Abstract
Vestibular rehabilitation is a critical tool facilitating recovery after peripheral or central vestibular deficits. In this chapter, we will discuss state-of-the-art clinical practice strategies. We will focus on incremental vestibular ocular reflex (VOR) adaptation, with specific focus on the influence of training target contrast on the adaptive process, the influence of position and velocity error signals driving the adaptive process, and the role of active versus passive head rotation. We will then discuss the important effects of aging on VOR adaptation. Finally, we will summarize new developments in vestibular rehabilitation and provide a succinct review of vestibular rehabilitation in atypical medical populations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Current Best Practice
Vestibular rehabilitation (VPT) is recognized as a critical component addressing the impairments of patients with disorders to the peripheral vestibular labyrinth and the pathways that mediate its afference. Meta-analysis evidence supports that VPT should be the primary intervention when treating vestibular hypofunction and benign paroxysmal positional vertigo (Hillier and McDonnell 2011, 2016; McDonnell and Hillier 2015; Hilton and Pinder 2004). For this chapter, we will focus on new advances in VPT as related to the treatment of vestibular hypofunction. In particular, we will focus on gaze stability training, which represents the uniquely “vestibular” component of VPT. While balance exercises are also critical for rehabilitation in vestibular labyrinth and nerve hypofunction, it is the gaze stability component that distinguishes VPT as most valuable.
The current standard of care in delivering VPT involves the prescription of gaze and gait stability exercises, which evidence shows improves visual acuity during head rotation, reduces fall risk, and improves both static and dynamic balance (Herdman et al. 2003, 2007, Hall et al. 2004; Schubert et al. 2008a). Clinical practice guidelines (CPG) are now available that specify clinicians prescribe a home exercise program of gaze stability exercises for a minimum of three times per day for a total of 12 minutes per day in patients with acute/subacute vestibular hypofunction (Hall et al. 2016). For patients with chronic vestibular hypofunction, the recommendations are a minimum of 20 minutes per day (Hall et al. 2016). Unfortunately, compliance performing these exercises is relatively poor (Meldrum et al. 2012; Huang et al. 2014).
2 Incremental VOR Adaptation
The angular vestibulo-ocular reflex (VOR) maintains images stable on the retina during rapid head rotations by rotating the eyes in the opposite direction to the head. Typically, the gain of the VOR is unity, that is, eye velocity magnitude is equal to head velocity magnitude. In this case, eye velocity divided by head velocity equals 1. However, after an injury to the peripheral vestibular organ or nerve, the VOR becomes weakened and does not generate an eye velocity of equal magnitude to the head velocity, in which case the gain is less than 1 (Halmagyi et al. 1990; Aw et al. 1996). When the VOR is injured, retinal image slip occurs that results in gaze instability during rapid head movements.
Rehabilitation exercises attempt to improve gaze instability during active head movements by increasing or “adapting up” the VOR gain and enlisting other oculomotor systems (Schubert et al. 2006, 2008a). However, the amount of VOR gain adaptation that occurs from these exercises is minimal, with little evidence that the VOR gain to passive head rotation changes at all (Herdman et al. 2007). In 2008, Schubert et al. developed the incremental velocity error method (Schubert et al. 2008a) for VOR adaptation. This method tasks subjects to make active head rotations while viewing a laser-projected target that moves in the opposite direction of the head at a fraction of the head velocity (Fig. 1; US Patent # 9782068; Todd et al. 2018). The target velocity then gradually increases over a period of 15 minutes until it reaches the head velocity (still oppositely directed).
Motion of the laser target during a training session where the left side is being adapted. The laser target appears stationary on the wall (gain of 1) for all rightward rotations. For leftward rotations, the VOR gain demand for epoch one is set to 1. The gain demand increases every epoch by 0.1. The dashed line shows the path of the laser target as seen by a stationary observer. For instance, during epoch 1, the laser appears to remain stationary. By epoch 10, the laser draws a long line on the wall in the opposite direction to the head – a gain of 1.9. (Modified from Todd et al. 2018)
We recently showed unilateral VOR short-term adaptation is possible in humans (Migliaccio and Schubert 2013). Nine normal subjects underwent the IVE protocol for rotations to one side (adapting side), but for rotations toward the other (non-adapting) side, the visual stimulus was removed. The result was a significant VOR gain increase toward the adapting side for both active (23%) and passive (11%) head rotations, suggesting that VOR short-term adaptation was the main mechanism minimizing retinal image slip (Fig. 2). In a later study, we showed that unilateral VOR adaptation in patients with an isolated peripheral vestibular lesion was possible for rotations toward the side(s) with VOR hypofunction (Migliaccio and Schubert 2014). The increase in VOR gain toward the ipsilesional ear was less consistent in patients compared to controls, but this may have been a compliance issue. Two of the six patients quickly learned the adaptation training exercise, i.e., within 5 minutes, and performed the training without complication. During active head impulses, both these subjects had significant adaptation toward the ipsilesional adapting side (+43.2% and + 39.2%) and minimal adaptation toward the non-adapting side (−14.3% and − 5.6%) (Fig. 3). These increases were greater than those seen in previous studies on bilateral and unilateral incremental adaptation training in unilateral vestibular hypofunction (UVH) subjects (Schubert et al. 2008b) and normal subjects (Migliaccio and Schubert 2013), respectively. Out of the remaining four, two learned the adaptation training exercise reasonably well but were inconsistent in terms of rotating their head with the correct velocity profile and keeping their eyes on the laser target. Notwithstanding, there was evidence of unilateral adaptation in these subjects also. The remaining two patients found the training task too difficult and could not proceed with the experiment. This study determined that the undesirable VOR gain increase (8%) toward the non-adapting side during active head rotations in Migliaccio and Schubert (2013) occurred because the target was extinguished during head rotations toward the non-adapting side. This unwanted adaptation was prevented when a stationary target was presented during head rotations toward the non-adapting side, thereby introducing an asymmetrical training error signal for bilateral head rotation (Migliaccio and Schubert 2014).
