Abstract
Gaze stabilisation exercises are a mainstay of vestibular rehabilitation (VR). They are frequently prescribed to patients with vestibular hypofunction with the aim of improving the gain of the vestibular ocular reflex, improving visual acuity during head movement, and reducing the symptoms of dizziness and vertigo. This review will examine current evidence that has evaluated the efficacy of gaze stabilisation exercises on VOR gain, dynamic visual acuity and oscillopsia. In addition, recent experimental studies that have employed digital technologies and newer forms of gaze stabilisation exercises will be reviewed. The implications for future clinical practice and research in the area of VR will be discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular rehabilitation (VR) is a widely recognised treatment for vestibular hypofunction. Moderate to strong evidence for efficacy has been demonstrated in several systematic reviews [18, 36, 41, 43]. Improving gaze stability is one of the central principles of VR and gaze stability exercises (GSEs) are commonly prescribed for this purpose. GSEs are further classified into adaptation and substitution exercises [17]. Adaptation exercises promote “long-term changes in the neuronal response to head movements with the goal of reducing symptoms and normalizing gaze and postural stability” [17]. In contrast, substitution exercises employ other visual strategies such as enhanced smooth pursuit or central pre-programming of eye movements. GSEs are delineated from habituation exercises, with the latter thought to reduce vestibular-related symptoms by repeated exposure to a provoking stimulus (such as head movement) to decrease the response to the stimulus [17]. As a principle, habituation exercises do not involve the individual fixating on a target during the head and/or body movements.
This review will explore current literature pertaining to GSEs, firstly examining evidence of superiority when compared to habituation exercises, and secondly presenting what is known about the effect of GSEs on measures of vestibular function: the gain of the vestibulo-ocular reflex (VOR), dynamic visual acuity (DVA), and perception of apparent movement of the environment (oscillopsia). Throughout the review, the use of digital technologies to generate new knowledge in this area and their potential to develop new therapeutic applications will be discussed.
Gaze stabilisation exercises
Early reports of GSEs appeared in the late 1980s when knowledge about the importance of retinal slip being a required error signal to adapt the gain of the VOR emerged [13, 20]. The most frequently utilised GSEs are known as the “VORx1” and “VORx2” exercises [19], Fig. 1). In the VORx1 exercise, the patient visually fixates on a stationary target (usually a letter) and rotates the head sinusoidally in either the yaw or pitch plane. In VORx2, both the head and the target are rotated in equal and opposite directions, e.g., as the head rotates to the left the target is moved by the patient to the right and vice versa in a sinusoidal pattern. Parameters of distance from the target, head velocity, target size, and exercise frequency and duration are usually individualised and progressed over time [44]. GSEs are recommended for those with unilateral and bilateral vestibular loss [17, 43].
Adaptation Exercises; In VORx1, shown left, an individual fixates on a still target (usually a letter marked on the back of a business card or stick) and performs sinusoidal repetitive head movements in different planes. In VORx2, not shown the individual moves the target in an equal and opposite direction to the head movement. Copyright © 1995 by the American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. Reprinted by Permission of SAGE Publications, Inc. [22]
Szturm et al. [52] conducted one of the first randomised controlled trials that compared habituation exercises to GSEs and found a significant reduction in VOR gain asymmetry and significant improvement in computerised dynamic posturography scores in the GSEs group and not the habituation group. This suggested that the gaze stabilisation aspect of a VR programme, inducing retinal slip, was superior to general head and eye movements. Later, Clendaniel [8] compared habituation to stabilisation exercises and failed to find differences; both improved dynamic visual acuity (DVA) and subjective dizziness scores. This study was limited in that it recruited very small numbers (n = 7). Apart from these two studies, no others have directly compared GSEs to habituation exercises. Presently, there is no robust evidence from the randomised controlled trials to select gaze stabilisation exercises over habituation exercises. It is likely that habituation also occurs during the repetitive movements in GSEs. It is the precise effect of fixation that requires elucidation. There is, however, evidence from several randomised controlled trials that GSEs as part of VR programmes are superior to no intervention or sham intervention [9, 12, 22, 51, 56].
Parameters used to quantify the effect of GSEs in clinical studies include VOR gain, DVA, and the amount of subjective oscillopsia. In the following, we review the evidence for effects of GSEs on these parameters, both in vestibular patients and healthy controls. We will also address the question, which one of these parameters might be meaningful for the patients functioning and participation.
Do gaze stabilisation exercises change the gain of the VOR?
