Abstract
The aim of this pilot study was to compare clinical aspects of tremor-dominant Parkinson’s disease (PD) patients with and without preceding essential tremor to identify characteristics of these two subgroups. Nineteen patients with diagnoses of both essential tremor (ET) and Parkinson’s disease in comparison to 18 patients with tremor-dominant Parkinson’s disease without preceding tremor were investigated. The profile of several motor and non-motor symptoms, including cognitive dysfunction, depression, sleep alterations, olfaction changes and some autonomic symptoms, as well as imaging aspects obtained by transcranial sonography were compared between groups. Parkinson’s patients with essential tremor scored higher in kinetic and postural tremor items (p < 0.05) and displayed an enlarged third ventricle on transcranial sonography (p = 0.010), which was not found in tremor-dominant Parkinson’s disease patients. All other motor and non-motor symptoms could not distinguish between either study group. Neither group showed a distinct clinical profile related to non-motor symptoms or symptoms other than tremor-specific motor aspects. The fact that non-motor symptoms were similar in ET-PD gives rise to the hypothesis that also the prodromal phase of PD is similar in ET patients later developing classical PD compared to individuals developing PD without preceding ET. This hypothesis needs to be followed in prospective studies to verify whether the establishment of an ET subgroup with prodromal markers for PD is feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
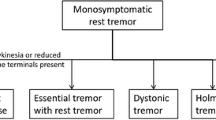
Parkinson’s disease (PD), characterized by well-described motor impairment [1], is the second most frequent neurodegenerative disorder affecting about 1–2 % of individuals older than 65 years of age [2]. Essential tremor (ET) with the classical motor features of action-triggered and postural tremor [3] is also a common neurological disorder with an overall prevalence of 0.9 %, which amounts to 4.6 % in individuals over 65 years of age, according to a meta-analysis [4].
Some neuropathological findings describe an increased loss of Purkinje cells and cerebellar gliosis in ET patients as a sign for a neurodegenerative disorder [5]; however, this finding is discussed widely and other groups did not find any differences between ET cases and healthy controls with regards to Purkinje cell loss [6]. Interestingly, in different studies, individuals with ET have been observed to have a four- to fivefold increased risk of developing PD during their lifetime (ET-PD) compared to healthy persons [5, 7]. Clinical studies could demonstrate non-motor symptoms known to be related to PD in some individuals with ET [8]. Moreover, in a small subgroup of ET cases, Lewy bodies have been detected [9] which are the neuropathological hallmark for Parkinson’s disease and dementia with Lewy bodies [10]. Additionally, imaging data verify abnormalities of the presynaptic dopamine status also in a subgroup of individuals with ET with the classical presentation of isolated action or postural tremor [11]. All these data indicate that there seems to be an ET-subgroup which shows Parkinson's-like non-motor, neuropathology and imaging characteristics. It is tempting to speculate that these particular ET patients may be quite likely to develop PD, whereas the majority of ET patients, who share neither the common non-motor symptoms nor the pathology or imaging findings with PD, will stay PD-free during their lifetime. It is well known that Parkinson’s disease is a very heterogenous entity of different clinical phenotypes and molecular pathways leading to disease manifestation. There are different monogenetic causes, e.g. mutations in the α-synuclein (SNCA), dardarin (LRKK2), parkin (PARK2) and other genes, and genetic risk factors like mutations in the glucocerebrosidase (GBA) gene [12]. Moreover, with different weightings, genetic risk factors [13], inflammation [14], mitochondrial dysfunction [15] and other factors seem also to play a role in sporadic PD. Thus, it may be hypothesized that ET-PD represents a specific PD-subgroup which may be clinically distinguished from “normal” PD even by other than the ET-specific motor features.
