Abstract
Axonal variants of Guillain–Barré syndrome (GBS) mainly include acute motor axonal neuropathy, acute motor and sensory axonal neuropathy, and pharyngeal-cervical-brachial weakness. Molecular mimicry of human gangliosides by a pathogen's lipooligosaccharides is a well-established mechanism for Campylobacter jejuni-associated GBS. New triggers of the axonal variants of GBS (axonal GBS), such as Zika virus, hepatitis viruses, intravenous administration of ganglioside, vaccination, and surgery, are being identified. However, the pathogenetic mechanisms of axonal GBS related to antecedent bacterial or viral infections other than Campylobacter jejuni remain unknown. Currently, autoantibody classification and serial electrophysiology are cardinal approaches to differentiate axonal GBS from the prototype of GBS, acute inflammatory demyelinating polyneuropathy. Newly developed technologies, including metabolite analysis, peripheral nerve ultrasound, and feature selection via artificial intelligence are facilitating more accurate diagnosis of axonal GBS. Nevertheless, some key issues, such as genetic susceptibilities, remain unanswered and moreover, current therapies bear limitations. Although several therapies have shown considerable benefits to experimental animals, randomized controlled trials are still needed to validate their efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A generic view of GBS
First reported in 1916 by Guillain et al. [1], Guillain–Barré syndrome (GBS) is a autoimmune disease of the peripheral nervous system (PNS) that is clinically characterized by acute flaccid paralysis and/or sensory/autonomous nerve dysfunction. The annual incidence of GBS is 0.81–1.89 per 100,000 persons worldwide, and appears to be increasing exponentially, along with increasing age, in Western countries [2, 3]. The relative risk of GBS for males is 1.78-fold higher than that for females [2]. A majority of patients with GBS exhibit tetraplegia with sensory disturbance and loss of deep tendon reflexes. About 10% of patients with atypical GBS share normal or even hyperexcitable tendon reflexes during the early phase, especially those with pure motor signs or those diagnosed with an acute motor axonal neuropathy (AMAN), based on electrophysiology [4, 5]. Patients with classical sensorimotor GBS usually present with rapidly progressive symmetric weakness with sensory loss [5, 6]. The initiation of GBS is suggested to be caused by a complicated hyperreactive autoimmune response targeting the PNS [7].
Albuminocytologic dissociation is a hallmark of GBS and can be detected in almost 90% of GBS cases [8]. Usually, albumin in the cerebrospinal fluid (CSF) increases from the 2nd week after onset; albuminocytologic dissociation is notable in 70% of patients at the end of this week, and peaks during the 3rd week [8]. Accompanied by obvious inflammatory infiltration and demyelination of the peripheral nerves, GBS was initially defined as an acute inflammatory demyelinating polyneuropathy (AIDP). Currently, AIDP is the most prevalent subtype of GBS worldwide, yet the incidence of axonal GBS has increased in Asia and Europe during the past decade [3, 9]. Recent work focusing on the axonal variants of GBS (axonal GBS) has mainly concentrated on optimizing diagnosis and treatments. Computer-assisted feature analysis has resulted in greater diagnostic accuracy and plasma metabolite measurement has provided novel biomarkers [10, 11]. Based on precision medicine, identification of individual gene polymorphisms may predict the risk of axonal GBS; immune therapies (e.g., anti-B cell therapy, anticomplement therapy, and anticytokine therapy, among others) appear to be promising for the treatment of axonal GBS [12,13,14].
From “Chinese paralysis” to axonal GBS
More than half a century had passed before axonal variants were recognized in the 100-year history of GBS (Fig. 1) [15, 16]. The earliest probable cases of axonal GBS were recorded in Jordan in 1978; 16 GBS patients developed a rapidly progressive paralysis after a polluted water-associated diarrhea epidemic, and electrophysiology revealed polyphasic and M-shaped motor units [17]. In 1986, axonal involvement, i.e., axonal degeneration in nerve roots and distal nerves, was pathologically confirmed in an autopsy study of GBS [18]. Nonetheless, it was not until 1993 that “Chinese paralysis”, a term previously used to describe annual epidemics of acute-onset flaccid paralysis among children and young adults in northern China during the summer months, was redefined as a new subtype of GBS, namely AMAN, characterized by axonal degeneration [19, 20]. Electrophysiological studies of such patients revealed a reduction in the compound muscle action potentials (CMAPs) [21]. Anti-GM1 antibody is commonly associated with AMAN, acting to block presynaptic transmitter release from motor nerves in a complement-dependent way [22]. High rates of Campylobacter jejuni (C. jejuni) infection and serum anti-GM1 IgG positivity have also been observed in AMAN [21]. In 2001, Yuki et al. for the first time established an AMAN animal model by inoculating rabbits with bovine brain gangliosides and described a Wallerian-like degeneration at the PNS caused by anti-GM1 antibodies [23].
Chronicle of the investigation of axonal GBS. aZipper methods (1 course): PE was conducted with 1.5 volume of patients’ plasma (5% albumin replacement) in the first session followed by a standard IVIg infusion (0.4 g/kg body weight). The second PE session was applied with one volume change after 24 hours from the end of the IVIg infusion. Each PE session was followed by IVIG infusions. This PE-IVIg cycle was repeated for 5 times. AMAN acute motor axonal neuropathy, AMSAN acute motor sensory axonal neuropathy, C. jejuni Campylobacter jejuni, GBS Guillain–Barré syndrome, IVIg intravenous immunoglobulin, LOS lipooligosaccharide, MFS Miller Fisher syndrome, PCB pharyngeal-cervical-brachial weakness, PE plasma exchange, ZIKV Zika virus
The International Guillain–Barré Syndrome Outcome Study (IGOS) has reported a higher incidence and morbidity of axonal GBS in Bangladesh than in other Asian and European countries [24]. Younger age, fewer sensory deficits, and a trend of poorer recovery were cardinal features in Bangladeshi GBS cases [24]. A retrospective study reported that AMAN is the most common subtype, accounting for 55.8% of GBS cases in northern China [25]. Classification of GBS subtypes can be made according to multiple factors, including antecedent infection, autoantibody classification, electrophysiological patterns, geographical differences, and genetic susceptibility [26].
Clinical features of axonal GBS
Axonal GBS includes systematic subtypes, i.e., AMAN and acute motor sensory axonal neuropathy (AMSAN), and several regional variants, e.g., pharyngeal-cervical-brachial weakness (PCB) [27]. Precedent infection with C. jejuni is most commonly seen in patients with axonal GBS. Besides C. jejuni, viruses including Zika virus (ZIKV), cytomegalovirus (CMV), hepatitis viruses (types A, B, C, and E), human immunodeficiency virus (HIV), Epstein–Barr virus (EBV), shigella, clostridium, Haemophilus influenzae and Mycoplasma pneumoniae, have all been associated with the disease onset of GBS [28, 29]. Patients with either AMAN or AMSAN display motor nerve involvements [30]. Electrophysiological studies on patients with AMAN during the early phase may reveal reversible conduction blocks (CBs), reversible conduction failures (RCFs), or decreased CMAP amplitudes [27]. Electrophysiological diagnosis 3–6 weeks after GBS onset, however, is more reliable than that within 1–2 weeks [27]. Antibody detection is mainly used for the classification of axonal GBS. Anti-ganglioside IgG and IgM antibodies were first detected in patients with GBS in 1988 [31]. Antibodies to GM1 and GD1a are frequently elevated in patients with AMAN/AMSAN [32]. For PCB, anti-GQ1b and anti-GT1a antibodies are identifiable in patients [33, 34]. Given the fact that commercialized antibody detection kits have barely exhibited satisfactory sensitivity and specificity, antibody diagnostics may be optimized using synthetic ganglioside mimics to provide more convincing diagnostic values [35].
Despite the fact that Miller Fisher syndrome (MFS) was occasionally classified as an axonal subtype, more researchers would rather consider MFS as an independent variant of GBS [33]. GQ1b is mainly localized in the paranodal myelin of cranial nerves innervating ocular muscles; MFS and Bickerstaff brainstem encephalitis (BBE) are associated with elevated levels of anti-GQ1b antibody [36, 37]. In this regard, both MFS and BBE have been categorized into anti-GQ1b antibody syndrome [38]. Autopsy studies on patients with MFS revealed segmental demyelination in the PNS and the spinal cord [39]. The high recurrence rates of MFS and BBE also support that anti-GQ1b antibody syndrome mainly involve myelin pathologically [40, 41]. PCB accounts for 3% of GBS cases and shares clinical features with axonal GBS, including facial palsy, dysarthria, muscle weakness, and areflexia in upper extremities [34]. Half of the patients with MFS developed PCB, BBE, and conventional GBS in the first 7 days after onset, while the proportion of autoantibodies did not change significantly during this shift [42], indicating that a portion of patients with PCB and conventional GBS also belong to anti-GQ1b antibody syndrome.
Presenting as unilateral or bilateral facial paralysis (BFP), Bell’s palsy was occasionally regarded as a regional subtype of GBS [43]. BFP is the most common cranial nerve feature of GBS and 23% of BFPs are Bell’s palsy [44]. In Colombia, 30% of GBS patients had accompanying facial palsy [45]. BFP with paresthesia is a GBS variant, and BFP itself is also highly indicative of GBS [5]. Nevertheless, typical anti-ganglioside antibodies were undetectable in patients with BFP with paresthesia [32]. Importantly, in a HSV-associated facial paralysis model, facial nerve demyelination was observed in the descending root [46]. More pathological evidence may be required to include or exclude Bell’s palsy as a subtype of axonal GBS.