The active VOR measured during each training epoch for a typical subject. The active VOR gain for head impulses toward the adapting side steadily increased from 0.9 to 1.14 during unilateral incremental training. In contrast, the gain toward the non-adapting side did not vary during the training. Best-line fits (adapting side – thick-dashed black; non-adapting side – thin-dashed black) for the training data across all subjects (n = 9) show that there was a significant relationship between gain and training epoch number only for head impulses toward the adapting side. (From Migliaccio and Schubert 2013)
Comparison of ipsilesional (adapting side) active VOR gain pre- and post-adaptation training. In this UVH patient, the gain increased from 0.79 ± 0.07 to 1.10 ± 0.08, a gain increase of ~40%. In this same patient, the contralesional non-adapting gain went from 0.90 ± 0.5 preadaptation to 0.85 ± 0.8 post-adaptation, a ~5% decrease that was not significant. (From Migliaccio and Schubert 2014)
Gimmon et al. examined whether the right and left VOR gains could be synchronously adapted in opposing directions (Gimmon et al. 2018). To do so, they used three separate VOR adaptation sessions, randomized such that the VOR was adapted up-bilaterally, down-bilaterally, or mixed (one side up, opposite side down). Each subject made active (self-generated) head impulse rotations for 15 min while following the IVE method. VOR training demand changed by 10% every 90 seconds. The results revealed the human VOR can be simultaneously driven in opposite directions suggesting functionally independent VOR circuits for each side of head rotation. It appears, therefore, that the brain relies on the salient error signal to drive bilateral VOR adaptation. This fits with the credit assignment theory, which states that resource assignment toward motor learning occurs when the brain considers the error signal accurate and thus worthy of resource expenditure (Kording et al. 2007). In the case of a bilateral error signal, the VOR from each side can be driven independently; in the case of unilateral adaptation, the brain presumes the error signal to be accurate and therefore makes effort toward bilateral adaptation.
3 The Influence of Training Target Contrast on VOR Adaptation
Like the VOR, smooth pursuit and optokinetic systems seek to stabilize images on the retina using an image slip error signal (e.g., Cohen et al. 1981; Büttner and Büttner-Ennever 2006). Studies have shown that visual contrast affects the perceived velocity of a stimulus and the smooth pursuit following gain (= eye/target velocity) (Thompson 1982, 1983). Visual contrast also affects the slow-phase velocity of optokinetic nystagmus such that it increases with increasing contrast for a given speed (Sumnall et al. 2003). For both smooth pursuit and optokinetic nystagmus, contrast must pass a certain threshold for the detection of image motion. As contrast increases, the internal estimate of stimulus speed reconstructed from prior retinal (movement of the retinal image) and extraretinal signals (efference copy and other proprioceptive cues) becomes more accurate (Waddington and Harris 2015).
In a recent study, we examined the effect of visual target contrast on human unilateral VOR adaptation (Mahfuz et al. 2017). When the visual target during visual-vestibular mismatch training had contrast levels between 1.5 k and 1.4 M, the VOR gain increase due to adaptation training did not change, suggesting that at these levels, the effect of contrast on VOR adaptation had saturated. When target contrast was reduced to 261, the active and passive VOR gain increase toward the adapting side was no longer significant and was similar to the non-adapting side, suggesting that 261 was below the threshold needed for adaptation to occur. Modeling suggested that the contrast threshold for VOR adaptation to occur was 250 and that a contrast level of above 1000 was required for robust VOR adaptation (Fig. 4). Compare these values to the maximum contrast level obtained from a typical LCD monitor (24″ 1920 x 1080 resolution VS243 Asus, Taiwan) of 37.7 in an otherwise dark room.
Scatterplot of VOR gain percentage increase toward the adapting side (after pooling active and passive gains) versus the contrast level plot on a log10 scale. Two-segment piecewise regression (R2 = 0.26) determined a knot at 836, indicating that at this contrast level, there was a significant difference between the two lines, respectively, modeling the data below and above this contrast level. Three-segment analysis revealed a lower knot at 854 and an upper knot at 1.3 M. Four-segment modeling (R2 = 0.28) revealed three knots: 225 (lower), 1197 (middle), and 1.2 M (upper). Overall, our analysis suggests there was a transition period starting at ~225 and ending at ~1000 (i.e., between 836 and 1197) where the VOR gain percentage increase gradually increased. Below 225, there was no significant (but constant) adaptation, and above 1000, there was maximal adaptation. (From Mahfuz et al. 2017)
Low image contrast may explain why classic human studies using normal lighting and magnifying or minifying lenses with full fields of view to drive VOR adaptation required long periods of training to significantly affect the VOR gain (Gauthier and Robinson 1975; Gonshor and Jones 1976). Increasing contrast to 1.5 k was sufficient for robust and rapid VOR adaptation to occur (Mahfuz et al. 2017). However, it is unlikely that an increase in contrast is the only factor. A prior study under similar lighting conditions to the maximum contrast level in Mahfuz et al. (2017) found that incremental adaptation training, rather than “all at once” training (as occurs during classic lens training), resulted in significantly larger gain increases (Schubert et al. 2008b), suggesting that visual contrast is but one of several factors affecting VOR adaptation. Contrast might also explain why many patients with incomplete vestibular hypofunction often have slow and incomplete recovery of VOR gains despite long exposure to the normal visual environment that typically drives the VOR gain to unity. We suggest that visual target contrast should be an important consideration during VOR adaptation/rehabilitation training. These data suggest that optimal VOR gain training can be achieved using a bright target (as emitted by a typical laser pointer) in low ambient lighting, i.e., the typical lighting of a room with curtains closed and lights turned off. With critical rehabilitation implications, this study also established the incremental VOR gain adaptation method can be achieved in conditions of incomplete dark (Fig. 5, <8 lux).
Mean (± SD) adapting (black bars) and non-adapting (gray bars) side pre- to post-adaptation training VOR gain increase as a percentage for the active (top row) and passive (bottom row) VOR across all subjects (n = 12) for each contrast level. In parentheses, beside each contrast level is the ambient light level in lux and the target brightness as a percentage of maximum laser power. Statistical analysis indicates there is a significant difference in percentage gain increase between the adapting and non-adapting sides at all contrast levels above and equal to 1.5 k (left side of vertical dashed line). (* denotes a significant increase (t-test between adapting and non-adapting-side percentage increase, p < 0.05)). (From Mahfuz et al. 2017)
4 Position and Velocity Error Signal Driving VOR Adaptation
Retinal image movement is the likely feedback signal that drives VOR modification/adaptation for different viewing contexts. However, it was not clear whether a retinal image position or velocity error was used primarily as the feedback signal. In a recent study, we examined the effect of varying the retinal image position error update rates (frequencies) to understand the role of visual feedback in human VOR adaptation (Fadaee and Migliaccio 2016).
Using the human unilateral incremental VOR adaptation technique, the study showed that adaptation declined as the retinal image position error signal used to drive adaptation became less frequent, i.e., as the update rate decreased from 50 (the target position was updated once every 20 ms) to 15 Hz. For 50 and 20 Hz update rates, there was a significant increase in VOR gain toward the adapting side for both the active and passive VOR, whereas at 15 Hz, there was no longer any adaptation (Fig. 6).
