Abstract
To assess the association, at diagnosis, between amyotrophic lateral sclerosis (ALS) and dementia in a large cohort of well-characterized Italian patients. We investigated the phenotypic profile of 1638 incident patients with definite, probable or laboratory-supported probable ALS, diagnosed from January 2009 to December 2013 in 13 Italian Referral Centers, located in 10 Italian Regions, and classified in two independent subsamples accounting for presence or not of dementia. The collected ALS features, including survival and other follow-up data, were compared between the two subgroups using a one-way analysis of variance and Chi-square test, as appropriate, logistic regression models and Kaplan–Meier survival analysis. Between-subgroup comparisons showed an older age at clinical observation (p = .006), at onset and at diagnosis (p = .002) in demented versus non demented ALS patients. After adjustment for these variables, diagnosis of dementia was significantly associated with higher odds of family history of ALS (p = .001) and frontotemporal dementia (p = .003) and of bulbar onset (p = .004), and lower odds of flail leg phenotype (p = .019) and spinal onset (p = .008). The median survival time was shorter in demented versus non-demented patients, especially in case of classical, bulbar and flail limb phenotypes and both bulbar and spinal onset. Our multicenter study emphasized the importance of an early diagnosis of comorbid dementia in ALS patients, which may have clinical impact and prognostic relevance. Moreover, our results may give further inputs to validation of ALS-specific tools for the screening of cognitive impairment in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder defined by loss of motor neurons, although growing evidence supports the multisystem extent of the disease, also affecting extra-motor functions, even in the earlier stages [1]. In particular, the concomitant cognitive impairment, ranging from mild cognitive or behavioural changes to frontotemporal lobar degeneration (FTLD) spectrum disorder, has been identified as prevalent in several cohorts of ALS patients, with the diagnosis of dementia occurring in rates of about 6–15% [2,3,4]. Interestingly, comorbid dementia has been associated with a shorter survival [4,5,6,7]. Furthermore, it has been shown that, also in the absence of dementia, executive dysfunction represents an important negative prognostic indicator in ALS [4, 7, 8]. However, although the effects of cognitive impairment on the survival time of ALS patients have been explored in previous studies [4,5,6,7,8,9], the potential effects of the association between dementia and other prognostic factors, such as disease onset and phenotype, has not been investigated in larger cohorts of ALS patients.
To fill up this gap, we performed a large multicenter study, focusing on the association between dementia and the clinical prognostic factors described in ALS.
Materials and methods
Patient data collection
The study has been performed in 13 ALS Italian referral centers, located in 10 Italian Regions, with a wide experience in multidisciplinary management of motor neuron diseases: ALS Centers of Turin, Padua, Genoa, Naples, Modena, Lecce, Rome, NEMO Clinical Centers in Milan, and Messina, ALS Centers of ICS Maugeri in Milan and Mistretta, ALS Centers at San Raffaele Institute and Istituto Auxologico Italiano in Milan [10].
The study included patients diagnosed with definite, probable or laboratory-supported probable ALS from January 1st, 2009 to December 31st, 2013 according to revised El Escorial criteria [11].
Data have been recorded into an electronic database available to all involved centers. Caring neurologists collected a detailed phenotypic profile for each ALS patient, including the following information: demographic data, age at onset, clinical observation and diagnosis, gender, site and time of onset, clinical phenotype [classic, bulbar, predominant upper motor neuron (UMN-p), flail arm, flail leg and respiratory ALS] [12], presence of concomitant dementia and family history of neurodegenerative disorders. At follow-up the following clinical information were collected: dates of percutaneous endoscopic gastrostomy (PEG), non-invasive ventilation (NIV) and tracheotomy/death.