Subjects and methods
Subjects
Eighteen individuals with tremor-dominant PD (tPD) and 19 individuals with ET-PD were investigated. Patients diagnosed with ET-PD were consecutively recruited between April 2010 and May 2011 from the outpatients’ clinic of the Department of Neurodegeneration of the University of Tübingen. Patients with tPD were selected to be as similar as possible to match the ET-PD group with regard to age, sex and duration of PD (see Table 1 for details). From onset until examination in this study, all tPD patients showed a tremor-dominant Parkinson's phenotype. The diagnosis of PD was done according to the United Kingdom Brain Bank criteria [1], which require the cardinal asymmetric signs: slowness of movements, rest tremor and/or rigidity, a progressive disease course, the absence of hints for an atypical parkinsonian syndrome, and response to levodopa therapy. The diagnosis of ET was made after the Tremor Investigation Group (TRIG) classification [3] which requires bilateral rather symmetric postural or kinetic tremor, involving hands and forearms and that this is visible and persistent. Moreover, criteria for inclusion included duration of such a tremor longer than 5 years as well as the lack of parkinsonian signs such as rest tremor and/or rigidity at ET-onset. The diagnosis of all PD cases was made by an experienced movement disorder specialist according to the consensus guidelines. All patients with ET-PD had postural or kinetic tremor of hands for at least 7 years before the onset of further PD characteristic motor signs.
The study was approved by the local ethical committee (197/2010801). All participants gave written informed consent.
Assessment of motor symptoms
The neurological examination was performed by a movement disorders specialist including the Movement Disorder Society (MDS)-sponsored new version of the Unified Parkinson’s Disease Rating Scale (UPDRS) parts III and IV [16], the Fahn–Tolosa–Marin Clinical Rating Scale for tremors (FTMRS) [17], as well as a segmental motor testing [18]. Moreover, part II (motor experiences of daily living) of the UPDRS was assessed.
Assessment of non-motor symptoms
To account for non-motor symptoms, part I (non-motor experiences of daily living) of the MDS-UPDRS, including questions about constipation, urinary dysfunction and orthostatic dysregulation, was assessed [16]. Olfactory function was evaluated with the 12-item Sniffin’ sticks test (Burghardt Medizintechnik, Germany) [19]. To cover for signs of depression, participants were asked to fill out the revised form of the Beck Depression Inventory (BDI-II) [20]. Night sleep disturbances were assessed by the Parkinson’s Disease Sleep Scale (PDSS) [21] and REM sleep disturbances by the REM Sleep Behavior Disorder Screening Questionnaire (RBD) [22]. All participants were given the Mini Mental Status Examination (MMSE) [23] and the Montreal Cognitive Assessment (MoCA) [24] to screen for cognitive decline.
Additional assessments
Using transcranial ultrasound, the brainstem was evaluated for echogenicity of the substantia nigra (SN), as SN hyperechogenicity is a typical sign of PD. In the third ventricular plane, width of the ventricular system (third and anterior horns of the lateral ventricles) was also recorded according to a standardized protocol [25].
Statistics
Statistical analysis was performed applying SPSS 20.0 software for Windows (SPSS Inc, Chicago, IL, USA). Normal distribution of values was verified by the Kolmogorov–Smirnov test. Between-groups analysis was applied by Student t test or χ 2 test for gender. Values below an alpha level of p = 0.05 were considered to be significant.
Results
Neither group, tPD and ET-PD, statistically differed with regard to age (p = 0.757), gender (p = 0.390), PD disease duration (p = 0.878), UPDRS-III total score (p = 0.277) or Hoehn and Yahr scale (p = 0.998) (see Table 1).
Severity of postural tremor and kinetic tremor assessed by the total FTMRS score, including Archimedes spiral drawing (p = 0.002) and the segmental motor test (p = 0.016), was more pronounced in ET-PD patients (see Table 2). On transcranial sonography (TCS), the size of the third ventricle was larger in the ET-PD group (p = 0.010), but the area of SN hyperechogenicity was comparable between study groups (left SN: p = 0.756, right SN: p = 0.401).
None of the examined non-motor, neuro-behavioural or motor symptoms other than postural and kinetic tremor differed statistically significant between the group of tPD and ET-PD (see Table 2 for details).
Discussion
In our study, PD patients with and without preceding ET showed no clinical differences in their clinical phenotype concerning non-motor or motor symptoms, except for the presence and severity of postural and kinetic tremor. This latter finding is in accordance with previous studies, which have additionally shown that ET and PD patients differ in tremor-related aspects not only with regard to severity of kinetic, postural and rest tremor, but also in tremor amplitude, localisation and electromyography pattern [26].