The active VOR measured during each training epoch across all subjects (pooled data, mean ± SD) at three laser target position update rates (50 Hz [n = 13], 20 Hz [n = 12], and 15 Hz [n = 9]). The active VOR gain for head impulses toward the adapting side (black traces) steadily increased from ~1 to ~1.2 during unilateral incremental training at 50 Hz. Between epochs 2 and 10, the difference in gain between the adapting and non-adapting side (gray traces) became increasingly significant with increasing epoch number. Similarly, adaptation training at 20 Hz initially showed a trend of increasing difference between adapting and non-adapting-side gains, which became significant for epochs 7 to 10. In contrast, adaptation training at 15 Hz results in minimal unilateral adaptation as a group, so that the difference between sides is no longer a function of increasing epoch number (*p < 0.05, **p < 0.01, and ***p < 0.001). (From Fadaee and Migliaccio 2016)
Unlike strobe lighting, the visual stimulus during training in this study provided both a position and a velocity error signal because although the laser target position (in-space) update rate was a programmable variable, the laser target itself was always on, providing constant visual input. Consequently, when target position was updated during each head impulse, it drove adaptation to increase the VOR gain (> 1), but when target position was not updated (i.e., laser position did not change during most of the head impulse), it essentially drove the gain toward unity (gain = 1). In other words, the position and velocity errors drove the VOR gain to change in opposite directions. In this study, the active VOR gain increased by ~23% at 50 Hz update rate, which is the same as that observed at the 1000 Hz update rate used previously (Migliaccio and Schubert 2013). Similarly, in this study, the passive VOR gain increased by ~10% at 20 Hz update rate (i.e., two position cues per impulse), which is similar to the ~11% increase observed at the 50 times greater (1000 Hz) update rate used previously (Migliaccio and Schubert 2013). These findings suggest that a position error signal too can provide an effective adaptive drive for the VOR.
5 Active Versus Passive Head Rotation and VOR Adaptation
The majority of VOR training stimuli used in prior VOR adaptation studies have consisted of predictable head motion, either via self-generation or whole-body sinusoidal passive head rotation (Hattori et al. 2000; Solomon et al. 2003; Shelhamer et al. 1994; Paige and Sargent 1991; Gauthier and Robinson 1975; Schubert et al. 2008b; Migliaccio and Schubert 2013 and 2014, Fadaee and Migliaccio 2016). The passive head impulse is unpredictable in direction and timing (Halmagyi and Curthoys 1988) and is considered to be a more physiologically relevant stimulus than a single-frequency sinusoidal stimulus (as would be obtained from chair testing) due to its high-frequency content (up to 6 Hz). Additionally, the VOR must be responsive to unpredictable head motion, particularly at frequencies greater than 1 Hz (and velocities >100°/s) where the VOR becomes the main vision-stabilizing mechanism. Below 1 Hz (and velocities <100°/s), other vision-stabilizing systems such as smooth pursuit and the optokinetic reflex are likely to play the major role (Meyer et al. 1985). Finally, motor learning within the VOR is context specific (human: Shelhamer et al. 1992; primate: Yakushin et al. 2003; Schubert et al. 2008c), which suggests that adaptation will be greatest when the VOR training and testing conditions are the same. The training context might therefore result in differences in retention of VOR adaptation depending on the similarity between training and testing conditions.
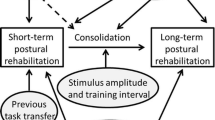
We recently examined the effects of passive versus active head movement training contexts on VOR adaptation and its short-term (1 hour) retention (Mahfuz et al. 2018). The results from this study suggest that in humans, the magnitude of unilateral VOR adaptation after active or passive head impulse training is the same for both the active and passive VOR. In other words, the active or passive head rotation context of the training had no effect on the VOR gain increase, suggesting that most of the adaptation observed, regardless of whether the stimulus was active or passive, was occurring in the central vestibular pathways common to both the active and passive VOR, as opposed to the nonoverlapping pathways. Similarly, the training context did not affect retention of VOR adaptation. The only factor that significantly affected retention over the 1 hour immediately after training was the brief exposure to a stationary fixation target before each head impulse during VOR testing (Fig. 7).
Normalized active (rows 1 and 3) and passive (rows 2 and 4) VOR gain percentage increases after active (top two rows) and passive (bottom two rows) VOR training toward the adapting side only. VOR gains were measured every 10 (first boxplot between dashed lines), 20 (second boxplot between dashed lines), or 60 minutes (third boxplot between dashed lines) for 60 minutes after adaptation training. In addition, the VOR gain was tested every 10 minutes, but the visual fixation light before the start of each impulse was only provided at testing times 0 and 60 minutes after adaptation training (fourth boxplot between dashed lines). Each box shows the median and goes from the first to the third quartile with whiskers denoting the maximum and minimum values. Taken together, these data suggest that the number of times the VOR is tested after training affects retention more so than the time lapsed after training. Gains measured immediately after active training and 60 minutes later with no other testing between these times (fourth boxplot) showed no significant loss in retention. (From Mahfuz et al. 2018)
Findings from this study suggest that as long as active head impulses have similar velocity profiles to passive head impulses, then optimal VOR training can be performed with active only head rotations, eliminating the need for expensive and bulky equipment (e.g., a rotary chair) or human assistance to deliver passive head impulses. Evidence from this study supports recent Cochrane meta-analysis studies that provide strong recommendations for vestibular rehabilitation providers to prescribe gaze stability exercises using active head rotation (Hillier and McDonnell 2011, 2016; McDonnell and Hillier 2015). Additionally, recent evidence suggests active head rotation training improves postural control (Matsugi et al. 2017). The only factor that affected short-term retention was the duration of exposure to a de-adaptation stimulus, which in this study drove the VOR gain down to unity. Presumably, retention would not be lost in vestibular patients whose ipsilesional VOR gain was increased due to training, but still below unity, because of the lack of a de-adaptation stimulus. In this case, real-world visual conditions would drive the VOR gain up to unity in vestibular patients and reinforce the training, rather than down to unity, and cancel the training as was the case in the healthy subjects used in this study.
6 The Effect of Aging on VOR Adaptation
Aging can have a profound impact on vestibular system function, as can be appreciated from the prevalence of vestibular-related disorders in the elderly. By the age of 70–80 years, a significant percent of our population has vestibular dysfunction – which is linked to increased dizziness and risk of falls (Agrawal et al. 2009). The prevalence of vestibular vertigo in this age group is three times that for young adults (< 30 years) (Neuhauser and Lempert 2009). Some of these symptoms are thought to be, in part at least, a consequence of senescence of the vestibular periphery (Ishiyama 2009). For example, approximately 40% of patients referred for fall risk assessment were found to have VOR deficits including abnormal gain, phase lead, and asymmetries (Jacobson et al. 2008). Aging has been shown to associate with loss of vestibular hair cells, vestibular afferents, and cells in the central vestibular nuclei (Johnsson 1971; Bergstrom 1973; Ross et al. 1976; Rosenhall 1973; Richter 1980; Lopez et al. 1997; Alvarez et al. 1998; Merchant et al. 2000; Velazquez-Villasenor et al. 2000; Park et al. 2001; Rauch et al. 2001).
