Abstract
Purpose
Although infliximab (IFX) decreases the risk of blindness due to refractory uveitis in patients with Behçet's disease (BD), there are no standard criteria for IFX switching or withdrawal. To evaluate the effect of IFX switching in patients with BD in long-term remission, a prospective, single-arm intervention trial was conducted, switching from IFX to cyclosporine A (CYA).
Study design
A prospective open-label study.
Methods
Eligible patients met the following criteria: administration of IFX without concomitant immunosuppressants for more than 5 years with no episodes of ocular attacks, no retinal vasculitis on fluorescein fundus angiography, negative C-reactive protein in serum, and no extraocular lesions at the time of IFX withdrawal. CYA 5 mg/kg/day was administered from 6 weeks after IFX withdrawal. The primary outcome was the rate of readministration of tumor necrosis factor inhibitors at 1 year after IFX withdrawal.
Results
Three of 45 BD patients treated with IFX for refractory uveitis were included in the study. At 1 year after withdrawal of IFX, no patient had experienced any ocular attacks or needed readministation of IFX. However, extraocular lesions, such as recurrent oral ulcers, folliculitis, and recurrent fevers, occurred in all patients. Liver or renal dysfunction, which may have been caused by CYA, was also observed in all patients.
Conclusions
Although no ocular attacks were observed for at least 1 year after IFX withdrawal, this prospective study indicates that IFX withdrawal should be considered carefully, even for patients in long term remission of ocular and extraocular lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behçet's disease (BD) is a systemic inflammatory vascular disease characterized by recurrent oral ulcers, genital ulcers, ocular lesions (anterior uveitis, posterior uveitis, and retinal vasculitis), skin lesions (folliculitis-like rash, skin ulcers, and erythema nodosum), neurological symptoms, and vascular lesions (arterial thrombosis, vena cava thrombosis, and phlebitis or superficial phlebitis) [1, 2].
The ocular lesions, consisting of recurrent attacks of vasculitis in the posterior pole of the retina, cause irreversible retinal and optic atrophy, leading to loss of vision [3]. Before the introduction of tumor necrosis factor (TNF) inhibitors and cyclosporine A (CYA), only 25% of patients with ocular attacks including the posterior pole unit maintained their visual function for 5 years [4].
In patients with BD ocular lesions, it is important to ameliorate acute paroxysmal ocular inflammation and reduce the frequency and severity of subsequent ocular attacks for a good visual prognosis [5]. The European Association for Rheumatology (EULAR) recommends treatment of sight-threatening uveitis of BD with high-dose corticosteroids, infliximab (IFX), or interferon alpha to induce and maintain remission of ocular involvement [6].
IFX is a human–mouse chimeric monoclonal antibody that binds to human TNF and neutralizes its activity, resulting in rapid amelioration of inflammation [7]. The serum level of TNF in active BD patients is significantly elevated compared with normal subjects [8], indicating the importance of TNF inhibitors such as IFX. Decrease in TNF production by modulating the functional activity of T-helper type 1 lymphocytes is thought to contribute to the marked clinical effect of IFX [8]. IFX produces rapid remission of ocular inflammation to prevent blindness in patients who are resistant to conventional immunosuppressive therapies (systemic corticosteroids, cyclophosphamide, azathioprine, CYA, thalidomide, methotrexate, etc.) [9,10,11,12,13]. The effectiveness of IFX was first reported in 2001 [12]. Since 2007, when IFX was approved for intractable uveitis of BD in Japan, IFX has shown a remarkable suppressive effect on ocular attacks [13, 14].
However, long-term administration of IFX may increase the risk of malignant lymphoma and opportunistic infections such as tuberculosis [15], as well as placing an economic burden on patients and the medical economy. Although some patients may be able to discontinue IFX because of long-term remission of ocular inflammation, there are no criteria for withdrawal from IFX treatment. No prospective study of switching or withdrawal of IFX in patients in long-term remission has been reported so far. Here we present the first short-term report of an open-label, prospective, single-arm study of switching from IFX to CYA for refractory uveitis in patients with BD in long-term remission.