Interestingly, in our study the size of the third ventricle on TCS was significantly enlarged in the ET-PD group (in comparison to the tPD group; see also Table 2) (age-related normal values over 60 years for the width of the third ventricle are 7.6 ± 2.1 mm [27]). Also, the side ventricles were larger in ET-PD than in tPD; however, this difference did not reach statistical significance. This unexpected finding may be due to the small sample size of our study. However, there are MRI studies showing cerebral and cerebellar atrophy in patients with ET when compared to controls [28]. Although these MRI studies do not explicitly report measurements of the ventricles, the reported atrophy may correspond to an outer and also inner atrophy of the brain. The latter may have been seen as enlargement of the ventricular system by transcranial ultrasound in our study.
Clinical studies demonstrated a higher prevalence of coincidental PD in patients with ET compared to healthy individuals. In addition, a positive family history of ET is often reported in PD [29]. This may emphasize that ET and PD either share common risk factors, or that ET predisposes to PD in a subgroup of ET patients. Importantly, only a rather small subgroup of ET patients will eventually develop PD. According to a study from 2009, the relative risk of 201 ET patients for developing PD was 3.47 with a 95 % confidence interval from 1.82 to 6.59 [7]. So far, it is not possible to predict later onset of PD in ET patients. In our study, we could show that the clinical phenotype of PD does not differ between ET-PD and tPD with regard to PD-specific motor symptoms, and several non-motor symptoms including cognitive, psychiatric, sleep related, some autonomic and olfaction aspects. Whether the prodromal stage of PD differs in ET-PD as compared to tPD needs to be investigated in prospective longitudinal studies. Importantly, typical prodromal PD features have already been identified in a subgroup of ET patients [8, 30, 31]. If longitudinal studies indeed verify that these individuals develop motor symptoms of classical PD, a new prodromal PD group could be followed. This is of great importance, as much effort is currently being put into the identification of individuals in the prodromal stage of PD to enable earlier disease-modulating therapeutic strategies. So far, primarily enriched risk cohorts are followed, including individuals with mutations bearing a high risk of later development of PD [i.e. in the LRRK2 consortium (www.michaeljfox.org/page.html?lrrk2-cohort-consortium)] or the European Project on Mendelian Forms of Parkinson’s Disease (www.mefopa.eu) or individuals with several prodromal features [the prodromal Parkinson’s progression markers initiative (P-PPMI, www.michaeljfox.org/], several RBD cohorts, Tübinger evaluation of risk factors for early detection of neurodegeneration (TREND, www.trend-studie.de). As the clinical phenotype of ET-PD resembles in the major aspects classical PD, it may be worth investigating ET individuals for prodromal features of PD to collect a cohort of individuals for studying the progression of non-motor and motor symptoms in the prodromal phase.
As a limitation of this study, the rather small sample size needs to be mentioned. However, although there is a subgroup of ET patients developing PD it is difficult to collect an adequate group of ET-PD matched to a group of tPD. Also, one may argue that the ET-PD patients may have had PD from onset on, which could explain the similar presentation with regard to non-motor signs. However, the long time between primarily postural or action tremor before manifestation of typical PD motor signs [25.89 (standard deviation 18.027)] in our study, rather symmetrical tremor presentation at that time, positive family history for ET, as well as positive response to alcohol and beta-blockers in many of the ET-PD cases strongly indicates that indeed ET tremor preceded manifestation of PD. Both groups presented in this pilot study are well characterized and we thus believe that this study may lay the groundwork for future studies on ET-PD, especially with regard to the prodromal phase of PD.