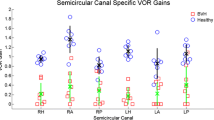
A fundamental question is whether or not GSEs change the gain of the VOR, and if so, is the response stable. The gain of the VOR is the ratio of head movement velocity to eye movement velocity and when measured in healthy adults with the video head impulse test it is usually above 0.79 [37] with reported mean values of 0.94–0.97 [1, 40]. It is important that improvements in VOR gain result in benefits and meaningfulness for the patient, e.g., a concurrent reduction in symptoms of oscillopsia (apparent movement of the environment), motion-provoked dizziness or improved dynamic visual acuity (DVA). Changes in active and passive VOR gains after GSEs have been examined, the active gain of the VOR is the gain measured when an individual actively moves their head (predictable) and passive VOR gain is the gain measured during an unpredictable head movement.
Several experimental studies have been performed which confirm that GSEs can improve VOR gain. Schubert et al. [48] in a single case report demonstrated increased passive VOR ipsilesional gain with GSEs (VORx1, VORx2) in an individual with unilateral vestibular loss (UVL). The changes were associated with improved DVA. In a subsequent study of n = 5 patients with vestibular hypofunction, GSEs resulted in a mean increase of 35 ± 29% in active VOR gains but a lesser effect on passive VOR gains. Parallel improvements in DVA and dizziness occurred [49].
Schubert et al. [45] using a case (UVL) control (healthy adults) design investigated differences between 2 paradigms of increasing VOR gain. Instead of VORx1 and VORx2 GSEs, they employed an exercise programme that reflected the frequency and amplitude under which the VOR is used during normal daily life (brief angular translations with a high velocities and accelerations). Scleral coils were used to measure eye movement velocity and a head sensor measured head position/velocity and was paired with a laser target that had the ability to move with adjustable proportions to the head velocity. Both paradigms consisted of just 15 min of training in the dark. Participants were trained to self-generate active yaw plane head rotations from neutral, 25° to right and, from neutral, 25° to the left. Over 15 min, 300 such head movements at a velocity of 180 deg/sec (3500 sec2) were performed (in 10 sets of 30 head movements). Rests of 30–60 s were provided between sets. In the first paradigm, VORx2, a laser target moved 100% in the opposite direction of the head movement and at the same velocity as the head, requiring a ×2 gain demand to maintain fixation on the target (i.e., the eye had to move twice as fast as the head to stay on the target). In the second paradigm, designated the “incremental velocity error” or IVE, the laser target velocity was incrementally adjusted to demand an increase in gain of just 10% per set (so that at the end of the 10 sets a ×2 gain was required, Fig. 2). Both healthy controls and patients with UVL were studied and the outcomes were changes in active and passive VOR gains. Results indicated that in healthy controls, the IVE paradigm achieved larger active VOR gains than the ×2 paradigm (17.3% vs 7.1%, respectively). In the UVL patients (n = 5), the IVE paradigm also led to greater mean active VOR gain change (for ipsilesional head rotations) than VORx2 (18% vs − 6%, respectively). Significantly higher passive VOR gains were also found for the IVE paradigm in controls but no differences were observed in UVL individuals. The conclusion was that an incremental adjustment of gain was superior to the larger “all at once” demand that the VORx2 paradigm required. The exercise programme in the study had demanded an increased gain of both sides, which is not necessary in UVL patients.
Incremental vestibular adaptation, the target is moved incrementally demanding an increase in gain of 0.1 per epoch (set) of exercises. Thread sensor detects the head movement velocity and moves the target in the opposite direction at velocities for the desired gain increase. Copyright © 2018 IEEE. Reprinted, with permission [55]
In a subsequent study, Migliaccio and Schubert [38] used the same IVE training paradigm as described above but investigated the merits of targeting an increase in gain towards one side only (and called this side the “adapting” side) in a group of healthy controls. The training programme was designed so that when the head movements were to the “adapting” side, the laser target moved in the opposite direction to head and with increasing gain demand. When moving to the “non-adapting side”, the laser target turned off (thus not demanding any gain change). The findings were surprising in that active VOR gains to both the adapting and non-adapting sides were significantly increased after the 15 min training session. Although the magnitude of the gain to the non-adapting side was 70% smaller (7% vs 21% to the adapting side), this was considered undesirable and probably as a result of commissural pathways. Passive VOR gains also increased but were only significant towards the adapting side. Retention, however, was not measured and the subjects were healthy.
