Abstract
Background
Rhegmatogenous retinal detachment and proliferative vitreoretinopathy (PVR) are eye diseases that are characterized by mechanical stress involving stretching of the retinal pigment epithelial (RPE) cells by the vitreous or the hyperplastic membranes. Here, we assessed whether mechanical force could change the expression of matrix metalloproteinases (MMPs) in RPE cells via the mitogen-activated protein kinase (MAPK) pathway.
Methods
Collagen-coated magnetite beads and magnetic fields were used to apply tensile forces to cultured RPE cells at focal adhesions. Activation of the MAPK, including extracellular signal-regulated protein kinase (ERK), c-jun N-terminal kinase (JNK), and p38 were determined over a time course from 5 to 30 min by Western-blot analysis. Activation of p38 was also tested using immunofluorescence staining. The mRNA levels of MMP-2, MMP-9, tissue inhibitor of MMP (TIMP)-2 and fibronectin (FN) were analyzed by RT-PCR. Active MMP-2 and MMP-9 were demonstrated by zymography. MMP-2 secretion was evaluated by enzyme immunoassay.
Results
Stimulation of RPE cells with mechanical stress did not change the total protein expression of the MAPK proteins ERK, JNK, and p38. However, of the three kinases, only active p38 showed an increased protein expression which was also shown by a 2.8-fold increase in immunofluorescence staining at 5 min following mechanical stress stimulation. This increase in active p38 expression was blocked by treating the cells with the p38 inhibitor SB203580. FN mRNA increased 2.4-fold at 15 min and MMP-2 mRNA increased 2.1-fold at 4 h. MMP-2 secretion increased 1.5-fold at 4 h and 1.9-fold at 12 h. The expression of MMP-2 and FN, and the activation and secretion of MMP-2, were inhibited in the presence of SB203580. The mRNA expression of MMP-9 and TIMP-2 did not change throughout.
Conclusions
This study shows that mechanical stress upregulates MMP-2 and FN expression through activation of the p38 pathway. The increase in MMP-2 levels evoked by mechanical force may contribute to the remodeling of the extracellular matrix around RPE cells, weakening the interlinkage and membrane attachment between RPE cells, and facilitate cellular migration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mechanical forces exerted on all living cells can induce specific physiological responses depending on the nature of the stress, triggering intracellular signaling mechanisms or pathological processes. In the eye, vitreous contacts directly with the inner limiting membrane of the retina. In proliferative diabetic retinopathy (PDR) or proliferative vitreoretinopathy (PVR), the forces from vitreous retinal traction, flow of liquefied vitreous and the contraction of epi/subretinal membrane can be transmitted through the neural retina layer to the retinal pigment epithelial (RPE) layer, separating the neural retina from the RPE layer and causing retinal detachment. Traction forces are transmitted to the RPE interface and to the RPE itself via interphotoreceptor matrix (IPM), which physically links the neural retina to the RPE [1]. IPM may prevent the detachment of the neural retina from the RPE by mechanical forces in vivo. RPE cells have been reported to undergo stretch during wound healing [2]. Additionally, applying mechanical force to RPE cells in vitro can induce secretion of growth factors such as vascular endothelial growth factor (VEGF) [3].
Matrix metalloproteinases (MMPs) and tissue inhibitor of MMPs (TIMPs) are expressed in IPM and vitreous [4]. MMPs could play a role in several retinal diseases, since they are most likely involved in normal turnover within the extracellular matrix (ECM) that surrounds the neural retina [5]. In neovascularization and proliferative retinopathies, the Bruch’s membrane and the IPM are disintegrated, which suggests that MMPs may contribute significantly to the pathogenesis of ocular diseases [6–8]. Also, in choroidal neovascularization, alteration in MMP production may result in migration of RPE and choroidal endothelial cells and matrix invasion [9]. MMP-2 is secreted mainly by RPE cells and ciliary smooth muscle cells. It is also the major endogenous matrix metalloproteinase in the vitreous [10–12]. In addition, under pathological conditions like PDR and PVR, the neural retina secretes MMP-2 [13].
Mechanical stretch can enhance MMP expression in many kinds of cells, such as hepatic stellate cells [14], cardiomyocytes [15], skeletal muscles [16], vein endothelial cells [17], and vascular smooth muscle cells [18]. However, we have little information about the MMP activation in RPE cells induced by mechanical force. Whether the application of mechanical force to RPE cells contributes to pathological processes is largely unknown. With this point in mind, we utilized a model to stretch RPE cells and investigate MMP expression. Further, since mechanical stretch can evoke multiple responses in mammalian cells via the mitogen-activated protein kinase (MAPK) signaling pathway, we studied this pathway at the same time.