Diagnosis of comorbid Alzheimer-type dementia and FTLD was based on New Research Criteria for the Diagnosis of Alzheimer disease [13] and ALS-frontotemporal spectrum disorder (ALS-FTSD) diagnostic criteria [14]. In particular, ALS-FTLD patients were originally diagnosed according to consensus criteria by Strong et al. [15] (i.e., ALS which coexists with a frontotemporal dementia, as defined by the Neary or Hodges criteria) and this diagnosis has been retrospectively confirmed in all cases according to the most recent ALS-FTSD criteria for ALS-FTD [14], accounting for both behavioural/cognitive dysfunctions [16] and/or language impairment. The neuropsychological battery performed allowed to evaluate five cognitive domains (i.e., executive function, memory, language, visuospatial skills and behaviour—for more details, see supplemental materials).
This study was approved by the Ethical Committees of the participating ALS centers.
Statistical analysis
Descriptive statistics of the two selected sub-samples (i.e., demented and non-demented patients) are reported as count and percentage, for categorical variables, or mean and standard deviation, for continuous variables. The between-subgroup comparisons were performed by one-way analysis of variance (ANOVA) and Chi square (χ 2), when appropriate.
With regard to the multivariate analysis, fifteen logistic regression models were used to compare the risk of ALS in demented versus non-demented patients in occurrence of: tracheotomy (I); PEG (II); NIV (III); familial history of ALS (IV), Parkinson’s disease (V) and FTLD (VI); and classic (VII), bulbar (VIII), flail arm (IX), flail leg (X), UMN-p (XI) and respiratory (XII) phenotypes, and spinal (XIII), bulbar (XIV), and respiratory (XV) onsets. All models were adjusted for demographic and clinical variables, which were significantly different by comparing the two subgroups of patients. Moreover, the variables were included in the logistic regression models using hierarchical or block-wise entry method. The results of multivariate analysis are presented as adjusted odds ratios (adjOR), with 95% confidence intervals (95% CI).
Survival time was defined as time from symptoms onset to death/tracheotomy. Univariate assessment of the survival effect of categorical variables was carried out by Kaplan–Meier survival analysis and equality of outcome was assessed using the log-rank test (\(\chi_{{{ \log } - {\text{rank test}}}}^{2}\)). A p value < .05 was significant. The analyses were carried out using SPSS version 19 (SPSS Inc., Chicago, IL, USA).
Results
For this study we collected 1638 incident patients with ALS. Table 1 shows descriptive statistics of each sub-group of ALS patients. In particular, with regard to demographic and clinical variables, age (at onset, diagnosis and clinical observation) was significantly higher in ALS patients with dementia (n = 163), fulfilling the diagnostic criteria for ALS-FTD [14, 15], compared to those with no evidence of dementia (n = 1475) (Table 1). In particular, all patients met the international consensus criteria for bvFTD [16] and psychotic symptoms, including hallucinations, delirium and aggressiveness, were reported in 11 patients. All patients with ALS-FTD showed predominant frontotemporal hypometabolism or hypoperfusion in single photon emission computed tomography or (18)F-fluorodeoxyglucose positron emission tomography (PET), according to international consensus criteria for probable bvFTD [16], although data about PET tracer (11)C-labeled Pittsburgh Compound-B ((11)C-PIB), specifically binding fibrillar amyloid-beta plaques, and cerebrospinal fluid (CSF) markers (i.e., biomarkers of amyloid metabolism and plaques, tau/TDP43 pathology, neuronal/axonal degeneration and neuroinflammation/astroglial activation) were not collected and available for this study.
After adjustment for age, between-subgroup comparisons showed that diagnosis of dementia was associated with higher adjORs of bulbar onset, familial history of ALS and FTLD and lower adjORs of flail leg phenotype and spinal onset (Table 2).
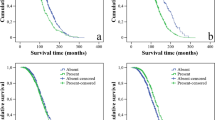
Log-rank test for equality of survival functions showed that the median survival time in demented patients was 13 months shorter in comparison to those without dementia [median survival of 29 months (95% CI 25–33) and 42 months (95% CI 39–45), respectively] (Fig. 1). These results were confirmed when the two subgroups were stratified for site of onset and phenotype, showing significant between-subgroup differences in the median survival time in case of classic, bulbar and flail limb phenotype (Fig. 2a–c) and bulbar and spinal onsets (Fig. 2d, e). Conversely, no significant differences in mean survival time were observed between the two subgroups in case of respiratory onset/phenotype and UMN-p variant.
