated by non-triple-helical domains in their C-terminal region. A domain in the C-terminal non-triple-helical region (NC1) of collagen XVIII, common to all variants, represents the anti-angiogenic molecule known as endostatin (Fig. 2b; Fukai et al. 2002). The anti-angiogenic activity of this 20-kDa proteolytic fragment of type XVIII collagen results in the inhibition of FGF-2- and VEGF-induced vascular endothelial cell adhesion, migration and proliferation as well as in the induction of apoptosis (Chang et al. 2001; Lai et al. 2007).
Angiogenesis plays an important role in many physiologic and pathologic processes. In the eye, it is implicated in several diseases including corneal disorders. The neovascularization of the cornea is often accompanied by inflammation or infections of the ocular surface which are usually associated with stromal edema, lipid deposits, keratitis or scarring that results in vision impairment and blindness. Consequently, corneal neovascularization is one of the most common causes of visual impairment and is also a high-risk factor for rejection of corneal allografts by facilitating the exposure of antigens in the donor cornea to the immune system. This process involves changes in vascular permeability, endothelial cell adhesion, migration, proliferation and differentiation (Lai et al. 2007; Ge, et al. 2013).
A variety of corneal injury models have implicated endostatin as an anti-angiogenic factor. For example, Lai et al. showed that the injection of recombinant adeno-associated viral vector carrying endostatin in mouse cornea was able to inhibit neovascularization after silver nitrate cauterization (Lai et al. 2007). Chen et al. (2010) used a similar approach to demonstrate the efficacy of endostatin in inhibiting mouse corneal neovascularization after alkaline burn injury (Chen et al. 2010). In addition, Murthy et al. (2003) showed that lentivirus overexpression of endostatin in rabbit allogenic corneal grafts not only inhibits corneal neovascularization but also prevents graft rejection.
Type XVIII collagen is also involved in other corneal pathologies. For example, in human, the rare autosomal recessive disorder Knobloch syndrome, which causes several eye abnormalities including high myopia, is induced by mutations in the gene that encodes the α1 (XVIII) chain. These mutations affect either the short or all type XVIII collagen isoforms (Ylikarppa et al. 2003; Maatta et al. 2006).
Proteoglycans in the correct functioning of the cornea
In addition to the FACITs, other molecules such as SLRPs play an important role in the structural and functional modifications of collagen fibrils (Michelacci 2003). Currently, the SLRP family includes 17 genes that encode proteoglycans assembled into five distinct classes based on common structure and function. Class I SLRPs include decorin and biglycan. These two proteoglycans share approximately 60 % homology (Iozzo et al. 1999). Class I also includes asporin and ECM protein 2. Class II contains five polyanionic members: fibromodulin, lumican, proline/arginine-rich end leucine-rich repeat protein or PRELP, keratocan and osteoadherin. Class III consists of three members: epiphycan, opticin and osteoglycan. Both Class IV and Class V are non-canonical, the former consisting of three members (chondroadherin, nyctalopin, and tsukushi) and the latter consisting of two members (podocan and the highly homologous podocan-like protein 1) (Mohan et al. 2011).
All classes of the SLRP family share a common basic structure composed of a protein core covalently bound to one or more glycoaminoglycan (GAG) chain(s) (Iozzo 1998). Protein cores have molecular weights between 20 and 450 kDa. The GAG chains are made up of disaccharide repeats with sulfated esters and can reach molecular weights of up to 70 kDa. There are three types of GAG chains: chondroitin/dermatan sulfate (CS/DS), keratan sulfate (KS) and heparan sulfate (HS) (Hassell and Birk 2010). Consequently, SLRPs have also been classified according to their GAG chain composition into chondroitin/dermatan sulfate, keratan sulfate and heparan sulfate macromolecules (Tanihara et al. 2002).
SLRP protein cores are synthesized in the rough endoplasmic reticulum (RER) and the GAG chains are added to the protein core in the Golgi apparatus. These proteoglycans are then secreted into the ECM (Hassell and Birk 2010).
SLRP studies carried out on bovine (Axelsson and Heinegard 1978), rabbit (Gregory et al. 1982), chicken (Funderburgh et al. 1986), monkey (Hassell et al. 1979) and human (Soriano, et al. 2000) have shown that dermatan sulfate and keratan sulfate constitute the predominant proteoglycans in the corneal structure (Michelacci 2003). Among the wide diversity of proteoglycans, the human adult corneal stroma consists of four leucine-rich variants, including one dermatan sulfate proteoglycan, decorin (Li et al. 1992) and three keratan sulfate proteoglycans: lumican (Blochberger et al. 1992; Kao et al. 2006), keratocan (Corpuz et al. 1996; Chakravarti 2006) and mimecan (Funderburgh et al. 1997), a gene product that was previously named proteoglycan-LB (Shinomura and Kimata 1992) and osteoglycin (Madisen et al. 1990). Heparan sulfate proteoglycans are also minor components of the cornea and are mainly synthesized by the corneal epithelial cells (Michelacci 2003).
