Abstract
Background
We evaluated the outcomes of patients with different forms of chronic uveitis treated with mycophenolate mofetil (MMF) as an immunomodulatory and steroid-sparing agent. The multi-system side effects that arise after long-term treatment with corticosteroids and other immunosuppressants prompted us to use MMF. MMF is a selective inhibitor of inosine monophosphate dehydrogenase, thus blocking purine synthesis via the de novo pathway preferentially used by T and B lymphocytes.
Methods
Between 1998 and 2003, 106 patients were treated for uveitis (anterior n=26, intermediate n=51, posterior n=23, panuveitis n=6) with MMF at a dose of 1g twice daily. Treatment duration was at least 6 months (n=10), in most cases greater than 12 months (n=77) and in 25 cases between 24 months and 41 months, when the present retrospective evaluation was undertaken. Patient charts were analysed according to a standardized evaluation protocol.
Results
In 95 patients MMF was combined with prednisolone at a dosage of 2.5–10 mg per day. In 8 patients MMF was used as a monotherapy, and in 3 cases one further systemic immunosuppressant was required. The number of recurrences during MMF treatment was none or one in 92 patients, two in 6 cases and three or more in 8 patients. In none of the patients had MMF been stopped at the time of data analysis. The most frequently observed side effects were gastrointestinal upset (15%), followed by headache (9.3%), fatigue (5.7%), eczema (5%), and hair loss (3.5%). Other side effects were sporadic. Most of these phenomena were transitory. Forty-two patients experienced no side effects at all. In 4 patients MMF was judged ineffective due to failure to reduce the number of recurrences of severe inflammation compared with the previous therapeutic regime, or indeed occurrence of persistent macular oedema.
Conclusions
Our results show that MMF is an effective immunosuppressant in patients with uveitis. We provide evidence that MMF controls the disease in the majority of patients with an acceptable profile of side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High doses of prednisolone alone or in combination with immunosuppressive agents such as cyclosporine A (CsA), and methotrexate (MTX) are often required to control the sight-threatening and sometimes blinding consequences of intraocular inflammation [7, 17]. However, up to a third of patients may fail on this regime [22], and CsA and prednisolone both bear a considerable long-term risk due to their toxic effects on protein and glucose metabolism and on the kidney [9]. Other immunomodulatory drugs such as tacrolimus [20] and azathioprine [17] have also been tried in patients with refractory uveitis, but their use is not widespread. Mycophenolic acid (MPA) is an immunosuppressive agent that was first used in the 1970s for the treatment of psoriasis [27]. Its immunosuppressive activity is based on inhibition of inosine monophosphate dehydrogenase, an enzyme required for the de novo synthesis of purines [2]. Because T and B cells rely solely on this pathway for the production of guanosine nucleotide for their DNA synthesis, the proliferation of these cells is inhibited by MPA [29]. Since the mid-1990s the greatest clinical experience has been with the morpholinoethyl ester of mycophenolic acid, mycophenolate mofetil (MMF), in renal allograft transplantation [11, 26, 28], where it is now of established efficacy [25]. The drug has also been used successfully for the treatment of bullous pemphigoid [6], pemphigus vulgaris [10], ocular pemphigoid [32], rheumatoid arthritis [12], autoimmune haemolytic anaemia [31], systemic lupus erythematosus [1] and Crohn's disease [19]. MMF has been shown to inhibit experimental autoimmune uveitis in rats [8], and its use in human inflammatory eye disease has been described in studies with up to 54 patients [4, 13–16] since 1998, including one from our own group [30]. To our knowledge the present retrospective analysis represents the first report of a large number of patients (n=106) affected exclusively by uveitis in its various forms that were treated over a prolonged period of time.
