Abstract
Background
Abnormal vestibular function has been reported in patients with vestibular migraine (VM). However, it is unclear whether the proportion of patients with vestibular dysfunction differs between the diagnoses of VM and probable VM (PVM).
Methods
We reviewed the medical records of 1736 patients who underwent cervical vestibular-evoked myogenic potential testing to air-conducted sound (ACS cVEMP), ocular VEMP testing to bone-conducted vibration (BCV oVEMP), and caloric testing. We used the diagnostic criteria for VM provided in the appendix of the International Classification of Headache Disorders 3 Beta, and the diagnostic criteria consensus published by the Barany Society and the International Headache Society for PVM. Twenty-two VM patients and a further 22 PVM patients were included. Binomial logistic regression analyses were performed to see whether the subjects’ age, sex, or the diagnostic certainty of VM (i.e., VM vs. PVM) have an association with the presence of vestibular dysfunction.
Results
There was no significant association between the diagnostic certainty of VM and abnormality in caloric or ACS cVEMP testing. On the other hand, VM had a significant positive association with abnormality in BCV oVEMPs compared with PVM.
Conclusion
VM is associated with dysfunction of the utriculo-ocular pathway more frequently than PVM, suggesting that the pathophysiology of VM involves the utriculo-ocular pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been well documented that patients experiencing migraine show symptoms of vertigo/dizziness [21, 22]. Vestibular migraine (VM) refers to recurrent vertigo or dizziness caused by migraine and presents with spontaneous or positional vertigo/dizziness that lasts for minutes to days, with migrainous symptoms [30]. In 2012, the International Headache Society Classification Committee and the Committee for Classification of the Barany Society published the first consensus on the diagnostic criteria for VM [23]. VM is described in the appendix of the International Classification of Headache Disorders 3 Beta (ICHD-3β) as a novel disease entity [11]. Taking into consideration the balance between sensitivity and specificity of the diagnostic criteria in establishing the diagnosis for VM, the categories VM and probable vestibular migraine (PVM) were retained. ICHD-3β included only the diagnostic criteria of VM, while the Barany classification included PVM as well as VM. PVM partially meets the diagnostic criteria of VM based on the symptoms of patients (see the Appendix for the diagnostic criteria).
Vestibular dysfunction in VM patients has been demonstrated using caloric testing and video head impulse testing (vHIT) to investigate the function of the semicircular canals (SCC) [2, 4, 8, 9, 13, 14, 20, 32, 34, 35], and cervical and ocular vestibular-evoked myogenic potential (cVEMP and oVEMP) testing for the function of the otolith organs [1, 3, 12, 13, 33, 36, 37]. Another recent study reported that the percentage of migraine among patients with bilateral vestibulopathy (BVP) of unknown cause was significantly higher than that among BVP patients with a definite or probable etiology. These findings suggest an association between migraine and vestibular dysfunction [24].
In the present study, we investigated whether the proportion of vestibular dysfunction differs between patients with VM and PVM. We revealed that patients with VM have dysfunction of the utriculo-ocular pathway (shown by abnormal oVEMPs) more frequently than PVM patients, suggesting that the pathophysiology of VM involves the utriculo-ocular pathway.
Material and methods
Study design
The present study was approved by the Research Ethics Committee, Graduate School of Medicine and Faculty of Medicine, at the University of Tokyo (#2487). The procedures in the present study were performed according to the tenets of the Declaration of Helsinki. Written informed consent was waived, because retrospective data from medical records were used in the present study.
Subjects
We retrospectively reviewed the medical records of 1736 consecutive patients who underwent cVEMP testing to air-conducted sound (ACS cVEMP), oVEMP testing to bone-conducted vibration (BCV oVEMP), and caloric testing between January 2013 and September 2019 at the Balance Disorder Clinic of the University of Tokyo Hospital. Caloric testing has been used to assess the function of the vestibulo-ocular pathway relating to the lateral SCC (LSCC) and superior vestibular nerve. ACS cVEMP testing has been used to assess the function of the sacculo-collic pathway [6, 26, 27] while BCV oVEMP testing has been used to assess the function of the utriculo-ocular pathway [7, 18, 26]. The diagnostic criteria for VM in the ICHD-3β appendix (see Appendix 1) and the agreed diagnostic criteria for PVM published by the Barany Society and the IHS (see Appendix 2) were used in the present study. Patients with co-existing vestibular diseases including Meniere’s disease were not included. Patients with co-existing any other otological or neurological disorders were not included. Patients with impairment of the middle ear transmission system were not included.
