Abstract
Objectives
The aim of the study is to analyze the ALS disease progression and respiratory function of Italian patients treated with edaravone (EVN), as well as the adherence to, and the effects of, the therapy.
Methods
We performed an observational study of patients treated with EVN from May 2017 to May 2019, in 39 Italian ALS Centers. Taking into account ALS patients with at least 12 months of EVN treatment, we compared the decline of ALSFRS-R and FVC with a group of matched historical controls from the Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) database, using both descriptive and survival analysis approaches.
Results
A total of 331 ALS Italian patients treated with EVN and 290 matched historical controls were recruited in this study. No significant differences on disease progression or respiratory function were found comparing the two cohorts in both descriptive and survival analyses. The EVN treatment was overall well tolerated.
Conclusions
The study showed that EVN treatment was well tolerated. No significant differences were reported in ALS patients treated and not treated with EVN, in terms of both disease progression and respiratory function. These findings prove that further studies are required to better clarify whether EVN could be considered an effective treatment for ALS disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An urgent unmet need persists for effective therapies significantly improving disease progression, survival, and/or quality of life in amyotrophic lateral sclerosis (ALS).
Edaravone (EVN) phase II study showed that in the group treated with 60 mg/day, there was a significant lower decline of ALSFRS score in the 6 months of treatment. A phase III clinical trial suggested no significant effects in ALS, although there was a trend towards slower disease progression in patients taking the drug [1]. A post hoc analysis was performed in a subgroup of patients with the following findings: % forced vital capacity (FVC) of ≥ 80%, ≥ 2 points for all item scores in the ALS Functional Rating Scale-Revised (ALSFRS-R) score before treatment, a diagnosis of ‘definite’ or ‘probable ALS according to the El Escorial revised diagnostic criteria (EEC) and onset of disease within 2 years. The results showed a significant reduction in the ALSFRS-R score decline in patients treated with EVN [2]. Subsequently, a double-blind trial (MCI-186-J19) showed a slowing of disease progression over the 24-week treatment period in patients of this specific subgroup [3]. Based on these results, the drug was approved for ALS in Japan and in the United States. Unfortunately, the only available data about the effects of the EVN on disease progression are limited to one small clinical trial [2] and the scientific community raised some questions about its real effect [4].
The aim of this study was to evaluate data in a “real world” context about the safety and the adherence to the EVN treatment of patients that was treated in different Italian Regions. Moreover, we evaluated the effect of EVN on disease progression, respiratory function, and survival comparing these patients with those extracted from the Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) database [5].
Patients and methods
All the patients included in the study fulfilled the MCI-186-J19 criteria (Table 1) such as a diagnosis of a clinically “probable” or “definite” ALS according to revised El Escorial Criteria, an age equal to or greater than, 18 years old, an FVC% equal or more than 80% predicted normal value for gender, height, and age in seated position at the screening visit, a score ≥ 2 in all items of ALSFRS-R at the screening visit, a disease duration from symptoms onset no longer than 24 months, and a decrease in the ALSFRS-R score of 1–4 during a 12-week observation period between the screening and the baseline. Otherwise, the exclusion criteria for the EVN treatment included concomitant significant neurological or neurodegenerative disease, concomitant significant disease in other systems or organs, creatine clearance lower than 50 mL/min, women who are pregnant or breastfeeding, and patients who do not understand or provide an informed consent.
Study design
We collected data of 331 ALS patients treated with EVN (EDARAV-ALS cohort). The study was approved by the local ethical committees of participating centers. All subjects signed an approved Informed Consent Form after receiving detailed written and verbal information about the reason, the nature, the required procedures, the intended duration, and the possible risks and benefits and any discomfort associated with the study. The informed consent procedure was in according to the guidelines provided in the Declaration of Helsinki and the ICH E6 Guideline for Good Clinical Practice [6].
To compare the disease progression of patients treated and not treated with EVN, a matched PRO-ACT cohort with the same inclusion and exclusion criteria of the EDARAV-ALS cohort (n = 290) was extrapolated [5]. This is a useful tool for investigators interested in ALS clinical research and is a useful publicly available repository of longitudinal ALS data (https://nctu.partners.org/ProACT/).
The disease progression was analyzed by both descriptive and survival analysis.
Objectives
The objectives of this observational study could be summarized as follows:
-
1.
To assess whether the disease progression, quarterly measured through ALSFRS-R, is different between the EDARAV-ALS and PRO-ACT cohorts [5];
-
2.