Materials and methods
Materials
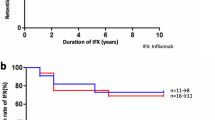
Forty-five BD patients being treated with IFX for ocular lesions of recurrent refractory retinal uveitis that was resistant to conventional treatments from 2007 to March 2017 at Yokohama City University Hospital were screened for the study (Fig. 1). The inclusion criteria were administration of IFX 5 mg/kg once every 8 weeks for more than 5 years, no concomitant administration of other immunosuppressive drugs at the time of IFX withdrawal, no episodes of ocular attacks after IFX administration, no retinal vasculitis on fluorescein fundus angiography (FA) at the time of IFX withdrawal, negative C-reactive protein in serum at the time of IFX withdrawal, and long-term remission of both ocular and extraocular lesions at the time of IFX withdrawal. The exclusion criteria were a history of renal dysfunction, liver dysfunction, pancreatic dysfunction, hypertension, active or latent infections, or cancer; taking cyclosporine combination contraindicated drugs (live vaccine, tacrolimus, etc.); and presence of IFX-neutralizing antibodies. Five of the 45 patients met all the criteria, and informed consent was obtained from 3 of the 5 patients.
Methods
CYA 5 mg/kg/day was administered orally as an alternative agent from 6 weeks after the last day of IFX administration. In order to avoid excessive immunosuppression, cyclosporine administration was started 6 weeks after discontinuation of IFX with the blood concentration of IFX sufficiently low.
Colchicine was adopted as a concomitant drug. In Japan, cyclosporine, colchicine, and prednisolone for eye inflammation caused by Behcet's disease are covered by health insurance. Cyclosporine and colchicine were selected as alternatives to IFX because prednisolone may induce eye attacks during tapering.
The observation period was 1 year. The patients were evaluated at the time of enrollment and 2 weeks, 1 month, 2 months, 4 months, 6 months, 8 months, 10 months, and 1 year after IFX withdrawal. For evaluation of ocular attacks, the Behçet’s disease ocular attack score 24 (BOS24), a scoring system for the severity of ocular attacks, was used [16]. BOS24-6 M, an integrated value for 6 months of BOS24, was also evaluated for the 6 months before withdrawal and the second half of the observation period.
When ocular inflammation was observed after IFX withdrawal and the switch to CYA, the dose of CYA was increased and topical ocular treatment by corticosteroid and mydriatic eyedrops was administered. TNF inhibitors were immediately reintroduced whenever a patient met any of the following criteria: an ocular attack with BOS24 ≥ 8; two or more ocular attacks with 4 ≤ BOS24 ≤ 8; or three or more ocular attacks with 2 ≤ BOS24 ≤ 3. Adalimumab was also accepted as a TNF inhibitor for reintroduction. The primary endpoint of this study was the rate of reintroduction of biologics due to relapse of ocular inflammation and extraocular symptoms after IFX withdrawal and CYA administration. Visual acuity, intraocular pressure, retinal vasculitis detected by fluorescent FA, and findings from blood tests were evaluated as secondary endpoints. Blood IFX-neutralizing antibodies were measured at 6 months and 1 year. Adverse events that occurred during the observation period were evaluated.
This study was approved by the Yokohama City University Hospital Ethics Committee and was conducted in accordance with the Declaration of Helsinki. All patients gave informed consent to participate.
Results
Three male patients with BD uveitis in long-term remission treated with IFX were enrolled in this study. The patients’ backgrounds are shown in Table 1. The patients were treated with IFX for frequent ocular attacks in the posterior pole causing impairment of visual acuity (Table 2). The mean age of onset was 28.3 ± 8.7 years. The mean duration of IFX administration was 8.8 ± 1.0 years, and the mean duration of remission of ocular inflammation was 7.3 ± 0.9 years after IFX administration.