Twenty-two patients (4 males and 18 females; age range 16–75 years, mean age ± standard deviation 37.0 ± 14.5 years) met the VM criteria, and 22 patients (4 males and 18 females; age range 13–63 years, mean age ± standard deviation 39.8 ± 12.2 years) met the PVM criteria (Table 1).
ACS cVEMP testing
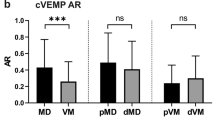
Surface electrodes were placed on the upper half of each sternocleidomastoid muscle (SCM), with a reference electrode on the lateral end of the upper sternum. During recordingm subjects, in a supine position, were asked to raise their heads off the bed to contract the SCM. 500 Hz short tone burst stimuli (135dBSPL, rise/fall time 1 ms, plateau time 2 ms) were presented via headphones at a repetition rate of 5 Hz. Analysis time was 100 ms. The signals were amplified and bandpass-filtered (20–2000 Hz) using Neuropack R (Nihon Kohden Co. Ltd., Tokyo, Japan). After confirming reproducibility with two runs for each ear, the amplitude and latency of the first positive–negative peak (p13–n23) recorded from the side ipsilateral to stimulation was obtained from the average of two responses. The cVEMP asymmetry ratio (AR) was used to evaluate any abnormality in the p13–n23 amplitude [28]. When a reproducible p13–n23 was not observed, it was judged as an absent response. When the cVEMP AR was greater than the normal upper limit, which was set at 34.0% [28], it was judged as a decreased response. A patient who showed absent responses on both sides was regarded as having bilaterally abnormal responses. When the p13 latency was outside the normal range [mean ± 2 standard deviations, 14.9 (± 0.53) ms] [28], it was judged as abnormal. Mean ± standard deviation was 14.9 ± 0.53 ms. When the n1 latency was longer than mean + 2 standard deviation (14.49 + 1.26 ms) [16], it was judged as a prolonged latency.
BCV oVEMP testing
Surface electrodes were placed on the skin 1 cm below the center of each lower eyelid, with a reference electrode on the skin 3 cm below the center of each lower eyelid. While recording EMG activity, the subjects were asked to look up by approximately 30°. The bone-conducted stimuli were 500 Hz tone bursts (rise/fall time 1 ms, plateau time = 2 ms) delivered by a 4810 mini-shaker (Bruel and Kjaer, Naerum, Denmark), which was placed on the forehead in the midline (Fz), with a stimulation repetition rate of 3 Hz. The peak driving voltage was adjusted to 8.0 V which produced a 128 dB peak force level (re: 1 µN). Analysis time was 50 ms. The signal was amplified and bandpass-filtered (0.5–500 Hz) using Neuropack R. After confirming reproducibility with two runs for each ear, the amplitude and latency of the first negative–positive peak (n1–p1) recorded from the side contralateral to stimulation was obtained from the average of two responses. The oVEMP AR was used to evaluate any abnormality of the n1–p1 amplitude [5]. When a reproducible n1–p1 was not observed, it was judged it as absent response. When the oVEMP AR was greater than the normal upper limit, which was set at 27.3% [17], we judged it as decreased response. A patient who showed absent responses on both sides was regarded as having bilaterally abnormal responses. Mean ± standard deviation was 10.4 ± 0.63 ms. When the n1 latency was longer than mean + 2 standard deviation (10.4 + 1.26 ms) [16], it was judged as a prolonged latency.