The authors proceeded to investigate if it were possible to avoid the unwanted gain of increased adaptation towards the non-adapting side but this time involved individuals with UVL as well as healthy controls [39]. Subjects performed 300 self-generated head impulses (15° at velocities above 120° per second) in sets of 30 at a time over 15 min. A different measurement system was used, eye velocity was measured with a digital eye camera and head velocity was measured with a sensor on a portable helmet; the latter was linked to a visual laser target adjustable to head velocity. The VOR gain demand to the non-adapting side was 1 and to the adapting side 1.5 (in the case of the patients the adapting side was ipsilesional). The IVE paradigm was not used in this study. The results showed that in healthy controls, setting a gain of 1 to the “non-adapting” side resulted in no undesirable increase in that gain, whilst a significant increase in both passive and active head impulse gains was found for head impulses to the “adapting” side. In the group with vestibular hypofunction, more variable findings emerged. There was a desirable 29% increase in active VOR gain towards the lesioned side but this was non-significant. A significant decrease in gain was found for movements to the non-lesioned side. Importantly, of the six patients with vestibular loss, two were able to successfully complete the exercises, two were inconsistent with the speed and accuracy of the exercises and two were unable to perform them, suggesting that this paradigm may not be suitable for a proportion of cases. Finally, the gains achieved with a constant gain demand of + 1.5 were similar to the previous study, which used the IVE paradigm so the authors suggested that both were equally effective.
Taken together these studies demonstrated that active VOR gains improved with very short periods of GSEs. Passive VOR gains did not improve to the same degree. It has also been shown that the head movements during the IVE program can be actively or passively induced for achieving gain improvements [33]. However, RCTs that include this level of detail in outcome measurement and with the intervention provided over a longer term are required to fully investigate this. The increasing availability of the video head impulse test to measure VOR gain will likely facilitate these studies.
More recently, two studies [32, 34] investigated optimal motor learning parameters for gain increases and retention using the IVE paradigm (which, in these studies was termed IVA: incremental vestibular adaptation). In the first, which recruited healthy controls, five different exercise programmes were investigated. Four were 15 min in duration and one was 7.5 min in duration. Results showed a superiority for all the 15 min protocols over the 7.5 min protocol for increasing active VOR gain. Interestingly, the protocol with the largest gain achieved (+ 16%) was the only one in which the laser target was left on during exercise until the peak amplitude of head movement was attained (as opposed to peak velocity in the other four protocols). Thus, a longer duration of exercises and of laser target availability during the exercises were the factors that coupled together, improved gain the most.
In the second study, it was investigated whether exercises (using the IVA protocol) should be performed in one block or split into smaller time blocks. In the first, recruiting only healthy controls, it was found that gain increases obtained with IVA were 2.2 times larger if subjects got three five-minute training blocks with 20 min rest between blocks (7.1% increase in VOR gain towards the adapting side) as opposed to one 5 min block (3% increase). A greater gain demand (+ 20% per set) resulted in a smaller gain increase suggesting that smaller increments of gain change (+ 10% per set) over the 15 min were superior. Finally, when results were compared to a previous study on one block of 15 min with no rest periods, it was concluded that splitting training into 3 blocks was not superior in terms of increasing gain but resulted in better retention over time (4% loss vs 1% loss, respectively). This finding is consistent with the motor learning literature that massed practice is better for short-term retention but distributed results in more stable learning.
In this group of experimental studies, differential results were found in healthy controls compared to those with vestibular hypofunction. Also, UVL individuals could sometimes not generate high enough head velocities to participate. There was greater variability in VOR gain improvements in the patients than in the healthy controls showing that individuals recruit differential strategies after vestibular loss. The equipment and technological expertise demanded by these paradigms is beyond the capabilities of most rehabilitation programs at present. There is no commercial system available at the moment that can produce a laser target that is coupled to head movement and can incrementally adjust VOR gain to one side only, instead therapists use target size and incrementally increasing head velocities to facilitate VOR gain increases. This is likely to change in the future. Taken together, the results from these novel studies provide initial support for the clinical use of brief head impulse type exercise programmes and for incremental adjustment of VOR gain. In addition, short bursts with intervals for consolidation improve gain retention. Further work is required to clarify if the gain improvements seen in healthy controls translate to, and are stable in, cohorts of patients with vestibular loss.