Corneal proteoglycans appear to play important roles in collagen fibrillogenesis and matrix assembly. Morphological studies have shown the association of dermatan and keratan sulfate proteoglycans with specific groups of corneal collagen fibrils (Scott and Haigh 1985, 1988), suggesting that proteoglycan–collagen interactions may play a role in the assembly of corneal collagen fibrils, in matrix organization, and therefore in corneal transparency.
Several studies have shown that the synthesis of defective SLRPs causes blindness in humans by disruption of the organization of the collagen fibers. For example, in human, it has been reported that mutations in the decorin gene are associated with congenital stromal dystrophy, a disease that appears a short time after birth and leads to corneal opacity and visual abnormalities (Bredrup et al. 2005; Rodahl et al. 2006). These mutations lead to a synthesis of a decorin protein core truncated by 33 amino acids in the C-terminal region. This disease is autosomal dominant and only patients heterozygous for these mutations are alive and carry the mutations, suggesting that the homozygous are not viable and therefore embryonic lethal (Chen and Birk 2011).
Production of defective keratan sulfate proteoglycans in human has been shown to be the cause of hereditary corneal dystrophies. For example, it has been shown that mutations in the human KERA, the gene that encodes the keratocan protein core, are associated with cornea plana (CNA2), which is a congenital, bilateral and asymmetrical defect, characterized by a decrease in the curvature of the cornea that leads to a decrease in the refractive index (Pellegata et al. 2000) that goes along with a decrease in visual acuity (Liu et al. 2003).
In addition, human mutations in the carbohydrate sulfotransferase 6 gene (CHST6), which encodes one of the sulfotransferases responsible for the transfer of sulfate esters onto the keratan sulfate, cause a macular corneal dystrophy which is an autosomal recessive disorder (Hassell et al. 1980; Midura et al. 1990; Hayashida et al. 2006; Musselmann and Hassell 2006; Di Iorio et al. 2010).
Several studies have also implicated SLRPs in collagen fibril regulation. For example, the crucial role of decorin and lumican in the regulation of the growth and assembly of collagen fibrils was highlighted by inactivation of those genes in mice (Hassell and Birk 2010). Mice deficient in decorin expression have fragile skin and dysregulated lateral growth of fibrils (Chen and Birk 2011). Animals homozygous for a null mutation in the lumican gene present a laxity accompanied by skin fragility and bilaterally corneal opacity (Chakravarti et al. 1998; Michelacci 2003). Decorin and lumican protein cores, but not their GAG chains, have been shown to inhibit the formation of collagen fibrils and reduce their diameter during an in vitro test of collagen fibril formation (Rada et al. 1993). Decorin and lumican yield recombinant products that act at different stages of fibrillar growth, interact with the different regions of the collagen molecule and serve to stabilize the collagen fibrils once formed (Neame et al. 2000).
Keratocan knockout mice also display alterations in corneal structure. In fact, the mice lacking keratocan show corneal stromal thinning accompanied by large collagen fibril diameters and a poor spacing of the collagen fibrils in the corneal stroma (Liu et al. 2003; Meek et al. 2003). Also, mimecan deficiency in mice induces a thickening of collagen fibrils in tissues including cornea and skin (Tasheva et al. 2002).
The importance of the SLRP sulfation has also been demonstrated in animal models. SLRPs with unsulfated keratan sulfate chains were detected as early as 7 days of chicken embryonic development, whereas sulfated GAG chains were not detectable before the 15th day of embryonic development, when the corneal transparency starts to appear (Dunlevy et al. 2000). Also in the mouse embryo, keratan sulfate proteoglycans appear only after eye opening and therefore may contribute to corneal transparency (Ying et al. 1997). The presence of the sulfate group in the sulfate chains of the SLRPs is essential for proteoglycan function. In fact, the sulfate groups of the proteoglycan GAG chains bind water. At the normal hydration levels of the cornea, chondroitin/dermatan sulfate chains are perfectly hydrated while the keratan sulfate chains are not, suggesting that the keratan sulfate acts as a reservoir for hydration (Bettelheim and Plessy 1975). The sulfated esters in the keratan sulfate are also important for maintaining the solubility of the proteoglycan in an aqueous environment (Funderburgh 2000). These data suggest that the structure of GAG chains in keratan sulfate proteoglycans may be important for the development of corneal transparency, possibly leading to an organization and an optimal hydration of the corneal tissue (Michelacci 2003).
Concluding remarks
Different newly synthesized fibrillar collagen molecules can be associated with each other and with other proteins, such as proteoglycans and FACITs, to form a supramolecular entity with the collagen fibril (Fig. 3). This shows how several types of collagen can be present within the same fibril and how the proportions of these different types of collagen in the fibril is at the origin of its specific biomechanical properties (Kietly and Grant 2002). This may explain why the disruption of these proportions leads to a dysfunction or to a malformation of the considered tissue/organ. However, the formation of the collagen fibril is not just a simple “collagen molecule condensation”; the process of fibril arrangement is relatively complex. For example, the diameter of the fibril is accurately controlled by proteoglycans such as decorin or by non-fibrillar collagens such as type XII collagen that surround the collagen fibril (Fig. 3). These fibrils will interact with each other and with other molecules to constitute the connective tissue network which will be specific to the considered tissue/organ. Nevertheless, these mechanisms are not fully clarified as some aspects of fibrilogenesis still remain to be determined, as well as the mechanism of fibril arrangement for the different types of collagen molecules and the control of their respective proportions.