To interpret the pathogenesis of axonal GBS through AMAN
C. jejuni infection and molecular mimicry
The preceding infections in patients with AMAN involve a variety of bacteria and viruses; in fact, 40–70% of GBS cases are preceded by a prodromal acute infection [47]. In southern China, antecedent gastrointestinal infection was closely associated with development of AMAN [48]. Similarly, 53% of C. jejuni-associated GBS cases in the Netherlands were diagnosed as axonal GBS [49]. In line with these findings, C. jejuni was demonstrated as a major GBS-associated pathogen in the greater Paris area between 1996 and 2007 [50]. Notwithstanding, more than half of the patients with anti-ganglioside antibodies did not have an antecedent C. jejuni infection in Japan [51]. A possible explanation for the inconsistency is that the virulence or antigen composition may differ between different strains of C. jejuni. An alternative explanation is that infections with other pathogens may account for the production of anti-ganglioside antibodies. Besides C. jejuni, Haemophilus influenzae-associated respiratory tract infections have been proposed to precede GBS; non-encapsulated Haemophilus influenzae has a GM1-like structure and may trigger axonal GBS [52]. The associations between anti-ganglioside antibodies and various pathogens merit further investigation. For example, the cathelicidin release, inflammasome responses, cell receptor and signaling pathways in intestinal epithelial cells and their roles in immune network in C. jejuni-associated gastrointestinal infection are still unknown [53].
Molecular mimicry is a widely accepted hypothesis to explain hyperreactive autoimmunity in C. jejuni-associated axonal GBS (Fig. 2) [54]. The presence of GM1-like epitopes on the lipopolysaccharide (LPS) of C. jejuni was first illustrated by Yuki et al. [55]. After recognizing that C. jejuni LPS carried GQ1b and GD1a-like epitopes [56], researchers hypothesized that a similarity in human gangliosides and lipooligosaccharide (LOS) of C. jejuni may trigger molecular mimicry [54]. Consistently, GT1a-like LOS expressed on C. jejuni promoted the production of anti-GT1a antibody in almost 53% of patients with GBS [57]. Interestingly, GM1-like and GD1a-like LOS may constitute a complex mimicking GM1b and trigger anti-GM1b IgG antibody release [58]. In this regard, LOS subtyping may benefit axonal GBS classification: C. jejuni isolated from patients with AMAN frequently had GM1-like and GD1a-like LOS [7]. After comparing the proteins extracted from the peripheral nerves of GBS patients and C. jejuni, researchers found that heat shock protein (HSP) chaperones of both also shared a high primary sequence homology and conservation of epitopes, implying a possible HSP mimicry [59]. In summary, molecular mimicry is a widely accepted hypothesis to explain the pathogenesis of axonal GBS. Nevertheless, only a few pathogens (i.e., C. jejuni and Mycoplasma pneumoniae, among others) have been corroborated to trigger GBS by molecular mimicry [54, 60]. Further investigations are required to identify unknown antibodies and explore other pathogens that may cause mimicry.
Cellular mechanism in AMAN pathogenesis. Ganglioside-like LOS loaded on C. jejuni is recognized by TLRs expressed on APCs. APCs activate B cell and T helper cell proliferation. B cells develop into plasma cells and produce anti-ganglioside antibodies. Activated T helper cells secrete pro-inflammatory cytokines and chemokines and facilitate the penetration of macrophages across the blood–nerve barrier. Anti-ganglioside antibodies attack the nodes of Ranvier and activate complements to form MAC. MACs target axolemma and injure paranodal myelin and Nav channels. Anti-Gal-C and anti-LM1 antibodies also damage Schwann cells and myelin sheaths. IL-1β, TNF-α and MMPs aggravate the autoimmunity and macrophages phagocytose injured axons. (AMAN acute motor axonal neuropathy, Caspr contactin-associated protein, IL interleukin, C. jejuni Campylobacter jejuni, Gal-C galactocerebroside, Kv voltage-gated potassium channels, GBS Guillain–Barré syndrome, LOS lipooligosaccharide, MAC membrane attack complex, MMPs matrix metalloproteinases, Nav voltage-gated sodium channels, Th1 and Th2 cell T helper cell 1 and 2, TLR Toll-like receptor, TNF-α tumor necrosis factor-α)
Unknown pathogenesis with other antecedent bacterial or viral infections
A case report proposed that a potential neurotropism of ZIKV may be associated with GBS onset [61]. Anti-ZIKV IgM was detected in most AMAN cases in Colombia [27, 62]. During the outbreak of ZIKV in Colombia, 20 of 42 patients with GBS had an antecedent ZIKV infection [63]. Interestingly, when a ZIKV outbreak occurred during 2013–2014 in French Polynesia, most patients with GBS were compatible with the electrophysiological diagnostic criteria of AMAN [64]. The positive rate of typical anti-ganglioside antibody emerging in ZIKV-associated AMAN was 31% at onset and was increased to 48% after 3 months [64]. Notably, during this epidemic anti-GA1 antibody was the most common anti-ganglioside antibody in ZIKV-associated GBS patients’ sera [64]. In an outbreak of ZIKV in Bangladesh, cranial, autonomic, and sensory nerves were involved in ZIKV-associated GBS patients, yet electrophysiological studies confirmed most patients as AIDP [65]. In Brazil, ZIKV accounted for almost the same incidence of AMAN and AIDP [66]. ZIKV-associated GBS bears a higher morbidity during the acute phase and more frequent cranial nerve deficits alongside acute neuropathy and 6 months afterwards [67]. Interestingly, ZIKV infection has been shown to damage the Golgi apparatus in neurons, implying a possible intracellular mechanism by a disruption of posttranslational modification [68]. ZIKV-infected mice mainly develop seizures, neurodegeneration, and behavioral changes without typical GBS features [69]. The mechanisms underlying ZIKV-triggered GBS are unknown and need to be deciphered, e.g. through antibody and cytokine detection via high-throughput ELISA or flow cytometry.
Besides ZIKV, other viruses have been associated with axonal GBS. For instance, AMAN has been attributed to the initiation of hepatitis E infection [70]. Influenza A H1N1 infection may trigger AMAN as well [71]. CMV infection has been associated with 15% of GBS cases, mainly causing severe sensory symptoms [72]. Interestingly, electrophysiological results in virus-associated GBS exhibited higher motor and lower sensory action potentials compared to C. jejuni-associated GBS, providing a new strategy to differentiate between the two [49]. Although infections caused by C. jejuni and Mycoplasma pneumoniae have been demonstrated to trigger GBS by molecular mimicry [51, 59], whether other pathogens induce GBS in a similar manner or by sharing unknown pathways remains unclear.
Does ganglioside administration trigger AMAN?
The first AMAN model was established in rabbits by inoculation with a bovine brain ganglioside mixture [23]. Ganglioside as a nutritional drug has hitherto been widely used in China for nerve regeneration, although ganglioside-associated GBS cases have scarcely been documented [73]. GBS may occur following intravenous administration of exogenous ganglioside [74], and high titers of anti-GM1 antibodies were identified in these patients [75]. In fact, ganglioside-associated GBS had been reported in Europe several decades before, leading to the withdrawal of ganglioside from the European market [76]. In spite of this, no significant relationship between ganglioside use and incidence of GBS was found in a consistent study from 1981 to 2001 in Italy [77, 78].
Anti-GM1 antibodies have been detected in patients receiving ganglioside therapy [75]. More severe functional deficits at nadir and poorer recovery in ganglioside-associated GBS have been reported in northeast China [79]. Ganglioside-associated GBS bears more severe clinical features with poorer short-term prognosis than non-ganglioside-associated GBS [79]. Up to 91.67% of patients with ganglioside-associated GBS were diagnosed with AMAN according to the Rajabally’s criteria [74]. However, most patients who received ganglioside did not develop either AIDP or AMAN [80]. We speculate that ganglioside might be contaminated with endotoxin during the production process, which could cause GBS by serving as immunogen and adjuvant. More evidence is needed to reach a con or pro consensus on the clinical use of ganglioside.
Does vaccination trigger AMAN or AIDP?
Vaccination has frequently been monitored as a trigger for GBS, and the guidelines for disease presentation, data collection, and analysis of vaccination-associated GBS have been documented elsewhere [81]. Vaccines, including the influenza, rabies, oral polio, diphtheria and tetanus toxoid, meningococcal, measles and mumps, hepatitis, and smallpox vaccines have all been associated with sporadic GBS [82]. Indeed, swine flu vaccine-induced GBS during the 1976–1977 outbreak is considered to be the earliest and most severe vaccination-associated GBS [83].
In addition to introducing pandemic flu outbreaks, the influenza virus can trigger antecedent upper respiratory tract and gastrointestinal infections, which are also closely associated with the development of GBS [84]. The influenza vaccine prevents influenza infections as well as lowering the risk of influenza-associated GBS [85]. According to a meta-analysis, influenza A (H1N1) 2009 monovalent inactivated vaccines resulted in approximately 1.6 excess cases of GBS per million people vaccinated; nonetheless, the overall effects were beneficial [86, 87]. Several subsequent studies supported the safety of vaccinations [88,89,90,91,92]. Nevertheless, a study in Québec argued that H1N1 vaccine led to a small but significant risk (2 per million), especially in people older than 50 [93]. Ganglioside contamination in nerve tissue-derived vaccines may account for GBS triggered by the rabies vaccination [94]. Quality control during production is therefore of utmost importance for ganglioside or LPS to be used as an exogenous supplement or contamination.
Generally, specific biological markers that represent a cause-and-effect association with the disorder have been proved to exclude causality in vaccine-associated GBS; however, GBS cases are only temporally associated with numerous vaccines [81]. The interval between vaccination and onset of GBS must be defined to better evaluate the association. Unfortunately, GBS surveillance after vaccination in recent years has provided few valuable results [84, 92]. Instead, sporadic cases were continuously reported, alerting the public to vaccination-associated GBS. Vaccination itself can introduce symptoms similar to mild GBS, including, fatigue and limb weakness. Likewise, mild GBS cases may be less frequently referred to neurologists, leading to a possible underestimation of vaccination-associated GBS [95]. Nonetheless, vaccinations largely may indirectly reduce GBS incidence by controlling ZIKV or hepatitis viruses; whereas the influenza vaccine may introduce a small increase of GBS risk, the benefits from inactivated vaccines remarkably outweigh the risks [84].