An open question remains on the retention of the effects. A recent report showed that the incremental paradigm performed daily at home for 15 min for just under 2 years resulted in increased passive VOR gains in a single patient with profound bilateral vestibular loss (BVL). There was a concurrent improved balance and gait, despite the fact that the exercise program was completed in the sitting position. A proportion of the gain was retained over time [11]. Another single case study [6], of a patient with chronic unilateral UVL, employed the vHIT to deliver a 5-day program of passive, predictable and ipsilesional head impulses. The patient had previously undergone conventional VR (including VORx1 and VORx2) with fluctuating benefit. Ten sets of 15 horizontal head movements towards the lesioned side were completed at each session. After treatment the ipsilesional VOR gain had improved from 0.57 to 0.71. Concurrent improvements were measured in DVA and subjective dizziness which remained stable at a year.
These are the only two studies to investigate longer term retention of improved VOR gains and gait and balance correlates using the IVA (or similar) paradigm. Clearly, future studies with larger numbers and precise measurements of adherence will clarify the factors that may influence retention using this paradigm.
A final consideration for the IVA paradigm is that there is limited knowledge whether patients with UVL will tolerate such fast movements and if increased gains translate to improved dynamic visual acuity, changes in oscillopsia, gait or balance or decreased symptom burden.
The extent to which improvements in VOR gains are associated with dynamic dysfunction is clearly an important consideration. Improving VORs gain per se may be of limited use if the improvement does not transfer to improved dynamic function. A recent retrospective analysis of VR in a group with sub-acute and chronic dizziness (UVL and BVL) found improved gains of the VOR in 39% of patients. However, in 70% of those whose gains did not improve, Dynamic Gait Index scores nonetheless improved [7]. This suggests that improved gains in VOR may not be necessary for improvement in dynamic function and the authors suggested that this may reflect the ability of the CNS to use multiple other processes to improve dynamic function in the absence of VOR gain improvement.
Do gaze stabilisation exercises improve dynamic visual acuity?
Dynamic visual acuity is the ability to fixate on a target and see it clearly, when one’s head is moving. It is considered to be a functional measure of the VOR and is usually measured as the difference between visual acuity when the head is stationary and when it is moving (at velocities that only the VOR can generate an eye movement to fixate). Many DVA testing paradigms have been developed and active DVA testing (where the patient self generates/predicts the head movement) results in better DVA values than passive/unpredictable DVA testing, where the examiner imposes the head movement during testing). The DVA of patients with UVL is more impaired during ipsilesional than contralesional head movements and higher gains are associated with better DVA during unpredictable DVA testing [47]. Impaired DVA (measured in sitting) has been found at outset of VR in 46% of those with UVL [23] and 60–72% of those with BVL [25,26,27]. When measured during walking (6 km/h), DVA abnormalities were found 73% of those with BVL and 27% of those with UVL [16]. Reduced DVA measured with the gaze stabilization test is correlated with impaired dynamic gait function [57]. One study found that vertical DVA in BVL was significantly worse in those who also reported a history of falling. The same study also found that reduced DVA in BVL did not correlate with the quality of life [26].
Three randomised controlled trials [8, 21, 24] showed that GSEs (VORx1 and VORx2 provided with gait and balance retraining) improved DVA in patients with UVL and BVL. Significant improvements in DVA were found only in the groups performing GSEs in the latter two studies.
During head movements that require visual fixation unique saccadic eye movements that occur in the direction of a deficient slow phase, compensatory saccades (CSs) or catch up saccades are produced, which reduce gaze error in patients with vestibular loss [54]. They are either produced during the head movement (covert saccades) or after the head movement (overt saccades). Hermann et al. [27] found covert saccades in 76% of the passive vHITs of patients with BVL. A higher frequency and occurrence of covert saccades and higher gains and shorter latencies were all significantly and positively associated with better DVA. Covert saccades contributed to a mean of 42% of the total eye movement.
There is evidence that the organisation of CSs has an association with patient-reported symptoms. Batuecas-Caletrio et al. [4] quantified covert and overt saccades in a group of 49 patients who had undergone resection of an acoustic neuroma at least a year previously (none of whom had VR). Patients were arbitrarily divided into two groups based on the organisation of the covert and overt saccades during passive VOR gain testing, as being either random or highly organised (based on consistency of CS latency). They found that the group in which saccades were highly organised had lower DHI scores. CSs are, therefore, of importance to therapists providing VR. Matino-Soler et al. [35] elucidated how GSEs impact on compensatory saccades in a group of heterogenous chronic, uncompensated UVL patients. A progressive programme of GSEs was delivered via a computer and head sensor over 2 weeks and VOR gain, DHI and the organisation of compensatory saccades were measured. Results indicated that passive VOR gain did not change significantly but DHI scores decreased and CSs became more organised and remained stable at a 3-month follow-up suggesting that GSEs have a modifying effect on CS organisation and in turn reduce subjective symptoms. Of interest, the subjects in the study did not appear to do any balance and gait rehabilitation so the effect was probably confined to the GSE. These early studies suggest that CSs are an important variable to consider when prescribing GSEs. Factors affecting the ability to generate CSs are as yet unclear but it has been observed that increased age may have negative effects on their temporal organisation [5].