Methods
Between 1998 and 2003 we used MMF (CellCept; Hoffmann-La Roche, Grenzach-Wyhlen, Germany) to treat 106 patients affected by different forms of uveitis at our tertiary referral centre. Twenty-six patients suffered from anterior uveitis, 51 from intermediate uveitis, 23 from posterior uveitis and 6 patients had panuveitis. The rationale for introducing MMF was intolerance to high-dose steroids (>20 mg/day) administered over at least 6 months continuously, arterial hypertension and impairment of kidney function parameters on CsA or significant alterations of the differential blood count on MTX, or refractory uveitis where prednisolone had been used in combination with CsA or MTX or both. The MMF dosage used was 1 g orally twice daily, which is the standard dose recommended to prevent allograft rejection in renal transplant patients [28]. However, according to anecdotal unpublished reports, the incidence of side effects may be reduced if MMF is initially introduced at a reduced dosage, before administering the full dose of 2 g daily. In fact, all patients entered into this retrospective evaluation had received MMF at 1 g per day (i.e. 500 mg twice daily) during the first week of treatment. The full dose of 2 g per day (i.e. 1 g twice daily) was not administered until 7 days after MMF therapy was instituted. Subsequently the MMF dose was neither increased nor tapered throughout the time of therapy.
At the start of treatment prednisolone was given concomitantly in all patients evaluated. Prednisolone was started at a dose of 1 mg/kg body weight per day when the inflammation was active and was reduced slowly but in standardized fashion in weekly steps of 10 mg until reaching 30 mg/day, then in weekly steps of 5 mg or 2.5 mg, depending on the clinical findings, with the aim of achieving maintenance levels of between 10 mg and 2.5 mg per day. No glucocorticoid agent other than prednisolone was used in any patient. In those individuals in whom the clinical course of disease was favourable, with one recurrence or none at all under MMF/prednisolone and achievement of maintenance doses of ≤2.5 mg of steroid, the ultimate goal was MMF monotherapy. Mean treatment duration was 15.5 months in the anterior uveitis group, 20.0 months in the intermediate uveitis group, 15.3 months in the posterior uveitis group and 19.5 months in the panuveitis group. Patient case sheets were analysed according to a standardized protocol. Before commencement of MMF administration, the patient's history of uveitis was taken. Patients were asked about associated diseases, in case they were not already known to us by our own medical records. Routine laboratory investigations included a complete blood count with differential, urea, creatinine and electrolytes, and liver function tests. Other laboratory studies such as antinuclear antibody, HLA type, fluorescent antitreponemal antibody absorption test for syphilis and a test for angiotensin-converting enzyme activity were performed on first presentation to our service. All our patients received a chest X-ray examination at baseline. Effectiveness of treatment was assessed by standard ophthalmic examination techniques, including measurement of visual acuity in both eyes in European decimals, a slit-lamp examination and indirect binocular ophthalmoscopy to determine disease severity (the following parameters were recorded: anterior chamber activity, vitreous infiltration, retinal vascultis, macular oedema and disc swelling). At each visit patients were asked about drug side effects and blood pressure was determined. In all patients full blood count, blood chemistry and liver function tests were performed during the first month of treatment weekly, during the second and third months twice per month and thereafter once monthly. This was considered important, particularly in view of the fact that MMF may cause bone marrow dysfunction in ≥10% of treated patients [28]. We measured treatment efficacy in this study primarily by the improvement in symptoms and signs of ocular inflammation along with the effect of the treatment with MMF on visual acuity. Another important criterion for therapeutic success was the amount by which the prednisolone could be reduced. The treatment with MMF was judged ineffective if there was no advantage over the previously used immunosuppressives in terms of recurrences of uveitis and/or the recurrence or persistence of macular oedema.
Results
The patient details are given in Tables 1, 2. By their own account, the majority of patients in all groups had suffered between 5 and 10 recurrences in the 5-year period prior to commencing MMF, despite various immunosuppressive regimes, and/or were dependent on inacceptably high doses of prednisolone. In Table 3 the length of time for which MMF treatment had been in place at the time of data evaluation is shown for all patients within each type of uveitis.
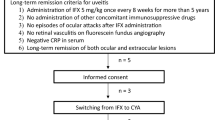
A graphic representation of the raw data (Fig. 1) shows that, looking at all forms of uveitis together, the frequency of recurrences was one or none in the majority of patients (n=92), two in 6 cases and three or more in 8 patients. In four of the latter patients treatment with MMF was discontinued as the drug was judged ineffective in controlling the disease (as defined above). In 95 patients MMF was combined with prednisolone in a dosage of 2.5–10 mg/day. In 8 patients MMF was used as a monotherapy and in 3 cases one further systemic immunosuppressant (CsA) was required (data not shown).