Materials and methods
Reagents
Anti-p38, anti-ERK 1/2, and anti-JNK rabbit polyclonal antibodies as well as the phosphorylated antibodies to each of these kinases were purchased from New England BioLabs (Beverly, MA, USA). An anti beta-actin mouse monoclonal antibody, horseradish peroxidase-conjugated goat antibodies against rabbit or mouse IgG, a fluorescein isothiocyanate-conjugated goat antibody against rabbit IgG, and SB203580 were purchased from Sigma (St. Louis, MO, USA). MMP-2 concentrations were determined by an MMP-2 ELISA kit (Amersham Pharmacia Biotech, Piscataway, NJ, USA). Dulbecco’s Modified Eagle’s Medium (DMEM) and FCS were from Invitrogen-Gibco (Rockville, MD, USA). All other chemicals were reagent grade.
RPE cell culture
Two healthy donor eyes from one adult person were obtained from the Xi’an Central Eye Bank (Xi’an, China) and used in accordance with applicable laws and with the tenets of the Declaration of Helsinki. As previously described [19], eyes were fully bisected by a 360° incision beginning at a position posterior to the ora serrata. The vitreous and retina were removed. The remaining eyecup was washed with phosphate-buffered saline (PBS), followed by addition of 0.025% trypsin-EDTA and then incubation for 30 min at 37°C. The cells were gently scraped and seeded in DMEM with 15% FCS in a culture dish. After proliferation, the cells were retrypsinized with 0.1% trypsin-EDTA solution for 5 min at 37°C. The cells were washed with DMEM and planted in six-well plates at 2 × 104 cells/well. The third or fourth passage cells were used for experiments.
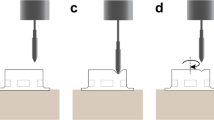
Force generation
Force was produced by a model system described previously [20]. Briefly, magnetite micro particles (Fe3O4, Sigma, St. Louis, MO, USA) were incubated with purified collagen (Vitrogen 100, Cohesion Technologies, Palo Alto, CA, USA; 1 mg/ml), at pH 7.4. After rinsing with PBS, the beads (1 g, 9 × 109) were added into the RPE culture dish (60 mm) and incubated for 30 min. Then, excess non-adherent beads were removed by washing, and the cells were supplemented with fresh DMEM. A ceramic permanent magnet was placed on top of the dish to generate a perpendicular mechanical force (4.4 pN per bead). The treatment time was specific for each individual experiment.
Scanning electronic microscopy (SEM)
RPE cells grown on uncoated glass coverslips were incubated with beads for 30 min. After washing with PBS, the cells were subjected to magnetic force for 30 min. Then, after fixation and dehydration, the specimens were coated with gold. The surface of RPE cells was recorded by SEM (Hitachi, at 20 kV and 80 mA).
Immunoblotting
Cell lysates were prepared from subconfluent RPE cells in 60-mm diameter dishes. Cells were rinsed with PBS and collected in the presence of lysis buffer [50 mM Tris/HCl (pH 7.4), 150 mM NaCl, 0.1% (v/v) SDS, 1% (v/v) NP-40, 1 mM EDTA, 0.2 mM PMSF, 50 mM NaF, 20 μl/ml protease inhibitor cocktail]. Freshly isolated cell homogenates were centrifuged 30 min at 15,000 × g at 4°C. The supernatant was collected and protein concentration was determined by BCA protein assay. All samples were then diluted in Laemmli buffer and boiled. Samples were subjected to SDS-PAGE in 10% gels and transferred to nitrocellulose membranes. The membranes were blocked with 5% skim milk in PBS overnight, washed three times with TBST, and incubated with the primary antibody, which was diluted with Tween-PBS (JNK and ERK1/2 were diluted 1:2000; p38 was diluted 1:1000), for 2 h at room temperature. The membranes were washed three times with TBST, incubated with the secondary antibody, diluted 1:2000 with Tween-PBS, for 1 h at room temperature, washed three times with TBST, and developed by chemiluminescence with LumiGLO (New England BioLabs, Beverly, MA, USA).
Immunofluorescence staining
RPE cells grown on uncoated glass coverslips were subjected to magnetic force for 30 min. Samples were collected and fixed with methanol for 30 min, followed by permeabilization in PBS with 0.3% Triton X-100 for 15 min at room temperature. The cells were then incubated with primary antibody (anti-phospho p38; 1:150) for 1 h at 37°C, and washed three times in PBS with 0.03% Triton and 0.2% BSA, and incubated with FITC-conjugated secondary antibody (1:300). Nonspecific control staining was performed on the same slide by using secondary antibody only. Coverslips were washed in PBS and mounted with the anti-fade mounting medium (Sigma, St. Louis, MO, USA). The cells were analyzed by a confocal laser scanning microscope (Leica TCS-NT, Germany). Fifty cells were selected randomly in each sample for fluorescence quantification (Leica Confocal software).