Do gaze stabilisation exercises improve oscillopsia?
Oscillopsia is the perception that the world is moving during head movements and is a consequence of impaired gain of the VOR. Oscillopsia is reported in 69–100% of patients with BVL [16, 29,30,31] and is correlated with subjective Dizziness Handicap Inventory scores [15, 26]. It is reported to a lesser extent (9–48%) in those with unilateral loss [16, 23].
There is evidence that oscillopsia improves with VR. Herdman et al. [23, 25] in two retrospective studies on patients with UVL and BVL measured oscillopsia on a visual analogue scale (where higher scores represented greater oscillopsia) before and after a programme of VR (including GSEs). Significant improvements from a mean of 3.05/10 to 0.79/10 and from 3.6/10 to 1.0/10 were found in UVL and BVL, respectively.
However, VR may not need to include GSEs to have an effect on oscillopsia. One RCT on UVL patients found significant improvements in oscillopsia in both control (balance and gait exercises only) and experimental groups (GSEs balance and gait). In addition, no correlation was found between improvement in DVA (predictable or unpredictable) and improvement in oscillopsia [21].
Oscillopsia does not correlate with DVA when it is measured with predictable head movements [2, 46] but does when measured with passive (unpredictable) head movements [3]. DVA measured during walking in a group of patients with BVL and UVL showed no correlation with severity of oscillopsia [16]. Furthermore, in one study on patients with BVL, greater retinal slip was associated with reduced reports of oscillopsia (one would expect higher oscillopsia with greater retinal slip). In this study, oscillopsia was correlated with locus of control, those who perceived themselves to have a greater control over their health reported less oscillopsia [14]. The authors suggested that psychological parameters are important when considering oscillopsia and also the extent to which individuals with vestibular loss develop a tolerance to retinal slip (through reduction of visual motion sensitivity). DVA was not directly measured in this study and whether the subjects in this study had undergone VR was not clear. Finally, in one case series, oscillopsia did not correlate with VOR gains in patients with BVL [29].
In conclusion, the precise effects of GSEs on oscillopsia remain to be quantified. It would be helpful if future studies on efficacy incorporated measures of oscillopsia and investigated their interaction with DVA, VOR gain and physical measures.
What is the optimal time course for initiating GSEs and over what time period?
Whether there are critical time periods for initiation of GSEs is unclear [17]. Positive outcomes have been found when GSEs are initiated in the acute phase [9, 50, 53] but direct comparisons with delayed commencement are lacking. Time from onset of symptoms to commencement of GSEs does not correlate with outcomes in those with UVL and BVL suggesting that benefits can be obtained at all phases of the disease process [23, 25]. However, animal data have provided strong support for early exposure to sensori-motor therapy demonstrating positive effects on vestibular neuronal responses, so further investigation in humans would be instructive [28].
The optimal time course for VR varies according to type of vestibular loss. At present, clinical guidelines based on expert opinion recommend 2–3 weeks of once weekly supervised VR for acute UVL, 4–6 weeks for chronic UVL and 8–12 for BVL. Home exercise 2–3 times a day is also recommended [17]. A higher level of evidence in this regard is needed.
The future of gaze stabilisation exercises
Appropriately powered randomised controlled trials are needed to further evaluate the efficacy of GSEs. A study in which a habituation programme is compared to a gaze stabilisation programme could investigate the superiority of one approach over the other. As well as measuring VOR gains, changes in compensatory saccades and DVA, and the clinical meaningfulness of improvements in these outcomes could be concurrently addressed. If gain and DVA improvements are observed, what does this mean to the patient in daily life, do improvements translate to decreased subjective symptoms of oscillopsia, dizziness and vertigo or to improved balance or gait? The video head impulse test is likely to be a valuable outcome measure in future studies, allowing the effects of GSEs on important parameters of compensatory saccades (and their clinical correlates) to be determined. In addition, the differential effects of GSEs on types of vestibular loss, i.e., total loss, partial loss, UVL, BVL and sequential loss will need further investigation.