References
Adachi E, Hayashi T (1986) In vitro formation of hybrid fibrils of type V collagen and type I collagen. Limited growth of type I collagen into thick fibrils by type V collagen. Connect Tissue Res 14:257–266
Akhtar S, Kerr BC, Hayes AJ, Hughes CE, Meek KM, Caterson B (2008) Immunochemical localization of keratan sulfate proteoglycans in cornea, sclera, and limbus using a keratanase-generated neoepitope monoclonal antibody. Invest Ophthalmol Vis Sci 49:2424–2431
Akimoto Y, Yamakawa N, Furukawa K, Kimata K, Kawakami H, Hirano H (2002) Changes in distribution of the long form of type XII collagen during chicken corneal development. J Histochem Cytochem 50:851–862
Alberto D, Garello R (2013) Corneal sublayers thickness estimation obtained by high-resolution FD-OCT. Int J Biomed Imaging 2013:989624
Anderson S, SundarRaj S, Fite D, Wessel H, SundarRaj N (2000) Developmentally regulated appearance of spliced variants of type XII collagen in the cornea. Invest Ophthalmol Vis Sci 41:55–63
Axelsson I, Heinegard D (1978) Characterization of the keratan sulphate proteoglycans from bovine corneal stroma. Biochem J 169:517–530
Bateman JF, Chan D, Mascara T, Rogers JG, Cole WG (1986) Collagen defects in lethal perinatal osteogenesis imperfecta. Biochem J 240:699–708
Bettelheim FA, Plessy B (1975) The hydration of proteoglycans of bovine cornea. Biochim Biophys Acta 381:203–214
Birk DE (2001) Type V collagen: heterotypic type I/V collagen interactions in the regulation of fibril assembly. Micron 32:223–237
Birk DE, Fitch JM, Babiarz JP, Linsenmayer TF (1988) Collagen type I and type V are present in the same fibril in the avian corneal stroma. J Cell Biol 106:999–1008
Birk DE, Fitch JM, Babiarz JP, Doane KJ, Linsenmayer TF (1990) Collagen fibrillogenesis in vitro: interaction of types I and V collagen regulates fibril diameter. J Cell Sci 95(Pt 4):649–657
Blochberger TC, Vergnes JP, Hempel J, Hassell JR (1992) cDNA to chick lumican (corneal keratan sulfate proteoglycan) reveals homology to the small interstitial proteoglycan gene family and expression in muscle and intestine. J Biol Chem 267:347–352
Bohme K, Li Y, Oh PS, Olsen BR (1995) Primary structure of the long and short splice variants of mouse collagen XII and their tissue-specific expression during embryonic development. Dev Dyn 204:432–445
Bonanno JA (2003) Identity and regulation of ion transport mechanisms in the corneal endothelium. Prog Retin Eye Res 22:69–94
Borel JP, Bellon G (1985) Vascular collagens. General review. Pathol Biol (Paris) 33:254–260
Bredrup C, Knappskog PM, Majewski J, Rodahl E, Boman H (2005) Congenital stromal dystrophy of the cornea caused by a mutation in the decorin gene. Invest Ophthalmol Vis Sci 46:420–426
Cameron GJ, Alberts IL, Laing JH, Wess TJ (2002) Structure of type I and type III heterotypic collagen fibrils: an X-ray diffraction study. J Struct Biol 137:15–22
Canty EG, Kadler KE (2005) Procollagen trafficking, processing and fibrillogenesis. J Cell Sci 118:1341–1353
Chakravarti S (2006) Focus on molecules: keratocan (KERA). Exp Eye Res 82:183–184
Chakravarti S, Magnuson T, Lass JH, Jepsen KJ, LaMantia C, Carroll H (1998) Lumican regulates collagen fibril assembly: skin fragility and corneal opacity in the absence of lumican. J Cell Biol 141:1277–1286
Chang JH, Gabison EE, Kato T, Azar DT (2001) Corneal neovascularization. Curr Opin Ophthalmol 12:242–249
Chen S, Birk DE (2011) Focus on molecules: decorin. Exp Eye Res 92:444–445
Chen S, Birk DE (2013) The regulatory roles of small leucine-rich proteoglycans in extracellular matrix assembly. FEBS J 280:2120–2137
Chen L, Kato T, Toshida H, Nakamura S, Murakami A (2005) Immunohistochemical characterization of epithelial cells implanted in the flap-stroma interface of the cornea. Jpn J Ophthalmol 49:79–83
Chen YT, Huang CW, Huang FC, Tseng SY, Tseng SH (2006) The cleavage plane of corneal epithelial adhesion complex in traumatic recurrent corneal erosion. Mol Vis 12:196–204
Chen P, Yin H, Wang Y, Mi J, He W, Xie L, Wang Y (2010) Multi-gene targeted antiangiogenic therapies for experimental corneal neovascularization. Mol Vis 16:310–319
Cintron C, Kublin CL (1977) Regeneration of corneal tissue. Dev Biol 61:346–357