To assess whether the decline of the FVC% score, quarterly measured, is different between the EDARAV-ALS and PRO-ACT cohorts;
-
3.
To assess whether EVN improves the survival time until the D-50 (defined as the time point when ALSFRS-R drops to 24 [7]), or the time to reach the 60% of the FVC, comparing the two cohorts of EDARAV-ALS and PRO-ACT;
-
4.
To assess the EVN safety and tolerability in a long-term period (48 weeks), taking into account the following variables: adverse events (AEs) occurrence and arising changes in physical examination due to treatment, vital signs (blood pressure, pulse rate, and body temperature), body weight, and clinical laboratory tests (biochemistry and hematology).
The following clinical data were collected: age at the start of treatment; sex; date of symptoms onset; type of onset (bulbar or spinal); El Escorial revised diagnostic criteria at the start of treatment; date of treatment start; number of treatment cycles; ALSFRS-R at treatment beginning and at each follow-up visit; disease progression rate (ΔFS),Footnote 1 considered as categorical variable stratified using Kimura et al. [8] criteria; FVC% at the start of treatment and at each follow-up visit; date of interruption of the treatment; reason for the interruption of the treatment; date of death.
Statistical analysis
ALSFRS-R and FVC measures were quarterly extracted during 1-year follow-up, achieving a total of five time points. Changes in ALSFRS-R total score and FVC % were calculated as the difference between the baseline value and each time point’s value.
Disease progression and survival analysis were performed in accordance with the intention-to-treat principle, considering patients with at least one follow-up visit in addition to the baseline visit (n = 197 for the EDARAV-ALS group and n = 290 for the PRO-ACT cohort).
For each variable, Shapiro–Wilk test and Levene’s test were used to evaluate the normality of the distribution and the homogeneity of the variance, respectively. Data were summarized using median and interquartile range for continuous variables. Wilcoxon rank sum test and Chi-square test were used to assess the differences in demographic and clinical features between EDARAV-ALS and PRO-ACT cohorts at baseline. Wilcoxon rank sum test was used to compare the difference in changes in both ALSFRSr total score and FVC% between the two groups.
Moreover, comparing the EDARAV-ALS and PRO-ACT cohorts, Chi-square test and Wilcoxon rank sum test were used to analyze the proportion of patients who reached the D-50 (for the ALSFRSr total score), the 60% FVC, and the time between the first visit and the achievement of D-50 or 60% FVC.
Finally, a survival analysis was performed, with a follow-up from the first ALS symptoms to D-50 and/or 60% FVC. Patients who died or who did not reach the milestones by the end of the 1-year follow-up period were considered as censored at the end of the follow-up. Survival curves between the two groups were estimated by the Kaplan–Meier analysis and were compared using the log-rank test. Multivariable Cox proportional hazard regression model was used to analyze the survival effect of the EVN treatment, adjusted for age, sex, site of onset, diagnostic delay, and ΔFS. Effect size was expressed in hazard ratio (with 95% confidence interval). These two outcomes, derived from ALSFRS-R and FVC, were chosen because of the floor effect of the ALS disease at the end of its trajectory, and because of the lack of information about date of tracheostomy in the PRO-ACT database.
All tests were two-tailed, and a p value < 0.05 was considered as statistically significant.
Numbers and percentages of side effects related to the treatment were reported, considering also the patients who reported only the baseline visit (n = 331).
The analyses were performed by two biostatisticians of two different ALS Centers, using common criteria and independent scripts, wrote using SAS version 9.3 (SAS Institute, Inc, Cary, NC, USA) and STATA version 13.1 (StataCorp, College Station, TX, USA).
Protocol approval
The study was approved by the ethical committee of each center. Patients signed a written informed consent.
Data availability statement
Data will be available upon request by interested researchers.
Results
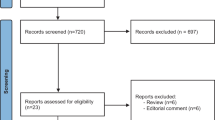
A total of 331 ALS patients treated with EVN between May 2017 and May 2019 in 39 ALS Italian Centers were collected for this study; a descriptive analysis of treated patients is reported in Table 2.
In the survival analysis, we excluded 134 patients due to incomplete data at follow-up; therefore, only 197 ALS patients were considered.