The lower cost of movement sensor technologies will enable parameters of head motion to be tracked. At present, tracking head motion is technically easier than tracking eye motion (but the latter will likely be readily available at some stage also). Using technology in real time, to intelligently adjust the speed and frequency of the exercises, and perhaps incrementally adjust the VOR gain will be possible and greatly inform practice. Technology could also be used to measure both symptomatic burden of exercises and adherence. Adherence is a significant factor in positive outcomes from VR [58] but other parameters such as frequency, intensity, type and time (so-called FITT principles) remain to be precisely quantified. Finally, VR gaze stability exercises can be boring and repetitive. Systems incorporating virtual reality and gamification of exercises may be of benefit and will become available. Using technology alone, though it is unlikely to confer maximum benefit, studies have shown that adherence is poorer if patients receive no face to face treatment [10, 42]. The change from delivering exercises via traditional pen and paper methods towards technology-based methods will require supportive evidence on efficacy, acceptance, usability, and opportunity costs. It represents a paradigm shift that will require behavioural change both in clinicians and patients.
References
Alhabib SF, Saliba I (2017) Video head impulse test: a review of the literature. Eur Arch Otorhinolaryngol 274:1215–1222
Anson ER, Gimmon Y, Kiemel T, Jeka JJ, Carey JP (2018) A tool to quantify the functional impact of oscillopsia. Front Neurol 9:142
Badaracco C, Labini FS, Meli A, Tufarelli D (2010) Oscillopsia in labyrinthine defective patients: comparison of objective and subjective measures. Am J Otolaryngol 31:399–403
Batuecas-Caletrio A, Santacruz-Ruiz S, Munoz-Herrera A, Perez-Fernandez N (2014) The vestibulo-ocular reflex and subjective balance after vestibular schwannoma surgery. Laryngoscope 124:1431–1435
Batuecas-Caletrio A, Santacruz-Ruiz S, Munoz-Herrera A, Sousa P, Otero A, Perez-Fernandez N (2013) Vestibular compensation after vestibular schwannoma surgery: normalization of the subjective visual vertical and disability. Acta Otolaryngol 133:475–480
Binetti AC, Varela AX, Lucarelli DL, Verdecchia DH (2017) Unilateral head impulses training in uncompensated vestibular hypofunction. Case Rep Otolaryngol 2017:2145173
Chang TP, Schubert MC (2018) Association of the video head impulse test with improvement of dynamic balance and fall risk in patients with dizziness. JAMA Otolaryngol Head Neck Surg 144:696–703
Clendaniel RA (2010) The effects of habituation and gaze stability exercises in the treatment of unilateral vestibular hypofunction: a preliminary results. J Neurol Phys Ther 34:111–116
Enticott JC, O’leary SJ, Briggs RJS (2005) Effects of vestibulo-ocular reflex exercises on vestibular compensation after vestibular schwannoma surgery. Otol Neurotol 26:265–269
Geraghty AWA, Essery R, Kirby S, Stuart B, Turner D, Little P, Bronstein A, Andersson G, Carlbring P, Yardley L (2017) Internet-based vestibular rehabilitation for older adults with chronic dizziness: a randomized controlled trial in primary care. Ann Fam Med 15:209–216
Gimmon Y, Migliaccio AA, Kim KJ, Schubert MC (2019) VOR adaptation training and retention in a patient with profound bilateral vestibular hypofunction. Laryngoscope. https://doi.org/10.1002/lary.27838 (Epub ahead of print)
Giray M, Kirazli Y, Karapolat H, Celebisoy N, Bilgen C, Kirazli T (2009) Short-term effects of vestibular rehabilitation in patients with chronic unilateral vestibular dysfunction: a randomized controlled study. Arch Phys Med Rehabil 90:1325–1331
Gonshor A, Jones GM (1976) Short-term adaptive changes in the human vestibulo-ocular reflex arc. J Physiol 256:361–379
Grunfeld EA, Morland AB, Bronstein AM, Gresty MA (2000) Adaptation to oscillopsia: a psychophysical and questionnaire investigation. Brain 123(Pt 2):277–290