We recently examined the effects of aging on the VOR and VOR adaptation in 30-month-old mice (equivalent to an 80-year-old human; Yuan et al. 2009) (Khan et al. 2017). This study showed that the baseline VOR gain for aged mice was significantly lower to controls during high-frequency, high-acceleration, transient head rotations (Khan et al. 2017). The study found that aging minimally affected the static counter-tilt response and sinusoidal VOR gain but significantly affected VOR adaptation, particularly for gain-decrease adaptation training (Fig. 8).
(a) Comparison of post-adaptation VOR gain for gain-increase (×1.5) (filled circles) and gain-decrease (×0.5) (open circles) adaptation training in young (top panel) and aged mice (bottom panel). The baseline VOR response is shown as dashed lines (mean). For both young and aged mice, the difference between VOR gains post gain increase and gain decrease after adaptation training was maximal when tested at the training velocity (20 o/s; left column). The effect of gain-increase adaptation was significant for both young and aged mice, whereas gain-decrease adaptation was only significant for young mice. The vertical dashed line represents the adaptation training frequency 0.5 Hz. (b) Comparison of gain-increase (×1.5) (filled circles) and gain-decrease (×0.5) (open circles) adaptation pooled across frequencies for each stimulus peak velocity (20, 50, and 100 o/s) in young (left panel) and aged mice (right panel). The mean baseline VOR response is shown by the dashed line. The vertical dashed line denotes the adaptation training velocity. VOR gain-decrease adaptation was ~85% lower in aged mice compared to young mice. VOR gain-increase adaptation was also significantly reduced in aged mice, albeit by a lesser extent of ~30%. (From Khan et al. 2017)
It is possible that vestibular plasticity mechanisms behind VOR adaptation and compensation normalize VOR function as structural losses to the vestibular system occur with aging. Presumably, there is a threshold of vestibular loss below which these plasticity mechanisms can no longer mask the underlying vestibular system deficit. This might explain why human VOR function is steady up to age 70, followed by a steep decline (Matiño-Soler et al. 2015). If VOR plasticity can compensate for potentially large vestibular losses due to aging, one could ask why does the behavioral VOR in patients with partial lesions to their vestibular organs not fully recover? The reason could be due to the sudden onset of the lesion. Our prior studies have shown that significant VOR adaptation can be induced in a short period of time if the VOR-adapting stimulus challenges the VOR gain to change in small increments (Schubert et al. 2008b; Migliaccio and Schubert 2013, 2014; Fadaee and Migliaccio 2016; Mahfuz et al. 2017, 2018). In contrast, when the required adaptive change is large, for example, when the VOR gain must double, then VOR adaptation becomes more difficult and less optimal (Gauthier and Robinson 1975; Schubert et al. 2008b). Unlike most other injuries, structural degradation due to aging is a gradual process, and so small losses in vestibular system function might be more easily accommodated by the VOR.
Some of this loss in VOR adaptation is likely explained by degeneration of the vestibulocerebellum, which plays a major role during VOR-dependent adaptation. Purkinje cells in the cerebellar flocculus are well positioned to encode information used to induce plasticity (Ito 1982; Lisberger and Pavelko 1986; Lisberger and Fuchs 1978). It has been postulated that gain-increase and gain-decrease VOR adaptation occurs through two distinct cerebellar mechanisms, with the former involving long-term depression (LTD) and the latter long-term potentiation (LTP) at Purkinje cells in the cerebellar flocculus, although other pathways and sites in the VOR circuitry are also implicated (Schonewille et al. 2011; Titley and Hansel 2016). Age-related degeneration of Purkinje cells could explain the Khan et al. (2017) results, if Purkinje cell death affected these two mechanisms differently. It is known that Purkinje cells in the cerebellum are particularly affected by aging with their number decreasing with age (Andersen et al. 2003; Rogers et al. 1984; Woodruff-Pak et al. 2010; Zhang et al. 2010). In humans, the decline in Purkinje cell population is less marked before age 60 but becomes pronounced afterward (Hall et al. 1975). Intriguingly, we observed a similar asymmetrical effect on VOR adaptation and compensation in alpha-9-knockout mice (these have an impaired cholinergic efferent vestibular system) (Hübner et al. 2015, 2017). Notably, cholinergic neurotransmission in the cerebellar flocculus has also been implicated in impaired gain-decrease VOR adaptation (Prestori et al. 2013). These findings raise the possibility of an involvement of the cholinergic system in the age-related changes in VOR adaptation.
7 New Developments in Vestibular Rehabilitation
7.1 Ipsilesional-Only Rotation
A recent case study used ipsilesional passive head rotation to reduce VOR gain asymmetry in a patient with a unilateral vestibular hypofunction (Binetti et al. 2017). The authors report that until applying the following method, the patient was unable to recover. The authors applied 10 epochs of 15 passive ipsilesional-only head impulses while the patient attempted to keep eyes focused on a stationary target (i.e., times one VOR exercise). The patient rested 30 seconds between each training epoch. This was repeated for five consecutive days. The authors used video HIT equipment to ensure head velocities were greater than 120 d/s. After training, the ipsilesional VOR gain improved 24% (pre 0.57 ± 0.11, post 0.71 ± 0.10). At 6- and 12-month follow-up, the patient reported no further vestibular symptoms.
7.2 Galvanic Vestibular Stimulation
Preliminary studies using galvanic vestibular stimulation suggest it may be able to improve postural stability in standing or while walking (Mulavara Fiedler et al. 2011; Pal et al. 2009). More recently, applying weak, nonlinear electrical signals that are imperceptible to human sensory threshold (stochastic resonance – SR) holds some promise at improving vestibular function and imbalance. Serrador et al. showed an improved gain of ocular counter roll (OCR) in elderly with an initially reduced OCR gain (Fig. 9). In those elderly with healthy OCR gain, the application of SR was negligible for the OCR (Serrador et al. 2018). Wuehr et al. used SR to reduce the variability of stride time, stride length, and base of support in patients with bilateral vestibular loss compared to sham control (Wuehr et al. 2016). Furthermore, the authors report most of the patients noted an improved sensation of walking balance most pronounced during slow gait speed.
OCR of one subject to 0.125 Hz during ±25° passive roll tilt during both no stimulation and SN trials. The bottom panel demonstrates the gain calculations from the linear regression. This subject demonstrated a significant increase in OCR from control (left side) to stimulation (right side). (From Serrador et al. 2018)
7.3 Auditory Feedback
Encouraging, though preliminary, evidence suggests auditory feedback may improve both balance and gait. A case series study suggests that patients with bilateral vestibular hypofunction and hearing impairment used hearing to improve both duration standing on foam and gait speed (Shayman et al. 2017).