RNA isolation, reverse transcription (RT), and PCR analysis
RNA isolation was performed with TRI reagent (Molecular Research, Cincinnati, Ohio, USA). All RNA preparations were treated with RQ1 DNase (Promega Corp., Madison, WI, USA) for 30 min. The RT-PCR protocol was performed as described in detail elsewhere [21]. RT was conducted on total RNA (1 μg) using 15 units of AMV reverse transcriptase (Promega Corp., Madison, WI, USA) and 0.5 μg of oligo(dT) primer. The cDNA product was subjected to 30 cycles of amplification in a 30-μl reaction system. PCR-amplified products were shown via agarose gel electrophoresis. Quantification of PCR products was performed by using the UVP Gel Documentation System GDS7500 (UVP, Inc., Upland, CA, USA). The density of each lane was normalized to the density of β-actin. Sequences of the oligonucleotides used in the RT-PCR are shown in Table 1.
Zymographic analysis
The cell homogenate supernatants were collected and the protein concentration was determined. A final concentration of 0.1% gelatin was added to 1-mm-thick minislab gels (10% acrylamide) [22]. Briefly, 20 μg of protein from RPE cells were used. The medium was diluted to normalize for protein quantity before the addition of 5× Laemmli buffer under nonreducing conditions. Electrophoresis was performed at 4°C, and then the gels were washed in 2.5% Triton X-100 for 1 h at room temperature to remove SDS. Gelatinase reactions were facilitated by incubation in 50 mM Tris buffer at 37°C for 24 h. After a rinse in distilled water, the gels were stained with Coomassie brilliant blue (Merck Ltd. Dorset, UK) for 1 h. After subsequent destaining with 10% acetic acid/10% methanol (vol/vol), metalloproteinases could be identified by clear bands against a dark-blue background.
Enzyme-linked immunosorbent assay
RPE cells were seeded in 60-mm diameter dishes and allowed to grow in DMEM with 10% FCS for 12 h. The medium was then replaced with fresh DMEM without FCS. Subconfluent RPE cells were subjected to force. Culture-conditioned, serum-free media were collected. MMP-2 concentration was determined with immunoassays performed according to the instructions of the manufacturers (Amersham Pharmacia Biotech). All samples were evaluated in triplicate.
Statistics
For all assays, mean±SD from the experiments were calculated. The data were analyzed for significance by ANOVA or the paired Student’s t-test. P < 0.01 was considered to be statistically significant.
Results
The magnetic model involves the addition of Fe3O4 beads to RPE cells
We utilized the magnetic model to stretch RPE cells. The beads were rinsed and incubated in collagen solution. After 1 h, a thin collagen layer was formed on the beads’ surface. This allowed the beads to bind to collagen receptors on the surface of RPE cells and allow the applied force to be transmitted directly to the cytoskeleton via the receptors [20]. The cells were washed to remove any unbound beads and then placed under a magnet. After half an hour of force treatment, the cells were observed by SEM. The bound beads were distributed on the dorsal surface of RPE cells (Fig. 1). Most of the beads clumped on the cell membrane above the nucleolus while others separated nearby. This kind of distribution was consistent with a cytoskeletal change evoked by force. There were no beads detached from the cell membrane after force treatment, demonstrating that the applied force was consistent throughout the experiment.
Mechanical force activates the p38 signaling pathway in RPE cells
Since the MAPK signaling pathway is related to many important physiological functions and can be activated by force in other cell types, we checked whether force could activate MAPK in RPE cells. Cell lysates were analyzed by Western blotting to measure total protein levels and phosphorylated forms of ERK1/2, JNK, and p38. ERK1/2 and JNK were both expressed in RPE cells. However, application of mechanical force did not change the protein level of either total ERK1/2 and JNK or the phosphorylated form of ERK1/2, Phospho JNK expression could not be detected (data not shown). This suggests that neither phospho ERK1/2 nor phospho JNK are stimulated by force (Fig. 2a).