Discussion
Our study, performed on a large ALS cohort coming from the main tertiary referral centers in Italy, supports the prognostic impact of comorbid FTLD in ALS patients. We revealed that, compared to non-demented patients, newly diagnosed ALS patients with comorbid FTLD are older, at higher risk of bulbar onset and with shorter survival, especially in case of classical, bulbar and flail limb phenotype. These results are mostly consistent with previous investigations [2,3,4, 8, 9], although the large sample size and the stratification in different clinical variants are valuable aspects of our analysis.
The described association between older age and comorbid FTLD, although confirming some previous evidence [4, 5], was not consistent with other investigations [3, 7, 8], probably because of the different sample sizes examined. To note, most studies found that older age at onset is among the known factors for a poor ALS prognosis [17,18,19], significantly impacting several clinical features, such as progression and survival time [18, 19]. However, although recently investigated in the light of the potential interactions revealed between intraneuronal protein aggregation and reactive neuroinflammation with consequent excitotoxicity and neuronal death [20], the molecular mechanisms underlying the triggering of the neurodegenerative process in the aging brain have not been completely elucidated.
Our finding of an higher risk of comorbid dementia in occurrence of bulbar onset is consistent with other investigations [4, 21], although not all studies are in agreement on this point [2, 3, 8]. Probably, these conflicting results may be due to the heterogeneous cohorts of patients studied, who have not been frequently explored for pseudobulbar symptoms, commonly detected in patients with bulbar impairment and mainly related to frontal cortex dysfunctions [22, 23]. Furthermore, we found that the diagnosis of FTLD was less frequently associated with a spinal onset of ALS. Probably, the divergent neuropsychological patterns identified in the two disease onsets may resemble previous neuroimaging evidence of a more widespread cerebral microstructural [24] and functional [25] impairment, especially in frontotemporal areas, in patients with bulbar onset compared to those with spinal onset, in favour of the growing evidence of cognitive and extramotor changes in bulbar pathology, prominently associated with neuropathological abnormalities in brain regions involved in speech and language processing and characterized by atypical features, such as neurofibrillary tangles and basophilic inclusions, not reported in cases with spinal onset [26].
Our multivariate analysis revealed a significant increased risk of family history of ALS and FTLD in case of ALS-FTD, highlighting the potential role of the genetic background on influencing the risk of cognitive impairment in ALS [27]. However, our cohort was negative for the most common ALS-related gene mutations (i.e., the genetic panel shared by all ALS centers included SOD1, C9ORF72, TARDBP, FUS) in the 90% of patients (n = 955) who have been tested for genetics (n = 1059). Nevertheless, although these data could suggest that a substantial genetic contribution may be also discovered in “apparently” sporadic ALS, the lacking information on gene mutations in a portion of the collected patients and the genetic panel investigated, that did not include in each center all gene mutations associated to ALS-FTD (i.e., VCP, SQTSM1, UBQLN2, TUBA4A, MATR3, OPTN and TBK1 [28]), may explain the apparently negativity for genetic mutations.