7.4 Transcranial Cerebellar Direct Current Stimulation
Sixteen patients with chronic dizziness (> 6 months) due to UVH (e.g., vestibular neuritis, Ramsay Hunt syndrome) were treated for five days each performing three 25 min sessions of vestibular rehabilitation exercises every 4 hours. Subjects were randomized to the Sham group (VPT only) or Stim group (Koganemaru et al. 2017). On the first day only, the Stim group received 20 minutes of transcranial cerebellar direct current stimulation (tcDCS, 2 mA of electrical constant direct current). The tcDCS was applied via electrodes placed 2 cm below the inion, medial to the mastoid apophysis. Those subjects receiving the tcDCS showed significantly improved dizziness handicap inventory (DHI) scores for the physical and functional domains, in addition to the total scores compared with the VPT-only group.
7.5 Home Computerized Dynamic Visual Acuity
Crane and Schubert developed a home training device based on computerized dynamic visual acuity testing that involved wearing a rate sensor and interactive online software that subjects accessed using their own computers and internet service. The training asked subjects to move their heads and identify letters that flashed on the monitor only during rapid head rotation (>100 d/s) (Crane and Schubert 2018). Data revealed that subjects who previously tried vestibular rehabilitation but had no appreciable improvement in their dizziness handicap inventory (DHI) showed significantly improved DHI scores after completing 4 weeks of the home therapy regimen. Initial mean DHI was 42 (range, 32–56) and post DHI (4 weeks) was 11.5 (p < 0.004; range, 0–16). Three of the subjects continued to do the home treatment and noted a further reduction in DHI (range, 2–6; p < 0.002).
7.6 Virtual Reality
There remains an impression that virtual reality (VR) applications hold great promise as an exciting and better method to deliver vestibular rehabilitation. However, recent studies that have directly compared physical therapy outcomes using VR versus traditional VPT reveal no advantage in using virtual reality (Alahmari et al. 2014; Smaerup et al. 2017; Micarelli et al. 2017). As technology advances, VR certainly may offer unique training regimens, but for now, it appears to offer only a more engaging rehabilitation experience at best.
7.7 Atypical Medical Populations
More recently, VPT has been used in nontraditional medical populations that include stroke, attention deficit disorder, and headache. Using a controlled and randomized design, patients with hemorrhagic or ischemic strokes with onset less than 6 months were randomized into either VPT or traditional CVA rehab groups (Mitsutake et al. 2017). The VPT group included VOR gaze stability and gait stability exercises; the CVA group performed exercises focused on muscle strength, posture and gait exercises, range of motion, and walking indoors and outdoors. After 3 weeks of treatment, the VPT group showed a significantly improved fall risk score (assessed by the Dynamic Gait Index) and ability to move their head quickly and read letters (assessed by the gaze stability test), compared to the CVA group.
Children with attention deficit disorder and concurrent vestibular impairment were randomized into a VPT or control group (Lotfi et al. 2017). The VPT group did 45 min of exercise two times per week for 12 weeks that include gaze stability, postural stability, and daily living activities. The control group received no intervention. After 12 weeks, choice reaction time and spatial working memory significantly improved only for those children in the VPT group. The authors concluded that the severity of vestibular pathology should be assessed in children with ADHD and that inclusion of such children into a VPT program can improve their cognitive abilities.
Finally, a study compared the effect of VPT to reduce headache, reduce fall risk, and reduce dizziness in two types of sufferers – vestibular migraine and tension type (Sugaya et al. 2017). The VPT improved headache, fall risk, dizziness, and psychological factors as measured by the Hospital Anxiety and Depression Scale and Somatosensory Catastrophizing Scale. What was novel was the improvement of symptoms in the patients with tension-type headache. Although this study confirmed patients with vestibular migraine had the greater reduction in symptoms, literature already has confirmed benefit in this patient population (Whitney et al. 2000; Vitkovic et al. 2013).
8 Conclusion
Vestibular rehabilitation will remain useful and first line of defense in treating the functional deficits associated with reduced vestibular sensation. Dosing amounts for VPT remain unknown, though exciting new technologies such as incremental VOR adaptation holds promise that more efficient delivery is possible.
References
Agrawal, Y., Carey, J. P., Della Santina, C. C., Schubert, M. C., & Minor, L. B. (2009). Disorders of balance and vestibular function in US adults: Data from the National Health and Nutrition Examination Survey, 2001–2004. Archives of Internal Medicine, 169, 938–944.
Alahmari, K. A., Sparto, P. J., Marchetti, G. F., Redfern, M. S., Furman, J. M., & Whitney, S. L. (2014). Comparison of Virtual Reality Based Therapy with Customized Vestibular Physical Therapy for the Treatment of Vestibular Disorders. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 22(2), 389–399. PMCID: PMC5527704.
Alvarez, J. C., Díaz, C., Suárez, C., Fernández, J. A., González del Rey, C., Navarro, A., & Tolivia, J. (1998). Neuron loss in human medial vestibular nucleus. The Anatomical Record, 251, 431–438.
Andersen, B. B., Gundersen, H. J., & Pakkenberh, B. (2003). Ageing of the human cerebellum: A stereological study. The Journal of Comparative Neurology, 466, 356–365.
Aw, S. T., Halmagyi, G. M., Haslwanter, T., Curthoys, I. S., Yavor, R. A., & Todd, M. J. (1996). Three-dimensional vector analysis of the human vestibuloocular reflex in response to high-acceleration head rotations. II. Responses in subjects with unilateral vestibular loss and selective semicircular canal occlusion. Journal of Neurophysiology, 76, 4021–4030.
Bergstrom, B. (1973). Morphology of the vestibular nerve: Part II- the number of myelinated vestibular nerve fibers in man at various ages. Acta Oto-Laryngologica, 76, 173–179.
Binetti, A. C., Varela, A. X., Lucarelli, D. L., & Verdecchia, D. H. (2017). Unilateral head impulses training in uncompensated vestibular hypofunction. Case Reports in Otolaryngology, 2017, 2145173. PMID: 28243476.
Büttner, U., & Büttner-Ennever, J. A. (2006). Present concepts of oculomotor organization. Progress in Brain Research, 151, 1–42.
Cohen, B., Henn, V., Raphan, T., & Dennett, D. (1981). Velocity storage, nystagmus, and visual-vestibular interactions in humans. Annals of the New York Academy of Sciences, 374, 421–433.
Crane, B. T., & Schubert, M. C. (2018). An adaptive vestibular rehabilitation technique. The Laryngoscope, 128(3), 713–718. PMID: 28543062.