Cintron C, Hassinger LC, Kublin CL, Cannon DJ (1978) Biochemical and ultrastructural changes in collagen during corneal wound healing. J Ultrastruct Res 65:13–22
Corpuz LM, Funderburgh JL, Funderburgh ML, Bottomley GS, Prakash S, Conrad GW (1996) Molecular cloning and tissue distribution of keratocan. Bovine corneal keratan sulfate proteoglycan 37A. J Biol Chem 271:9759–9763
Dawson DG, Kramer TR, Grossniklaus HE, Waring GO 3rd, Edelhauser HF (2005) Histologic, ultrastructural, and immunofluorescent evaluation of human laser-assisted in situ keratomileusis corneal wounds. Arch Ophthalmol 123:741–756
Del Pero RA, Gigstad JE, Roberts AD, Klintworth GK, Martin CA, L’Esperance FA Jr, Taylor DM (1990) A refractive and histopathologic study of excimer laser keratectomy in primates. Am J Ophthalmol 109:419–429
Di Iorio E, Barbaro V, Volpi N, Bertolin M, Ferrari B, Fasolo A, Arnaldi R, Brusini P, Prosdocimo G, Ponzin D, Ferrari S (2010) Localization and expression of CHST6 and keratan sulfate proteoglycans in the human cornea. Exp Eye Res 91:293–299
Dunlevy JR, Beales MP, Berryhill BL, Cornuet PK, Hassell JR (2000) Expression of the keratan sulfate proteoglycans lumican, keratocan and osteoglycin/mimecan during chick corneal development. Exp Eye Res 70:349–362
Ebihara N, Mizushima H, Miyazaki K, Watanabe Y, Ikawa S, Nakayasu K, Kanai A (2000) The functions of exogenous and endogenous laminin-5 on corneal epithelial cells. Exp Eye Res 71:69–79
Esipov R, Beyrakhova K, Likhvantseva V, Stepanova E, Stepanenko V, Kostromina M, Abramchik Y, Miroshnikov A (2012) Antiangiogenic and antivascular effects of a recombinant tumstatin-derived peptide in a corneal neovascularization model. Biochimie 94:1368–1375
Fichard A, Kleman JP, Ruggiero F (1995) Another look at collagen V and XI molecules. Matrix Biol 14:515–531
Font B, Eichenberger D, Goldschmidt D, Boutillon MM, Hulmes DJ (1998) Structural requirements for fibromodulin binding to collagen and the control of type I collagen fibrillogenesis–critical roles for disulphide bonding and the C-terminal region. Eur J Biochem 254:580–587
Fournié P, Gordon GM, Ledee DR, Roberts CJ, Fini ME (2008) Corneal stroma: shape, structure and biomechanical properties. In: Brightbill FS, McDonnell PJ, McGhee CNJ, Farjo AA, Serdarevic O (eds) Corneal surgery: theory, technique and tissue (4th edn). Elsevier, New York, pp 33–44
Fukai N, Eklund L, Marneros AG, Oh SP, Keene DR, Tamarkin L, Niemela M, Ilves M, Li E, Pihlajaniemi T, Olsen BR (2002) Lack of collagen XVIII/endostatin results in eye abnormalities. EMBO J 21:1535–1544
Funderburgh JL (2000) Keratan sulfate: structure, biosynthesis, and function. Glycobiology 10:951–958
Funderburgh JL, Caterson B, Conrad GW (1986) Keratan sulfate proteoglycan during embryonic development of the chicken cornea. Dev Biol 116:267–277
Funderburgh JL, Corpuz LM, Roth MR, Funderburgh ML, Tasheva ES, Conrad GW (1997) Mimecan, the 25-kDa corneal keratan sulfate proteoglycan, is a product of the gene producing osteoglycin. J Biol Chem 272:28089–28095
Funderburgh JL, Hevelone ND, Roth MR, Funderburgh ML, Rodrigues MR, Nirankari VS, Conrad GW (1998) Decorin and biglycan of normal and pathologic human corneas. Invest Ophthalmol Vis Sci 39:1957–1964
Galiacy SD, Fournie P, Massoudi D, Ancele E, Quintyn JC, Erraud A, Raymond-Letron I, Rolling F, Malecaze F (2011) Matrix metalloproteinase 14 overexpression reduces corneal scarring. Gene Ther 18:462–468
Ge H, Tian P, Guan L, Yin X, Liu H, Xiao N, Xiong Y, Luo X, Sun Y, Qi D, Ni S, Liu P (2013) A C-terminal fragment BIGH3 protein with an RGDRGD motif inhibits corneal neovascularization in vitro and in vivo. Exp Eye Res 112:10–20
Gelse K, Poschl E, Aigner T (2003) Collagens–structure, function, and biosynthesis. Adv Drug Deliv Rev 55:1531–1546
Gerecke DR, Meng X, Liu B, Birk DE (2003) Complete primary structure and genomic organization of the mouse Col14a1 gene. Matrix Biol 22:209–216
Gipson IK, Spurr-Michaud SJ, Tisdale AS (1987) Anchoring fibrils form a complex network in human and rabbit cornea. Invest Ophthalmol Vis Sci 28:212–220
Gipson IK, Spurr-Michaud S, Tisdale A, Keough M (1989) Reassembly of the anchoring structures of the corneal epithelium during wound repair in the rabbit. Invest Ophthalmol Vis Sci 30:425–434