Guinand N, Boselie F, Guyot J-P, Kingma H (2012) Quality of life of patients with bilateral vestibulopathy. Ann Otol Rhinol Laryngol 121:471–477
Guinand N, Pijnenburg M, Janssen M, Kingma H (2012) Visual acuity while walking and oscillopsia severity in healthy subjects and patients with unilateral and bilateral vestibular function loss. Arch Otolaryngol Head Neck Surg 138:301–306
Hall CD, Herdman SJ, Whitney SL, Cass SP, Clendaniel RA, Fife TD, Furman JM, Getchius TS, Goebel JA, Shepard NT, Woodhouse SN (2016) Vestibular rehabilitation for peripheral vestibular hypofunction: an evidence-based clinical practice guideline: from the american physical therapy association neurology section. J Neurol Phys Ther 40:124–155
Hansson EE (2007) Vestibular rehabilitation—for whom and how? A systematic review. Adv Physiother 9:106–116
Herdman SJ, Clendaniel R (2014) Vestibular rehabilitation. FA Davis, Philadelphia
Herdman SJ (1989) Exercise strategies for vestibular disorders. Ear Nose Throat J 68:961–964
Herdman SJ, Schubert MC, Das VE, Tusa RJ (2003) Recovery of dynamic visual acuity in unilateral vestibular hypofunction. Arch Otolaryngol Head Neck Surg 129:819–824
Herdman SJ, Clendaniel RA, Mattox DE, Holliday MJ, Niparko JK (1995) Vestibular adaptation exercises and recovery: acute stage after acoustic neuroma resection. Otolaryngol Head Neck Surg 113:77–87
Herdman SJ, Hall CD, Delaune W (2012) Variables associated with outcome in patients with unilateral vestibular hypofunction. Neurorehabilit Neural Repair 26:151–162
Herdman SJ, Hall CD, Schubert MC, Das VE, Tusa RJ (2007) Recovery of dynamic visual acuity in bilateral vestibular hypofunction. Arch Otolaryngol Head Neck Surg 133(4):383–389
Herdman SJ, Hall CD, Maloney B, Knight S, Ebert M, Lowe J (2015) Variables associated with outcome in patients with bilateral vestibular hypofunction: preliminary study. J Ves Res 25(3–4):185–194
Hermann R, Ionescu EC, Dumas O, Tringali S, Truy E, Tilikete C (2018) Bilateral vestibulopathy: vestibular function, dynamic visual acuity and functional impact. Fron Neurol 9:555
Hermann R, Pelisson D, Dumas O, Urquizar C, Truy E, Tilikete C (2018) Are covert saccade functionally relevant in vestibular hypofunction? Cerebellum 17:300–307
Lacour M, Bernard-Demanze L (2014) Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Front Neurol 5:285
Levo H, Aalto H, Hirvonen TP (2017) Bilateral vestibular hypofunction in quantitative head impulse test: clinical characteristics in 23 patients. J Int Adv Otol 13(3):354–357
Lucieer F, Duijn S, van Rompaey V, Pérez Fornos A, Guinand N, Guyot JP, Kingma H, van de Berg R (2018) Full spectrum of reported symptoms of bilateral vestibulopathy needs further investigation-A systematic review. Front Neurol 9:352
Lucieer F, Vonk P, Guinand N, Stokroos R, Kingma H, van de Berg R (2016) Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol 7:26
Mahfuz MM, Schubert MC, Figtree WVC, Todd CJ, Migliaccio AA (2018) Human vestibulo-ocular reflex adaptation training: time beats quantity. J Assoc Res Otolaryngol 19(6):729–739
Mahfuz MM, Schubert MC, Figtree WVC, Todd CJ, Khan SI, Migliaccio AA (2018) Optimal human passive vestibulo-ocular reflex adaptation does not rely on passive training. J Assoc Res Otolaryngol 19:261–271
Mahfuz MM, Schubert MC, Figtree WVC, Todd CJ, Migliaccio AA (2018) Human vestibulo-ocular reflex adaptation: consolidation time between repeated training blocks improves retention. J Assoc Res Otolaryngol 19:601–610
Matino-Soler E, Rey-Martinez J, Trinidad-Ruiz G, Batuecas-Caletrio A, Perez Fernandez N (2016) A new method to improve the imbalance in chronic unilateral vestibular loss: the organization of refixation saccades. Acta Otolaryngol 136:894–900
Mcdonnell MN, Hillier SL (2015) Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005397.pub4
Mcgarvie LA, Macdougall HG, Halmagyi GM, Burgess AM, Weber KP, Curthoys IS (2015) The video head impulse test (vHIT) of semicircular canal function—age-dependent normative values of VOR gain in healthy subjects. Front Neurol 6:154