MAPK activity in RPE cells. a After mechanical force exposure, cells lysates were prepared and Western blot analysis was performed on the indicated proteins. b The band of active p38 was scanned and calculated as the number of pixels by Glyko Bandscan software. Values are the band-density ratios compared to the control group. *P < 0.01 versus control, n = 3 experiments. c RPE cells were pre-incubated with SB203580 (2 μM), and then exposed to force for 30 min. Samples were collected and probed for active p38. d, e Active p38 immunofluorescence stains in RPE cells. The control group (e) showed a weak fluorescence in the nuclear membrane and cytoplasm, while the cells treated with force (d) showed increased fluorescence intensity. f Quantification of fluorescence intensity in RPE cells. Values are the ratios compared to the control group. *P < 0.01 versus control, n = 50 cells
Although force application did not alter the level of total p38, levels of phospho-p38 increased at 5 min (Fig. 2b). Addition of SB203580, an inhibitor of p38, could selectively inhibit force-induced p38 activation (Fig. 2c). Phospho-p38 fluorescence intensity increased 2.8-fold (278.7% ± 42.2%; P < 0.01; n = 50 cells) in the nuclear membrane and cytoplasm of force treated RPE cells (Fig. 2d, e, f). The beads on the surface of the cells shielded some of the fluorescence emitted from the cytoplasm and nuclear membrane, making the outline of the positive area blurred and interrupted.
Mechanical force upregulates MMP-2 and FN mRNA expression
The balance between MMPs and TIMPs is very important for its direct role in the vitreous liquefaction during aging and pathological processes. To test whether express levels of MMPs and TIMPs were altered during force treatment, mRNA expression was measured by semi quantitative RT-PCR. RPE cells were exposed to force for 15 min, 30 min, 1 h, 4 h, or 12 h. FN mRNA increased approximately 2.4-fold (247.4% ± 31.7%; P < 0.01; n = 3) at 15 min. MMP-2 mRNA increased 2.1-fold (216.7% ± 28.3%; P < 0.01; n = 3) at 4 h (Fig. 3a, b). SB203580 completely abolished the increased mRNA expression of MMP-2 and FN at 12 h (Fig. 3c, d). However, both MMP-9 and TIMP-2 mRNA levels did not change during the time course of the experiment (data not shown).
MMP-2 and FN mRNA expression in RPE cells. a Cells were treated with force for different times and total RNA was isolated. Representative amplicons of MMP-2, FN and β-actin were analyzed by RT-PCR. b The density of each lane was normalized to the density of β-actin. c RPE cells were pre-incubated with SB203580 (2 μM), and then exposed to force for 12 h. Representative amplicons of MMP-2 and FN from the treated group were shown in the last lane. The control group was shown in the first lane. d The quantification of each lane was shown as percentage of the control. *P < 0.01 versus control, n = 3 experiments
Mechanical force upregulates MMP-2 protein expression
MMPs protein-expression levels were measured by zymography. Both static and stretched RPE cells produced a constitutive 72-kD gelatinolytic band consistent with inactive MMP-2, with an increase noticeable at 12 h. The 68-kD gelatinolytic bands consistent with active MMP-2 did not change until 4 h (Fig. 4a, b). Levels of both inactive and active MMP-2 did not change in stretched cells pretreated with SB203580 at 12 h, relative to the unstretched cells (Fig. 4c, d). No active MMP-9 was detected in stretched cells (data not shown).
Force-induced MMP-2 activity in RPE cells. a Cells were treated with force for different times. Extracted protein was analyzed by gelatin zymogram to show inactive and active MMP-2. b The quantification of each band is shown as percentage of the control. c After SB203580 (2 μM) pretreatment, cells were exposed to force for 12 h. The treated group is shown in the last lane. The control group is shown in the first lane. d The quantification of each lane was shown as percentage of the control. *P < 0.01 versus control, n = 3 experiments
Mechanical force upregulates MMP-2 secretion
We collected culture-conditioned, serum-free media to measure the secreted MMP-2 concentration by ELISA. In the supernatants of untreated RPE cells, MMP-2 release was detected at a level of 29.33 ± 7.62 ng/105 cells. In force-treated groups, MMP-2 concentration increased approximately 1.5-fold (1.5 ± 0.23; P < 0.01; n = 3) at 4 h and 1.9-fold (1.94 ± 0.29; P < 0.01; n = 3) at 12 h. These increases could be blocked by SB203580 pretreatment (Fig. 5).
Discussion
Our previous work showed that force application could alter the polarity of RPE cells [23]. Furthermore, after force exposure, an increased expression of both monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) was demonstrated. If pretreated with an inhibitor of actin polymerization, the RPE cells could no longer overexpress both chemokines. This suggests that the cytoskeleton is involved in regulating the expression [24]. However, it was unknown whether the ECM is involved in this process. In the present study, our analysis revealed that the expression of MMP-2 and FN in RPE cells increased after mechanical stress stimulation via the p38 signaling pathway.