Fadaee, S. B., & Migliaccio, A. A. (2016). The effect of retinal image error update rate on human vestibulo-ocular reflex gain adaptation. Experimental Brain Research, 234(4), 1085–1094.
Gauthier, G. M., & Robinson, D. A. (1975). Adaptation of the human vestibuloocular reflex to magnifying lenses. Brain Research, 92, 331–335.
Gonshor, A., & Jones, G. M. (1976). Short-term adaptive changes in the human vestibulo-ocular reflex arc. Journal of Physiology, 256, 361–379.
Gimmon Y, Migliaccio AA, Todd C, Figtree W, Schubert MC. (2018). Simultaneous laterally-inversive vestibulo-ocular reflex adaptation during head impulses. American Physical Therapy Association, combined sections meeting, New Orleans, LA.
Hall, C. D., Schubert, M. C., & Herdman, S. J. (2004). Prediction of fall risk reduction as measured by dynamic gait index in individuals with unilateral vestibular hypofunction. Otology & Neurotology, 25(5), 746–751.
Hall, C. D., Herdman, S. J., Whitney, S. L., Cass, S. P., Clendaniel, R. A., Fife, T. D., Furman, J. M., Getchius, T. S., Goebel, J. A., Shepard, N. T., & Woodhouse, S. N. (2016). Vestibular rehabilitation for peripheral vestibular hypofunction: An evidence-based clinical practice guideline: From the American Physical Therapy Association Neurology Section. Journal of Neurologic Physical Therapy, 40(2), 124–155. PMID: 26913496.
Hall, T. C., Miller, A. K. H., Corsellis, J. A. N. (1975). Variation in the human purkinje cell population according to age and sex. Neuropathol Appl Neurobiol, 1, 267–292.
Halmagyi, G. M., & Curthoys, I. S. (1988). A clinical sign of canal paresis. Archives of Neurology, 45, 737–739.
Halmagyi, G. M., Curthoys, I. S., Cremer, P. D., Todd, M. J., & Curthoys, I. S. (1990). The human horizontal vestibulo-ocular reflex in response to high-acceleration stimulation before and after unilateral vestibular neurectomy. Experimental Brain Research, 81, 479–490.
Hattori, K., Watanabe, S., Nakamura, T., & Kato, I. (2000). Flexibility in the adaptation of the vestibulo-ocular reflex to modified visual inputs in humans. Nihon Jibiinkoka Gakkai Kaiho, 103, 1186–1194.
Herdman, S. J., Schubert, M. C., Das, V. E., & Tusa, R. J. (2003). Recovery of dynamic visual acuity in unilateral vestibular hypofunction. Archives of Otolaryngology – Head & Neck Surgery, 129(8), 819–824.
Herdman, S. J., Hall, C. D., Schubert, M. C., Das, V. E., & Tusa, R. J. (2007). Recovery of dynamic visual acuity in bilateral vestibular hypofunction. Archives of Otolaryngology – Head & Neck Surgery, 133(4), 383–389.
Hillier, S. L., & McDonnell, M. (2011). Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database of Systematic Reviews, (2), CD005397. https://doi.org/10.1002/14651858.CD005397.pub3.
Hillier, S., & McDonnell, M. (2016). Is vestibular rehabilitation effective in improving dizziness and function after unilateral peripheral vestibular hypofunction? An abridged version of a Cochrane Review. European Journal of Physical and Rehabilitation Medicine, 52, 541–556.
Hilton, M., & Pinder, D. (2004). The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database of Systematic Reviews, (2), CD003162. Review. Update in: Cochrane Database Syst Rev. 2014;12: CD003162.
Huang, K., Sparto, P. J., Kiesler, S., Siewiorek, D. P., & Smailagic, A. (2014). iPod-based in-home system for monitoring gaze-stabilization exercise compliance of individuals with vestibular hypofunction. Journal of Neuroengineering and Rehabilitation, 11, 69. https://doi.org/10.1186/1743-0003-11-69.
Hübner, P. P., Khan, S. I., & Migliaccio, A. A. (2015). The mammalian efferent vestibular system plays a crucial role in the high-frequency response and short-term adaptation of the vestibulo-ocular reflex. Journal of Neurophysiology, 114(6), 3154–3165.
Hübner, P. P., Khan, S. I., & Migliaccio, A. A. (2017). The mammalian efferent vestibular system plays a crucial role in vestibulo-ocular reflex compensation after unilateral labyrinthectomy. Journal of Neurophysiology, 117(4), 1553–1568.
Ishiyama, G. (2009). Imbalance and vertigo: The aging human vestibular periphery. Seminars in Neurology, 29, 491–499.
Ito, M. (1982). Cerebellar control of the vestibulo-ocular reflex—Around the flocculus hypothesis. Annual Review of Neuroscience, 5, 275–296.
Jacobson, G. P., McCaslin, D. L., Grantham, S. L., & Piker, E. G. (2008). Significant vestibular system impairment is common in a cohort of elderly patients referred for assessment of falls risk. Journal of the American Academy of Audiology, 19, 799–807.
Johnsson, L. G. (1971). Degenerative changes and anomalies of the vestibular system in man. Laryngoscope, 81, 1682–1694.
Khan, S. I., Hübner, P. P., Brichta, A. M., Smith, D. W., & Migliaccio, A. A. (2017). Ageing reduces the high-frequency and short-term adaptation of the vestibulo-ocular reflex in mice. Neurobiology of Aging, 51, 122–131.
Koganemaru, S., Goto, F., Arai, M., Toshikuni, K., Hosoya, M., Wakabayashi, T., Yamamoto, N., Minami, S., Ikeda, S., Ikoma, K., & Mima, T. (2017). Effects of vestibular rehabilitation combined with transcranial cerebellar direct current stimulation in patients with chronic dizziness: An exploratory study. Brain Stimulation, 10(3), 576–578.
Kording, K. P., Tenenbaum, J. B., & Shadmehr, R. (2007). The dynamics of memory as a consequence of optimal adaptation to a changing body. Nature Neuroscience, 10(6), 779–786. Epub 2007 May 13..
Lisberger, S. G., & Pavelko, T. A. (1986). Vestibular signals carried by pathways subserving plasticity of the vestibulo-ocular reflex in monkeys. The Journal of Neuroscience, 6, 346–354.
Lisberger, S. G., & Fuchs, A. F. (1978). Role of primate flocculus during rapid behavioral modification of vestibule-ocular reflex. I. Purkinje cell activity during visually guided horizontal smooth-pursuit eye movements and passive head rotation. Journal of Neurophysiology, 41, 733–763.
Lopez, I., Honrubia, V., & Baloh, R. W. (1997). Ageing and the human vestibular nucleus. Journal of Vestibular Research, 7, 77–85.