Caloric testing
Caloric testing was conducted by irrigating the external auditory canal with 2 ml ice water (4 ℃) for 20 s. The induced nystagmus was recorded using electronystagmography in a darkened room. This ice-water caloric testing shows a high sensitivity and specificity for the detection of canal paresis (CP) [31]. An abnormal response was defined by either of the following criteria: (1) CP percentage > 20% for unilaterally abnormal responses [15]; (2) maximum slow phase eye velocity of caloric nystagmus < 10 degrees/s for bilaterally abnormal responses [10].
Data analysis
Data are expressed as the mean ± standard deviation. Statistical analyses were performed using SAS software version 9.4 (SAS Inc., Cary, NC, USA). Binomial logistic regression analyses were performed to see whether the subjects’ age, sex, or the diagnostic certainty of VM have an association with the presence of vestibular dysfunction. The dependent variables were abnormalities in the results of caloric, ACS cVEMP, or BCV oVEMP testing, and the independent variables were age, sex (i.e., male vs female), and the diagnostic certainty of VM (i.e., VM vs. PVM). p < 0.05 was considered statistically significant without adjustment for multiple testing.
Results
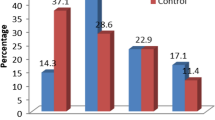
Abnormal caloric responses were found in 36% (n = 8) of the VM patients and 27% (n = 6) of the PVM patients (Table 2). All of the patients with abnormal caloric responses were unilaterally abnormal. Abnormal cVEMP responses were shown in 36% (n = 8) of the VM patients and 36% (n = 8) of the PVM patients (Table 2). Four of the eight VM patients and three of the eight PVM patients had bilaterally abnormal cVEMPs. Abnormal oVEMP responses were found in 41% (n = 9) of the VM patients and 9% (n = 2) of the PVM patients (Table 2). Five of the nine VM patients showed bilaterally abnormal oVEMPs.
With regard to VEMP latency, cVEMP latency was prolonged in only one patient (5%) in VM and one patient (5%) in PVM. oVEMP latency was prolonged in only one patient (5%) in VM, but not in PVM. These three patients showed prolonged VEMP latency unilaterally.
The percentage of patients with a pure-tone-average threshold of 25 dB HL or more for frequencies of 0.5, 1, and 2 kHz on at least one side was 18% in the definite VM group and 18% in the probable VM group. There was no difference in the proportion of patients with hearing loss between the two groups.
First, we investigated whether age, sex, or the diagnostic certainty of VM had an association with abnormalities in caloric testing. Logistic regression analysis indicated that there was no significant association [p = 0.668 (age), p = 0.728 (sex), and p = 0.548 (diagnostic certainty of VM)] (Table 3). The odds ratio of abnormal caloric responses for age, sex, and for VM compared with PVM was 0.989 [95% confidence interval (CI), 0.942–1.039), 1.330 (95% CI, 0.266–6.656] and 1.484 (95% CI, 0.409–5.393), respectively.
Next, we investigated whether age, sex, or the diagnostic certainty of VM had an association with abnormalities in ACS cVEMP testing. Logistic regression analysis showed that only age had a significant positive association with abnormalities in ACS cVEMP testing [p = 0.0242 (age), and p = 0.761 (sex) and p = 0.780 (diagnostic certainty of VM)] (Table 4). The odds ratio of abnormal ACS cVEMPs for age, sex, and for VM compared with PVM was 1.069 [95% confidence interval (CI), 1.009–1.133], 1.311 (95% CI, 0.229–7.506), and 1.211 (95% CI, 0.317–4.628), respectively.
We then investigated whether age, sex, or the diagnostic certainty of VM had an association with abnormalities in BCV oVEMP testing. Logistic regression analysis showed that only the diagnostic certainty of VM had a significant positive association with abnormalities in BCV oVEMP testing [p = 0.121 (age), p = 0.277 (sex), and p = 0.0143 (diagnostic certainty of VM)] (Table 5). The odds ratio of abnormal BCV oVEMPs for age, sex, and for VM compared with PVM was 1.052 [95% confidence interval (CI), 0.987–1.121], 0.243 (95% CI, 0.019–3.120), and 10.353 (95% CI, 1.597–67.114), respectively.