RPE cells are stretched by the vitreous, which would presumably apply lateral shear force. Force from hyperplastic membranes of PVR or PDR could be multi-directional. When the neural retina is detached, the outer segments often appear bent in one direction in what appears to be shear-force distortion. It is very difficult, however, to mimic all of the complex situations in vitro as they occur in vivo. Although the model does not exactly replicate the in vivo condition, it does allow an in vitro method for testing the mechanical tension in cells. So it is worth applying the simple model to detect whether mechanical stretch, an important factor that has never been evaluated before, might play a role in the pathological process.
Mechanical stretch occurs in the human eye with PVR or PDR [1]. PVR is a common complication to retinal detachment and the leading cause of anatomical failure in surgery. PVR is associated with the production of inflammatory cytokines, ECM deposition, and release of MMPs from activated cells. RPE cells are a major type of proliferative cell in PVR. Thus far, few studies have examined mechanical force in relation to RPE cells. If the mechanical stretch affects ECM deposition and MMP expression, force should be an important factor in the pathological process. RPE cells, a source of MMPs, proliferate and migrate toward the neural retina and contribute largely to the formation of fibrocellular retinal membranes [25, 26]. In this study, we report that force affects the balance between MMPs and TIMPs, which might affect migration of RPE cells and proliferative membrane formation.
A precise balance between MMP and TIMP activities may be important for the integrity of ECM components. In the family of MMPs, MMP-2 plays a vital role in the eye. MMP-2 exists in an inactive form and an increase in activity is associated with pathologic conditions [27]. During vitreous liquefaction in aging and various pathological states, MMP-2 activity is considered a potential mechanism [28]. In the development of postoperative PVR, all of the vitreous samples express MMP-2 [29]. MMP-2 is the predominant type of MMP in subretinal fluid. The proteolytic activity in subretinal fluid may be connected to the release of RPE cells into subretinal fluid and to vitreous degradation [30]. In the fibrovascular tissues of PDR, ProMMP-2 is efficiently activated, which indicates that the activity of MMP-2 may be involved in the formation of the fibrovascular tissues [31].
The balance between MMPs and TIMPs in RPE cells may be disrupted in some ocular diseases. MMP-2 can reduce sub-RPE deposits formed most notably in age related macular degeneration [32–34]. The integrity of the Bruch's membrane may regulate MMP and TIMP secretion by RPE cells. ECM also sends signals that regulate MMP and TIMP synthesis in RPE cells [35]. RPE cell migration stimulated by cytokines may be facilitated by an increased release of MMPs accompanied by comparatively lower levels of TIMPs [36]. In our study, mechanical stretch enhances MMP-2 expression in RPE cells. Hence, we suggest such a mechanism: when RPE cells are stimulated by the force either from liquefied vitreous or hyperplastic membranes, increased secretion of MMP-2 destroys the balance between MMPs and TIMPs, and changes both the structure and function of IPM and Bruch membrane (unpublished studies), which may facilitate cellular migration. When RPE cells disperse into the vitreous cavity and appear in subretinal fluid, both inflammatory cytokines and MMPs could modulate proliferation and migration of RPE cells, thus causing further development of PVR or PDR.
FN is a substrate of MMPs and a chemoattractant for RPE cells. As an ECM component, FN enhances RPE cell attachment and is present in PVR membranes. Mechanical stretch can upregulate FN mRNA expression in vascular smooth muscle cells [37] and mesangial cells [38]. Our data show a similar result in RPE cells. As cytoskeletal redistribution induced by force seems to be one kind of stress response, upregulation of FN should be considered another one. FN may help to build up and strengthen the ECM around RPE cells.
The change in ECM may activate several signaling pathways, which leads to altered regulation of genes that synthesize and catabolize ECM proteins. At the same time, cell division and tissue structure and function may be altered as well [39]. MAP kinases can be activated in response to various stresses, such as mechanical force, hyperosmolar conditions, oxidative stress, and cytokines [40–42]. Mechanical force activates p38 MAP kinase in rat ventricular myocytes [43]. p38 is the only MAP kinase affected by tensile forces in cardiac fibroblasts [44] and human gingival fibroblasts [45]. In our study, the fluorescence intensity of p38 markedly increased in the cytoplasm and nuclear membrane of RPE cells after force stimulation. We conclude that mechanical force can activate p38 in RPE cells. It is well known that mechanical stretch can evoke many kinds of responses in mammalian cells via the MAPK signaling pathway. MMP-2 is stimulated by cyclic strain in endothelial cells in vitro, in part through both p38- and ERK-dependent pathways [46]. Force inhibits smooth muscle actin in cardiac fibroblasts through p38 pathway [47]. In human mesangial cells, stretch force induces transforming growth factor-ß1 and FN expression via p38 [48]. Our results indicate that force-induced p38 activation plays a central role in MMP and FN expression in RPE cells and influences ECM turnover. Furthermore, since the specific p38 inhibitor SB203580 blocked overexpression of MMPs and FN, p38 appears to be very important to pass force signals downstream to genes and proteins such as MMP-2 and FN. The mechanism may underscore a possible role of p38 inhibitors as anti-decompensate agents of ECM.