Lotfi, Y., Rezazadeh, N., Moossavi, A., Haghgoo, H. A., Rostami, R., Bakhshi, E., Badfar, F., Moghadam, S. F., Sadeghi-Firoozabadi, V., & Khodabandelou, Y. (2017). Preliminary evidence of improved cognitive performance following vestibular rehabilitation in children with combined ADHD (cADHD) and concurrent vestibular impairment. Auris, Nasus, Larynx, 44(6), 700–707. PMID: 28238393.
Mahfuz, M. M., Schubert, M. C., Todd, C. J., Figtree, W. V. C., Khan, S. I., & Migliaccio, A. A. (2017). The effect of visual contrast on human vestibulo-ocular reflex training. Journal of the Association for Research in Otolaryngology, 19(1), 113–122.
Mahfuz, M. M., Schubert, M. C., Figtree, W. V. C., Todd, C. J., Khan, S. I., & Migliaccio, A. A. (2018). Optimal human passive vestibulo-ocular reflex adaptation does not rely on passive training. Journal of the Association for Research in Otolaryngology, 19(3), 261–271.
Matiño-Soler, E., Esteller-More, E., Martin-Sanchez, J. C., Martinez-Sanchez, J. M., & Perez-Fernandez, N. (2015). Normative data on angular vestibule-ocular responses in the yaw axis measured using the video head impulse test. Otology & Neurotology, 36, 466–471.
Matsugi, A., Ueta, Y., Oku, K., Okuno, K., Tamaru, Y., Nomura, S., Tanaka, H., & Mori, N. (2017). Effect of gaze-stabilization exercises on vestibular function during postural control. Neuroreport, 28, 439–443.
McDonnell, M. N., & Hillier, S. L. (2015). Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database of Systematic Reviews, 1, CD005397. https://doi.org/10.1002/14651858.CD005397.pub4.
Meldrum, D., Herdman, S., Moloney, R., Murray, D., Duffy, D., Malone, K., French, H., Hone, S., Conroy, R., & McConn-Walsh, R. (2012). Effectiveness of conventional versus virtual reality based vestibular rehabilitation in the treatment of dizziness, gait and balance impairment in adults with unilateral peripheral vestibular loss: a randomised controlled trial. BMC Ear, Nose and Throat Disorders, 12, 3. https://doi.org/10.1186/1472-6815-12-3.
Merchant, S. N., Velazquez-Villasenor, L., Tsuji, K., Glynn, R. J., Wall, C., & Rauch, S. D. (2000). Temporal bone studies of the human peripheral vestibular system. Normative vestibular hair cell data. The Annals of Otology, Rhinology, and Laryngology, 181, 3–13.
Meyer, C. H., Lasker, A. G., & Robinson, D. A. (1985). The upper limit of human smooth pursuit velocity. Vision Research, 25, 561–563.
Micarelli, A., Viziano, A., Augimeri, I., Micarelli, D., & Alessandrini, M. (2017). Three-dimensional head-mounted gaming task procedure maximizes effects of vestibular rehabilitation in unilateral vestibular hypofunction: A randomized controlled pilot trial. International Journal of Rehabilitation Research, 40(4), 325–332. PMID: 28723718.
Migliaccio, A. A., & Schubert, M. C. (2013). Unilateral adaptation of the human angular vestibulo-ocular reflex. Journal of the Association for Research in Otolaryngology, 14(1), 29–36.
Migliaccio, A. A., & Schubert, M. C. (2014). Pilot study of a new rehabilitation tool: Improved unilateral short-term adaptation of the human angular vestibulo-ocular reflex. Otology & Neurotology, 35(10), e310–e316.
Mitsutake, T., Sakamoto, M., Ueta, K., Oka, S., & Horikawa, E. (2017). Effects of vestibular rehabilitation on gait performance in poststroke patients: A pilot randomized controlled trial. International Journal of Rehabilitation Research, 40(3), 240–245. PMID: 28542112.
Mulavara Fiedler, M. J., Kofman, I. S., Wood, S. J., Serrador, J. M., Peters, B., Cohen, H. S., Reschke, M. F., & Bloomberg, J. J. (2011). Improving balance function using vestibular stochastic resonance: Optimizing stimulus characteristics. Experimental Brain Research, 210, 303–312. PMID: 21442221.
Neuhauser, H. K., & Lempert, T. (2009). Vertigo: epidemiologic aspects. Semin Neurol, 29, 473–481. Ogata R, Ikari K, Hayashi M, Tamai K. Age related changes in the Purkinje’s cells in the rat cerebellar cortex: a quantitative electron microscopic study. Folia Psychiatrica et Neurologica Japonica 1984;38.159–67.
Paige, G. D., & Sargent, E. W. (1991). Visually-induced adaptive plasticity in the human vestibulo-ocular reflex. Experimental Brain Research, 84(1), 25–34.
Pal, S., Rosengren, S. M., & Colebatch, J. G. (2009). Stochastic galvanic vestibular stimulation produces a small reduction in sway in Parkinson’s disease. Journal of Vestibular Research, 19, 137–142.
Park, J. J., Tang, Y., Lopez, I., & Ishiyama, A. (2001). Age-related change in the number of neurons in the human vestibular ganglion. The Journal of Comparative Neurology, 431, 437–443.
Prestori, F., Bonardi, C., Mapelli, L., Lombardo, P., Goselink, R., De Stefano, M. E., Gandolfi, D., Mapelli, J., Bertrand, D., Schonewille, M., De Zeeuw, C., & D'Angelo, E. (2013). Gating of long-term potentiation by nicotinic acetylcholine receptors at the cerebellum input stage. PLoS One, 8, e64828.
Rauch, S. D., Velazquez-Villasenor, L., Dimitri, P. S., & Merchant, S. N. (2001). Decreasing hair cell counts in aging humans. Annals of the New York Academy of Sciences, 942, 220–227.
Richter, E. (1980). Quantitative study of human Scarpa’s ganglion and vestibular sensory epithelia. Acta Oto-Laryngologica, 90, 199–208.
Rogers, J., Zornetzer, S. F., Bloom, F. E., & Mervis, R. E. (1984). Senescent microstructural changes in rat cerebellum. Brain Research, 292, 23–32.
Rosenhall, U. (1973). Degenerative patterns in the aging human vestibular neuro-epithelia. Acta Oto-Laryngologica, 76, 208–220.
Ross, M. D., Peacor, D., Johnsson, L. G., & Allard, L. F. (1976). Observation on normal and degenerating human otoconia. The Annals of Otology, Rhinology, and Laryngology, 85, 310–326.