In summary, the only variable that had a significant positive association with the diagnostic certainly of VM was abnormality of BCV oVEMPs.
Discussion
In the present study, we investigated the association between the diagnostic certainty of VM and the results of vestibular function tests. We showed that there was no significant association between the diagnostic certainty of VM and abnormality in caloric or ACS cVEMP testing. On the other hand, VM had a significant positive association with abnormality in BCV oVEMP testing compared with PVM.
The function of the SCCs in VM patients has been evaluated by caloric testing [2, 4, 8, 9, 13, 14, 32, 34, 35] and vHIT [2, 20, 35]. The prevalence of CP in caloric testing in VM patients ranged from 8 to 42% according to the previous reports [2, 4, 8, 9, 13, 14, 32, 34, 35]. The prevalence of abnormalities in caloric testing was higher in VM patients than in healthy controls [13]. Abnormal vHIT results in the LSCC plane was found in approximately 10% of VM patients [2, 20, 35]. A previous study reported that abnormalities in the caloric test and vHIT in VM patients predicted a requirement for prolonged preventive medication [35], suggesting that vestibular abnormalities are closely related to disease control in VM patients. A recent study reported that the percentage of migraine among patients with BVP of unknown cause was significantly higher than that among BVP patients with a definite or probable etiology [24]. Since BVP in that study was assessed by the caloric test, their results suggest an association between the pathophysiology of migraine and the function of the vestibulo-ocular pathway relating to the LSCC.
The function of the otolith organs has been evaluated by cVEMP [1, 3, 12, 13, 19, 29, 36, 37] and oVEMP testing [13, 33, 36, 37]. Some cVEMP studies have reported that abnormal responses, defined by reduced amplitudes, low ARs, or absent responses, were more prevalent in VM patients than in healthy controls [1, 3, 12, 13, 36, 37], suggesting an association between VM and dysfunction of the sacculo-collic pathway. On the other hand, others have reported that there were no differences in cVEMP amplitude or the prevalence of cVEMP abnormalities between VM patients and healthy controls [13, 19, 29]. As for oVEMPs, some studies have shown that abnormal oVEMP responses, defined by reduced amplitudes or low ARs, were found more often in VM patients than in healthy controls, suggesting an association between VM and dysfunction of the utriculo-ocular pathway [13, 36]. In contrast, the other studies have reported that there were no differences in oVEMP amplitude or the prevalence of oVEMP abnormalities between VM patients and healthy controls [13, 33, 37]. The conflicting results among these VEMP studies may be due to differences in the stimulation methods used to evoke VEMPs, in the evaluation methods of abnormal VEMP responses, and/or in the profiles of the VM patients.
VM was described in the appendix of ICHD-3β as a novel disease entity by consensus of the International Headache Society Classification Committee and the Barany Society Classification Committee [11]. The Barany classification included PVM as well as VM by considering the balance between the sensitivity and specificity of the diagnostic criteria. Although vestibular dysfunction is not used as the diagnostic criteria for VM, our finding that vestibular dysfunction involving the utriculo-ocular pathway (revealed by abnormal BCV oVEMPs) occurs more frequently in patients with definite VM than probable VM suggests that dysfunction in the utriculo-ocular pathway might be associated with the pathology of VM. We consider that the pathology of VM is more advanced than that of PVM. Vestibular dysfunction can be more developed in VM than in PVM. The patients with prolonged VEMP latency were very few, suggesting that vestibular dysfunction in VM may be caused by peripheral rather than central mechanism.
It is still unclear why there was a significant difference between the two groups in the proportion of BCV oVEMP abnormalities and no significant difference between the two groups in the proportion of abnormalities in caloric testing and ACS cVEMPs. However, one previous report revealed that VM patients were more likely than patients with vestibular disorders other than VM to exhibit normal ACS cVEMPs in the presence of unilaterally abnormal ACS oVEMPs [25]. This result supports a possible pathophysiological association between the utriculo-ocular reflex and VM.