Baseline clinical features of EDARAV-ALS and PRO-ACT cohorts are reported in Table 3. No statistical significant differences emerged from the analysis, except for the age at the beginning of the treatment/first evaluation—which was significantly lower in the PRO-ACT group (60 years [54.0–68.0] for EDARAV-ALS cohort vs 55 years [47.5–63.0] for the PRO-ACT cohort; p < 0.01)—and for the ΔFS for which we found a significantly higher proportion of fast progressors’ patients in the PRO-ACT group.
To clearly articulate findings, the results section will be structured following the objectives of the study (see above).
Comparison between patients treated vs. not treated with EVN, using ALSFRS-R and FVC scores (objectives 1 and 2)
There were no significant differences between EDARAV-ALS and PRO-ACT cohorts in any of the five time points, except for the difference between baseline and T3, and between baseline and T6 for both the ALSFRSr and the FVC%, in which the scores were significantly higher in the PRO-ACT (Fig. 1).
No significant differences emerged considering the proportion of patients that reached the D-50 and of patients that reached the 60% FVC, between the two cohorts. During the 1-year follow-up period, the D-50 was reached by 46 patients (23.3%) in the EDARAV-ALS cohort and by 62 patients (21.4%) in the PRO-ACT cohort (p = 0.61). Similar results were obtained considering the 60% FVC as event, reached by 51 patients (25.9%) in the EDARAV-ALS group and by 68 patients (23.45%) in the PRO-ACT group (p = 0.54). For both events, the differences in proportions between the two cohorts are represented in Fig. 2.
Moreover, no significant differences were reported as far as the interval between time of the first evaluation and time of reaching D-50 (6 months [6.0–9.0] vs 7 months [5.0–9.0], p = 0.98), or 60% FVC (6 months [3.0–6.0] vs 6 months [3.0–9.0], p = 0.76).
Survival analysis for EVN treated vs. not treated patients, from ALS onset to D-50 and/or time to reach 60% FVC (objective 3)
No significant differences were found regarding survival among the two groups, considering both the end points: D-50 (log-rank p = 0.94) and 60% FVC (log-rank p = 0.77) (Fig. 3). These results were confirmed also in the multivariable Cox proportional hazard model (HR = 1.40; 95% CI = 0.81–2.41, p = 0.23 considering D-50 as endpoint, and HR = 1.42; 95% CI = 0.88–2.29, p = 0.15 considering 60% FVC as endpoint).
Table 4 summarizes the aforementioned results, in accordance with the three objective sessions.
EVN safety and tolerability in a long-term period (objective 4)
Side effects were collected for all the patients who received at least one dose of the treatment (n = 331). A qualitative analysis revealed that EVN was generally well tolerated. The adverse events were similar to those reported in the EVN literature. In particular, we recorded six cases of nephrotic syndrome and four cases of deep venous thrombosis. Minor adverse events included mild dizziness (four cases) and burning sensation at the injection site (five cases). No remarkable events were observed after interruption of treatment.
Twenty-two patients voluntarily suspended the treatment after approximately 6 months due to lack of effects and to the burdensome treatment in terms of duration and route of administration.
Discussion
In this observational study, EVN resulted to be overall well tolerated, without significant adverse events, in keeping with the previous studies performed in Japan, Europe, and South Korea [1,2,3, 9, 10].
Although, in Italy, the treatment with EVN was allowed in ALS patients with the specific clinical findings of the MCI-186-J19 trial, our multi-centre analysis did not show a positive effects of EVN on ALS progression [1,2,3] found in the previous studies: a trend towards slower disease progression in the patients taking the drug in the phase III clinical trial [1], a significant reduction in the ALSFRS-R score decline in patients treated with EVN compared to those treated with placebo in a post hoc analysis performed in a subgroup of patients [2], a statistically significant slowing of disease progression over the 24-week treatment period in patients of this specific subgroup taking EVN in a double-blind trial [3]. Also the limited improvement in a more advanced stage of ALS shown in a Korean observational study [10], which considered 22 patients treated with EVN, was not observed in our study.
Our results confirm the findings of an Italian retrospective study, conducted by Fortuna et al. [9], performed right after July 2017, when Edaravone was formally admitted as compassionate therapy for ALS by the Italian Medicines Agency (AIFA). The study recruited 31 consecutive patients with ALS treated with EVN in the Motor Neuron Disease Clinic of the University of Padova (Italy), and showed no significant effects on disease progression.
The higher number of patients recruited in our study (n = 331), compared to the previous studies on this topic, represents an important strength. This was possible thanks to a huge effort on data collection and an excellent coordination among several ALS Academic and non-Academic centres located all over Italy.