After IFX withdrawal, no ocular attacks were observed in any patient during the observation period. The rate of the reintroduction of biologics at one year was 0% (Table 3). Best-corrected visual acuity was maintained between 1.0 and 1.2 before and after IFX withdrawal. In patient 3, although signs of ocular inflammation, such as anterior chamber cells, retinal exudates, and hemorrhage, were not observed by slit-lamp examination, FA examination at 1 year detected slight leakage of fluorescent dye from the retinal blood vessels (Fig. 2).
In contrast to the absence of ocular lesions, extraocular symptoms, such as folliculitis, stomatitis, low back pain, and recurrent fever, were observed in all patients. In patients 1 and 2, oral colchicine was administered for extraocular symptoms, but it did not prove effective for stomatitis and folliculitis.
All patients showed symptoms of liver or renal dysfunction that might have been caused by CYA at the starting dose of 5.0 mg/kg/day. After the dose of CYA was reduced to an average maintenance dose of 3.0 mg/kg/day, liver and renal function was improved.
In all cases, systemic symptoms recurred immediately after the dose of cyclosporine was reduced.
IFX-neutralizing antibody was measured at 6 months and 1 year from the starting time to IFX withdrawal. No IFX-neutralizing antibody was detected in any patient.
Beyond the observation period, at 14 months after the discontinuation of IFX, patient 3 had ocular inflammation and exacerbation of extraocular symptoms, such as oral ulcers, low back pain, and recurrent fever; therefore, adalimumab was introduced. Remission of ocular and extraocular lesions was achieved after adalimumab administration.
Discussion
All three patients in this study were administered IFX during long-term remission of both ocular and extraocular inflammation without any severe side effects, confirming the tolerability and safety of IFX for patients with refractory BD uveitis.
No ocular inflammatory attacks were seen after the withdrawal of IFX, and the reintroduction rate of TNF inhibitors at 1 year was 0%. Slit-lamp examination did not reveal any findings suggestive of ocular inflammation, such as inflammatory cells in the anterior chamber, retinal hemorrhage, or exudative spots. However, in patient 3, FA revealed mild leakage from the retinal capillaries at 1 year after withdrawal of IFX, indicating possible inflammation. Fourteen months later, adalimumab was introduced to patient 3 due to the exacerbation of ocular inflammation and extraocular symptoms. After adalimumab introduction, remission was maintained in this patient without any lesions.
There have been several studies of IFX withdrawal for recurrent retinal uveitis in BD. In an open-label, prospective, single-arm study, Niccoli et al. reports that seven of nine patients (77.8%) who discontinued IFX remained in remission 1 year later, and oral ulcers recurred in two patients [17]. In a 1-year retrospective study, Kawaguchi et al. reported that five of seven patients (71.4%) who were forced to discontinue IFX due to side effects remained in remission with conventional treatments [18]. In a retrospective study of withdrawal of IFX, Adán et al. report that, on average two of four patients who remained in remission for more than 1 year maintained remission at 7.5 months [19].
Sultan Al Rashidi et al. report that as a result of discontinuing IFX in 9 patients (mean period: 55.7 ± 22.8 months) who maintained complete remission after the introduction of IFX, 5 patients (56%) continued or discontinued immunosuppressants at an average of 55.7 ± 22.8 months and were able to maintain remission[20].
In the present study, at least 1 year after withdrawal of IFX, the rate of reintroduction of TNF inhibitors was 0%, the rate of remission of ocular inflammation was 67.7%, and the rate of recurrence of systemic inflammation was 100%. Although the rate of remission of ocular inflammation was similar to that in previous reports, recurrence of extraocular symptoms was observed in all cases. Therefore, withdrawal of IFX should be carefully considered even in patients with long-term remission of ocular inflammation.
Sfikakis et al. retrospectively reviewed 29 patients with intractable uveitis who were in remission with TNF inhibitors, and report a 41% remission rate 3 years after withdrawal of [21]. A comparison of patients with drug-free remission and patients in remission with low-dose azathioprine shows that patients in the drug-free group were significantly younger (26.3 vs. 37.2 years) and had a shorter disease duration at the time of initiation of TNF inhibitors (1.0 vs. 4.2 years). The mean disease duration at the time of initiation of TNF inhibitors in the present study was relatively long, at more than 3 years. The patient with retinal vasculitis detected by FA was 40 years old and had a disease duration of 2.2 years at the time of initiation of TNF inhibitors. Our results confirm the findings of Sfikakis et al. and suggest that a long remission period with IFX is not necessarily associated with remission after withdrawal of IFX.
