Abstract
Phobic postural vertigo (PPV) is the most common cause of chronic dizziness in middle-aged patients. Many patients report symptoms involving gait. We investigated the gait performance and its relationship to the fear of falling and attention of PPV patients in a prospective study of 24 patients with PPV and 24 healthy subjects (HS) using a pressure-sensitive mat (GAITRite®). Subjects walked at three different speeds (slow, preferred, fast), both during cognitive dual tasks (DTc) and with eyes closed (EC). Falls efficacy and balance confidence were rated by the Falls Efficacy Scale-International (FES-I) and the Activities-specific Balance Confidence Scale (ABC). PPV patients walked slower, with reduced cadence (all p < 0.01), stride length (p < 0.05), and increased double support (p < 0.01) compared to HS. These changes correlated with FES-I (R = −0.528, p < 0.001) and ABC (R = 0.481, p < 0.01). Walking deterioration under DTc did not differ between PPV patients and HS, but patients showed a reduced cognitive processing speed (p < 0.05). When walking with EC, gait speed decreased more in PPV patients compared to HS (p < 0.05). Patients with PPV show gait changes which correlate with their fear of falling and balance confidence. Absent visual feedback leads to more pronounced gait deteriorations in PPV patients than in HS, indicating a higher reliance of patients on visual information during walking. These findings support the view that the gait characteristics of PPV can be attributed to an inadequate, cautious gait control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The syndrome of phobic postural vertigo (PPV) is characterized by subjective dizziness and disturbance of balance. However, these patients have normal values in clinical balance tests [5]. It can be classified among the primary and secondary somatoform dizziness syndromes, which are also termed visual vertigo syndrome [9] or chronic subjective dizziness [40]. The visual vertigo syndrome covers symptoms that are regularly provoked during or after moving visual environmental stimuli, whereas PPV often presents symptoms which are not directly associated to such stimuli. Moreover, PPV differs from chronic subjective dizziness by the presence of phobic avoidance behavior. One-third of the PPV patients further present panic attacks associated with vertigo and dizziness.
PPV is one of the most frequent causes of chronic dizziness [4, 15, 16] and represents an important entity in the differential diagnosis of chronic dizziness disorders. It has a great impact on functioning and quality of life [4]. A negative correlation between the duration of the condition before diagnosis and the improvement of symptoms [6] indicates that an early identification of typical symptoms is essential for the successful treatment of PPV patients.
The majority of PPV patients report having balance disturbances, mainly while walking and standing, with exacerbation during perceptional stimuli (e.g., walking on a bridge, walking stairs, walking in empty rooms) and during social situations (crowds, supermarkets, concerts, restaurants). Typically, PPV follows a period of particular emotional stress or vestibular or non-vestibular illness. While the stance behavior of PPV patients has been intensively investigated [8, 9, 11, 23, 30, 37, 41], little is known about changes in gait control of these patients.
The aim of this study was to determine gait changes of patients with PPV and to evaluate whether these changes are associated with their subjective imbalance and fear of falling. Spatial and temporal gait variables, and variability markers, as well as the correlations to subjective fear of falling and balance confidence measures, were analyzed. Since gait abnormalities in patients with vertigo and dizziness depend on walking speed [7, 38], walking behavior was examined at different walking speeds. Moreover, we investigated the walking performance under cognitive dual tasks of PPV patients. By doing so, we investigated how shared attentional resources influence walking control schemes of PPV patients. The reliance on visual inputs during walking was tested by examining the gait behaviour during walking with eyes closed. A higher reliance on visual information would result in a greater decline of walking capacity in PPV patients compared to HS.
Methods
Patients
Twenty-four patients with PPV (12 females; mean age 49 ± 15 years; mean height: 1.78 ± .14 m; mean weight: 74.4 ± 5.3 kg) and 24 age-matched healthy subjects (12 females; mean age 48 ± 16 years; mean height: 1.79 ± 0.11 m; mean weight: 72.5 ± 7.0 kg) participated in the study. The diagnosis of PPV was based on the diagnostic criteria proposed by Brandt [5]. The study protocol was approved by the local ethics committee and has been performed in accordance to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their written informed consent prior to the experiments.