Among the main limitations of this study, some important considerations need to be addressed-R. Since there was not a parallel control group, a cohort of controls was extrapolated by PRO-ACT database, including only patients with the same inclusion and exclusion criteria of the EDARAV-ALS cohort. This represents the main limitation of the study, even considering only patients monitored by the revised ALSFRS-R measures. To minimize this possible selection bias, the analysis was performed using two different approaches, each one with pros and cons. The descriptive analysis proposed for the first and second objectives represents a clear and efficient way of comparing the ALS disease progression between EDARAV-ALS and PRO-ACT groups. Nevertheless, this approach could be affected by a selection bias due to the exclusion of ALS patients for whom ALS measures were collected out of the quarter time windows.
For this reason, we performed also a survival analysis up to the D-50 for both EDARAV-ALS and PRO-ACT groups. The strength of this approach is to consider all ALSFRS-R collected for both groups, avoiding the possible selection bias of the quarterly-time windows analysis. Nevertheless, this approach could be still biased because of the different time intervals among the ALSFRS-R measures between the two groups (20 days for PRO-ACT and 35 days for EDARAV-ALS group). Anyhow, it is reasonable to assume that the different time-interval gradients between the two groups of subjects were not so relevant in the light of negative findings resulted from the analysis.
The two approaches did not show significant differences among the two groups in terms of disease progression, with findings very similar to each other, proving that we need further studies, in a placebo-controlled setting, to well clarify whether EVN could be considered an efficacious treatment for ALS disease.
This study showed data in a “real world” context about the safety, the adherence to the therapy, and its effect on the disease progression and respiratory function in patients treated with EVN, administered intravenously, in Italy. Compared to all previous studies on EVN effectiveness, this study involved the largest number of patients (331).
The treatment was overall well tolerated, but no significant differences in disease progression and respiratory functions were observed between the two cohorts of ALS patients treated and not treated with EVN.
Additional large studies with longer follow-up should be performed to further assess the effectiveness of this treatment among “real world” ALS patients focusing as well on determination of its long-term effects.
Data availability
Data will be available upon request by interested researchers. The sponsor organizations had no role in data collection and analysis and did not participate to writing and approving the manuscript. The information reported in the manuscript has never been reported elsewhere.
Notes
- $$\Delta \text{FS}=\frac{48-\text{ALSFRS}-\text{R}\,\, \text{at}\,\,\text{start}\,\, \text{of}\,\,\text{treatment}}{\text{start}\,\,\text{date}\,\,\text{of}\,\,\text{treatment}-\text{date}\,\, \text{of}\,\,\text{onset}\,\, (\text{month})}.$$
References
Abe K, Itoyama Y et al (2014) Confirmatory double-blind, parallel-group, placebo-controlled study of efficacy and safety of Edaravone (MCI-186) in amyotrophic lateral sclerosis patients. Amyotroph Lateral Scler Frontotemporal Degener 15:610–617
Edaravone (MCI-186) ALS 16 Study Group (2017) A post-hoc subgroup analysis of outcomes in the first phase III clinical study of edaravone (MCI-186) in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 18:11–19
Akimoto M, Nakamura K, Writing Group on behalf of the Edaravone (MCI-186) ALS 19 Study Group ( 2017) Edaravone for treatment of early-stage ALS. Lancet Neurol 16:772
Al-Chalabi A, Andersen PM et al (2017) ENCALS statement on edaravone. Amyotroph Lateral Scler Frontotemporal Degener 18:471–474
Atassi N, Berry J, Shui A, Zach N, Sherman A, Sinani E et al (2014) The PRO-ACT database: design, initial analyses, and predictive features. Neurology 83:1719–1725
Singh J (2015) International conference on harmonization of technical requirements for registration of pharmaceuticals for human use. J Pharmacol Pharmacother 6(3):185–187. https://doi.org/10.4103/0976-500X.162004