Differentiation between axonal GBS and AIDP
Antibody classification of axonal GBS
The differences between axonal and AIDP mainly refer to their associated antecedent infections, neurological features, electrophysiological results, and serum antibodies (Table 1) [73]. Antibodies to gangliosides are instrumental to differentiate GBS subtypes (Table 2). Antibody-dependent membrane attack complex (MAC) formation, C3b receptor-dependent phagocytosis, and cytokines released by infiltrated CD4 + T helper (Th) cells are all involved in GBS pathogenesis (Fig. 2) [14, 96]. Clinical and electrophysiological features appeared to be determined by anti-ganglioside antibodies, and the antibodies were associated with motor axonal GBS in both Japan and Italy [27]. Motor and sensory nerves express similar quantities of GM1 and GD1a, although their expression in other tissues may differ [32]. Anti-GM1 and anti-GT1a antibodies were predominantly of the IgG1 and IgG3 subclasses [97]. IgG1 and IgG3, as complement-fixing IgGs, promote MAC generation and alter Na+ channel function in axonal injury, leading to a transient conduction block and accounting for rapid recovery of AMAN after treatment [98]. Higher titers of antibodies against neurofascin and persistent IgG4 responses to neurofascin-155 have also been detected in autoimmune neuropathies [99]. Of note is that the presence of IgM antibody does not always support a diagnosis of GBS in that this antibody can be detected in patients with C. jejuni enteritis but without GBS [100]. Although predominant antibody-mediated immunity was hypothesized in AMAN, the usefulness of rituximab and corticosteroids in GBS, even if in the early phase, is still controversial [101, 102]. Putatively, autoantibody classification instead of early electrophysiology better predicts the final diagnosis and electrophysiological profiles of GBS [27]. In a European study, serum IgG antibodies were detected in over 80% of the patients with AMAN [103]. Fc gamma receptors of gangliosides can be targeted by autoantibodies, initiating MAC formation and axonal degeneration [104]. In murine experimental autoimmune neuritis (EAN), axonal degeneration was observed at onset (day 10 post-immunization), became severe at peak (day 16 post-immunization), and persisted during recovery (days 22–25 post-immunization) [105]. Autoantibodies induce both axon and myelin deficits through autoimmune reactivity simultaneously, but the potency of autoimmunity may differ [106]. PCB was identified accompanied with anti-GQ1b and anti-GT1a antibody in case studies [8, 34]. Interestingly, GT1a was found in the neuropil of the spinal cord dorsal horn and spinal trigeminal nucleus; GQ1b was mainly expressed in the paranodal myelin of oculomotor nerves, muscle spindle afferents, peripheral nerves, and reticular formation [107] (Fig. 3).
Molecular mimicry in GBS variants. C. jejuni or other pathogens synthesize GM1-, GD1a-, GT1a-, GD1c-, and GD3-like LOS and trigger anti-ganglioside antibody production. In AMAN, anti-GM1, and anti-GD1a antibodies target axolemmas located at anterior roots and nerve terminals, and cause limb weakness. In PCB, antibodies specifically against GT1a expressed at glossopharyngeal and vagal nerves lead to oropharyngeal and cervicobrachial weakness with areflexia. In MFS, anti-GQ1b and anti-GT1a antibodies bind to oculomotor, trochlear and abducens nerves and muscle spindles as well as Purkinje neurons in the cerebellum, causing ophthalmoplegia, areflexia and cerebellar ataxia. Anti-GQ1b and anti-GT1a antibodies also react with the reticular formation and introduce BBE. AMAN acute motor axonal neuropathy, BBE Bickerstaff brainstem encephalitis, C. jejuni Campylobacter jejuni, GBS Guillain–Barré syndrome, LOS lipooligosaccharide, MFS Miller Fisher syndrome, PCB pharyngeal-cervical-brachial weakness
However, the detection of autoantibodies has limitations. Although GQ1b antibody in serum has a relatively high specificity for MFS and BBE [108], most other anti-ganglioside antibodies have been proposed by only a few groups, with unknown reproducibility. Moreover, the antibody diagnosis for GBS is currently time-consuming and assay-dependent; hence, Leonhard et al. suggest not waiting for antibody test results before starting treatment [5]. A retrospective study in Islamabad reported negative anti-ganglioside antibodies in 15 patients with GBS, including 9 patients with axonal profiles in NCS [109]. Moreover, the antibody titer and affinity are not correlated to disease severity, although high titers of specific anti-GM1 antibody targeting cellular GM1 were more frequently detected in patients with severe GBS [110]. Collectively, limited specificity and sensitivity of anti-ganglioside antibodies, unknown pathogenetic role of diverse antibodies, and lack of reliable commercialized assay kits are the major concerns for utilizing antibodies as a diagnostic tool. Their utilization should be further optimized by using antibody-triggered GBS animal models or established models (e.g. the EAN model). Drugs that specifically target an antibody can be developed for precision medicine only when specific antibodies are confirmed to play a pivotal role in the etiology of axonal GBS.
Electrophysiological manifestations of axonal GBS
The classical electrophysiological criteria to differentiate GBS subtypes were put forward by Ho et al. [21] in 1995 and Hadden et al. [111] in 1998. Notably, electrophysiological studies in the early phase of GBS have occasionally yielded equivocal results [112]. Early-reversible changes on the axolemma may probably explain the rapid resolution of conduction slowing/block upon electrophysiological studies [51]. Thus electrophysiological studies 3–6 weeks after GBS onset may efficiently differentiate AMAN from AIDP [27]. In other words, the reduction patterns in serial recordings of RCFs at the axolemma of the node of Ranvier and the length-dependent CMAP caused by axonal degeneration can be later disclosed in AMAN [112]. By using sensitive and specific cut-off values for demyelination, Rajabally et al. proposed new criteria for electrodiagnosis in 2015 [113] (Table 3). If the criteria of neither AIDP nor axonal variants are met, a serial recording of distal motor latency (DML) and CMAP amplitudes is conducive to the differential diagnosis of GBS; patients without GBS have been characterized with prolonged DMLs and rapidly increasing CMAP amplitudes [114].
For the electrophysiological profiles of PCB, NCS showed prolongation of DMLs and F-wave latencies in median and ulnar nerves 4 days after PCB onset [115]. CBs at the cubital tunnel and decreased CMAP amplitudes between the Erb’s point and axilla were confirmed in these cases [115]. Collectively, NCS of PCB exhibits an axonal loss and polyradicular nerve involvement pattern, similar to the electrodiagnostic features of AMAN [116] (Table 4).
Genetic polymorphisms in axonal GBS
While GBS is not considered a genetic disease, host factors do play a role in the pathogenesis of GBS following C. jejuni infection [22]. The different morbidities of axonal GBS in Western and Asian countries could reflect genetic polymorphisms and may dictate individual sensitivity to diverse GBS variants [22, 25]. Patients with AMAN have been shown more likely to have the TNFA-863AA allele of a tumor necrosis factor (TNF)-α encoding gene than healthy controls [117], while patients with the TNFA-238A allele were more likely to develop anti-GM1 autoantibody [117]. Fas receptor-Fas ligand (Fas-FasL) is a classical apoptotic pathway involved in eliminating autoreactive B and T cells involved in molecular mimicry. Single nucleotide polymorphisms (SNPs) of Fas, including FAS-670G and FAS-1377G/-670G, were associated with elevated anti-GM1 antibody titers [118]. A meta-analysis illustrated that differentiating polymorphisms of HLA-DQB1 may facilitate GBS diagnosis: the HLA-DQB1*030 × polymorphism and HLA-DQB1*060 × polymorphism were significantly associated with Asian patients and all patients, respectively, when compared to healthy controls [119]. HLA-DQB1*0501-*0602 and DQB1*0201 alleles exhibited a difference between patients with C. jejuni-associated axonal GBS and AIDP, but this difference was not significant after Bonferroni corrections [120].
The genetic polymorphisms of C. jejuni may account for the severity and diversity of GBS. Eleven classes of new LOS loci were identified after sequencing LOS biosynthesis loci and LOS biosynthesis regions were found to be highly variable zones in C. jejuni strains [121]. A single-base deletion in a glycosyltransferase gene, cgtA, involved in LOS biosynthesis led to failed GT1a mimicry in the host [57]. Furthermore, the cst-II gene in C. jejuni has been shown to determine the terminal sugar regions of LOS to mimic different sugar residues of gangliosides; patients with cst-II (Thr51)-type C. jejuni antecedent infection were found more likely to have elevated anti-GM1 and anti-GD1a antibodies and to develop AMAN [122]. Orf10/orf11 genes regulate sialic acid biosynthesis and transfer during LOS biosynthesis, and their deficiency has been reported to attenuate the immune reactivity of plasma cells in GBS patients’ sera and prevent axonal degeneration in an AMAN mouse model [123]. H and P classes C. jejuni with nonsialylated LOS were detected in patients with GBS, which have different Orf28 and Orf39 deletion and insertion conditions, both contributing to truncated LOS [124]. NeuA1 also contributes to the biosynthesis of LOS; GBS cases triggered by C. jejuni with neuA1 deficiency showed ameliorated immune reactivity in sera [4]. Despite these genes being associated with C. jejuni virulence, whether C. jejuni-associated axonal GBS correlates with virulence is unclear. C. jejuni-associated infection was common, but few cases developed GBS. The risk of GBS in C. jejuni-infected cohorts may depend on the genetic backgrounds of individuals, variation in the virulence of C. jejuni, and the severity of infections. A genome-wide association study (GWAS) on a GBS cohort reported no significant associations in individual SNPs and imputed HLA types between patients with GBS and healthy controls [125]. To further understand these blind spots, larger GWAS studies for GBS cases and C. jejuni strains should be conducted to reveal the underlying interrelationship between genetic background, GBS epidemiology, and clinical characteristics.