Gordon MK, Hahn RA (2010) Collagens. Cell Tissue Res 339:247–257
Gordon MK, Foley JW, Birk DE, Fitch JM, Linsenmayer TF (1994) Type V collagen and Bowman’s membrane quantitation of mRNA in corneal epithelium and stroma. J Biol Chem 269:24959–24966
Gordon MK, Foley JW, Lisenmayer TF, Fitch JM (1996) Temporal expression of types XII and XIV collagen mRNA and protein during avian corneal development. Dev Dyn 206:49–58
Gould DB, Marchant JK, Savinova OV, Smith RS, John SW (2007) Col4a1 mutation causes endoplasmic reticulum stress and genetically modifiable ocular dysgenesis. Hum Mol Genet 16:798–807
Greenhill NS, Ruger BM, Hasan Q, Davis PF (2000) The alpha1(VIII) and alpha2(VIII) collagen chains form two distinct homotrimeric proteins in vivo. Matrix Biol 19:19–28
Gregory JD, Coster L, Damle SP (1982) Proteoglycans of rabbit corneal stroma Isolation and partial characterization. J Biol Chem 257:6965–6970
Han S, Makareeva E, Kuznetsova NV, DeRidder AM, Sutter MB, Losert W, Phillips CL, Visse R, Nagase H, Leikin S (2010) Molecular mechanism of type I collagen homotrimer resistance to mammalian collagenases. J Biol Chem 285:22276–22281
Hanna KD, Pouliquen Y, Waring GO 3rd, Savoldelli M, Cotter J, Morton K, Menasche M (1989) Corneal stromal wound healing in rabbits after 193-nm excimer laser surface ablation. Arch Ophthalmol 107:895–901
Hassell JR, Birk DE (2010) The molecular basis of corneal transparency. Exp Eye Res 91:326–335
Hassell JR, Newsome DA, Hascall VC (1979) Characterization and biosynthesis of proteoglycans of corneal stroma from rhesus monkey. J Biol Chem 254:12346–12354
Hassell JR, Newsome DA, Krachmer JH, Rodrigues MM (1980) Macular corneal dystrophy: failure to synthesize a mature keratan sulfate proteoglycan. Proc Natl Acad Sci U S A 77:3705–3709
Hassell JR, Cintron C, Kublin C, Newsome DA (1983) Proteoglycan changes during restoration of transparency in corneal scars. Arch Biochem Biophys 222:362–369
Hatami-Marbini H, Etebu E (2013) Hydration dependent biomechanical properties of the corneal stroma. Exp Eye Res 116:47–54
Hayashida Y, Akama TO, Beecher N, Lewis P, Young RD, Meek KM, Kerr B, Hughes CE, Caterson B, Tanigami A, Nakayama J, Fukada MN, Tano Y, Nishida K, Quantock AJ (2006) Matrix morphogenesis in cornea is mediated by the modification of keratan sulfate by GlcNAc 6-O-sulfotransferase. Proc Natl Acad Sci U S A 103:13333–13338
Helena MC, Baerveldt F, Kim WJ, Wilson SE (1998) Keratocyte apoptosis after corneal surgery. Invest Ophthalmol Vis Sci 39:276–283
Igo RP Jr, Kopplin LJ, Joseph P, Truitt B, Fondran J, Bardenstein D, Aldave AJ, Croasdale CR, Price MO, Rosenwasser M, Lass JH, Iyengar SK (2012) Differing roles for TCF4 and COL8A2 in central corneal thickness and fuchs endothelial corneal dystrophy. PLoS ONE 7, e46742
Illidge C, Kielty C, Shuttleworth A (2001) Type VIII collagen: heterotrimeric chain association. Int J Biochem Cell Biol 33:521–529
Iozzo RV (1998) Matrix proteoglycans: from molecular design to cellular function. Annu Rev Biochem 67:609–652
Iozzo RV, Moscatello DK, McQuillan DJ, Eichstetter I (1999) Decorin is a biological ligand for the epidermal growth factor receptor. J Biol Chem 274:4489–4492
Izu Y, Sun M, Zwolanek D, Veit G, Williams V, Cha B, Jepsen KJ, Koch M, Birk DE (2011) Type XII collagen regulates osteoblast polarity and communication during bone formation. J Cell Biol 193:1115–1130
Jester JV, Petroll WM, Barry PA, Cavanagh HD (1995) Expression of alpha-smooth muscle (alpha-SM) actin during corneal stromal wound healing. Invest Ophthalmol Vis Sci 36:809–819
Jun AS, Meng H, Ramanan N, Matthaei M, Chakravarti S, Bonshek R, Black GC, Grebe R, Kimos M (2012) An alpha 2 collagen VIII transgenic knock-in mouse model of Fuchs endothelial corneal dystrophy shows early endothelial cell unfolded protein response and apoptosis. Hum Mol Genet 21:384–393
Kabosova A, Azar DT, Bannikov GA, Campbell KP, Durbeej M, Ghohestani RF, Jones JC, Kenney MC, Koch M, Ninomiya Y, Patton BL, Paulsson M, Sado Y, Sage EH, Sasaki T, Sorokin LM, Steiner-Champliaud MF, Sun TT, Sundarraj N, Timpl R, Virtanen I, Ljubimov AV (2007) Compositional differences between infant and adult human corneal basement membranes. Invest Ophthalmol Vis Sci 48:4989–4999