IFX treatment of extraocular lesions, which recurred in this study, has not been approved in Japan. However, EULAR recommends consideration of the use of TNF inhibitors, as well as colchicine, thalidomide, azathioprine, interferon alpha, and apremilast, for mucocutaneous involvement. As reported in previous studies, IFX may be effective not only for uveitis but also for extraocular lesions by systemic inhibition of TNF [6]. Recently, Keino et al. conducted a retrospective study on four patients who discontinued IFX and found no ocular inflammatory attacks in 56 months without its reintroduction [22]. However, two of those patients had oral ulcers and fever after the discontinuation of IFX. Their findings, as well as those of this prospective study, suggest that IFX may be effective for extraocular manifestations and that the risk of extraocular manifestations being affected by its discontinuation must be considered.
Although switching to CYA was adopted to maintain ocular remission in this study, CYA had to be reduced due to liver and renal dysfunction, and the extraocular symptoms recurred in all three patients. Relapsed extraocular symptoms were mild in all cases and did not require reintroduction of biologics. In the future, when planning an IFX discontinuation study, it will be necessary to determine the criteria for IFX reintroduction in the event of extraocular symptoms. Thus, extraocular symptoms should also be considered in the choice of alternative treatments for IFX withdrawal.
This study has several limitations. It was a single-center study as well as a short-term report. The small number of cases enrolled in this study is a major limitation in investigating the impact of IFX discontinuation on ocular lesions. However, the findings of this first prospective study regarding the withdrawal of IFX and switching to CYA for refractory BD uveitis with long-term remission may be significant. Further studies and long-term observations will be needed to establish the criteria for withdrawal of IFX in patients with BD uveitis.
Although no ocular attacks occurred for at least one year after IFX withdrawal, extraocular lesions occurred in all patients, so a TNF inhibitor was reintroduced in one patient. This prospective study indicates that IFX withdrawal should be considered carefully, even in patients who maintain long remission of ocular and extraocular lesions with IFX treatment.
References
International Team for the Revision of the International Criteria for Behçet’s Disease (ITR-ICBD). The international criteria for Behcet’s disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28:338–47.
Sakane T, Takeno M, Suzuki N, Inaba G. Behcet’s disease. N Engl J Med. 1999;341:1284–91.
Nussenblatt RB. Uveitis in Behcet’s disease. Int Rev Immunol. 1997;14:67–79.
Mishima S, Masuda K, Izawa Y, Mochizuki M, Namba K. The eighth Frederick H. Verhoeff Lecture. presented by saiichi mishima, MD Behcet’s disease in Japan: ophthalmologic aspects. Trans Am Ophthalmol Soc. 1979;77:225–79.
Evereklioglu C. Current concepts in the etiology and treatment of Behcet disease. Surv Ophthalmol. 2005;50:297–350.
Hatemi G, Christensen R, Bang D, Bodaghi B, Celik AF, Fortune F, et al. 2018 update of the EULAR recommendations for the management of Behcet’s syndrome. Ann Rheum Dis. 2018;77:808–18.
Saravanan V, Hamilton J. Advances in the treatment of rheumatoid arthritis: old versus new therapies. Expert Opin Pharmacother. 2002;3:845–56.
Evereklioglu C, Er H, Turkoz Y, Cekmen M. Serum levels of TNF-alpha, sIL-2R, IL-6, and IL-8 are increased and associated with elevated lipid peroxidation in patients with Behcet’s disease. Mediators Inflamm. 2002;11:87–93.
Sayarlioglu M, Cinal A, Topcu N, Demirok A. Effect of infliximab on refractory uveitis in Behcet’s disease. Ann Pharmacother. 2004;38:901–2.