Stubendorff B, Grehl T, Neuwirth C, Rödiger A, Gunkel A, Radscheidt M et al (2017) P 48 The time of the ALSFRS-R to decrease to 50% (D50) in a sigmoidal decay model sufficiently describes the complete disease course of amyotrophic lateral sclerosis. Clin Neurophysiol 128(10):e353–e354
Kimura F, Fujimura C, Ishida S, Nakajima H, Furutama D, Uehara H, Shinoda K, Sugino M, Hanafusa T (2006) Progression rate of ALSFRS-R at time of diagnosis predicts survival time in ALS. Neurology 66(2):265–267. https://doi.org/10.1212/01.wnl.0000194316.91908.8a
Fortuna A, Gizzi M, Bello L, Martinelli I, Bertolin C, Pegoraro E, Corbetta M, Sorarù G, Edaravone Study Group (2019) Safety and efficacy of edaravone compared to historical controls in patients with amyotrophic lateral sclerosis from North-Eastern Italy. J Neurol Sci 404:47–51
Park JM, Kim SY, Park D, Park JS (2020) Effect of edaravone therapy in Korean amyotrophic lateral sclerosis (ALS) patients. Neurol Sci 41(1):119–123
Acknowledgements
We thank all the patients and their caregiver for the support in the collection of data, all the nurses for their essential support in the intravenous drug administration, and the hospital pharmacists in the Edaravone supply. We are grateful with “Io corro con Giovanni” association for their support. We are also grateful to Pooled Resource Open-Access ALS Clinical Trials (PRO-ACT) database for data used in the preparation of this article. As such, the following organizations and individuals within the PRO-ACT Consortium contributed to the design and implementation of the PRO-ACT database and/or provided data, but did not participate in the analysis of the data or the writing of this report: Neurological Clinical Research Institute, MGH; Northeast ALS Consortium; Novartis; Prize4Life; Regeneron Pharmaceuticals, Inc; Sanofi; Teva Pharmaceutical Industries, Ltd. The authors thank Dr Salvatore Stano, Dr GianMarco Milella, Dr Isabella Paolino, Dr Maurizio Grassano, Dr Alessandro Bombaci, Dr Luca Solero, Dr Margherita Daviddi, Dr Francesca Palumbo, Dr Maria Claudia Torrieri for their support. The members of the EDARAV-ALS Study Group Liana Africa MD, Nicoletta De Angelis (Department of Medical and Surgery Sciences and Neurosciences, University of Siena, Siena, Italy); Stefania Angelocola MD, Patrizio Cardinali MD (Neurology Unit, Murri Hospital of Fermo, ASUR Marche, Italy); Paolo Barone MD PhD (ALS Center, Operative Unit of Neurology, AOU “San Giovanni di Dio e Ruggi d’Aragona”, Salerno, Italy); Virginio Bonito MD (Neurology Unit, ASST Papa Giovanni XXIII, Bergamo, Italy); Giuseppe Borghero MD (Neurologic Unit, Monserrato University Hospital, Cagliari University, Cagliari, Italy); Corrado Cabona MD (Department of Neurosciences, Rehabilitation Ophtalmology, Genetics, Mother and child disease, IRCCS Ospedale Policlinico San Martino Genova, Italy); Elena Canali MD (Neurology Unit, Azienda Ospedaliera Arcispedale Santa Maria Nuova, IRCCS, Reggio Emilia, Italy); Antonio Canosa MD PhD, Giuseppe Fuda MS, Umberto Manera MD, Paolina Salamone MS PhD, Rosario Vasta MD (ALS Centre, “Rita Levi Montalcini” Department of Neuroscience, University of Turin, Turin, Italy); Margherita Capasso MD (Unit of Neurology, Ospedale Clinicizzato SS Annunziata, Chieti, Italy); Cecilia Carlesi MD (Neurology Unit, Azienda USL Toscana Nord Ovest, Versilia Hospital, Lido di Camaiore, Lucca, Italy); Mario Casmiro MD (ALS Center, Department of Neurology, Faenza and Ravenna Hospital, Ravenna, Italy); Mauro Ceroni MD, Luca Diamanti MD (Department of Brain and Behavioral Sciences, University of Pavia; Istituto Nazionale Neurologico Fond IRCCS Mondino Pavia, Italy); Amelia Conte MD (IRCCS Foundation Policlinico A. Gemelli, Rome, Italy; NEMO Clinical Center Roma, Fondazione Serena Onlus-Pol. A. Gemelli, Rome, Italy); Eleonora Dalla Bella MD, Giuseppe Lauria MD (3rd Neurology Unit, Motor Neuron Diseases Centre, Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan, Italy Department of Biomedical and Clinical Sciences Luigi Sacco, University of Milan, Milan, Italy); Fabiola De Marchi MD (ALS Centre, Neurologic Clinic, University Hospital “Maggiore della Carità”, Novara, Italy); Massimiliano