References
Daniel SE, Lees AJ (1993) Parkinson’s Disease Society Brain Bank, London: overview and research. J Neural Transm Suppl 39:165–172
Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R (2007) How common are the “common” neurologic disorders? Neurology 68(5):326–337
Deuschl G, Bain P, Brin M (1998) Consensus statement of the Movement Disorder Society on Tremor Ad Hoc Scientific Committee. Mov Disord Off J Mov Disord Soc 13(Suppl 3):2–23
Louis ED, Ferreira JJ (2010) How common is the most common adult movement disorder? Update on the worldwide prevalence of essential tremor. Mov Disord Off J Mov Disord Soc 25(5):534–541. doi:10.1002/mds.22838
Tan EK, Lee SS, Fook-Chong S, Lum SY (2008) Evidence of increased odds of essential tremor in Parkinson’s disease. Mov Disord Off J Mov Disord Soc 23(7):993–997. doi:10.1002/mds.22005
Rajput AH, Robinson CA, Rajput ML, Robinson SL, Rajput A (2012) Essential tremor is not dependent upon cerebellar Purkinje cell loss. Parkinsonism Relat Disord 18(5):626–628. doi:10.1016/j.parkreldis.2012.01.013
Benito-Leon J, Louis ED, Bermejo-Pareja F, Neurological Disorders in Central Spain Study G (2009) Risk of incident Parkinson’s disease and parkinsonism in essential tremor: a population based study. J Neurol Neurosurg Psychiatry 80(4):423–425. doi:10.1136/jnnp.2008.147223
Chandran V, Pal PK (2012) Essential tremor: beyond the motor features. Parkinsonism Relat Disord 18(5):407–413. doi:10.1016/j.parkreldis.2011.12.003
Louis ED, Faust PL, Vonsattel JP, Honig LS, Rajput A, Robinson CA, Pahwa R, Lyons KE, Ross GW, Borden S, Moskowitz CB, Lawton A, Hernandez N (2007) Neuropathological changes in essential tremor: 33 cases compared with 21 controls. Brain J Neurol 130(Pt 12):3297–3307. doi:10.1093/brain/awm266
Okazaki H, Lipkin LE, Aronson SM (1961) Diffuse intracytoplasmic ganglionic inclusions (Lewy type) associated with progressive dementia and quadriparesis in flexion. J Neuropathol Exp Neurol 20:237–244
Coria F, Gimenez-Garcia M, Samaranch L, Mora FJ, Sampol-Bas C, Pastor P (2012) Nigrostriatal dopaminergic function in subjects with isolated action tremor. Parkinsonism Relat Disord 18(1):49–53. doi:10.1016/j.parkreldis.2011.08.025
Lill CM, Roehr JT, McQueen MB, Kavvoura FK, Bagade S, Schjeide BM, Schjeide LM, Meissner E, Zauft U, Allen NC, Liu T, Schilling M, Anderson KJ, Beecham G, Berg D, Biernacka JM, Brice A, DeStefano AL, Do CB, Eriksson N, Factor SA, Farrer MJ, Foroud T, Gasser T, Hamza T, Hardy JA, Heutink P, Hill-Burns EM, Klein C, Latourelle JC, Maraganore DM, Martin ER, Martinez M, Myers RH, Nalls MA, Pankratz N, Payami H, Satake W, Scott WK, Sharma M, Singleton AB, Stefansson K, Toda T, Tung JY, Vance J, Wood NW, Zabetian CP, Me Genetic Epidemiology of Parkinson’s Disease C, International Parkinson’s Disease Genomics C, Parkinson’s Disease GC, Wellcome Trust Case Control C, Young P, Tanzi RE, Khoury MJ, Zipp F, Lehrach H, Ioannidis JP, Bertram L (2012) Comprehensive research synopsis and systematic meta-analyses in Parkinson’s disease genetics: the PDGene database. PLoS Genet 8(3):e1002548. doi:10.1371/journal.pgen.1002548
Valente EM, Arena G, Torosantucci L, Gelmetti V (2012) Molecular pathways in sporadic PD. Parkinsonism Relat Disord 18(Suppl 1):S71–S73. doi:10.1016/S1353-8020(11)70023-2
Hamza TH, Zabetian CP, Tenesa A, Laederach A, Montimurro J, Yearout D, Kay DM, Doheny KF, Paschall J, Pugh E, Kusel VI, Collura R, Roberts J, Griffith A, Samii A, Scott WK, Nutt J, Factor SA, Payami H (2010) Common genetic variation in the HLA region is associated with late-onset sporadic Parkinson’s disease. Nature Genet 42(9):781–785. doi:10.1038/ng.642
Subramaniam SR, Chesselet MF (2013) Mitochondrial dysfunction and oxidative stress in Parkinson’s disease. Progr Neurobiol 106–107:17–32. doi:10.1016/j.pneurobio.2013.04.004
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N, Movement Disorder Society URTF (2008) Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord Off J Mov Disord Soc 23(15):2129–2170. doi:10.1002/mds.22340
Nicaretta DH, Pereira JS, Pimentel ML (1997) Tremor: adaptation of a clinical scale. Arq Neuropsiquiatr 55(3A):381–386