Kania AM, Reichenberger E, Baur ST, Karimbux NY, Taylor RW, Olsen BR, Nishimura I (1999) Structural variation of type XII collagen at its carboxyl-terminal NC1 domain generated by tissue-specific alternative splicing. J Biol Chem 274:22053–22059
Kao WW, Funderburgh JL, Xia Y, Liu CY, Conrad GW (2006) Focus on molecules: lumican. Exp Eye Res 82:3–4
Keene DR, Lunstrum GP, Morris NP, Stoddard DW, Burgeson RE (1991) Two type XII-like collagens localize to the surface of banded collagen fibrils. J Cell Biol 113:971–978
Kietly CM, Grant ME (2002) The collagen family: structure, assembly, and organization of the extracellular matrix. In: Royce PM, Steinmann B (eds) Connective tissue and its heritable disorders. Wiley, New York, pp 159–221
Knupp C, Pinali C, Lewis PN, Parfitt GJ, Young RD, Meek KM, Quantock AJ (2009) The architecture of the cornea and structural basis of its transparency. Adv Protein Chem Struct Biol 78:25–49
Koch M, Bernasconi C, Chiquet M (1992) A major oligomeric fibroblast proteoglycan identified as a novel large form of type-XII collagen. Eur J Biochem 207:847–856
Koch M, Bohrmann B, Matthison M, Hagios C, Trueb B, Chiquet M (1995) Large and small splice variants of collagen XII: differential expression and ligand binding. J Cell Biol 130:1005–1014
Lai LJ, Xiao X, Wu JH (2007) Inhibition of corneal neovascularization with endostatin delivered by adeno-associated viral (AAV) vector in a mouse corneal injury model. J Biomed Sci 14:313–322
Li W, Vergnes JP, Cornuet PK, Hassell JR (1992) cDNA clone to chick corneal chondroitin/dermatan sulfate proteoglycan reveals identity to decorin. Arch Biochem Biophys 296:190–197
Linsenmayer TF, Fitch JM, Schmid TM, Zak NB, Gibney E, Sanderson RD, Mayne R (1983) Monoclonal antibodies against chicken type V collagen: production, specificity, and use for immunocytochemical localization in embryonic cornea and other organs. J Cell Biol 96:124–132
Linsenmayer TF, Gibney E, Igoe F, Gordon MK, Fitch JM, Fessler LI, Birk DE (1993) Type V collagen: molecular structure and fibrillar organization of the chicken alpha 1(V) NH2-terminal domain, a putative regulator of corneal fibrillogenesis. J Cell Biol 121:1181–1189
Liu CY, Birk DE, Hassell JR, Kane B, Kao WW (2003) Keratocan-deficient mice display alterations in corneal structure. J Biol Chem 278:21672–21677
Ljubimov AV, Burgeson RE, Butkowski RJ, Michael AF, Sun TT, Kenney MC (1995) Human corneal basement membrane heterogeneity: topographical differences in the expression of type IV collagen and laminin isoforms. Lab Invest 72:461–473
Ljubimov AV, Alba SA, Burgeson RE, Ninomiya Y, Sado Y, Sun TT, Nesburn AB, Kenney MC, Maguen E (1998) Extracellular matrix changes in human corneas after radial keratotomy. Exp Eye Res 67:265–272
Maatta M, Heljasvaara R, Sormunen R, Pihlajaniemi T, Autio-Harmainen H, Tervo T (2006) Differential expression of collagen types XVIII/endostatin and XV in normal, keratoconus, and scarred human corneas. Cornea 25:341–349
Madisen L, Neubauer M, Plowman G, Rosen D, Segarini P, Dasch J, Thompson A, Ziman J, Bentz H, Purchio AF (1990) Molecular cloning of a novel bone-forming compound: osteoinductive factor. DNA Cell Biol 9:303–309
Maguen E, Alba SA, Burgeson RE, Butkowski RJ, Michael AF, Kenney MC, Nesburn AB, Ljubimov AV (1997) Alterations of corneal extracellular matrix after multiple refractive procedures: a clinical and immunohistochemical study. Cornea 16:675–682
Marchant JK, Hahn RA, Linsenmayer TF, Birk DE (1996) Reduction of type V collagen using a dominant-negative strategy alters the regulation of fibrillogenesis and results in the loss of corneal-specific fibril morphology. J Cell Biol 135:1415–1426
Massoudi D, Malecaze F, Soler V, Butterworth J, Erraud A, Fournie P, Koch M, Galiacy SD (2012) NC1 long and NC3 short splice variants of type XII collagen are overexpressed during corneal scarring. Invest Ophthalmol Vis Sci 53:7246–7256
Meek KM, Quantock AJ, Boote C, Liu CY, Kao WW (2003) An X-ray scattering investigation of corneal structure in keratocan-deficient mice. Matrix Biol 22:467–475
Merjava S, Liskova P, Sado Y, Davis PF, Greenhill NS, Jirsova K (2009) Changes in the localization of collagens IV and VIII in corneas obtained from patients with posterior polymorphous corneal dystrophy. Exp Eye Res 88:945–952