Filosto MD PhD, Alessandro Padovani MD PhD (Center for Neuromuscular Diseases ERN-EURO NMD Center, Unit of Neurology, ASST “Spedali Civili” and University of Brescia, Italy); Valeria Ada Sansone MD PhD, Francesca Gerardi MS (NEMO Clinical Center Milano, Fondazione Serena Onlus, Milan, Italy; Neurorehabilitation Unit, University of Milan, Italy); Carlo Guidi MD (Neurology Unit of Forlì, AUSL Romagna, Italy); Maurizio Inghilleri MD PhD (ALS Center, Department of Human Neuroscience, Sapienza University, Rome, Italy); Vincenzo La Bella MD (ALS Clinical Research Center, Department of Biomedicine, Neuroscience and Advanced Diagnostics, University of Palermo, Palermo, Italy); Giancarlo Logroscino MD PhD (Department of Basic Medical Sciences, Neuroscience and Sense Organs, University of Bari Aldo Moro, Bari; Center for Neurodegenerative Diseases and the Aging Brain, Department of Clinical Research in Neurology, University of Bari Aldo Moro, Pia Fondazione Cardinale G Panico, Tricase, Italy); Francesca Lupidi MD (Neurological Clinic, AOU Ospedali Riuniti of Ancona, Ancona, Italy); Jessica Mandrioli MD, Elisabetta Zucchi (Department of Neurosciences, Ospedale Civile S. Agostino Estense, Azienda Ospedaliero-Universitaria di Modena, Modena, Italy); Sonia Messina MD PhD (NEMO Sud Clinical Center, Fondazione Aurora, Messina, Italy); Maria Rosaria Monsurrò MD, Gioacchino Tedeschi MD PhD (University of Campania “Luigi Vanvitelli”, Department of Advanced Medical and Surgical Sciences, Naples, Italy); Gabriele Mora MD (Department of Neurorehabilitation, Istituti Clinici Scientifici Maugeri IRCCS, Institute of Milan, Milan, Italy); Cecilia Nozzoli MD (Operative Unit of Neurology, Ospedale Perrino, Brindisi, Italy); Francesco Patti MD PhD (Department “GF Ingrassia” Section of Neuroscience, University of Catania, Catania, Italy); Massimiliano Plastino MD UOC Neurology/Stroke Unit “S. Giovanni di Dio” Hospital, Crotone, Italy); Nilo Riva MD PhD (Department of Neurology and Clinical Neurophysiology, IRCCS “San Raffaele Scientific Institute”, Milan, Italy); Massimo Russo MD (Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy); Lucio Santoro MD PhD (Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples Federico II, Naples, Italy); Gaspare Scaglione MD (Department of Medical Sciences and Neuroscience, University “Aldo Moro” of Bari, Policlinic, Bari, Italy); Elisabetta Sette MD, Valeria Tugnoli MD UOC (Neurologia, D.A.I. Neuroscienze Riabilitazione, AOU Ferrara, Ferrara, Italy); Vincenzo Silani MD, Nicola Ticozzi MD PhD (Department of Pathophysiology and Transplantation, “Dino Ferrari” Center, Università degli Studi di Milano, Milan, Italy; Istituto Auxologico Italiano IRCCS, Milan, Italy); Costanza Simoncini MD PhD (Neurological Clinic, Department of clinical and Experimental Medicine, University Hospital of Pisa, Pisa, Italy); Rossella Spataro MD PhD (IRCCS Centro Neurolesi Bonino Pulejo, Palermo, Italy); Raffaella Tanel MD, (Operative Unit of Neurology, S. Chiara Hospital, Trento, Italy); Maria Claudia Trapasso MD, Lucia Zinno MD (Dipartimento di Medicina Generale e Specialistica, Neurology Unit, AOU of Parma, Parma, Italy); Lucio Tremolizzo MD PhD (Neurology Unit, San Gerardo Hospital Monza, University of Milano Bicocca, Monza, Italy); Paolo Volanti MD (Neurorehabilitation Unit, ALS Center, Istituti Clinici Scientifici (ICS) Maugeri, Mistretta (ME), Italy).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
All those listed as authors fulfill the authorship criteria. Study concept and design: CL, CM, and AC. Acquisition of data: CL, CM, LA, SA, PB, VB, GB, PB, CC, EC, AC, MC, CC, PC, CC, MC, MC, AC, EDB, NDA, FDM, LD, RD, MF, MF, FG, FG, CG, MI, VLB, GL, FL, UM, SM, LM, SM, MRM, CN, AP, MP, NR, MR, MS, VAS, LS, GS, ES, GS, CS, ILS, GS, RS, RT, GT, AT, MCT, FT, VT, RV, MV, PV, LZ, and EZ. Analysis and interpretation of data: CL, CM, AL, FDO, MF, and AC. Drafting of the manuscript: CL, CM, AL, FDO, MP, and AC. Critical revision of the manuscript for important intellectual content: CL, CM, AL, FDO, AC, MF, GL, GM, FP, VS, LT, and NT. Obtained funding: NA. Administrative, technical, and material support: CL, CM, AL, FDO, AC, UM, PS, GF, and FG. Study supervision: CL, CM, AL, FDO, MF, and AC.