Goossens PH, Verburg RJ, Breedveld FC. Remission of Behcet’s syndrome with tumour necrosis factor alpha blocking therapy. Ann Rheum Dis. 2001;60:637.
Sfikakis PP. Behcet’s disease: a new target for anti-tumour necrosis factor treatment. Ann Rheum Dis. 2002;61(Suppl 2):ii51–3.
Sfikakis PP, Theodossiadis PG, Katsiari CG, Kaklamanis P, Markomichelakis NN. Effect of infliximab on sight-threatening panuveitis in Behcet’s disease. Lancet. 2001;358:295–6.
Ohno S, Nakamura S, Hori S, Shimakawa M, Kawashima H, Mochizuki M, et al. Efficacy, safety, and pharmacokinetics of multiple administration of infliximab in Behcet’s disease with refractory uveoretinitis. J Rheumatol. 2004;31:1362–8.
Ohno S, Umebayashi I, Matsukawa M, Goto T, Yano T. Safety and efficacy of infliximab in the treatment of refractory uveoretinitis in Behcet’s disease: a large-scale, long-term postmarketing surveillance in Japan. Arthritis Res Ther. 2019;21:2.
Sfikakis PP. The first decade of biologic TNF antagonists in clinical practice: lessons learned, unresolved issues and future directions. Curr Dir Autoimmun. 2010;11:180–210.
Kaburaki T, Namba K, Sonoda KH, Kezuka T, Keino H, Fukuhara T, et al. Behcet’s disease ocular attack score 24: evaluation of ocular disease activity before and after initiation of infliximab. Jpn J Ophthalmol. 2014;58:120–30.
Niccoli L, Nannini C, Benucci M, Chindamo D, Cassara E, Salvarani C, et al. Long-term efficacy of infliximab in refractory posterior uveitis of Behcet’s disease: a 24-month follow-up study. Rheumatology (Oxford). 2007;46:1161–4.
Kawaguchi T, Kawazoe Y, Kamoi K, Miyanaga M, Takase H, Sugita S, et al. Clinical course of patients with Behcet’s uveitis following discontinuation of infliximab therapy. Jpn J Ophthalmol. 2014;58:75–80.
Adan A, Hernandez V, Ortiz S, Molina JJ, Pelegrin L, Espinosa G, et al. Effects of infliximab in the treatment of refractory posterior uveitis of Behcet’s disease after withdrawal of infusions. Int Ophthalmol. 2010;30:577–81.
Al Rashidi S, Al Fawaz A, Kangave D, Abu El-Asrar AM. Long-term clinical outcomes in patients with refractory uveitis associated with Behcet disease treated with infliximab. Ocul Immunol Inflamm. 2013;21:468–74.
Sfikakis PP, Arida A, Panopoulos S, Fragiadaki K, Pentazos G, Laskari K, et al. Brief report: drug-free long-term remission in severe Behcet’s disease following withdrawal of successful anti-tumor necrosis factor treatment. Arthritis Rheumatol. 2017;69:2380–5.
Keino H, Watanabe T, Nakayama M, Komagata Y, Fukuoka K, Okada AA. Long-term efficacy of early infliximab-induced remission for refractory uveoretinitis associated with Behçet’s disease. Br J Ophthalmol. 2020. https://doi.org/10.1136/bjophthalmol-2020-316892.
Acknowledgements
This work was supported by the JSPS under Grant 17K11428; the Ministry of Health, Labor and Welfare, Japan under Grant H29-Nanchi-Ippan-050.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y. Ida, None; M. Takeuchi, None; M. Ishihara, None; E. Shibuya, None; T. Yamane, None; Y. Hasumi, None; S. Kawano, None; I. Kimura, None; N. Mizuki, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Masaki Takeuchi
About this article
Cite this article
Ida, Y., Takeuchi, M., Ishihara, M. et al. An open-label, prospective, single-arm study of switching from infliximab to cyclosporine for refractory uveitis in patients with Behçet’s disease in long-term remission. Jpn J Ophthalmol 65, 843–848 (2021). https://doi.org/10.1007/s10384-021-00872-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00872-2