A possible association between migraine and BVP has been previously reported [24]. In our study, with respect to whether the abnormal responses in vestibular function tests in VM and PVM were unilateral or bilateral, caloric testing showed unilaterally abnormal responses, whereas VEMP testing showed bilaterally as well as unilaterally abnormal responses. As for cVEMPs, an association between aging and abnormal responses was found independent of the diagnostic certainty of VM (Table 2). Therefore, the aging effect on cVEMP abnormal responses should be considered apart from the pathogenesis of migraine.
The present study has some limitations. First, as this is a retrospective study, there might be the potential for selection bias and information bias. Second, the present study is exploratory to assess whether diagnostic certainty of VM is associated with the abnormality of either caloric responses, cVEMPs or oVEMPs. In future confirmatory studies that focus on the association between diagnostic certainty of VM and oVEMPs, adjustment for multiple testing is required to protect against wrong conclusions. The study also requires formal sample size estimation. Third, the present study is a cross-sectional study, and whether the abnormalities in vestibular function tests are variable or permanent cannot be determined. Vestibular functions were measured in the quiescent period of VM in the present study. The time period between the most recent attack and subsequent testing, and the frequency of the attacks, varied between patients. The results of vestibular function tests might be affected by the time elapsed since the patient's last attack and the frequency of the attacks. Fourth, the confidence interval for the odds ratio between BCV oVEMPs and the diagnostic certainty of VM was relatively wide. Fifth, cVEMP amplitudes were not corrected for muscular activity of the SCM and that this might affect the AR values.
In conclusion, we revealed that VM has a significant positive association with abnormalities in BCV oVEMPs compared with PVM, suggesting that the pathophysiology of VM involves the utriculo-ocular pathway.
References
Baier B, Stieber N, Dieterich M (2009) Vestibular-evoked myogenic potentials in vestibular migraine. J Neurol 256:1447–1454
Blodow A, Heinze M, Bloching MB, von Brevern M, Radtke A, Lempert T (2014) Caloric stimulation and video-head impulse testing in Meniere's disease and vestibular migraine. Acta Otolaryngol 134:1239–1244
Boldingh MI, Ljostad U, Mygland A, Monstad P (2011) Vestibular sensitivity in vestibular migraine: VEMPs and motion sickness susceptibility. Cephalalgia 31:1211–1219
Celebisoy N, Gokcay F, Sirin H, Bicak N (2008) Migrainous vertigo: clinical, oculographic and posturographic findings. Cephalalgia 28:72–77
Chihara Y, Iwasaki S, Ushio M, Murofushi T (2007) Vestibular-evoked extraocular potentials by air-conducted sound: another clinical test for vestibular function. Clin Neurophysiol 118:2745–2751
Colebatch JG, Halmagyi GM, Skuse NF (1994) Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry 57:190–197
Curthoys IS, Kim J, McPhedran SK, Camp AJ (2006) Bone conducted vibration selectively activates irregular primary otolithic vestibular neurons in the guinea pig. Exp Brain Res 175:256–267
Cutrer FM, Baloh RW (1992) Migraine-associated dizziness. Headache 32:300–304
Dieterich M, Brandt T (1999) Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol 246:883–892
Fujimoto C, Murofushi T, Chihara Y, Suzuki M, Yamasoba T, Iwasaki S (2009) Novel subtype of idiopathic bilateral vestibulopathy: bilateral absence of vestibular evoked myogenic potentials in the presence of normal caloric responses. J Neurol 256:1488–1492
Headache Classification Committee of the International Headache S (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33:629–808
Hong SM, Kim SK, Park CH, Lee JH (2011) Vestibular-evoked myogenic potentials in migrainous vertigo. Otolaryngol Head Neck Surg 144:284–287