From the start of MMF treatment to the time of evaluation we looked at the development of visual acuity in each affected eye. In the case of bilateral disease it was decided that the better eye at the onset of treatment would provide a more accurate measure of treatment efficacy, as in most cases of long disease duration, even with no disease activity, the morphological changes that have taken place in the worse eye preclude any improvement in visual acuity. Figure 2 shows that in the anterior and intermediate uveitis group there was no deterioration in visual acuity during MMF treatment (see Table 4). In all patients of these groups visual acuity improved or stayed the same. Five patients with posterior uveitis and two patients with panuveitis, however, worsened slightly during the study period. As the most pressing reason for using MMF was the occurrence of intolerable side effects with other immunosuppressive combinations of drugs, we were surprised to see that the profile of side effects during MMF therapy was comparatively mild (Fig. 3). The most frequently observed side effects were gastrointestinal symptoms such as stomach pain, nausea and diarrhoea (15%), followed by headache (9.3%), fatigue (5.7%), eczema (5%), and hair loss (3.5%). Most of these phenomena were transitory and subsided after a few weeks' treatment. Forty-two patients experienced no side effects at all. In one patient MMF was stopped after 8 months when the patient contracted a viral infection with ensuing encephalitis requiring treatment in an intensive care unit. Laboratory parameters changed only slightly in a few patients, in particular there was no change noted in any patients with regard to parameters indicating bone marrow dysfunction. In two patients cholesterol-lowering drugs were deemed necessary by the consulting physician. Interestingly, in both of these patients the dosage of MMF did not need to be increased, although cholesterol-lowering drugs are known to bind biliary acids and thus may affect the entero-hepatic circulation of MPA and reduce its bioavailability.
Discussion
The results of this study are in agreement with other encouraging long-term findings in the treatment of atopic dermatitis, Wegener's granulomatosis and microscopic polyangiitis [5, 21]. We found that MMF successfully controlled intraocular inflammation as well as achieving prednisolone reduction, albeit in only four patients. Of our cohort of patients that remained stable, in eight patients we were able to use MMF as a monotherapy; in all others a low maintenance dose of prednisolone was required. We were impressed with the therapeutic success we obtained. However, we did not evaluate the efficacy of MMF on its own but only in combination with prednisolone. Indeed, this combination was used in each patient right from the start of treatment, with the aim of slowly tapering the steroid, thus taking advantage of the steroid-sparing property of MMF. We did not test MMF as a sole immunosuppressive agent in acute uveitis. A direct comparison with cyclosporine is therefore not possible. CsA was evaluated in a randomized, double-masked study in comparison with prednisolone in uveitis patients [22]. In this study patients who could not efficiently be treated by either drug were however ultimately classed as therapeutic successes when cyclosporine and prednisolone were combined. Although the ophthalmologist is often faced with the precarious task of balancing the efficacy of immunosuppressants against their potential side effects even at the manufacturer's recommended dosage, in this retrospective analysis long-term tolerance to MMF was as good as has been found in patients undergoing kidney transplantation [23]. This could be explained by the fact that MPA is a more potent inhibitor of the type II isoform of the inosine monophosphate dehydrogenase (IMPDH) enzyme expressed in activated lymphocytes than of the type I isoform of IMPDH expressed in most other cell types [2]. MPA therefore has a more potent cytostatic effect on lymphocytes than on other cell types. Thus proliferation of T and B cells is more heavily