Emerging diagnostic technologies
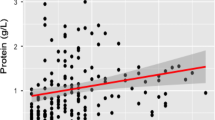
Electrophysiological studies and antibody classification have been used as basic diagnostic techniques [30]. Intriguingly, several newly developed technologies and biomarkers could assist the differentiation of GBS subtypes. For instance, soluble receptor for advanced glycation end products (sRAGE) can prevent degenerative or inflammatory neurological diseases by blocking expression of RAGE, an initiator of inflammation and oxidative stress [126]. sRAGE was decreased in the serum of patients with early phase AMAN, suggesting its potential as a sensitive biomarker [126]. In addition, levels of 55 plasma lipid metabolites showed significant differences between GBS and healthy controls after metabolomic analysis; patients with GBS were characterized with lower levels of creatinine, serotonin, and higher levels of isoleucine [11]. An integrative metabolomic approach was used to analyze CSF samples of 86 patients with GBS in Korea [127]. Significant elevations of lysophosphatidylcholines and sphingomyelins seemed unique for AIDP and AMAN; these lipids exhibited a potential association with the Hughes functional scale scores, according to a metabolome-wide multivariate correlation analysis [127]. Feature selection from datasets using a cluster algorithm provided a high purity of GBS characterization through artificial intelligence, implying a possibility for computer-assisted GBS diagnosis [10]. Imaging technologies like MRI may help exclude CNS disorders like stroke [5]. Peripheral nerve ultrasound, developed in recent years, can differentiate AIDP with a sensitivity > 85% [128]. Additionally, ultrasound indicators, including three sub-scores and ultrasound pattern sum scores, were significantly increased in chronic inflammatory demyelinating polyradiculoneuropathy but without evident changes in axonal GBS [129]. Nerve ultrasound may reveal segmental enlargement of spinal and proximal nerve roots in patients with GBS and MRI may show the thickening part of spinal nerve roots and cauda equina [130].
Cytokines and T-cell ratios can predict AMAN with considerable accuracy. For instance, elevated IL-23 and IL-27 levels have been identified in patients with AMAN [131]. The ratio of circulating memory T follicular helper (Tfh) subsets, Tfh2 and Tfh17 appears promising for identifying GBS subtypes: the ratio of (Tfh2 + Tfh17)/Tfh1 was significantly higher in AMAN than in AIDP [132]. Moreover, (Tfh2 + Tfh17)/Tfh1 ratio is a promising biomarker for predicting the severity and progression of AMAN [132].
The diagnostic accuracy of axonal GBS could be improved. Particularly, whether autoimmune antibodies can be used as clinical biomarkers of axonal GBS merits further investigation. Electrophysiological studies have not been able to define a part of GBS; serial electrophysiological recordings and new criteria are in urgent need for the undefined GBS subtypes. Different criteria of electrophysiology should be compared for a better definition of electrophysiological profiles for axonal GBS. Likewise, the diagnostic value of imaging methods, including MRI and nerve ultrasound, awaits corroboration for accurate diagnosis. Taken together, electrophysiology remains a mainstay in the diagnosis of axonal GBS, although the electrophysiological criteria of regional GBS have yet to reach consensus.
Canonical and advanced treatments for AMAN
Despite persistent efforts in laboratory and preclinical studies, treatments for patients with AMAN still rely on IVIg and plasma exchange (PE) [133,134,135]. Corticosteroids have been proven useless and even detrimental in patients on mechanical ventilation (MV) or after the acute phase [136]. IVIg mainly functions by inhibiting macrophage activation and preventing the binding of antibodies and complements [133]. IVIg may dimerize anti-ganglioside IgG antibodies and remonomerize IgG dimers to disable autoantibodies whereby mitigating immunoreactivity in patients’ sera [137]. IVIg efficacy has been shown to differ between AMAN and AIDP: a higher Hughes functional grading scale (HFGS) score was observed in patients with AMAN after IVIg treatment compared to those with AIDP; however, only 24% of AMAN patients experienced rapid recovery after IVIg treatment [138]. Regarding pediatric cases, children with AMAN respond better to IVIg [139]. AMAN patients with CBs displayed a higher reduction of HFGS after IVIg treatment compared to those without CBs and patients with AIDP [140]. In contrast, investigation of the long-term prognosis of GBS patients revealed that IVIg treatment did not improve the long-term outcomes of patients [141]. In current practice, patients with treatment-related fluctuations and treatment failures are frequently retreated with a second course of IVIg or PE [142], despite inconsistent conclusions from clinical observations [143, 144].
PE is usually conducted as five sessions with 40–50 mL plasma/kg per session within 7–14 days, which remarkably hastens recovery compared to supportive care alone [145]. IVIg started at the 2nd week after onset achieved comparable benefits without an increase of adverse events [133]. A recent pilot study reported that combined use of IVIg and PE reduced mortality, facilitated earlier weaning from MV, and shortened hospital stay, with an excellent outcome in AMAN patients who required intensive care [146]. In fact, PE scavenges pathogenetic antibodies and IVIg neutralizes or blocks pathogenetic antibodies [143, 147], implying that either PE or IVIg is more effective in patients with ganglioside autoantibody-associated axonal GBS than those with lymphocyte infiltration-dominated AIDP. Theoretically, the use of PE followed by IVIg can be a more effective and safer treatment for patients with GBS. Notwithstanding, a previous study illustrated that IVIg after PE did not provide any extra benefit [133]. To optimize treatment of axonal GBS, whether the combination of PE and IVIg facilitates prognosis of axonal GBS remains to be explored. Clinical trials testing PE or IVIg efficacy can put more emphasis on treating axonal GBS because of its pathogenic humoral immune response.
Newly developed drugs, including rEV576 [148], erythropoietin [149], cysteine protease [150], and nafamostat mesilate (NM) [151], targeting the hyperreactive immune responses in AMAN exhibited promising therapeutic potentials in GBS animal models. Monoclonal antibodies against eculizumab [152], anti-C1q [153], anti-GD3, anti-idiotype [154], anti-IL-17 [14], anti-CD2, and anti-selectin [101] inhibit the initiation of complement deposition, and MAC, immune cell recruitment, and axonal injury are attenuated in GBS animal models. Evidence suggests that complement inhibition combined with IVIg might improve outcome in GBS [155]. In line with these findings, eculizumab was tested in a multicenter, double-blind, randomized phase 2 clinical trial, and 61% of patients with GBS in the eculizumab-treated group were able to walk independently after 4 weeks compared to 45% in the placebo control group [13]. Rituximab, an anti-CD20 monoclonal antibody, was demonstrated to facilitate EBV resolution and muscle strength recovery in an allogeneic hematopoietic stem cell transplantation-triggered AMAN case [12]. IFN-β can decrease adhesion and transmigration capacities of lymphocytes extracted from GBS patients' blood [156]. In spite of this, a randomized controlled clinical trial involving 13 patients treated with IFN-β and IVIg showed insignificant difference in any efficacy measure compared to six patients treated with placebo and IVIg [157]. Further, no benefits were verified in improving progressive limb weakness or motor deficits of patients after applying OKT3, an anti-T-cell monoclonal antibody [158]. Thus far, no biological drugs have been approved by the FDA; more preclinical investigations to identify their efficacy and side effects are under way [101].
Vitamin deficiency can induce peripheral neuropathy [159], and serum folate was found to correlate with GBS severity and progression duration [160]. Likewise, nutritional loss caused by bariatric surgery or alcoholism may lead to poor nutritional status and worsen the prognosis in patients with axonal neuropathy [161]. Hence, neurotrophic therapies, including vitamin supplementation, might benefit the outcome of GBS. To normalize the inconsistent therapies, Leonhard et al. summarized ten steps in GBS diagnosis and management from early GBS suspicion to final rehabilitation, providing an acceptable standard for effective GBS treatment [5]. Even with those traditional or advanced therapies, sequelae are frequent, highlighting the importance of rehabilitation after discharge.
Whether the combination of PE and IVIg facilitates the prognosis of axonal GBS remains to be explored. Potential therapies using monoclonal antibodies to target pro-inflammatory cytokines or complements should be further investigated and translated into clinical practice (Table 5). Importantly, strategies to impede relapses and reduce complications (i.e., pressure ulcers, infection, deep vein thrombosis, and hospital-associated psychiatric disorders, among others) should be integrated to achieve a better prognosis. More importantly, it remains an unmet need to identify self-limited cases in the outpatient settings so as to avoid unnecessary treatment and to alleviate iatrogenic injury.
Conclusions
Axonal GBS is unique as to its pathogenesis being autoantibody-mediated immune responses to incompletely characterized antigens that exist in the axolemma or the node of Ranvier with subsequent axonal degeneration. C. jejuni and ganglioside administration-triggered molecular mimicry are specific pathogenic factors when comparing axonal GBS with other subtypes. Decreased CMAP amplitudes and RCFs are typical electrophysiological features of axonal GBS. Serial electrophysiological recordings may identify reversible nerve conduction block and help differentiate axonal GBS from AIDP. Potential biomarkers, like autoantibody classification, can assist in differentiating between axonal subtypes, including AMAN/AMSAN and PCB, and other biomarkers (i.e., lipid metabolites, sRAGE, lysophosphatidylcholines, and sphingomyelins, among others) are still under investigation. Until now, IVIg and PE have still been the mainstay for the treatment of either AIDP or axonal GBS. Monoclonal antibodies, including eculizumab, rituximab, and alemtuzumab, have shown preliminary potentials; however, more clinical trials are needed to validate their efficacy and identify possible side effects. To further investigate novel therapeutic targets of axonal GBS, the animal model for AMAN should be optimized. Large GWAS studies on patients with axonal GBS may identify the correlation between genetic background and disease onset of axonal GBS. More sensitive biomarkers should be investigated to differentiate between moderate GBS and self-limiting courses. Moreover, infection-associated and vaccination-associated GBS surveillance networks should be consolidated.