Migliaccio AA, Schubert MC (2013) Unilateral adaptation of the human angular vestibulo-ocular reflex. J Assoc Res Otolaryngol 14:29–36
Migliaccio AA, Schubert MC (2014) Pilot study of a new rehabilitation tool: improved unilateral short-term adaptation of the human angular vestibulo-ocular reflex. Otol Neurotol 35:e310–e316
Mossman B, Mossman S, Purdie G, Schneider E (2015) Age dependent normal horizontal VOR gain of head impulse test as measured with video-oculography. J Otolaryngol Head Neck Surg 44:29
Passier L, Doherty D, Smith J, Mcphail SM (2012) Vestibular rehabilitation following the removal of an acoustic neuroma: a systematic review of randomized trials. Head Neck Oncol 4:59
Pavlou M, Bronstein AM, Davies RA (2013) Randomized trial of supervised versus unsupervised optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabilit Neural Repair 27:208–218
Porciuncula F, Johnson CC, Glickman LB (2012) The effect of vestibular rehabilitation on adults with bilateral vestibular hypofunction: a systematic review. J Vestib Res 22:283–298
Roller RA, Hall CD (2018) A speed-based approach to vestibular rehabilitation for peripheral vestibular hypofunction: a retrospective chart review. J Vestib Res 28:349–357
Schubert MC, Della Santina CC, Shelhamer M (2008) Incremental angular vestibulo-ocular reflex adaptation to active head rotation. Exp Brain Res 191:435–446
Schubert MC, Herdman SJ, Tusa RJ (2002) Vertical dynamic visual acuity in normal subjects and patients with vestibular hypofunction. Otol Neurotol 23:372–377
Schubert MC, Migliaccio AA, Della Santina CC (2006) Dynamic visual acuity during passive head thrusts in canal planes. J Assoc Res Otolaryngol 7:329–338
Schubert MC, Migliaccio AA, Della Santina CC (2006) Modification of compensatory saccades after aVOR gain recovery. J Vestib Res 16:285–291
Schubert MC, Migliaccio AA, Clendaniel RA, Allak A, Carey JP (2008) Mechanism of dynamic visual acuity recovery with vestibular rehabilitation. Arch Phys Med Rehabilit 89:500–507
Sparrer I, Duong Dinh TA, Ilgner J, Westhofen M (2013) Vestibular rehabilitation using the Nintendo® Wii balance board—a user-friendly alternative for central nervous compensation. Acta Otolaryngol 133:239–245
Strupp M, Arbusow V, Maag KP, Gall C, Brandt T (1998) Vestibular exercises improve central vestibulospinal compensation after vestibular neuritis. Neurology 51:838–844
Szturm T, Ireland DJ, Lessing-Turner M (1994) Comparison of different exercise programs in the rehabilitation of patients with chronic peripheral vestibular dysfunction. J Vestib Res 4:461–479
Teggi R, Caldirola D, Fabiano B, Recanati P, Bussi M (2009) Rehabilitation after acute vestibular disorders. J Laryngol Otol 123:397–402
Tian J, Crane BT, Demer JL (2000) Vestibular catch-up saccades in labyrinthine deficiency. Exp Brain Res 131:448–457
Todd CJ, Hübner PP, Hübner P, Schubert MC, Migliaccio AA (2018) StableEyes—a portable vestibular rehabilitation device. IEEE Trans Neural Syst Rehabil Eng. 26(6):1223–1232
Viirre E, Sitarz R (2002) Vestibular rehabilitation using visual displays: preliminary study. Laryngoscope 112:500–503
Whitney SL, Marchetti GF, Pritcher M, Furman JM (2009) Gaze stabilization and gait performance in vestibular dysfunction. Gait Posture 29:194–198
Yardley L, Kirby S (2006) Evaluation of booklet-based self-management of symptoms in Meniere disease: a randomized controlled trial. Psychosom Med 68:762–769
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
An approval by an ethics committee was not applicable.
Additional information
This manuscript is part of a supplement sponsored by the German Federal Ministry of Education and Research within the funding initiative for integrated research and treatment centers.
Rights and permissions
About this article
Cite this article
Meldrum, D., Jahn, K. Gaze stabilisation exercises in vestibular rehabilitation: review of the evidence and recent clinical advances. J Neurol 266 (Suppl 1), 11–18 (2019). https://doi.org/10.1007/s00415-019-09459-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09459-x