Schupbach WM, Corvol JC, Czernecki V, Djebara MB, Golmard JL, Agid Y, Hartmann A (2010) Segmental progression of early untreated Parkinson’s disease: a novel approach to clinical rating. J Neurol Neurosurg Psychiatry 81(1):20–25. doi:10.1136/jnnp.2008.159699
Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G (1997) ‘Sniffin sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22(1):39–52
Leentjens AF, Verhey FR, Luijckx GJ, Troost J (2000) The validity of the Beck Depression Inventory as a screening and diagnostic instrument for depression in patients with Parkinson’s disease. Mov Disord Off J Mov Disord Soc 15(6):1221–1224
Chaudhuri KR, Pal S, DiMarco A, Whately-Smith C, Bridgman K, Mathew R, Pezzela FR, Forbes A, Hogl B, Trenkwalder C (2002) The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry 73(6):629–635
Stiasny-Kolster K, Mayer G, Schafer S, Moller JC, Heinzel-Gutenbrunner M, Oertel WH (2007) The REM sleep behavior disorder screening questionnaire: a new diagnostic instrument. Mov Disord Off J Mov Disord Soc 22(16):2386–2393. doi:10.1002/mds.21740
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699. doi:10.1111/j.1532-5415.2005.53221.x
Walter U, Wittstock M, Benecke R, Dressler D (2002) Substantia nigra echogenicity is normal in non-extrapyramidal cerebral disorders but increased in Parkinson’s disease. J Neural Transm 109(2):191–196
Sternberg EJ, Alcalay RN, Levy OA, Louis ED (2013) Postural and intention tremors: a detailed clinical study of essential tremor vs. Parkinson’s Disease. Frontiers Neurol 4:51. doi:10.3389/fneur.2013.00051
Seidel G, Kaps M, Gerriets T, Hutzelmann A (1995) Evaluation of the ventricular system in adults by transcranial duplex sonography. J Neuroimaging Off J Am Soc Neuroimaging 5(2):105–108
Bagepally BS, Bhatt MD, Chandran V, Saini J, Bharath RD, Vasudev MK, Prasad C, Yadav R, Pal PK (2012) Decrease in cerebral and cerebellar gray matter in essential tremor: a voxel-based morphometric analysis under 3T MRI. J Neuroimaging 22(3):275–278. doi:10.1111/j.1552-6569.2011.00598.x
Rocca WA, Bower JH, Ahlskog JE, Elbaz A, Grossardt BR, McDonnell SK, Schaid DJ, Maraganore DM (2007) Increased risk of essential tremor in first-degree relatives of patients with Parkinson’s disease. Mov Disord Off J Mov Disord Soc 22(11):1607–1614. doi:10.1002/mds.21584
Gerbin M, Viner AS, Louis ED (2012) Sleep in essential tremor: a comparison with normal controls and Parkinson’s disease patients. Parkinsonism Relat Disord 18(3):279–284. doi:10.1016/j.parkreldis.2011.11.004
Louis ED, Jurewicz EC (2003) Olfaction in essential tremor patients with and without isolated rest tremor. Mov Disord Off J Mov Disord Soc 18(11):1387–1389. doi:10.1002/mds.10603
Acknowledgments
We thank all patients who took part in the study. There was no specific funding, resources from the University of Tübingen and Hertie-Institute for Clinical Brain Research.
Conflicts of interest
Isabel Wurster has received funding for travel from GlaxoSmithKline and received research support from dPV (German Parkinson’s disease association). Annegret Abaza and Dr. Inga Liepelt Scarfone have nothing to disclose. Dr. Kathrin Brockmann has received speaker honoraria from GlaxoSmithKline and Orion Corporation and funding for travel from GlaxoSmithKline, UCB, and the Movement Disorders Society. Prof. Daniela Berg has served on scientific advisory boards for Novartis, UCB/SCHWARZ PHARMA, Merz Pharma GmbH & Co. KGaA.; has received funding for travel or speaker honoraria from Boehringer Ingelheim, Lundbeck Inc., Janssen Pharmaceutica, GlaxoSmithKline, UCB/SCHWARZ PHARMA, and Teva Pharmaceutical Industries Ltd.; and has received research support from Teva Pharmaceutical Industries Ltd., Solvay Pharmaceuticals, Inc./Abbott, Michael J. Fox Foundation, BMBF, dPV (German Parkinson’s disease association) and Center of Integrative Neurosciences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wurster, I., Abaza, A., Brockmann, K. et al. Parkinson’s disease with and without preceding essential tremor-similar phenotypes: a pilot study. J Neurol 261, 884–888 (2014). https://doi.org/10.1007/s00415-014-7285-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7285-z