References
Guillain G, Barré J, Strohl A (1916) Sur un syndrome de radiculonevrite avec hyperalbuminose du liquide cephalo-rachidien sans reaction cellulaire: remarques sur les caracteres cliniques et graphiques des reflexes tendineux. Bull Mem Soc Med Hop Paris 28:1462–1470
Sejvar JJ, Baughman AL, Wise M, Morgan OW (2011) Population Incidence of Guillain–Barré syndrome: a systematic review and meta-analysis. Neuroepidemiology 36:123–133. https://doi.org/10.1159/000324710
Benedetti L, Briani C, Beronio A et al (2019) Increased incidence of axonal Guillain–Barré syndrome in La Spezia area of Italy: A 13-year follow-up study. J Peripher Nerv Syst 24:80–86. https://doi.org/10.1111/jns.12292
Yuki N (2012) Guillain–Barré syndrome and anti-ganglioside antibodies: a clinician-scientist’s journey. Proc Jpn Acad Ser B Phys Biol Sci 88:299–326. https://doi.org/10.2183/pjab.88.299
Leonhard SE, Mandarakas MR, Gondim FAA et al (2019) Diagnosis and management of Guillain–Barré syndrome in ten steps. Nat Rev Neurol 15:671–683. https://doi.org/10.1038/s41582-019-0250-9
Zeng Y, Liu Y, Xie Y et al (2019) Clinical features and the validation of the Brighton criteria in Guillain–Barré syndrome: retrospective analysis of 72 hospitalized patients in three years. Eur Neurol 81:231–238. https://doi.org/10.1159/000503101
van Doorn PA, Ruts L, Jacobs BC (2008) Clinical features, pathogenesis, and treatment of Guillain–Barré syndrome. Lancet Neurol 7:939–950. https://doi.org/10.1016/S1474-4422(08)70215-1
Dimachkie MM, Barohn RJ (2013) Guillain–Barré syndrome and variants. Neurol Clin 31:491–510. https://doi.org/10.1016/j.ncl.2013.01.005
Peric S, Milosevic V, Berisavac I et al (2014) Clinical and epidemiological features of Guillain–Barré syndrome in the Western Balkans. J Peripher Nerv Syst 19:317–321. https://doi.org/10.1111/jns.12096
Hernández-Torruco J, Canul-Reich J, Frausto-Solís J, Méndez-Castillo JJ (2014) Feature selection for better identification of subtypes of Guillain–Barré syndrome. Comput Math Methods Med 2014:432109. https://doi.org/10.1155/2014/432109
Tang HY, Chiu DT, Lin JF et al (2017) Disturbance of plasma lipid metabolic profile in Guillain–Barré syndrome. Sci Rep 7:8140. https://doi.org/10.1038/s41598-017-08338-7
Ostronoff F, Perales MA, Stubblefield MD, Hsu KC (2008) Rituximab-responsive Guillain–Barré syndrome following allogeneic hematopoietic SCT. Bone Marrow Transpl 42:71–72. https://doi.org/10.1038/bmt.2008.81
Misawa S, Kuwabara S, Sato Y et al (2018) Safety and efficacy of eculizumab in Guillain–Barré syndrome: a multicentre, double-blind, randomised phase 2 trial. Lancet Neurol 17:519–529. https://doi.org/10.1016/S1474-4422(18)30114-5
Ebrahim Soltani Z, Rahmani F, Rezaei N (2019) Autoimmunity and cytokines in Guillain–Barré syndrome revisited: review of pathomechanisms with an eye on therapeutic options. Eur Cytokine Netw 30:1–14. https://doi.org/10.1684/ecn.2019.0424
Hughes RAC, Cornblath DR, Willison HJ (2016) Guillain–Barré syndrome in the 100 years since its description by Guillain, Barré and Strohl. Brain 139:3041–3047. https://doi.org/10.1093/brain/aww247
Hughes RAC (2020) Guillain–Barré syndrome: looking back… and forward. J Neurol Neurosurg Psychiatry 91:111–112. https://doi.org/10.1136/jnnp-2019-322361
Sliman NA (1978) Outbreak of Guillain–Barré syndrome associated with water pollution. Br Med J 1:751–752. https://doi.org/10.1136/bmj.1.6115.751
Feasby TE, Gilbert JJ, Brown WF et al (1986) An acute axonal form of Guillain–Barré polyneuropathy. Brain 109:1115–1126. https://doi.org/10.1093/brain/109.6.1115
McKhann GM, Cornblath DR, Griffin JW et al (1993) Acute motor axonal neuropathy: a frequent cause of acute flaccid paralysis in China. Ann Neurol 33:333–342. https://doi.org/10.1002/ana.410330402
Ye Y, Zhu D, Wang K et al (2010) Clinical and electrophysiological features of the 2007 Guillain–Barré syndrome epidemic in northeast China. Muscle Nerve 42:311–314. https://doi.org/10.1002/mus.21701
Ho TW, Mishu B, Li CY et al (1995) Guillain–Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain 118:597–605. https://doi.org/10.1093/brain/118.3.597
Kaida K, Ariga T, Yu RK (2009) Antiganglioside antibodies and their pathophysiological effects on Guillain–Barré syndrome and related disorders—a review. Glycobiology 19:676–692. https://doi.org/10.1093/glycob/cwp027
Yuki N, Yamada M, Koga M et al (2001) Animal model of axonal Guillain–Barré syndrome induced by sensitization with GM1 ganglioside. Ann Neurol 49:712–720. https://doi.org/10.1002/ana.1012
Doets AY, Verboon C, van den Berg B et al (2018) Regional variation of Guillain–Barré syndrome. Brain 141:2866–2877. https://doi.org/10.1093/brain/awy232
Tian J, Cao C, Li T et al (2019) Electrophysiological subtypes and prognostic factors of Guillain–Barré syndrome in Northern China. Front Neurol 10:714. https://doi.org/10.3389/fneur.2019.00714
Bae JS, Yuki N, Kuwabara S et al (2014) Guillain–Barré syndrome in Asia. J Neurol Neurosurg Psychiatry 85:907–913. https://doi.org/10.1136/jnnp-2013-306212
Sekiguchi Y, Uncini A, Yuki N et al (2012) Antiganglioside antibodies are associated with axonal Guillain–Barré syndrome: a Japanese-Italian collaborative study. J Neurol Neurosurg Psychiatry 83:23–28. https://doi.org/10.1136/jnnp-2011-300309
Khaiboullina S, Uppal T, Martynova E et al (2018) History of ZIKV infections in India and management of disease outbreaks. Front Microbiol 9:2126. https://doi.org/10.3389/fmicb.2018.02126
Hao Y, Wang W, Jacobs BC et al (2019) Antecedent infections in Guillain–Barré syndrome: a single-center, prospective study. Ann Clin Transl Neurol 6:2510–2517. https://doi.org/10.1002/acn3.50946
van den Berg B, Walgaard C, Drenthen J et al (2014) Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol 10:469–482. https://doi.org/10.1038/nrneurol.2014.121
Ilyas AA, Willison HJ, Quarles RH et al (1988) Serum antibodies to gangliosides in Guillain–Barré syndrome. Ann Neurol 23:440–447. https://doi.org/10.1002/ana.410230503
Yuki N, Hartung HP (2012) Guillain–Barré syndrome. N Engl J Med 366:2294–2304. https://doi.org/10.1056/NEJMra1114525
Wakerley BR, Uncini A, Yuki N (2014) Guillain–Barré and Miller Fisher syndromes—new diagnostic classification. Nat Rev Neurol 10:537–544. https://doi.org/10.1038/nrneurol.2014.138
Wakerley BR, Yuki N (2014) Pharyngeal-cervical-brachial variant of Guillain–Barré syndrome. J Neurol Neurosurg Psychiatry 85:339–344. https://doi.org/10.1136/jnnp-2013-305397
Pukin AV, Jacobs BC, Tio-Gillen AP et al (2011) Detection of antibodies in neuropathy patients by synthetic GM1 mimics. Glycobiology 21:1642–1650. https://doi.org/10.1093/glycob/cwr093
Chiba A, Kusunoki S, Obata H et al (1993) Serum anti-GQ1b IgG antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain–Barré syndrome: clinical and immunohistochemical studies. Neurology 43:1911–1917. https://doi.org/10.1212/wnl.43.10.1911
Al Othman B, Raabe J, Kini A, Lee AG (2019) Update: the Miller Fisher variants of Guillain–Barré syndrome. Curr Opin Ophtalmol 30:462–466. https://doi.org/10.1097/ICU.0000000000000611
Shahrizaila N, Yuki N (2013) Bickerstaff brainstem encephalitis and Fisher syndrome: anti-GQ1b antibody syndrome. J Neurol Neurosurg Psychiatry 84:576–583. https://doi.org/10.1136/jnnp-2012-302824
Kornberg AJ, Pestronk A, Blume GM et al (1996) Selective staining of the cerebellar molecular layer by serum IgG in Miller-Fisher and related syndromes. Neurology 47:1317–1320. https://doi.org/10.1212/wnl.47.5.1317
Ishii J, Yuki N, Kawamoto M et al (2016) Recurrent Guillain–Barré syndrome, Miller Fisher syndrome and Bickerstaff brainstem encephalitis. J Neurol Sci 364:59–64. https://doi.org/10.1016/j.jns.2016.03.008
Notturno F, Kokubun N, Sekiguki Y et al (2016) Demyelinating Guillain–Barré syndrome recurs more frequently than axonal subtypes. J Neurol Sci 365:132–136. https://doi.org/10.1016/j.jns.2016.02.053
Sekiguchi Y, Mori M, Misawa S et al (2016) How often and when Fisher syndrome is overlapped by Guillain–Barré syndrome or Bickerstaff brainstem encephalitis? Eur J Neurol 23:1058–1063. https://doi.org/10.1111/ene.12983
Greco A, Gallo A, Fusconi M et al (2012) Bell’s palsy and autoimmunity. Autoimmun Rev 12:323–328. https://doi.org/10.1016/j.autrev.2012.05.008
Inaloo S, Katibeh P (2014) Guillain–Barré syndrome presenting with bilateral facial nerve palsy. Iran J Child Neurol 8:70–72. https://doi.org/10.22037/ijcn.v8i1.4258