In summary, these data indicate that mechanical stretch results in a shift in the balance between MMPs and TIMPs, caused in part by a mechanism involving the p38 signaling pathway. Increased MMP-2 activity evoked by mechanical force may potentially contribute to ECM remodeling around RPE cells, weaken the interlinkage between RPE cells and the membrane being attached, and facilitate cellular migration. These data deepen our understanding of pathological processes and open a potential avenue of therapy for PDR and PVR.
Abbreviations
- ECM:
-
Extracellular matrix
- ERK:
-
Extracelluar signal-regulated protein kinase
- FN:
-
Fibronectin
- IL-8:
-
Interleukin-8
- IPM:
-
Interphotoreceptor matrix
- JNK:
-
c-jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinase
- MCP-1:
-
monocyte chemoattractant protein-1
- MMP:
-
Matrix metalloproteinase
- PDR:
-
Proliferative diabetic retinopathy
- PVR:
-
Proliferative vitreoretinopathy
- RPE:
-
Retinal pigment epithelial
- SEM:
-
Scanning electronic microscopy
- TIMP:
-
Tissue inhibitor of matrix metalloproteinase
- VEGF:
-
Vascular endothelial growth factor
References
Hollyfield JG, Varner HH, Rayborn ME, Osterfeld AM (1989) Retinal attachment to the pigment epithelium: linkage through an extracellular sheath surrounding cone photoreceptors. Retina. 9:59–68
Kalnins VI, Sandig M, Hergott GJ, Nagai H (1995) Microfilament organization and wound repair in retinal pigment epithelium. Biochem Cell Biol. 73:709–722
Seko Y, Seko Y, Fujikura H, Pang J, Tokoro T, Shimokawa H (1999) Induction of vascular endothelial growth factor after application of mechanical stress to retinal pigment epithelium of the rat in vitro. Invest Ophthalmol Vis Sci. 40(13):3287–3291
Plantner JJ, Smine A, Quinn TA (1998) Matrix metalloproteinases and metalloproteinase inhibitors in human interphotoreceptor matrix and vitreous. Curr Eye Res. 17(2):132–140
De La Paz MA, Itoh Y, Toth CA, Nagase H (1998) Matrix metalloproteinases and their inhibitors in human vitreous. Invest Ophthalmol Vis Sci. 39(7):1256–1260
Plantner JJ, Jiang C, Smine A (1998) Increase in interphotoreceptor matrix gelatinase A (MMP-2) associated with age-related macular degeneration. Exp Eye Res. 67:637–645
Steen B, Sejersen S, Berglin L, Seregard S, Kvanta A (1998) Matrix metalloproteinases and metalloproteinase inhibitors in choroidal neovascular membranes. Invest Ophthalmol Vis Sci. 39:2194–2200
Sheridan CM, Occleston NL, Hiscott P, Kon CH, Khaw PT, Grierson I (2001) Matrix metalloproteinases: a role in the contraction of vitreo-retinal scar tissue. Am J Pathol. 159(4):1555–1566
Murphy G, Gavrilovich J (1999) Proteolysis and cell migration: creating a path? Curr Opin Cell Biol. 1:614–621
Alexander JP, Bradley JM, Gabourel JD, Acott TS (1990) Expression of matrix metalloproteinases and inhibitor by human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 31(12):2520–2528
Weinreb RN, Kashiwagi K, Kashiwagi F, Tsukahara S, Lindsey JD (1997) Prostaglandins increase matrix metalloproteinase release from human ciliary smooth muscle cells. Invest Ophthalmol Vis Sci. 38(13):2772–2780
Hunt RC, Fox A, al Pakalnis V, Sigel MM, Kosnosky W, Choudhury P, Black EP (1993) Cytokines cause cultured retinal pigment epithelial cells to secrete metalloproteinases and to contract collagen gels. Invest Ophthalmol Vis Sci. 34(11):3179–3186
Salzmann J, Limb GA, Khaw PT, Gregor ZJ, Webster L, Chignell AH, Charteris DG (2000) Matrix metalloproteinases and their natural inhibitors in fibrovascular membranes of proliferative diabetic retinopathy. Br J Ophthalmol. 84(10):1087–1088
Goto T, Mikami KI, Miura K, Ohshima S, Yoneyama K, Nakane K, Watanabe D, Otaka M, Watanabe S (2004) Mechanical stretch induces matrix metalloproteinase 1 production in human hepatic stellate cells. Pathophysiology. 11(3):153–158