Inoue A, Egami N, Fujimoto C, Kinoshita M, Yamasoba T, Iwasaki S (2016) Vestibular evoked myogenic potentials in vestibular migraine: do they help differentiating from meniere's disease? Ann Otol Rhinol Laryngol 125:931–937
Iwasaki S, Chihara Y, Smulders YE, Burgess AM, Halmagyi GM, Curthoys IS, Murofushi T (2009) The role of the superior vestibular nerve in generating ocular vestibular-evoked myogenic potentials to bone conducted vibration at Fz. Clin Neurophysiol 120:588–593
Iwasaki S, Smulders YE, Burgess AM, McGarvie LA, Macdougall HG, Halmagyi GM, Curthoys IS (2008) Ocular vestibular evoked myogenic potentials in response to bone-conducted vibration of the midline forehead at Fz. A new indicator of unilateral otolithic loss. Audiol Neurootol 13:396–404
Iwasaki S, Smulders YE, Burgess AM, McGarvie LA, Macdougall HG, Halmagyi GM, Curthoys IS (2008) Ocular vestibular evoked myogenic potentials to bone conducted vibration of the midline forehead at Fz in healthy subjects. Clin Neurophysiol 119:2135–2147
Iwasaki S, Takai Y, Ito K, Murofushi T (2005) Abnormal vestibular evoked myogenic potentials in the presence of normal caloric responses. Otol Neurotol 26:1196–1199
Iwasaki S, Ushio M, Chihara Y, Ito K, Sugasawa K, Murofushi T (2007) Migraine-associated vertigo: clinical characteristics of Japanese patients and effect of lomerizine, a calcium channel antagonist. Acta Otolaryngol Suppl 45–49
Kandemir A, Celebisoy N, Kose T (2013) Cervical vestibular evoked myogenic potentials in primary headache disorders. Clin Neurophysiol 124:779–784
Kang WS, Lee SH, Yang CJ, Ahn JH, Chung JW, Park HJ (2016) Vestibular function tests for vestibular migraine: clinical implication of video head impulse and caloric tests. Front Neurol 7:166
Kayan A, Hood JD (1984) Neuro-otological manifestations of migraine. Brain 107(Pt 4):1123–1142
Kuritzky A, Ziegler DK, Hassanein R (1981) Vertigo, motion sickness and migraine. Headache 21:227–231
Lempert T, Olesen J, Furman J, Waterston J, Seemungal B, Carey J, Bisdorff A, Versino M, Evers S, Newman-Toker D (2012) Vestibular migraine: diagnostic criteria. J Vestib Res 22:167–172
Lucieer F, Vonk P, Guinand N, Stokroos R, Kingma H, van de Berg R (2016) Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol 7:26
Makowiec KF, Piker EG, Jacobson GP, Ramadan NM, Roberts RA (2018) Ocular and cervical vestibular evoked myogenic potentials in patients with vestibular migraine. Otol Neurotol 39:e561–e567
Murofushi T (2016) Clinical application of vestibular evoked myogenic potential (VEMP). Auris Nasus Larynx 43:367–376
Murofushi T, Curthoys IS, Gilchrist DP (1996) Response of guinea pig vestibular nucleus neurons to clicks. Exp Brain Res 111:149–152
Murofushi T, Matsuzaki M, Wu CH (1999) Short tone burst-evoked myogenic potentials on the sternocleidomastoid muscle: are these potentials also of vestibular origin? Arch Otolaryngol Head Neck Surg 125:660–664
Murofushi T, Ozeki H, Inoue A, Sakata A (2009) Does migraine-associated vertigo share a common pathophysiology with Meniere's disease? Study with vestibular-evoked myogenic potential. Cephalalgia 29:1259–1266
Neuhauser HK, Radtke A, von Brevern M, Feldmann M, Lezius F, Ziese T, Lempert T (2006) Migrainous vertigo: prevalence and impact on quality of life. Neurology 67:1028–1033
Schmal F, Lubben B, Weiberg K, Stoll W (2005) The minimal ice water caloric test compared with established vestibular caloric test procedures. J Vestib Res 15:215–224
Shin JE, Kim CH, Park HJ (2013) Vestibular abnormality in patients with Meniere's disease and migrainous vertigo. Acta Otolaryngol 133:154–158
Taylor RL, Zagami AS, Gibson WP, Black DA, Watson SR, Halmagyi MG, Welgampola MS (2012) Vestibular evoked myogenic potentials to sound and vibration: characteristics in vestibular migraine that enable separation from Meniere's disease. Cephalalgia 32:213–225