Gómez Á, Díaz A, Carrión-Penagos J et al (2019) Clinical and electrophysiological characteristics of Guillain–Barré syndrome in Colombia. J Peripher Nerv Syst 24:268–271. https://doi.org/10.1111/jns.12340
Wakisaka H, Hato N, Honda N et al (2002) Demyelination associated with HSV-1-induced facial paralysis. Exp Neurol 178:68–79. https://doi.org/10.1006/exnr.2002.8035
McGrogan A, Madle GC, Seaman HE, de Vries CS (2009) The epidemiology of Guillain–Barré syndrome worldwide. A systematic literature review. Neuroepidemiology 32:150–163. https://doi.org/10.1159/000184748
Liu S, Xiao Z, Lou M et al (2018) Guillain–Barré syndrome in southern China: retrospective analysis of hospitalised patients from 14 provinces in the area south of the Huaihe River. J Neurol Neurosurg Psychiatry 89:618–626. https://doi.org/10.1136/jnnp-2017-316930
Drenthen J, Yuki N, Meulstee J et al (2011) Guillain–Barré syndrome subtypes related to Campylobacter infection. J Neurol Neurosurg Psychiatry 82:300–305. https://doi.org/10.1136/jnnp.2010.226639
Sivadon-Tardy V, Porcher R, Orlikowski D et al (2014) Increased incidence of Campylobacter jejuni-associated Guillain–Barré syndromes in the Greater Paris area. Epidemiol Infect 142:1609–1613. https://doi.org/10.1017/S095026881300263X
Ogawara K, Kuwabara S, Mori M et al (2000) Axonal Guillain–Barré syndrome: relation to anti-ganglioside antibodies and Campylobacter jejuni infection in Japan. Ann Neurol 48:624–631. https://doi.org/10.1002/1531-8249(200010)48:4%3c624:AID-ANA9%3e3.0.CO;2-O
Mori M, Kuwabara S, Miyake M et al (2000) Haemophilus influenzae infection and Guillain Barré syndrome. Brain 123:2171–2178. https://doi.org/10.1093/brain/123.10.2171
Hameed A (2019) Human immunity against campylobacter infection. Immune Netw 19:e38. https://doi.org/10.4110/in.2019.19.e38
Yuki N, Susuki K, Koga M et al (2004) Carbohydrate mimicry between human ganglioside GM1 and Campylobacter jejuni lipooligosaccharide causes Guillain–Barré syndrome. PNAS 101:11404–11409. https://doi.org/10.1073/pnas.0402391101
Yuki N, Taki T, Inagaki F et al (1993) A bacterium lipopolysaccharide that elicits Guillain–Barre syndrome has a GM1 ganglioside-like structure. J Exp Med 178:1771–1775. https://doi.org/10.1084/jem.178.5.1771
Yuki N, Taki T, Takahashi M et al (1994) Penner’s serotype 4 of Campylobacter jejuni has a lipopolysaccharide that bears a GM1 ganglioside epitope as well as one that bears a GD1a epitope. Infect Immun 62:2101–2103
Zhang M, Gilbert M, Yuki N et al (2015) Association of anti-GT1a antibodies with an outbreak of Guillain–Barré syndrome and analysis of ganglioside mimicry in an associated campylobacter jejuni strain. PLoS ONE 10:e0131730. https://doi.org/10.1371/journal.pone.0131730
Koga M, Gilbert M, Li J, Yuki N (2015) Complex of GM1- and GD1a-Like lipo-oligosaccharide mimics GM1b, inducing anti-GM1b antibodies. PLoS ONE 10:e0124004. https://doi.org/10.1371/journal.pone.0124004
Loshaj-Shala A, Regazzoni L, Daci A et al (2015) Guillain Barré syndrome (GBS): new insights in the molecular mimicry between C. jejuni and human peripheral nerve (HPN) proteins. J Neuroimmunol 289:168–176. https://doi.org/10.1016/j.jneuroim.2015.11.005
Kusunoki S, Shiina M, Kanazawa I (2001) Anti-Gal-C antibodies in GBS subsequent to mycoplasma infection: evidence of molecular mimicry. Neurology 57:736–738. https://doi.org/10.1212/wnl.57.4.736
Brasil P, Sequeira PC, Freitas AD et al (2016) Guillain–Barré syndrome associated with Zika virus infection. Lancet 387:1482. https://doi.org/10.1016/S0140-6736(16)30058-7
Lynch RM, Mantus G, Encinales L et al (2019) Augmented Zika and dengue neutralizing antibodies are associated with Guillain–Barré syndrome. J Infect Dis 219:26–30. https://doi.org/10.1093/infdis/jiy466
Parra B, Lizarazo J, Jiménez-Arango JA et al (2016) Guillain–Barré syndrome associated with Zika virus infection in Colombia. N Engl J Med 375:1513–1523. https://doi.org/10.1056/NEJMoa1605564
Cao-Lormeau VM, Blake A, Mons S et al (2016) Guillain–Barré syndrome outbreak associated with Zika virus infection in French Polynesia. Lancet 387:1531–1539. https://doi.org/10.1016/S0140-6736(16)00562-6
GeurtsvanKessel CH, Islam Z, Islam MB et al (2018) Zika virus and Guillain–Barré syndrome in Bangladesh. Ann Clin Transl Neurol 5:606–615. https://doi.org/10.1002/acn3.556
Styczynski AR, Malta JMAS, Krow-Lucal ER et al (2017) Increased rates of Guillain–Barré syndrome associated with Zika virus outbreak in the Salvador metropolitan area. Brazil PLoS Negl Trop Dis 11:e0005869. https://doi.org/10.1371/journal.pntd.0005869
Dirlikov E, Major CG, Medina NA et al (2018) Clinical features of Guillain–Barré syndrome with vs without Zika virus infection, Puerto Rico, 2016. JAMA Neurol 75:1089–1097. https://doi.org/10.1001/jamaneurol.2018.1058
Sánchez-San Martín C, Li T, Bouquet J et al (2018) Differentiation enhances Zika virus infection of neuronal brain cells. Sci Rep 8:14543. https://doi.org/10.1038/s41598-018-32400-7
Nem de Oliveira Souza I, Frost PS, França JV et al (2018) Acute and chronic neurological consequences of early-life zika virus infection in mice. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aar2749
Al-Saffar A, Al-Fatly B (2018) Acute Motor Axonal Neuropathy in Association with Hepatitis E. Front Neurol 9:62. https://doi.org/10.3389/fneur.2018.00062
Kutleša M, Santini M, Krajinović V et al (2010) Acute motor axonal neuropathy associated with pandemic H1N1 influenza A infection. Neurocrit Care 13:98–100. https://doi.org/10.1007/s12028-010-9365-y
Van der Meché FG, Van Doorn PA, Meulstee J, Jennekens FG, GBS-consensus group of the Dutch Neuromuscular Research Support Centre (2001) Diagnostic and classification criteria for the Guillain–Barré syndrome. Eur Neurol 45:133–139. https://doi.org/10.1159/000052111
Kuwabara S, Yuki N (2013) Axonal Guillain–Barré syndrome: Concepts and controversies. Lancet Neurol 12:1180–1188. https://doi.org/10.1016/S1474-4422(13)70215-1
Shi M, Zhu J, Deng H (2019) Clinical characteristics of intravenous injection of Monosialotetrahexosyl Ganglioside Sodium-Related Guillain–Barré syndrome. Front Neurol 10:225. https://doi.org/10.3389/fneur.2019.00225
Odaka M, Yuki N, Nobile-Orazio E et al (2000) Antibodies to GM1(NeuGc) in Guillain–Barré syndrome after ganglioside therapy. J Neurol Sci 175:96–106. https://doi.org/10.1016/S0022-510X(00)00287-2
Figueras A, Morales-olivas FJ, Capellà D et al (1992) Bovine gangliosides and acute motor polyneuropathy. BMJ 305:1330–1331. https://doi.org/10.1136/bmj.305.6865.1330
Govoni V, Granieri E, Casetta I et al (1996) The incidence of Guillain–Barré syndrome in Ferrara, Italy: Is the disease really increasing? J Neurol Sci 137:62–68. https://doi.org/10.1016/0022-510X(95)00333-W
Govoni V, Granieri E, Manconi M et al (2003) Is there a decrease in Guillain–Barré syndrome incidence after bovine ganglioside withdrawal in Italy? A population-based study in the Local Health District of Ferrara, Italy. J Neurol Sci 216:99–103. https://doi.org/10.1016/S0022-510X(03)00215-6
Wu X, Wu W, Wang Z et al (2014) More severe manifestations and poorer short-term prognosis of ganglioside-associated Guillain–Barré syndrome in northeast China. PLoS ONE 9:e010474. https://doi.org/10.1371/journal.pone.0104074
Díez-Tejedor, E, Gutiérrez-Rivas, E, Gil-Peralta A (1993) Gangliosides and Guillain–Barré syndrome: the Spanish data. Neuroepidemiology 12:251–256. https://doi.org/10.1159/000110325
Sejvar JJ, Kohl KS, Gidudu J et al (2011) Guillain–Barré syndrome and Fisher syndrome: Case definitions and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine 29:599–612. https://doi.org/10.1016/j.vaccine.2010.06.003
Haber P, Sejvar J, Mikaeloff Y, Destefano F (2009) Vaccines and Guillain–Barré syndrome. Drug Saf 32:309–323. https://doi.org/10.2165/00002018-200932040-00005
Breman JG, Hayner NS (1984) Guillain–Barré syndrome and its relationship to swine influenza vaccination in Michigan, 1976–1977. Am J Epidemiol 119:880–889. https://doi.org/10.1093/oxfordjournals.aje.a113810
Sanz Fadrique R, Martín Arias L, Molina-Guarneros JA et al (2019) Guillain–Barré syndrome and influenza vaccines: current evidence. Rev Esp Quimioter 32:288–295
Vellozzi C, Iqbal S, Broder K (2014) Guillain–Barré syndrome, influenza, and influenza vaccination: the epidemiologic evidence. Clin Infect Dis 58:1149–1155. https://doi.org/10.1093/cid/ciu005