We also revealed that the median survival time was shorter in case of patients with comorbid dementia in comparison to the non-demented ones. Moreover, stratifying the patients for disease phenotype and onset, the median survival time was shorter in demented versus non-demented patients with classic, bulbar and flail limb phenotypes and with bulbar and spinal onsets. These results confirmed previous data on the shortest survival time in case of ALS-FTD [4,5,6,7], although we did not verify this association in all the studied phenotypes. In particular, we did not observe a significantly different survival time in the demented versus non-demented patients in case of respiratory onset/phenotype and UMN-p phenotype, respectively, characterized by the most and less aggressive clinical course of ALS [12]. Our findings on survival in case of respiratory onset/phenotype are only apparently in disagreement with previous evidence regarding the effects on survival of the association between respiratory and frontotemporal dysfunctions [7, 17, 29]. In particular, it was revealed that ALS patients with a frontotemporal syndrome had a shorter survival after NIV initiation compared to classic ALS patients and this was attributed to the impact of neurobehavioral disfunctions (i.e., mainly apathy, disinhibition or dysexecutive behaviour) on compliance to NIV [7, 17, 29]. Probably, in our cohort of patients the lacking evidence of different survival time in demented versus non-demented patients with respiratory onset/phenotype may be due to the absence of a more disease-specific analysis of behavioural dysfunctions, proven to consistently impact adherence to therapies and the decision-making process [29, 30]. On the other hand, the similarity of survival data in demented versus non-demented ALS patients also in case of UMN-p phenotype may be mainly due to the fact that in this subset of ALS patients the prognosis has been proven to be related to the appearance and degree of lower motor neuron dysfunctions, that may cause a gradual assimilation of this clinical phenotype to classic ALS, as also described in primary lateral sclerosis [12, 31]. Interestingly, with regard to the lower motor neuron predominant phenotypes (i.e., flail limb patients), although we observed that the flail leg phenotype was associated with a lower risk of ALS-FTD, it was revealed that, when FTLD co-occurred, the median survival time of the flail limb patients resulted significantly reduced. These findings suggest that, although patients with this phenotype may have a longer median survival time, in agreement with previous literature [32,33,34], the potential comorbidity with dementia, revealed in our dataset only in a few patients (n = 8) and rarely described in this variant of ALS [12], may significantly impact the prognosis.
The major strength of this study is the great number of patients involved. However, our study has also some major limitations, principally related to the multi-centric (and not population-based) design and the retrospective nature of the study, that may have caused sample selection bias because of our cases ascertainment, which includes patients coming from tertiary centers. In this regard, a recent comparison between two ALS populations, respectively, derived from an Italian ALS registry and from the same 13 referral centers involved in this study, revealed that a multi-centric analysis may cause a selection of patients with milder phenotypes and less disability, thus characterized by a better prognosis in comparison to those observed in the ALS population [10]. Furthermore, not all cases have been genotyped and there was a lack of homogeneous and extensive genetic screening across the 13 ALS centers, that did not investigate all genetic mutations associated to ALS-FTD, leaving the possibility that some cases may be related to known or unknown genetic mutations. Patients with “possible ALS”, according to the Revised El Escorial criteria, were not included, thus potentially excluding patients in early stages of disease. With regard to the differential diagnosis between Alzheimer’s disease and FTLD, (11)C-PIB PET and CSF data were not available. Finally, we did not evaluate the correlations potentially existing between the clinical and prognostic factors studied and the scores derived from the examination of each cognitive and behavioural domain because of some inhomogeneity in the neuropsychological tools used by the different ALS centers, given the retrospective design of our analysis. In particular, at the time of data collection, neuropsychological tools specifically designed for screening ALS populations in clinical and research settings, such as ALS cognitive behavioural screen (ALS-CBS) [35], which assesses mainly the executive domain, and Edinburgh cognitive and behavioural ALS screen (ECAS) [36], designed to assess heterogeneous cognitive involvement, were not still available. However, the battery administered included evaluation of (semantic and phonemic) verbal fluency with the estimation of fluency indices [37], that, together with Stroop executive factor [3] and trail making test B-A [38], allow to control for either limb or speech motor disability, thus decreasing the potential effects of the physical aspects of the disease on cognitive performances. Moreover, with regard to the evaluation of behavioural disturbances, we used tests (i.e., Frontal Behavioural Inventory, Frontal Systems Behaviour scale and UCLA Neuropsychiatric Inventory; see Supplemental Materials S1) that comprised components unable to accommodate for physical disability, thus exaggerating behavioural change, instead of other more recently validated disease-specific instruments [39, 40]. Finally, we did not include information on mood assessment because not available in most patients.
In conclusion, our findings on a large cohort of newly diagnosed ALS patients corroborated the evidence that information on cognitive impairment could further supplement the clinical characterization of ALS patients from the early stages, integrating the current phenotypic evaluation and, thereby, leading to potential improvements both in real life and in clinical trials.