Michelacci YM (2003) Collagens and proteoglycans of the corneal extracellular matrix. Braz J Med Biol Res 36:1037–1046
Midura RJ, Hascall VC, MacCallum DK, Meyer RF, Thonar EJ, Hassell JR, Smith CF, Klintworth GK (1990) Proteoglycan biosynthesis by human corneas from patients with types 1 and 2 macular corneal dystrophy. J Biol Chem 265:15947–15955
Mohan RR, Tovey JC, Gupta R, Sharma A, Tandon A (2011) Decorin biology, expression, function and therapy in the cornea. Curr Mol Med 11:110–128
Murthy RC, McFarland TJ, Yoken J, Chen S, Barone C, Burke D, Zhang Y, Appukuttan B, Stout JT (2003) Corneal transduction to inhibit angiogenesis and graft failure. Invest Ophthalmol Vis Sci 44:1837–1842
Musselmann K, Hassell JR (2006) Focus on molecules: CHST6 (carbohydrate sulfotransferase 6; corneal N-acetylglucosamine-6-sulfotransferase). Exp Eye Res 83:707–708
Neame PJ, Kay CJ, McQuillan DJ, Beales MP, Hassell JR (2000) Independent modulation of collagen fibrillogenesis by decorin and lumican. Cell Mol Life Sci 57:859–863
Nishiyama T, McDonough AM, Bruns RR, Burgeson RE (1994) Type XII and XIV collagens mediate interactions between banded collagen fibers in vitro and may modulate extracellular matrix deformability. J Biol Chem 269:28193–28199
Noske W, Fromm M, Levarlet B, Kreusel KM, Hirsch M (1994) Tight junctions of the human corneal endothelium: morphological and electrophysiological features. Ger J Ophthalmol 3:253–257
Oh SP, Griffith CM, Hay ED, Olsen BR (1993) Tissue-specific expression of type XII collagen during mouse embryonic development. Dev Dyn 196:37–46
Pellegata NS, Dieguez-Lucena JL, Joensuu T, Lau S, Montgomery KT, Krahe R, Kivela T, Kucherlapati R, Forsius H, de la Chapelle A (2000) Mutations in KERA, encoding keratocan, cause cornea plana. Nat Genet 25:91–95
Poschl E, Schlotzer-Schrehardt U, Brachvogel B, Saito K, Ninomiya Y, Mayer U (2004) Collagen IV is essential for basement membrane stability but dispensable for initiation of its assembly during early development. Development 131:1619–1628
Rada JA, Cornuet PK, Hassell JR (1993) Regulation of corneal collagen fibrillogenesis in vitro by corneal proteoglycan (lumican and decorin) core proteins. Exp Eye Res 56:635–648
Rodahl E, Van Ginderdeuren R, Knappskog PM, Bredrup C, Boman H (2006) A second decorin frame shift mutation in a family with congenital stromal corneal dystrophy. Am J Ophthalmol 142:520–521
Rodahl E, Knappskog PM, Majewski J, Johansson S, Telstad W, Krakenes J, Boman H (2013) Variants of anterior segment dysgenesis and cerebral involvement in a large family with a novel COL4A1 mutation. Am J Ophthalmol 155:946–953
Saika S, Ooshima A, Shima K, Tanaka S, Ohnishi Y (1996) Collagen types in healing alkali-burned corneal stroma in rabbits. Jpn J Ophthalmol 40:303–309
Scott JE, Haigh M (1985) ‘Small’-proteoglycan:collagen interactions: keratan sulphate proteoglycan associates with rabbit corneal collagen fibrils at the ‘a’ and ‘c’ bands. Biosci Rep 5:765–774
Scott JE, Haigh M (1988) Identification of specific binding sites for keratan sulphate proteoglycans and chondroitin-dermatan sulphate proteoglycans on collagen fibrils in cornea by the use of cupromeronic blue in ‘critical-electrolyte-concentration’ techniques. Biochem J 253:607–610
Seppinen L, Pihlajaniemi T (2011) The multiple functions of collagen XVIII in development and disease. Matrix Biol 30:83–92
Shaw LM, Olsen BR (1991) FACIT collagens: diverse molecular bridges in extracellular matrices. Trends Biochem Sci 16:191–194
Shinomura T, Kimata K (1992) Proteoglycan-Lb, a small dermatan sulfate proteoglycan expressed in embryonic chick epiphyseal cartilage, is structurally related to osteoinductive factor. J Biol Chem 267:1265–1270
Smith LT, Holbrook KA, Madri JA (1986) Collagen types I, III, and V in human embryonic and fetal skin. Am J Anat 175:507–521
Soriano ES, Campos MS, Michelacci YM (2000) Effect of epithelial debridement on glycosaminoglycan synthesis by human corneal explants. Clin Chim Acta 295:41–62
Sun M, Chen S, Adams SM, Florer JB, Liu H, Kao WW, Wenstrup RJ, Birk DE (2011) Collagen V is a dominant regulator of collagen fibrillogenesis: dysfunctional regulation of structure and function in a corneal-stroma-specific Col5a1-null mouse model. J Cell Sci 124:4096–4105