targeted by MMF than that of other cells, and the use of MMF is associated with lesser myelosuppression and toxic effects on other cells. Other cells can use both the de novo pathway and the salvage pathway for purine synthesis. Furthermore, by depleting GTP, MMF is able to inhibit the glycosylation of adhesion molecules and the binding of activated human lymphocytes to activated human endothelial cells [8]. MMF is the ester of MPA, which in turn represents a fermentation product of several Penicillium species [3]. It is absorbed within 30 min and broken down in the liver to MPA, its metabolically active form. Its mean half-life, including the entero-hepatic circulation, is 15.8 h. Steady-state plasma levels are reached after 7 days, which accounts for the rapid onset of action of MMF in comparison with other systemic immunosuppressants. Due to its relative selectivity, MMF is typically not associated with adverse effects such as nephrotoxicity, hypertension, electrolyte imbalance, hyperglycaemia, hyperuricaemia, hypercholesterolaemia (the manufacturer has found the incidence of changes in metabolic parameters to range between 1% and <10% in controlled clinical studies of kidney, heart and liver transplant patients where MMF was used in combination with cyclosporine and corticosteroids) and osteoporosis. In the present study, the reported side effects were usually mild and transitory at the beginning of MMF treatment, the gastrointestinal symptoms being the most troublesome to the patients subjectively. The use of MMF has been associated with severe fungal infections and malignancies in patients receiving pancreatic transplants [24] and with myelosuppression in renal transplant patients [18]. Such adverse effects were not found in the present study, where we used a maximum dose of 2 g per day. Previous reports also suggest that the risk of developing lymphoma is lower on MMF than on CsA maintenance therapy in renal transplant patients [11, 26]. This may be of great value given that patients with uveitis are often young and require treatment for many years. The present study shows that treatment with MMF retained its efficacy with the passage of time in the majority of uveitis patients. Although we observed a relatively large number of patients over a considerable time span, the present study is limited by its open and uncontrolled nature. Although our results encourage the administration of MMF for treatment of severe uveitis with sight-threatening inflammation, its use is somewhat limited due to its considerable cost. However, MMF should be considered where a high prednisolone maintenance dosage is required or when other immunosuppressive agents show toxicity or lack of efficacy.
References
Adu D, Cross J, Jayne DR (2001) Treatment of systemic lupus erythematosus with mycophenolate mofetil. Lupus 10:203–208
Allison AC, Eugui EM (1993) Immunosuppressive and other effects of mycophenolic acid and an ester prodrug, mycophenolate mofetil. Immunol Rev 136:5–28
Allison AC, Eugui EM (1994) Mycophenolate mofetil (RS-61443): mode of action and effects on graft rejection. In: Thompson AW, Starzl TE (eds) Immunosuppressive drugs: developments in anti-rejection therapy. Arnold, London, pp 141–159
Baltatzis S, Tufail F, Yu EN, Vredeveld CM, Foster CS (2003) Mycophenolate mofetil as an immunomodulatory agent in the treatment of chronic ocular inflammatory disorders. Ophthalmology 110:1061–1065
Benez A, Fierlbeck G (2001) Successful long-term treatment of severe atopic dermatitis with mycophenolate mofetil. Br J Dermatol 144:638–639
Böhm M, Beissert S, Schwarz T et al (1997) Bullous pemphigoid treated with mycophenolate mofetil. Lancet 349:541
Bom S, Zamiri P, Lightman S (2001) Use of methotrexate in the management of sight-threatening uveitis. Ocul Immunol Inflamm 9:35–40
Chanaud MP, Vistica BP, Eugin E et al (1995) Inhibition of experimental autoimmune uveoretinitis by mycophenolate mofetil, an inhibitor of purine metabolism. Exp Eye Res 61:429–434
Deray G, Benhmida M, Le Hoang P et al (1992) Renal function and blood pressure in patients receiving long-term, low-dose cyclosporin therapy for idiopathic autoimmune uveitis. Ann Intern Med 117:578–583