Patients underwent a standardized diagnostic work-up. Afferent somatosensory deficits were excluded by testing vibrotactile sensitivity, surface sensibility, and acrognosis. Vestibular testing included caloric irrigation (30/44 °C) and a head-impulse test of the horizontal vestibulo-ocular reflex [20]. All subjects were found to have normal somatosensory and vestibular functions.
Gait assessment
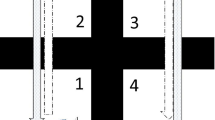
Gait analysis was performed using a 6.7-m-long pressure-sensitive carpet (GAITRite®, CIR System, Havertown, USA) with a sampling rate of 120 Hz. All patients had to walk over the carpet at three different speeds (preferred, slow, and maximally fast). Gait was then examined while walking at the preferred speed and performing a cognitive dual task (DTc) (serial 7 task) with the instruction to focus on the cognitive task. Afterwards walking at the preferred speed with eyes closed (EC) was examined. The different gait tasks were performed in a fixed order: walking with preferred speed, walking with slow speed, walking with fast speed, walking with a cognitive dual task, and walking with eyes closed. Each walk was started 1.5 m in front of the mat and continued for 1.5 m beyond it in order to allow steady-state locomotion. Each task was tested twice. During the serial 7 dual task, the calculation steps and the time from the beginning to the end of the condition were documented. The Functional Gait Assessment (FGA), a 10-item gait test developed for patients with balance deficits and vestibular disorders [43], was used to clinically assess the gait capacity and the Berg Balance Scale (BBS) to assess balance [2].
Falls efficacy and balance confidence assessment
All patients completed the Falls Efficacy Scale-International (FES-I) and the Activity-specific Balance Confidence Scale (ABC) as described elsewhere [19, 36]. The FES-I comprises 16 questions on the subjective fall efficacy in daily life situations. A total score is obtained by adding the scores (1–4) of each question. That will give a range from 16 (no concerns about falling) to 64 (severe concerns about falling) points. The ABC is a self-reported questionnaire of 16 questions evaluating the subject’s level of self-confidence in daily mobility situations.
Data analysis
The following standard gait parameters were analyzed: Functional Ambulation Profile (FAP) as described elsewhere [32], velocity, cadence, stride time, stride length, base of support, double support percentage, and the coefficient of variation (CV) of stride time, stride length, and base of support as markers for the magnitude of gait variability. These gait parameters comprehensively represent the pace, rhythm, gait cycle, support, and the dynamic stability domains of gait behavior (for overview see [31]). Matlab® and SPSS® were used for data analysis. A Matlab routine was written to calculate the CV values by using the formula:
To quantify the subjects’ ability to walk while performing a cognitive dual task (DTc) or with eyes closed (EC) compared to walking at preferred speed with eyes open (EO), a variation rate (VR) on analogy to the Romberg quotient [17] was calculated with the formula:
Cognitive processing speeds (CPS) while walking with DTc were calculated for each subject. The mean of calculation steps (correct and false calculation steps) per second of walking under DTc was analyzed using the formula:
For each subject, the ratio of false and correct calculation steps was determined by using the formula:
Analysis of Variance (ANOVA) was used with the factors (1) “group”: PPV, HS and (2) “condition”: slow, preferred, maximally fast, cognitive dual task, eyes closed. ANOVA models were corrected for multiple comparisons (Scheffé), and the covariates age, gender, height, leg length were included into the model. As the Wilcoxon and Mann–Whitney-U test revealed no significant side asymmetries for the different gait parameters and the different conditions, data of both limbs were pooled together in order to increase the number of steps and improve the quality of the CV values. Correlations were calculated using Pearson’s and Kendall-Tau procedures. The results were considered significant if p < 0.05.
Results
Characteristics of the enrolled subjects
Basic demographics and patient characteristics are summarized in Table 1. The PPV cohort had a mean age of 49 ± 15 years and a mean duration of symptoms of 47 months (range 2; 180). Six patients showed a secondary form of PPV, i.e., an episode with vertigo or dizziness preceded the PPV symptoms (Table 1). Seventeen of the 18 patients with a primary PPV course reported that an unspecific situation of stress or a non-vestibular disease preceded the symptoms.