Schonewille, M., Gao, Z., Boele, H. J., Veloz, M. F., Amerika, W. E., Simek, A. A., De Jeu, M. T., Steinberg, J. P., Takamiya, K., Hoebeek, F. E., Linden, D. J., Huganir, R. L., & De Zeeuw, C. I. (2011). Reevaluating the role of LTD in cerebellar motor learning. Neuron, 70, 43–50.
Schubert, M. C., Migliaccio, A. A., & Della Santina, C. C. (2006). Modification of compensatory saccades after VOR gain recovery. Journal of Vestibular Research, 16, 285–291.
Schubert, M. C., Migliaccio, A. A., Clendaniel, R. A., Allak, A., & Carey, J. P. (2008a). Mechanism of dynamic visual acuity recovery with vestibular rehabilitation. Archives of Physical Medicine and Rehabilitation, 89(3), 500–507. PMID: 18295629.
Schubert, M. C., Della Santina, C. C., & Shelhamer, M. (2008b). Incremental angular vestibulo-ocular reflex adaptation to active head rotation. Experimental Brain Research, 191(4), 435–446. PMID: 18712370.
Schubert, M. C., Migliaccio, A. A., Minor, L. B., & Clendaniel, R. A. (2008c). Retention of VOR gain following short-term VOR adaptation. Experimental Brain Research, 187, 117–127.
Serrador, J. M., Deegan, B. M., Geraghty, M. C., & Wood, S. J. (2018). Enhancing vestibular function in the elderly with imperceptible electrical stimulation. Scientific Reports, 8(1), 336. PMID: 29321511.
Shelhamer, M., Robinson, D. A., & Tan, H. S. (1992). Context-specific adaptation of the gain of the vestibulo-ocular reflex in humans. Journal of Vestibular Research, 2, 89–96.
Shelhamer, M., Tiliket, C., Roberts, D., Kramer, P. D., & Zee, D. S. (1994). Short-term vestibulo-ocular reflex adaptation in humans. II. Error signals. Experimental Brain Research, 100, 328–336.
Solomon, D., Zee, D. S., & Straumann, D. (2003). Torsional and horizontal vestibular ocular reflex adaptation: Three-dimensional eye movement analysis. Experimental Brain Research, 152, 150–155.
Sugaya, N., Arai, M., & Goto, F. (2017). Is the headache in patients with vestibular migraine attenuated by vestibular rehabilitation? Frontiers in Neurology, 8, 124.
Sumnall, J. H., Freeman, T. C., & Snowden, R. J. (2003). Optokinetic potential and the perception of head-centred speed. Vision Research, 43, 1709–1718.
Shayman, C. S., Earhart, G. M., & Hullar, T. E. (2017). Improvements in gait with hearing aids and cochlear implants. Otology & Neurotology, 38(4), 484–486. PMID:28187057.
Smaerup, M., Grönvall, E., Larsen, S. B., Laessoe, U., Henriksen, J. J., & Damsgaard, E. M. (2017). Exercise gaming – A motivational approach for older adults with vestibular dysfunction. Disability and Rehabilitation. Assistive Technology, 12(2), 137–144. Epub 2016 Jan 4.
Titley, H. K., & Hansel, C. (2016). Asymmetries in cerebellar plasticity and motor learning. Cerebellum, 15, 87–92.
Thompson, P. (1982). Perceived rate of movement depends on contrast. Vision Research, 22, 377–380.
Thompson, P. (1983). Discrimination of moving gratings at and above detection threshold. Vision Research, 23, 1533–1538.
Todd, C. J., Hübner, P. P., Hübner, P., Schubert, M. C., & Migliaccio, A. A. (2018). StableEyes – A Portable vestibular rehabilitation device. IEEE Trans Neural Syst Rehabil Eng. 2018 Jun;26. (6):1223–1232. https://doi.org/10.1109/TNSRE.2018.2834964. PMID: 29877847.
Velazquez-Villasenor, L., Merchant, S. N., Tsuji, K., Glynn, R. J., Wall, C., 3rd, & Rauch, S. D. (2000). Temporal bone studies of the human peripheral vestibular system. Normative Scarpa’s ganglion cell data. The Annals of Otology, Rhinology, and Laryngology, 181, 14–19.
Vitkovic, J., Winoto, A., Rance, G., Dowell, R., & Paine, M. (2013). Vestibular rehabilitation outcomes in patients with and without vestibular migraine. Journal of Neurology, 260(12), 3039–3048. PMID: 24061769.
Waddington, J., & Harris, C. M. (2015). Human optokinetic nystagmus and spatial frequency. Journal of Vision, 15, 7. https://doi.org/10.1167/15.13.7.
Whitney, S. L., Wrisley, D. M., Brown, K. E., & Furman, J. M. (2000). Physical therapy for migraine-related vestibulopathy and vestibular dysfunction with history of migraine. The Laryngoscope, 110(9), 1528–1534. PMID: 10983955.
Woodruff-Pak, D. S., Foy, M. R., Akopian, G. G., Lee, K. H., Zach, J., Nguyen, K. P., Comalli, D. M., Kennard, J. A., Agelan, A., & Thompson, R. F. (2010). Differential effects and rates of normal aging in cerebellum and hippocampus. Proceedings of the National Academy of Sciences, 107, 1624–1629.
Wuehr, M., Nusser, E., Decker, J., Krafczyk, S., Straube, A., Brandt, T., Jahn, K., & Schniepp, R. (2016). Noisy vestibular stimulation improves dynamic walking stability in bilateral vestibulopathy. Neurology, 86(23), 2196–2202.
Yakushin, S. B., Raphan, T., & Cohen, B. (2003). Gravity-specific adaptation of the angular vestibuloocular reflex: Dependence on head orientation with regard to gravity. Journal of Neurophysiology, 89, 571–586.
Yuan, R., Tsaih, S. W., Petkova, S. B., Marin de Evsikova, C., Xing, S., Marion, M. A., Bogue, M. A., Mills, K. D., Peters, L. L., Bult, C. J., Rosen, C. J., Sundberg, J. P., Harrison, D. E., Churchill, G. A., & Paigen, B. (2009). Aging in inbred strains of mice: study design and interim report on median lifespans and circulating IGF1 levels. Aging Cell, 8, 277–287.
Zhang, C., Zhu, Q., & Hua, T. (2010). Aging of cerebellar Purkinje cells. Cell and Tissue Research, 341, 341–347.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Migliaccio, A.A., Schubert, M.C. (2019). Advanced Vestibular Rehabilitation. In: Shaikh, A., Ghasia, F. (eds) Advances in Translational Neuroscience of Eye Movement Disorders. Contemporary Clinical Neuroscience. Springer, Cham. https://doi.org/10.1007/978-3-030-31407-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-31407-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31406-4
Online ISBN: 978-3-030-31407-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)