Enk AH, Knop J (1997) Treatment of pemphigus vulgaris with mycophenolate mofetil. Lancet 350:494
European Mycophenolate Mofetil Cooperative Study Group (1995) Placebo-controlled study of mycophenolate mofetil combined with cyclosporine and corticosteroids for prevention of acute rejection. Lancet 345:1321–1325
Goldblum R (1993) Therapy of rheumatoid arthritis with mycophenolate mofetil. Clin Exp Rheumatol 11(Suppl 8):S117–S119
Greiner K, Varikkara M, Santiago C, Forrester JV (2002) Efficiency of mycophenolate mofetil in the treatment of intermediate and posterior uveitis. Ophthalmologe 99:691–694
Kilmartin DJ, Forrester JV, Dick AD (1998) Rescue therapy with mycophenolate mofetil in refractory uveitis. Lancet 352:35–36
Larkin G, Lightman S (1999) Mycophenolate mofetil. A useful immunosuppressive in inflammatory eye disease. Ophthalmology 218:222–228
Lau CH, Comer M, Lightman S (2003) Long-term efficacy of mycophenolate mofetil in the control of severe intraocular inflammation. Clin Exp Ophthalmol 31:487–491
Lightman S (1996) New therapeutic options in uveitis. Eye 11:222–226
Lipsky JJ (1996) Mycophenolate mofetil. Lancet 348:1357–1359
Meihsler W, Reinisch W, Moser G et al (2001) Is mycophenolate mofetil an effective alternative in azathioprine-intolerant patients with chronic active Crohn's disease? Am J Gastroenterol 96:782–787
Mochizuki M, Masuda K, Sakane T et al (1993) A clinical trial of FK506 in refractory uveitis. Am J Ophthalmol 115:763–769
Nowack R, Gobel U, Klooker P et al (1999) Mycophenolate mofetil for maintenance therapy of Wegener's granulomatosis and microscopic polyangiitis: a pilot study in 11 patients with renal involvement. J Am Soc Nephrol 10:1965–1971
Nussenblatt RB, Palestine AG, Chan CC et al (1991) Randomised, double-masked study of cyclosporin compared to prednisolone in the treatment of endogenous uveitis. Am J Ophthalmol 112:138–146
Pirsch J, Bekersky I, Vincenti F et al (2000) Coadministration of tacrolimus and mycophenolate mofetil in stable kidney transplant patients: pharmacokinetics and tolerability. J Clin Pharmacol 40:527–532
Rigotti P, Cadrobbi R, Baldan N et al (2000) Mycophenolate mofetil (MMF) versus azathioprine (AZA) in pancreas transplantation: a single-center experience. Clin Nephrol 53:52–54
Sarwal MM, Yorgin PD, Alexander S et al (2001) Promising early outcomes with a novel, complete steroid avoidance immunosuppression protocol in pediatric renal transplantation. Transplantation 72:13–21
Sollinger HW (1995) US Renal Transplant Mycophenolate Mofetil Study Group. Mycophenolate mofetil for the prevention of acute rejection in primary cadaveric renal allograft recipients. Transplantation 60:225–232
Spatz S, Rudnicka A, McDonald CJ (1978) Mycophenolic acid in psoriasis. Br J Dermatol 98:429–435
Tricontinental Mycophenolate mofetil Renal Transplantation Study Group (1996) A blinded, randomized clinical trial of mycophenolate mofetil for the prevention of acute rejection in cadveric renal transplantation. Transplantation 61:1029–1037
Young CJ, Sollinger HW (1994) Mycophenolate mofetil (RS-61443). In: Kupiec-Weglinski JW (ed) New immunosuppressive modalities in organ transplantation. Landes, Austin, TX, pp 1–17
Zierhut M, Stübiger N, Aboalchamat W et al (2001) Immunosuppressive treatment with mycophenolate mofetil (CellCept) in the therapy of uveitis. Ophthalmologe 98:647–651
Zimmer-Molsberger B, Knauf W, Thiel E (1997) Mycophenolate mofetil for severe autoimmune haemolytic anaemia. Lancet 350:1003–1004
Zurdel J, Aboalchamat B, Zierhut M et al (2001) Erste klinische Erfahrungen mit Mycophenolat mofetil bei der immunsuppressiven Therapie des okulären Pemphigoids. Klin Monatsbl Augenheilkd 218:222–228
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siepmann, K., Huber, M., Stübiger, N. et al. Mycophenolate mofetil is a highly effective and safe immunosuppressive agent for the treatment of uveitis. Graefe's Arch Clin Exp Ophthalmo 244, 788–794 (2006). https://doi.org/10.1007/s00417-005-0066-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-005-0066-8