Anxiety during balance situations was reported or admitted on direct questioning by 22 patients, whereas vegetative symptoms such as palpitations, sweating, dyspnea, or diarrhea were present in 18 patients. Only three had a history of coexisting panic disorder and/or agoraphobia, and two patients had a confirmed history of depression or generalized anxiety disorder. Eighteen patients reported observing an avoidance behavior in triggering situations, i.e., open spaces, enclosed places like elevators, crowds, and bridges. None of the patients admitted regularly using benzodiazepines, antidepressants or other neuromodulators. Six patients had a history of receiving physiotherapeutic interventions, but none of the participants had received continued balance training which could affect the gait measurement. The FGA revealed mild to moderate gait impairments with a median of 24 points [11, 30] for the PPV cohort. FES-I with a median score of 26 (16; 58) and the ABC with a mean of 73.4 (20; 100) showed a wide range covering normal to severe fear of falling and balance uncertainty.
These measures did not correlate with the duration of symptoms. Twenty-two patients had no history of falls in the previous 6 months (two patients had fallen once).
Gait characteristics of PPV patients
Two-way ANOVA testing revealed a significant reduction of walking speeds in PPV patients under the conditions of walking at slow speed (p < 0.001) and walking at preferred speed (p < 0.01) (Fig. 1). Under these conditions, the cadence and stride length of PPV patients were reduced (p < 0.05), and double support phases (p < 0.01) and stride time (p < 0.05) were increased consequently. We found no significant changes of the base of support and of temporal and spatial gait variability markers between HS and PPV patients. Walking at maximally fast speed did not reveal a significant difference in walking speed between both groups. A slight but significant reduction of cadence (p < 0.05) of PPV patients was found (details in Table 2).
Gait velocity in PPV patients and HS in three different speed sections. Asterisks represent results of a two-way ANOVA with the factors group (HS, PPV) and gait condition (slow walking, preferred walking, maximally fast walking); ** p < 0.01; *** p < 0.001. PPV phobic postural vertigo, HS healthy subjects
None of these gait parameters showed a significant correlation with the duration of the symptoms. Pearson’s correlation found a significant negative correlation between the score on the ABC and walking speed of PPV patients (R = 0.481, p < 0.01). Kendall-Tau correlations were significant for the score on the FES-I and the walking speed of PPV patients (R = −0.528, p < 0.001) (Fig. 2).
Relationship between the subjective fear of falling and preferred walking speed of the PPV patients. Kendall-Tau correlation for the the FES-I scores and preferred walking speeds of the patients. Each dot represents the mean preferred walking velocity of a PPV patient. The dotted line represents the linear fit function. R = −0.526, p < 0.001. PPV phobic postural vertigo, FES-I Falls Efficacy Scale-International
Walking characteristics during cognitive dual task or with eyes closed
The addition of a DTc (subtracting 7) while walking caused changes of gait parameters in both PPV patients and HS: a slight reduction of walking speed, cadence, and stride length with an increase of gait cycle parameters (stride time, double support percentage) and gait variability parameters (details in Table 3) could be detected. Calculation of individual VR for gait changes under DTc revealed no significant differences between HS and PPV patients (Fig. 3). However, HS performed 0.9 ± 0.3 calculation steps per second compared to 0.5 ± 0.2 calculation steps per second in PPV patients (p < 0.05). The mean number of errors was not significantly different between HS and PPV patients (HS 0.2 ± 0.2; PPV 0.3 ± 0.1).
There was a weak negative correlation between the FES-I score and the VR for velocity under DTc in PPV patients (R = −0.297, p < 0.05).
Walking with eyes closed also revealed parallel changes in the walking patterns of HS and PPV patients: walking speed was reduced with a decrease of cadence and stride length (Table 3) and an increase of gait cycle parameters (stride time) and gait variability. Calculation of the VR revealed that the reduction of walking speed, cadence, and stride length was more pronounced in PPV patients (e.g., VR for velocity: PPV 24 %; HS 9 %, all p < 0.05) compared to HS.
No significant correlations were found for FES-I, ABC, and the VR for different gait parameters under walking with eyes closed.
Discussion
Our main findings are as follows:
-
1.
The gait of PPV patients is characterized by a reduction of walking speed which correlates with the fear of falling.
-
2.
Dual task experiments reveal a higher attentional demand for the gait task in PPV patients.
-
3.