Nelson KE (2012) Invited commentary: influenza vaccine and Guillain–Barré syndrome—Is there a risk? Am J Epidemiol 175:1129–1132. https://doi.org/10.1093/aje/kws194
Salmon DA, Proschan M, Forshee R et al (2013) Association between Guillain–Barré syndrome and influenza A (H1N1) 2009 monovalent inactivated vaccines in the USA: a meta-analysis. Lancet 381:1461–1468. https://doi.org/10.1016/S0140-6736(12)62189-8
Kwong JC, Vasa PP, Campitelli MA et al (2013) Risk of Guillain–Barré syndrome after seasonal influenza vaccination and influenza health-care encounters: a self-controlled study. Lancet Infect Dis 13:769–776. https://doi.org/10.1016/S1473-3099(13)70104-X
Ojha RP, Jackson BE, Tota JE et al (2014) Guillain–Barré syndrome following quadrivalent human papillomavirus vaccination among vaccine-eligible individuals in the United States. Hum Vaccines Immunother 10:232–237. https://doi.org/10.4161/hv.26292
Deceuninck G, Sauvageau C, Gilca V et al (2018) Absence of association between Guillain–Barré syndrome hospitalizations and HPV-vaccine. Expert Rev Vaccines 17:99–102. https://doi.org/10.1080/14760584.2018.1388168
Romio S, Weibel D, Dieleman JP et al (2014) Guillain–Barré syndrome and adjuvanted pandemic influenza A (H1N1) 2009 vaccines: a multinational self-controlled case series in Europe. PLoS ONE 9:e82222. https://doi.org/10.1371/journal.pone.0082222
Chen Y, Zhang J, Chu X et al (2019) Vaccines and the risk of Guillain–Barré syndrome. Eur J Epidemiol. https://doi.org/10.1007/s10654-019-00596-1
De Wals P, Deceuninck G, Toth E et al (2012) Risk of Guillain–Barré syndrome following H1N1 influenza vaccination in Quebec. JAMA 308:175–181. https://doi.org/10.1001/jama.2012.7342
Sakai H, Harun FM, Yamamoto N, Yuki N (2012) Contamination with gangliosides in brain-derived rabies vaccine may trigger Guillain–Barré syndrome. J Neurol Neurosurg Psychiatry 83:467–469. https://doi.org/10.1136/jnnp-2011-301102
Green DM, Ropper AH (2001) Mild Guillain–Barre syndrome. Arch Neurol 58:1098–1101. https://doi.org/10.1001/archneur.58.7.1098
Créange A (2000) A role for interferon-beta in Guillain–Barré Syndrome? BioDrugs 14:1–11. https://doi.org/10.2165/00063030-200014010-00001
Ilyas AA, Chen ZW, Cook SD et al (2001) Immunoglobulin G subclass distribution of autoantibodies to gangliosides in patients with Guillain–Barre syndrome. Res Commun Mol Pathol Pharmacol 109:115–123
Liu S, Dong C, Ubodu EE (2018) Immunotherapy of Guillain–Barré syndrome. Hum Vaccin Immunother 14:2568–2579. https://doi.org/10.1080/21645515.2018.1493415
Burnor E, Yang L, Zhou H et al (2018) Neurofascin antibodies in autoimmune, genetic, and idiopathic neuropathies. Neurology 90:e31–e38. https://doi.org/10.1212/wnl.0000000000004773
Koga M, Takahashi M, Yokoyama K, Kanda T (2015) Ambiguous value of anti-ganglioside IgM autoantibodies in Guillain–Barré syndrome and its variants. J Neurol 262:1954–1960. https://doi.org/10.1007/s00415-015-7806-4
Motamed-Gorji N, Matin N, Tabatabaie O et al (2017) Biological drugs in Guillain–Barré syndrome: an update. Curr Neuropharmacol 15:938–950. https://doi.org/10.2174/1570159X14666161213114904
Guillain–Barré Syndrome Steroid Trial Group (1993) Double-blind trial of intravenous methylprednisolone in Guillain–Barré syndrome. Lancet 341:586–590. https://doi.org/10.1016/0140-6736(93)90351-G
Galban-Horcajo F, Fitzpatrick AM, Hutton AJ et al (2013) Antibodies to heteromeric glycolipid complexes in multifocal motor neuropathy. Eur J Neurol 20:62–70. https://doi.org/10.1111/j.1468-1331.2012.03767.x
He L, Zhang G, Liu W et al (2015) Anti-ganglioside antibodies induce nodal and axonal injury via Fcγ receptor-mediated inflammation. J Neurosci 35:6770–6785. https://doi.org/10.1523/JNEUROSCI.4926-14.2015
Tomikawa E, Mutsuga M, Hara K et al (2019) Time course of axon and myelin degeneration in peripheral nerves in experimental autoimmune neuritis rats. Toxicol Pathol 47:542–552. https://doi.org/10.1177/0192623319838993
Susuki K, Yuki N, Schafer DP et al (2012) Dysfunction of nodes of Ranvier: a mechanism for anti-ganglioside antibody-mediated neuropathies. Exp Neurol 233:534–542. https://doi.org/10.1016/j.expneurol.2011.11.039
Irie F, Hashikawa T, Tai T et al (1994) Distribution of cholinergic neuron-specific gangliosides (GT1aα and GQ1bα) in the rat central nervous system. Brain Res 665:161–166. https://doi.org/10.1016/0006-8993(94)91169-X
Spatola M, Du Pasquier R, Schluep M, Regeniter A (2016) Serum and CSF GQ1b antibodies in isolated ophthalmologic syndromes. Neurology 86:1780–1784. https://doi.org/10.1212/WNL.0000000000002558
Saeed ML, Kaleem Baloch B, Mahmud SN et al (2019) Role of anti-ganglioside antibodies in the diagnosis of Guillain–Barré syndrome as an alternate investigation. Cureus 11:e4625. https://doi.org/10.7759/cureus.4625
Lardone RD, Yuki N, Odaka M et al (2010) Anti-GM1IgG antibodies in Guillain–Barré syndrome: fine specificity is associated with disease severity. J Neurol Neurosurg Psychiatry 81:629–633. https://doi.org/10.1136/jnnp.2009.183665
Hadden RD, Cornblath DR, Hughes RA et al (1998) Electrophysiological classification of Guillain–Barré syndrome: clinical associations and outcome. Ann Neurol 44:780–788. https://doi.org/10.1002/ana.410440512
Uncini A, Manzoli C, Notturno F, Capasso M (2010) Pitfalls in electrodiagnosis of Guillain–Barré syndrome subtypes. J Neurol Neurosurg Psychiatry 81:1157–1163. https://doi.org/10.1136/jnnp.2010.208538
Rajabally YA, Durand MC, Mitchell J et al (2015) Electrophysiological diagnosis of Guillain–Barré syndrome subtype: could a single study suffice? J Neurol Neurosurg Psychiatry 86:115–119. https://doi.org/10.1136/jnnp-2014-307815
Hosokawa T, Nakajima H, Unoda K et al (2016) Serial electrophysiological findings in Guillain–Barré syndrome not fulfilling AIDP or AMAN criteria. J Neurol 263:1709–1718. https://doi.org/10.1007/s00415-016-8192-2
Miyagi T, Higa K, Kido M et al (2017) The Sequential ultrasonographic, electrophysiological and MRI findings in a patient with the pharyngeal-cervical-brachial variant of Guillain–Barré syndrome from the acute phase to the chronic phase. Intern Med 56:1225–1230. https://doi.org/10.2169/internalmedicine.56.7807
Soriano Caminero A, Ahmed A (2013) Clinical and electrodiagnostic presentation of pharyngeal-cervical-brachial variant of Guillain–Barré syndrome. Neurology 80:P07.060 LP–P07.060
Jahan I, Ahammad RU, Farzana KS et al (2017) Tumor necrosis factor-alpha-863C/A polymorphism is associated with Guillain–Barré syndrome in Bangladesh. J Neuroimmunol 310:46–50. https://doi.org/10.1016/j.jneuroim.2017.06.005
Islam Z, Jahan I, Ahammad RU et al (2018) FAS promoter polymorphisms and serum sFas level are associated with increased risk of nerve damage in Bangladeshi patients with Guillain–Barré syndrome. PLoS ONE 13:e0192703. https://doi.org/10.1371/journal.pone.0192703
Jin PP, Sun LL, Ding BJ et al (2015) Human leukocyte antigen DQB1 (HLA-DQB1) Polymorphisms and the risk for Guillain–Barré syndrome: a systematic review and meta-analysis. PLoS ONE 10:e0131374. https://doi.org/10.1371/journal.pone.0131374
Hayat S, Jahan I, Das A et al (2019) Human leukocyte antigen-DQB1 polymorphisms and haplotype patterns in Guillain–Barré syndrome. Ann Clin Transl Neurol 6:1849–1857. https://doi.org/10.1002/acn3.50884
Parker CT, Gilbert M, Yuki N et al (2008) Characterization of lipooligosaccharide-biosynthetic loci of Campylobacter jejuni reveals new lipooligosaccharide classes: evidence of mosaic organizations. J Bacteriol 190:5681–5689. https://doi.org/10.1128/JB.00254-08
Koga M, Takahashi M, Masuda M et al (2005) Campylobacter gene polymorphism as a determinant of clinical features of Guillain–Barré syndrome. Neurology 65:1376–1381. https://doi.org/10.1212/01.wnl.0000176914.70893.14
Komagamine T, Yuki N (2006) Ganglioside mimicry as a cause of Guillain–Barré syndrome. CNS Neurol Disord Drug Targets 5:391–400. https://doi.org/10.2174/187152706777950765
Jiang H, Zhang MJ, Liu RC et al (2010) Characteristics of lipo-oligosaccharide loci of Campylobacter jejuni isolates associated with Guillain–Barré syndrome from Hebei, China. Int J Mol Sci 11:1155–1161. https://doi.org/10.3390/ijms11031155
Blum S, Ji Y, Pennisi D et al (2018) Genome-wide association study in Guillain–Barré syndrome. J Neuroimmunol 323:109–114. https://doi.org/10.1016/j.jneuroim.2018.07.016