Sundarraj N, Fite D, Belak R, Sundarraj S, Rada J, Okamoto S, Hassell J (1998) Proteoglycan distribution during healing of corneal stromal wounds in chick. Exp Eye Res 67:433–442
Tanihara H, Inatani M, Koga T, Yano T, Kimura A (2002) Proteoglycans in the eye. Cornea 21:S62–S69
Tasheva ES, Koester A, Paulsen AQ, Garrett AS, Boyle DL, Davidson HJ, Song M, Fox N, Conrad GW (2002) Mimecan/osteoglycin-deficient mice have collagen fibril abnormalities. Mol Vis 8:407–415
Tuori AJ, Virtanen I, Aine E, Kalluri R, Miner JH, Uusitalo HM (1997) The immunohistochemical composition of corneal basement membrane in keratoconus. Curr Eye Res 16:792–801
Tzortzaki EG, Tischfield JA, Sahota A, Siafakas NM, Gordon MK, Gerecke DR (2003) Expression of FACIT collagens XII and XIV during bleomycin-induced pulmonary fibrosis in mice. Anat Rec A 275:1073–1080
Van Agtmael T, Schlotzer-Schrehardt U, McKie L, Brownstein DG, Lee AW, Cross SH, Sado Y, Mullins JJ, Poschl E, Jackson IJ (2005) Dominant mutations of Col4a1 result in basement membrane defects which lead to anterior segment dysgenesis and glomerulopathy. Hum Mol Genet 14:3161–3168
van der Rest M, Dublet B, Champliaud MF (1990) Fibril-associated collagens. Biomaterials 11:28–31
Veit G, Hansen U, Keene DR, Bruckner P, Chiquet-Ehrismann R, Chiquet M, Koch M (2006) Collagen XII interacts with avian tenascin-X through its NC3 domain. J Biol Chem 281:27461–27470
Walchli C, Koch M, Chiquet M, Odermatt BF, Trueb B (1994) Tissue-specific expression of the fibril-associated collagens XII and XIV. J Cell Sci 107(Pt 2):669–681
Wessel H, Anderson S, Fite D, Halvas E, Hempel J, SundarRaj N (1997) Type XII collagen contributes to diversities in human corneal and limbal extracellular matrices. Invest Ophthalmol Vis Sci 38:2408–2422
Wilson SE, Kim WJ (1998) Keratocyte apoptosis: implications on corneal wound healing, tissue organization, and disease. Invest Ophthalmol Vis Sci 39:220–226
Wilson SE, He YG, Weng J, Li Q, McDowall AW, Vital M, Chwang EL (1996) Epithelial injury induces keratocyte apoptosis: hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Exp Eye Res 62:325–327
Yamagata M, Yamada KM, Yamada SS, Shinomura T, Tanaka H, Nishida Y, Obara M, Kimata K (1991) The complete primary structure of type XII collagen shows a chimeric molecule with reiterated fibronectin type III motifs, von Willebrand factor A motifs, a domain homologous to a noncollagenous region of type IX collagen, and short collagenous domains with an Arg-Gly-Asp site. J Cell Biol 115:209–221
Ying S, Shiraishi A, Kao CW, Converse RL, Funderburgh JL, Swiergiel J, Roth MR, Conrad GW, Kao WW (1997) Characterization and expression of the mouse lumican gene. J Biol Chem 272:30306–30313
Ylikarppa R, Eklund L, Sormunen R, Kontiola AI, Utriainen A, Maatta M, Fukai N, Olsen BR, Pihlajaniemi T (2003) Lack of type XVIII collagen results in anterior ocular defects. FASEB J 17:2257–2259
Young BB, Gordon MK, Birk DE (2000) Expression of type XIV collagen in developing chicken tendons: association with assembly and growth of collagen fibrils. Dev Dyn 217:430–439
Young BB, Zhang G, Koch M, Birk DE (2002) The roles of types XII and XIV collagen in fibrillogenesis and matrix assembly in the developing cornea. J Cell Biochem 87:208–220
Zhang G, Ezura Y, Chervoneva I, Robinson PS, Beason DP, Carine ET, Soslowsky LJ, Iozzo RV, Birk DE (2006) Decorin regulates assembly of collagen fibrils and acquisition of biomechanical properties during tendon development. J Cell Biochem 98:1436–1449
Zieske JD, Guimaraes SR, Hutcheon AE (2001) Kinetics of keratocyte proliferation in response to epithelial debridement. Exp Eye Res 72:33–39
Zwolanek D, Veit G, Eble JA, Gullberg D, Ruggiero F, Heino J, et al. (2014) Collagen XXII binds to collagen binding integrins via the novel motifs GLQGER and GFKGER. Biochem J. doi:10.1042/BJ20130642
Acknowledgment
We thank Dr David Hulmes for helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Massoudi, D., Malecaze, F. & Galiacy, S.D. Collagens and proteoglycans of the cornea: importance in transparency and visual disorders. Cell Tissue Res 363, 337–349 (2016). https://doi.org/10.1007/s00441-015-2233-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-015-2233-5