References
Turner MR, Swash M (2015) The expanding syndrome of amyotrophic lateral sclerosis: a clinical and molecular odyssey. J Neurol Neurosurg Psychiatry 86:667–673
Ringholz GM, Appel SH, Bradshaw M, Cooke NA, Mosnik DM, Schulz PE (2005) Prevalence and patterns of cognitive impairment in sporadic ALS. Neurology 65:586–590
Phukan J, Elamin M, Bede P et al (2012) The syndrome of cognitive impairment in amyotrophic lateral sclerosis: a population-based study. J Neurol Neurosurg Psychiatry 83:102–108
Montuschi A, Iazzolino B, Calvo A et al (2015) Cognitive correlates in amyotrophic lateral sclerosis: a population-based study in Italy. J Neurol Neurosurg Psychiatry 86:168–173
Gordon PH, Delgadillo D, Piquard A et al (2011) The range and clinical impact of cognitive impairment in French patients with ALS: a cross-sectional study of neuropsychological test performance. Amyotroph Lateral Scler 12:372–378
Rusina R, Ridzon P, Kulist’ák P et al (2010) Relationship between ALS and the degree of cognitive impairment, markers of neurodegeneration and predictors for poor outcome: a prospective study. Eur J Neurol 17:23–30
Olney RK, Murphy J, Forshew D et al (2005) The effects of executive and behavioral dysfunction on the course of ALS. Neurology 65:1774–1777
Elamin M, Phukan J, Bede P et al (2011) Executive dysfunction is a negative prognostic indicator in patients with ALS without dementia. Neurology 76:1263–1269
Murphy J, Factor-Litvak P, Goetz R et al (2016) Cognitive-behavioral screening reveals prevalent impairment in a large multicenter ALS cohort. Neurology 86:813–820
Calvo A, Moglia C, Lunetta C et al (2017) Factors predicting survival in ALS: a multicenter Italian study. J Neurol 264:54–63
Brooks BR, Miller RG, Swash M et al (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1:293–299
Chiò A, Calvo A, Moglia C et al (2011) Phenotypic heterogeneity of amyotrophic lateral sclerosis: a population based study. J Neurol Neurosurg Psychiatry 82:740–746
Dubois B, Feldman HH, Jacova C et al (2010) Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol 9:1118–1127
Strong MJ, Abrahams S, Goldstein LH et al (2017) Amyotrophic lateral sclerosis—frontotemporal spectrum disorder (ALS-FTSD): revised diagnostic criteria. Amyotroph Lateral Scler Frontotemporal Degener 18:153–174
Strong MJ, Grace GM, Freedman M et al (2009) Consensus criteria for the diagnosis of frontotemporal cognitive and behavioural syndromes in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 10:131–146
Rascovsky K, Hodges JR, Knopman D et al (2011) Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134:2456–2477
Govaarts R, Beeldman E, Kampelmacher MJ et al (2016) The frontotemporal syndrome of ALS is associated with poor survival. J Neurol 263:2476–2483
Chiò A, Logroscino G, Hardiman O et al (2009) Prognostic factors in ALS: a critical review. Amyotroph Lateral Scler 10:310–323
Yokoi D, Atsuta N, Watanabe H et al (2016) Age of onset differentially influences the progression of regional dysfunction in sporadic amyotrophic lateral sclerosis. J Neurol 263:1129–1136
Currais A, Fischer W, Maher P, Schubert D (2017) Intraneuronal protein aggregation as a trigger for inflammation and neurodegeneration in the aging brain. FASEB J 31:5–10
Schreiber H, Gaigalat T, Wiedemuth-Catrinescu U et al (2005) Cognitive function in bulbar- and spinal-onset amyotrophic lateral sclerosis. A longitudinal study in 52 patients. J Neurol 252:772–781
Hübers A, Kassubek J, Grön G et al (2016) Pathological laughing and crying in amyotrophic lateral sclerosis is related to frontal cortex function. J Neurol 263:1788–1795
Abrahams S, Goldstein LH, Al-Chalabi A et al (1997) Relation between cognitive dysfunction and pseudobulbar palsy in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 62:464–472