Wang TL, Yang YH, Chang H, Hung CR (2004) Angiotensin II signals mechanical stretch-induced cardiac matrix metalloproteinase expression via JAK-STAT pathway. J Mol Cell Cardiol. 37(3):785–794
Brown MD, Hudlicka O (2003) Modulation of physiological angiogenesis in skeletal muscle by mechanical forces: involvement of VEGF and metalloproteinases. Angiogenesis. 6(1):1–14
Wang BW, Chang H, Lin S, Kuan P, Shyu KG (2003) Induction of matrix metalloproteinases-14 and -2 by cyclical mechanical stretch is mediated by tumor necrosis factor-alpha in cultured human umbilical vein endothelial cells. Cardiovasc Res. 59(2):460–469
Grote K, Flach I, Luchtefeld M, Akin E, Holland SM, Drexler H, Schieffer B (2003) Mechanical stretch enhances mRNA expression and proenzyme release of matrix metalloproteinase-2 (MMP-2) via NAD(P)H oxidase-derived reactive oxygen species. Circ Res. 13;92(11):e80–86
Han QH, Hui YN, Du HJ, Zhang WJ, Ma JX, Wang SY (2001) Migration of retinal pigment epithelial cells in vitro modulated by monocyte chemotactic protein-1: enhancement and inhibition. Graefes Arch Clin Exp Ophthalmol. 239(7):531–538
Glogauer M, Ferrier J (1998) A new method for application of force to cells via ferric oxide beads. Pflugers Arch. 435(2):320–327
D’Addario M, Ahmad A, Xu JW, Menezes J (1999) Epstein-Barr virus envelope glycoprotein gp350 induces NF-kappaB activation and IL-1beta synthesis in human monocytes-macrophages involving PKC and PI3-K. FASEB J. 13(15):2203–2213
Zhang X, Sakamoto T, Hata Y, Kubota T, Hisatomi T, Murata T, Ishibashi T, Inomata H (2002) Expression of matrix metalloproteinases and their inhibitors in experimental retinal ischemia-reperfusion injury in rats. Exp Eye Res. 74(5):577–584
Zhang XG, Hui YN, Han QH, Hou X, Huang XF, Ma JX (2006) Cytoskeleton changes of cultured human retinal pigment epithelial cells in a mechanical stress model. Zhonghua Yan Ke Za Zhi. 42(2):121–126
Zhang XG, Hui YN, Han QH, Hou X, Chen LJ, Ma JX (2005) Effects of mechanical stress on expressions of monocyte chemoattractant protein-1 and interleukin-8 of cultured human retinal pigment epithelial cells. Zhonghua Yi Xue Za Zhi. 85(32):2264–2268
Webster L, Chignell AH, Limb GA (1999) Predominance of MMP-1 and MMP-2 in epiretinal and subretinal membranes of proliferative vitreoretinopathy. Exp Eye Res. 68:91–98
Hiscott P, Sheridan C, Magee RM, Grierson I (1999) Matrix and the retinal pigment epithelium in proliferative retinal disease. Prog Retinal Eye Res. 18:167–190
Brown D, Hamdi H, Bahri S, Kenney MC (1994) Characterization of an endogenous metalloproteinase in human vitreous. Curr Eye Res. 13(9):639–647
Brown DJ, Bishop P, Hamdi H, Kenney MC (1996) Cleavage of structural components of mammalian vitreous by endogenous matrix metalloproteinase-2. Curr Eye Res. 15(4):439–445
Kon CH, Occleston NL, Charteris D, Daniels J, Aylward GW, Khaw PT (1998) A prospective study of matrix metalloproteinases in proliferative vitreoretinopathy. Invest Ophthalmol Vis Sci. 39(8):1524–1529
Immonen I, Konttinen YT, Sorsa T, Tommila P, Siren V (1996) Proteinases in subretinal fluid. Graefes Arch Clin Exp Ophthalmol. 234(2):105–109
Noda K, Ishida S, Inoue M, Obata K, Oguchi Y, Okada Y, Ikeda E (2003) Production and activation of matrix metalloproteinase-2 in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci. 44(5):2163–2170
Amin S, Chong NH, Bailey TA, Zhang J, Knupp C, Cheetham ME, Greenwood J, Luthert PJ (2004) Modulation of Sub-RPE deposits in vitro: a potential model for age-related macular degeneration. Invest Ophthalmol Vis Sci. 45(5):1281–1288
Cousins SW, Marin-Castano ME, Espinosa-Heidmann DG, Alexandridou A, Striker L, Elliot S (2003) Female gender, estrogen loss, and Sub-RPE deposit formation in aged mice. Invest Ophthalmol Vis Sci. 44(3):1221–1229
Marin-Castano ME, Elliot SJ, Potier M, Karl M, Striker LJ, Striker GE, Csaky KG, Cousins SW (2003) Regulation of estrogen receptors and MMP-2 expression by estrogens in human retinal pigment epithelium. Invest Ophthalmol Vis Sci. 44(1):50–59