Corresponding author
Ethics declarations
Conflicts of interest
Christian Lunetta served as scientific consultant for Mitsubishi Tanabe Pharma Europe, Cytokinetics, Neuraltus, and Italfarmaco, and has received funds from ARISLA and Ministry of Health (CCM2011). Andrea Calvo has received a research grant from Cytokinetics. Jessica Mandrioli served on a scientific advisory board for Biogen and Italfarmaco, and has received research funding from ARISLA, AIFA, Emilia Romagna Region, and Ministry of Health. Vincenzo Silani is in the Editorial Board of Amyotroph Lateral Sclerosis, European Neurology, American Journal of Neurodegenerative Diseases, Frontiers in Neurology; received compensation for consulting services and/or speaking activities from AveXis, Cytokinetics, Italfarmaco, and Zambon, and receives research supports from the Italian Ministry of Health (Grant RF-201302355764), Fondazione Regione per la Ricerca Biomedica Regione Lombardia (Project nr. 2015-0023), and E-RARE JTC 2018 (Project Repetomics). Liana Africa, Stefania Angelocola, Paolo Barone, Virginio Bonito, Giuseppe Borghero, Paolo Bortolotti, Corrado Cabona, Elena Canali, Antonio Canosa, Margherita Capasso, Claudia Caponnetto, Patrizio Cardinali, Cecilia Carlesi, Mario Casmiro, Mauro Ceroni, Amelia Conte, Eleonora Dalla Bella, Fabiola De Marchi, Nicoletta De Angelis, Luca Diamanti, Raffaele Dubbioso, Massimo Filippi, Massimiliano Filosto, Giuseppe Fuda, Francesca Gerardi, Fabio Giannini, Carlo Guidi, Maurizio Inghilleri, Vincenzo LaBella, Giuseppe Lauria, Giancarlo Logroscino, Francesca Lupidi, Umberto Manera, Sabrina Matà, Letizia Mazzini, Sonia Messina, Maria Rosaria Monsurrò, Gabriele Mora, Cecilia Nozzoli, Alessandro Padovani, Francesco Patti, Massimiliano Plastino, Nilo Riva, Massimo Russo, Mario Sabatelli, Paolina Salamone, Valeria Ada Sansone, Lucio Santoro, Gaspare Scaglione, Elisabetta Sette, Gabriele Siciliano, Vincenzo Silani, Costanza Simoncini, Isabella Laura Simone, Gianni Sorarù, Rossella Spataro, Raffaella Tanel, Gioacchino Tedeschi, Nicola Ticozzi, Antonella Toriello, Maria Claudia Trapasso, Lucio Tremolizzo, Francesca Trojsi, Valeria Tugnoli, Rosario Vasta, Marcella Vedovello, Paolo Volanti, Lucia Zinno, Elisabetta Zucchi, and Fabrizio D’Ovidio: no disclosures.
Ethical approval
The study was approved by the ethical committee of each centres. Patients signed a written informed consent. All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Patients signed a written informed consent.
Consent for publication
All authors have given final approval of the version of the manuscript to be submitted. Each author takes public responsibility for appropriate portions of the content and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Additional information
The members of the EDARAV-ALS Study Group are listed in acknowledgements.
Rights and permissions
About this article
Cite this article
Lunetta, C., Moglia, C., Lizio, A. et al. The Italian multicenter experience with edaravone in amyotrophic lateral sclerosis. J Neurol 267, 3258–3267 (2020). https://doi.org/10.1007/s00415-020-09993-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09993-z