von Brevern M, Zeise D, Neuhauser H, Clarke AH, Lempert T (2005) Acute migrainous vertigo: clinical and oculographic findings. Brain 128:365–374
Yoo MH, Kim SH, Lee JY, Yang CJ, Lee HS, Park HJ (2016) Results of video head impulse and caloric tests in 36 patients with vestibular migraine and 23 patients with vestibular neuritis: a preliminary report. Clin Otolaryngol 41:813–817
Zaleski A, Bogle J, Starling A, Zapala DA, Davis L, Wester M, Cevette M (2015) Vestibular evoked myogenic potentials in patients with vestibular migraine. Otol Neurotol 36:295–302
Zuniga MG, Janky KL, Schubert MC, Carey JP (2012) Can vestibular-evoked myogenic potentials help differentiate Meniere disease from vestibular migraine? Otolaryngol Head Neck Surg 146:788–796
Acknowledgements
We thank all of the members of the Department of Otolaryngology and Head and Neck Surgery, Graduate School of Medicine, The University of Tokyo for helpful discussions. This work was supported by the Ministry of Education, Culture, Sports, Science and Technology [Grant number 15H05940].
Funding
This work was supported by the Ministry of Education, Culture, Sports, Science and Technology [Grant number 15H05940].
Author information
Authors and Affiliations
Contributions
CF: conceived of the study, conducted the experiments, and wrote the manuscript and edited the manuscript for content. TK, ST, MK, and KS: edited the manuscript for content. TK: provided statistical advice, performed statistical analysis, and edited the manuscript for content. TY and SI: supervised interpretation of data and edited the manuscript for content.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict of interest.
Ethics approval
The present study was approved by the Research Ethics Committee, Graduate School of Medicine and Faculty of Medicine, at the University of Tokyo (#2487).
Consent to participate
Written informed consent was waived, because retrospective data from medical records were used in the present study.
Additional information
Statistical Analysis conducted by Takuya Kawahara MPH PhD (Biostatistics Division, Clinical Research Promotion Center, The University of Tokyo Hospital).
Appendix
Appendix
Diagnostic criteria for VM
A. At least five episodes fulfilling criteria C and D.
B. A current or past history of 1.1 Migraine without aura or 1.2 Migraine with aura according to ICHD-3.
C. Vestibular symptoms of moderate or severe intensity, lasting between 5 min and 72 h.
D. At least 50% of episodes are associated with at least one of the following three migrainous features:
1. Headache with at least two of the following four characteristics: unilateral headache, pulsating quality, moderate to severe intensity, aggravation by routine physical activity.
2. Photophobia and phonophobia.
3. Visual aura.
E. Not better accounted for by another ICHD-3 diagnosis or by another vestibular disorder.
Diagnostic criteria for PVM
A. At least five episodes with vestibular symptoms of moderate or severe intensity, lasting 5 min to 72 h.
B. Only one of the criteria B1 and B2 is fulfilled (migraine history or migraine features,
during the episode).
B1 Current or previous history of migraine with or without aura according to the ICHD-3
B2 One or more migraine features with at least 50% of the vestibular episodes:
1. Headache with at least two of the following characteristics: one sided location, pulsating quality, moderate or severe pain intensity, and aggravation by routine physical activity.
2. Photophobia and phonophobia.
3. Visual aura.
C. Not better accounted for by another ICHD-3 diagnosis or by another vestibular disorder.
Rights and permissions
About this article
Cite this article
Fujimoto, C., Kamogashira, T., Takenouchi, S. et al. Utriculo-ocular pathway dysfunction is more frequent in vestibular migraine than probable vestibular migraine. J Neurol 267, 2340–2346 (2020). https://doi.org/10.1007/s00415-020-09851-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09851-y