Cardenas-Blanco A, Machts J, Acosta-Cabronero J et al (2014) Central white matter degeneration in bulbar- and limb-onset amyotrophic lateral sclerosis. J Neurol 261:1961–1967
Cistaro A, Valentini MC, Chiò A et al (2012) Brain hypermetabolism in amyotrophic lateral sclerosis: a FDG PET study in ALS of spinal and bulbar onset. Eur J Nucl Med Mol Imaging 39:251–259
Shellikeri S, Karthikeyan V, Martino R et al (2017) The neuropathological signature of bulbar-onset ALS: a systematic review. Neurosci Biobehav Rev 75:378–392
Chiò A, Brunetti M, Barberis M et al (2016) The role of APOE in the occurrence of frontotemporal dementia in amyotrophic lateral sclerosis. JAMA Neurol 73:425–430
Sabatelli M, Marangi G, Conte A et al (2016) New ALS-related genes expand the spectrum paradigm of amyotrophic lateral sclerosis. Brain Pathol 26:266–275
Chiò A, Ilardi A, Cammarosano S et al (2012) Neurobehavioral dysfunction in ALS has a negative effect on outcome and use of PEG and NIV. Neurology 78:1085–1089
Raaphorst J, Tuijp J, Verweij L et al (2013) Treatment of respiratory impairment in patients with motor neuron disease in the Netherlands: patient preference and timing of referral. Eur J Neurol 20:1524–1530
Le Forestier N, Maisonobe T, Piquard A et al (2001) Does primary lateral sclerosis exist? A study of 20 patients and a review of the literature. Brain 124:1989–1999
Wijesekera LC, Mathers S, Talman P et al (2009) Natural history and clinical features of the flail arm and flail leg ALS variants. Neurology 72:1087–1094
Hübers A, Hildebrandt V, Petri S et al (2016) Clinical features and differential diagnosis of flail arm syndrome. J Neurol 263:390–395
Dimachkie MM, Muzyka IM, Katz JS et al (2013) Leg amyotrophic diplegia: prevalence and pattern of weakness at US neuromuscular centers. J Clin Neuromuscul Dis 15:7–12
Woolley SC, York MK, Moore DH et al (2010) Detecting frontotemporal dysfunction in ALS: utility of the ALS cognitive behavioral screen (ALSCBS). Amyotroph Lateral Scler 11:303–311
Abrahams S, Newton J, Niven E et al (2014) Screening for cognition and behaviour changes in ALS. Amyotroph Lateral Scler Frontotemporal Degener 15:9–14
Abrahams S, Leigh PN, Harvey A et al (2000) Verbal fluency and executive dysfunction in amyotrophic lateral sclerosis (ALS). Neuropsychologia 38:734–747
Zalonis I, Christidi F, Paraskevas G et al (2012) Can executive cognitive measures differentiate between patients with spinal- and bulbar-onset amyotrophic lateral sclerosis? Arch Clin Neuropsychol 27:348–354
Raaphorst J, Beeldman E, Schmand B et al (2012) The ALS-FTD-Q: a new screening tool for behavioral disturbances in ALS. Neurology 79:1377–1383
Mioshi E, Hsieh S, Caga J et al (2014) A novel tool to detect behavioural symptoms in ALS. Amyotroph Lateral Scler Frontotemporal Degener 15:298–304
Acknowledgments
The authors thank all the collaborators of the ALS referral centers involved in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. Outside this work, Dr. F. Trojsi perceived fees from Italfarmaco and Aisla and a grant from Novartis; Prof. A. Chiò fees from Biogen and Mitsubishi; Prof. M.R. Monsurrò a grant from Italfarmaco; Prof. G. Tedeschi grants from Purytra, Abbvie, Genzyme and Ministry of Health (RF-2011-02351193).
Ethical standards
The study was performed in accordance with the ethical standards statement.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trojsi, F., Siciliano, M., Femiano, C. et al. Comorbidity of dementia with amyotrophic lateral sclerosis (ALS): insights from a large multicenter Italian cohort. J Neurol 264, 2224–2231 (2017). https://doi.org/10.1007/s00415-017-8619-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8619-4