Zhang DQ, Wang R, Li T et al (2016) Reduced soluble RAGE is associated with disease severity of axonal Guillain–Barré syndrome. Sci Rep 6:21890. https://doi.org/10.1038/srep21890
Park SJ, Kim JK, Kim HH et al (2019) Integrative metabolomics reveals unique metabolic traits in Guillain–Barré syndrome and its variants. Sci Rep 9:1077. https://doi.org/10.1038/s41598-018-37572-w
Grimm A, Rattay TW, Winter N, Axer H (2017) Peripheral nerve ultrasound scoring systems: benchmarking and comparative analysis. J Neurol 264:243–253. https://doi.org/10.1007/s00415-016-8305-y
Grimm A, Décard BF, Axer H, Fuhr P (2015) The Ultrasound pattern sum score—UPSS. A new method to differentiate acute and subacute neuropathies using ultrasound of the peripheral nerves. Clin Neurophysiol 126:2216–2225. https://doi.org/10.1016/j.clinph.2015.01.011
Telleman JA, Grimm A, Goedee S et al (2018) Nerve ultrasound in polyneuropathies. Muscle Nerve 57:716–728. https://doi.org/10.1002/mus.26029
Peng J, Zhang H, Liu P et al (2018) IL-23 and IL-27 levels in serum are associated with the process and the recovery of Guillain–Barré syndrome. Sci Rep 8:2824. https://doi.org/10.1038/s41598-018-21025-5
Che Y, Qiu J, Jin T et al (2016) Circulating memory T follicular helper subsets, Tfh2 and Tfh17, participate in the pathogenesis of Guillain–Barré syndrome. Sci Rep 6:20963. https://doi.org/10.1038/srep20963
Hughes RA, Swan AV, Van Doorn PA (2014) Intravenous immunoglobulin for Guillain–Barré syndrome. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD002063.pub6
Mathew T, Thomas K, Nadig R et al (2017) Bifacial variant of Guillain–Barre syndrome successfully treated with steroids—a case series. J Neurol Sci 381:652. https://doi.org/10.1016/j.jns.2017.08.1834
Islam B, Islam Z, Rahman S et al (2018) Small volume plasma exchange for Guillain–Barré syndrome in resource-limited settings: a phase II safety and feasibility study. BMJ Open 8:e22862. https://doi.org/10.1136/bmjopen-2018-022862
Wu X, Zhang B, Li C et al (2015) Short-term prognosis of mechanically ventilated patients with Guillain–Barré syndrome is worsened by corticosteroids as an add-on therapy. Med 94:e1898. https://doi.org/10.1097/MD.0000000000001898
Svačina MKR, Röth P, Bobylev I et al (2019) Changes of serum IgG dimer levels after treatment with IVIg in Guillain–Barré syndrome. J Neuroimmune Pharmacol 14:642–648. https://doi.org/10.1007/s11481-019-09871-0
Ye Y, Wang K, Deng F, Xing Y (2013) Electrophysiological subtypes and prognosis of Guillain–Barré syndrome in northeastern China. Muscle Nerve 47:68–71. https://doi.org/10.1002/mus.23477
Kalita J, Kumar M, Misra UK (2019) Role of IV immunoglobulin in Indian Children With Guillain–Barré Syndrome. Pediatr Crit Care Med 20:652–659. https://doi.org/10.1097/PCC.0000000000001935
Niu J, Liu M, Sun Q et al (2018) Motor nerve conduction block predicting outcome of Guillain–Barré syndrome. Front Neurol 9:399. https://doi.org/10.3389/fneur.2018.00399
Wang Y, Lang W, Zhang Y et al (2017) Long-term prognosis of Guillain–Barré syndrome not determined by treatment options? Oncotarget 8:79991–80001. https://doi.org/10.18632/oncotarget.20620
Verboon C, Doets AY, Galassi G et al (2019) Current treatment practice of Guillain–Barré syndrome. Neurology 93:E59–E76. https://doi.org/10.1212/WNL.0000000000007719
van Doorn PA, Kuitwaard K, Walgaard C et al (2010) IVIG treatment and prognosis in Guillain–Barré syndrome. J Clin Immunol 30(Suppl 1):S74–S78. https://doi.org/10.1007/s10875-010-9407-4
Verboon C, van den Berg B, Cornblath DR et al (2020) Second IVIg course in Guillain–Barré syndrome with poor prognosis: the non-randomised ISID study. J Neurol Neurosurg Psychiatry 91:113–121. https://doi.org/10.1136/jnnp-2019-321496
Saad K, Mohamad IL, Abd EI-Hamed MA et al (2016) A comparison between plasmapheresis and intravenous immunoglobulin in children with Guillain–Barre syndrome in Upper Egypt. Ther Adv Neurol Disord 9:3–8. https://doi.org/10.1177/1756285615610471
Kesici S, Tanyıldız M, Yetimakman F, Bayrakci B (2019) A novel treatment strategy for severe Guillain–Barré syndrome: Zipper method. J Child Neurol 34:277–283. https://doi.org/10.1177/0883073819826225
Chevret S, Hughes RA, Annane D (2017) Plasma exchange for Guillain–Barré syndrome. Cochrane Database Syst Rev 2:CD001798. https://doi.org/10.1002/14651858.CD001798.pub3
Halstead SK, Humphreys PD, Zitman FM et al (2008) C5 inhibitor rEV576 protects against neural injury in an in vitro mouse model of Miller Fisher syndrome. J Peripher Nerv Syst 13:228–235. https://doi.org/10.1111/j.1529-8027.2008.00181.x
Mausberg AK, Meyer zu Hörste G, Dehmel T et al (2011) Erythropoietin ameliorates rat experimental autoimmune neuritis by inducing transforming growth factor-β in macrophages. PLoS ONE 6:e26280. https://doi.org/10.1371/journal.pone.0026280
Wang Y, Shi Q, Lv H et al (2017) IgG-degrading enzyme of Streptococcus pyogenes (IdeS) prevents disease progression and facilitates improvement in a rabbit model of Guillain–Barré syndrome. Exp Neurol 291:134–140. https://doi.org/10.1016/j.expneurol.2017.02.010
Phongsisay V, Susuki K, Matsuno K et al (2008) Complement inhibitor prevents disruption of sodium channel clusters in a rabbit model of Guillain–Barré syndrome. J Neuroimmunol 205:101–104. https://doi.org/10.1016/j.jneuroim.2008.09.016
Halstead SK, Zitman FM, Humphreys PD et al (2008) Eculizumab prevents anti-ganglioside antibody-mediated neuropathy in a murine model. Brain 131:1197–1208. https://doi.org/10.1093/brain/awm316
McGonigal R, Cunningham ME, Yao D et al (2016) C1q-targeted inhibition of the classical complement pathway prevents injury in a novel mouse model of acute motor axonal neuropathy. Acta Neuropathol Commun 4:23. https://doi.org/10.1186/s40478-016-0291-x
Usuki S, Taguchi K, Thompson SA et al (2010) Novel anti-idiotype antibody therapy for lipooligosaccharide-induced experimental autoimmune neuritis: Use relevant to Guillain–Barré syndrome. J Neurosci Res 88:1651–1663. https://doi.org/10.1002/jnr.22330
Doets AY, Jacobs BC, van Doorn PA (2018) Advances in management of Guillain–Barré syndrome. Curr Opin Neurol 31:541–550. https://doi.org/10.1097/WCO.0000000000000602
Créange A, Chazaud B, Plonquet A et al (2001) IFN-β decreases adhesion and transmigration capacities of lymphocytes in Guillain–Barré syndrome. Neurology 57:1704–1706. https://doi.org/10.1212/WNL.57.9.1704
Pritchard J, Gray IA, Idrissova ZR et al (2003) A randomized controlled trial of recombinant interferon-beta 1a in Guillain–Barré syndrome. Neurology 61:1282–1284. https://doi.org/10.1212/01.WNL.0000092019.53628.88
Feasby TE (1991) Treatment of Guillain–Barré syndrome with anti-T cell monoclonal antibodies. J Neurol Neurosurg Psychiatry 54:51–54. https://doi.org/10.1136/jnnp.54.1.51
Staff NP, Windebank AJ (2014) Peripheral neuropathy due to vitamin deficiency, toxins, and medications. Continuum (Minneap Minn) 20:1293–1306. https://doi.org/10.1212/01.CON.0000455880.06675.5a
Gao Y, Zhang HL, Xin M et al (2018) Serum folate correlates with severity of Guillain–Barré syndrome and predicts disease progression. Biomed Res Int 2018:5703279. https://doi.org/10.1155/2018/5703279
Hamel J, Logigian EL (2018) Acute nutritional axonal neuropathy. Muscle Nerve 57:33–39. https://doi.org/10.1002/mus.25702
Acknowledgements
The work was supported by grants from the National Key R&D Program of China (No. 2017YFC0110304 to JF), and the National Natural Science Foundation of China to (No. 31600820 to MZ and No. 81771257 to JF).
Funding
The work was supported by grants from the National Key R&D Program of China (No. 2017YFC0110304 to JF), and the National Natural Science Foundation of China to (No. 31600820 to MZ and No. 81771257 to JF).
Author information
Authors and Affiliations
Contributions
HLZ conceived the topic and designed the outline of this review; PS drafted the manuscript; MZ and YW contributed to the literature review and manuscript writing; XZ and XW contributed to the figure preparation; JZ, HLZ and JF critically revised the manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shang, P., Zhu, M., Wang, Y. et al. Axonal variants of Guillain–Barré syndrome: an update. J Neurol 268, 2402–2419 (2021). https://doi.org/10.1007/s00415-020-09742-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09742-2