Padgett LC, Lui GM, Werb Z, LaVail MM (1997) Matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-1 in the retinal pigment epithelium and interphotoreceptor matrix: vectorial secretion and regulation. Exp Eye Res. 64(6):927–938
Eichler W, Friedrichs U, Thies A, Tratz C, Wiedemann P (2002) Modulation of matrix metalloproteinase and TIMP-1 expression by cytokines in human RPE cells. Invest Ophthalmol Vis Sci. 43(8):2767–2773
Tamura K, Chen YE, Chen Q, Nyui N, Horiuchi M, Takasaki I, Tamura N, Pratt RE, Dzau VJ, Umemura S (2000) Expression of renin-angiotensin system and extracellular matrix genes in cardiovascular cells and its regulation through AT1 receptor. Mol Cell Biochem. 212(1–2):203–209
Ishida T, Haneda M, Maeda S, Koya D, Kikkawa R (1999) Stretch-induced overproduction of fibronectin in mesangial cells is mediated by the activation of mitogen-activated protein kinase. Diabetes. 48(3):595–602
Silver FH, Siperko LM (2003) Mechanosensing and mechanochemical transduction: how is mechanical energy sensed and converted into chemical energy in an extracellular matrix? Crit Rev Biomed Eng. 31(4):255–331
Ruwhof C, van der Laarse A (2000) Mechanical stress-induced cardiac hypertrophy: mechanisms and signal transduction pathways. Cardiovasc Res. 47(1):23–37
Raingeaud J, Gupta S, Rogers J, Dickens M, Han J, Ulevitch RJ, Davis RJ (1995) Pro-inflammatory cytokines and environmental stress cause p38 MAP kinase activation by dual phosphorylation on tyrosine and threonine. J Biol Chem 270:7420–7426
Han J, Lee JD, Bibbs L, Ulevitch RJ (1994) A MAP kinase targeted by endotoxin and hyperosmolarity in mammalian cells. Science 265:808–811
Liang F, Gardner DG (1999) Mechanical strain activates BNP gene transcription through a p38/NF-kappaB-dependent mechanism. J Clin Invest. 104(11):1603–1612
Wang J, Seth A, McCulloch CA (2000) Force regulates smooth muscle actin in cardiac fibroblasts. Am J Physiol Heart Circ Physiol. 279(6):H2776–H2785
D'Addario M, Arora PD, Ellen RP, McCulloch CA (2002) Interaction of p38 and Sp1 in a mechanical force-induced, beta 1 integrin-mediated transcriptional circuit that regulates the actin-binding protein filamin-A. J Biol Chem. 277(49):47541–47550
von Offenberg Sweeney N, Cummins PM, Birney YA, Cullen JP, Redmond EM, Cahill PA (2004) Cyclic strain-mediated regulation of endothelial matrix metalloproteinase-2 expression and activity. Cardiovasc Res. 63(4):625–634
Wang J, Seth A, McCulloch CA (2000) Force regulates smooth muscle actin in cardiac fibroblasts. Am J Physiol Heart Circ Physiol. 279(6):H2776–H2785
Gruden G, Zonca S, Hayward A, Thomas S, Maestrini S, Gnudi L, Viberti GC (2000) Mechanical stretch-induced fibronectin and transforming growth factor-beta1 production in human mesangial cells is p38 mitogen-activated protein kinase-dependent. Diabetes. 49(4):655–661
Acknowledgments
This project was supported by the National Science Foundation of China (No. 30200311) and partly by the equipment donation from the Alexander von Humboldt Foundation in Germany (to YS Wang, V-8151/02085). We also acknowledge the editorial assistance provided by the NIH Fellows Editorial Board.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Foundation item: National Natural Science Foundation of China. (N30200311).
There are no commercial relationships to declare.
The authors have full control of all primary data and they agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Rights and permissions
About this article
Cite this article
Hou, X., Han, QH., Hu, D. et al. Mechanical force enhances MMP-2 activation via p38 signaling pathway in human retinal pigment epithelial cells. Graefes Arch Clin Exp Ophthalmol 247, 1477–1486 (2009). https://doi.org/10.1007/s00417-009-1135-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-009-1135-1