PPV patients rely more on visual feedback while walking.
Gait characteristics of PPV patients
The gait of PPV patients was characterized by changes in pace, rhythm, and gait cycle variables. The most prominent change in the walking pattern of PPV patients was a reduction of walking speed during slow and preferred walking, during walking with DTc, and during walking with EC. The decrease in cadence and stride length and the increase in double support phases can be attributed to the overall reduction of walking speed. How can this reduction of walking speed be best explained? Studies on patients with mixed vestibular entities demonstrated a reduction of walking speed, which was considered a compensatory strategy of these patients in order to increase dynamic equilibrium [34, 35]. However, studies with homogenous patient cohorts found preserved walking speeds in patients with reduced afferent sensory inputs [3, 10, 38]. In general, gait impairments due to impaired sensory function are most evident during slow walking [7, 26, 27, 38, 45, 46]. FMRI studies of locomotor imagery revealed a decrease of vestibular and somatosensory cortex activations during running compared to walking [24, 25, 28]. Based on the mentioned studies, it has been supposed that slow walking modes exhibit a higher dependence on sensory feedback than fast walking modes do. Fast walking or running are governed by a highly automated control of central pattern generators (CPG) according to the models of a hierarchical locomotion network [12]. Afferent somatosensory information has the strongest influence on the CPG operation during fast walking or running, when proprioceptive and cutaneous pressure information are most pronounced [13]. In this respect, the observed reduction of walking speed (during preferred and slow walking) in patients with PPV suggests a modification of their walking control. It implies a shift of gait control towards a more active, visual–vestibular-based control scheme. This is in accordance with recent posturographic studies on stance control schemes demonstrating that patients with PPV apply more actively controlled and sensory weighted feedback loops under normal standing conditions [39, 44]. A shift away from this control scheme might occur during maximally fast walking, which is associated with a highly automated gait pattern mostly independent from visual and vestibular control. Therefore, future PPV intervention studies should investigate whether a therapeutically induced acceleration of gait might be beneficial for PPV patients.
An alternative explanation for the reduction of walking speed in PPV patients can be extracted from the concept of “cautious gait”, an established term in the field of geriatric gait research [18, 22]. “Cautious gait” is typically marked by mild to moderate slowing, reduced stride length, and mild widening of the base of support [33]. Anxiety-related factors and the fear of falling are major contributors to a cautious gait. Some authors also state that a reduction of the walking speed increases the possibility for conscious gait control [1]. Correlation analysis in our PPV cohort supports this theory; PPV patients showed significant correlations between gait speed reduction and the subjective fear of falling (FES-I) and the scores for balance confidence (ABC).
In contrast to patients with vestibular deficits (e.g. bilateral vestibular loss) [38] or patients with cerebellar disorders [45], we found normal values of temporal and spatial gait variability parameters in PPV patients. Gait variability which represents the stride-to-stride fluctuations of the walking behaviour is a useful marker of dynamic stability during gait [21]. The distinct characteristics of gait variability in PPV patients on one side and somatic dizziness entities on the other side might be used in the differential diagnosis of patients with chronic dizziness during stance and gait. Gait variability measurements might be helpful in geriatric balance centers where gait analysis is more widely used than neuro-otological testing procedures (e.g. caloric testing of vestibular function).
PPV gait under dual task paradigms
A current concept of postural control is that it shares attentional resources with cognition [29]. Dual task paradigms, employing walking and cognitive tasks simultaneously, have been used to shed light on motor and cognitive interference with gait [42]. Whereas the decrement of gait quality in our study was similar for the HS and PPV groups (indicated by comparable VR in both groups), we found significant differences in the performance of the second, non-postural task; PPV patients showed a reduced cognitive processing speed under DTc, which denotes a disturbed dual task capacity in these patients. Changes of the non-postural task in DTc paradigms can be considered to indirectly reflect the attentional demands of posture, [14] which would then support the hypothesis that PPV patients pay more attention to gait control than do HS. On the other hand, one could argue that the obsessive–compulsive personality of a PPV patient per se could have influenced the performance of a cognitive task and that the reduced processing speed is not specific for dual task situations. This is unlikely, as the clinical contact with PPV patients does not support the idea of a general reduced cognitive processing speed. However, it cannot be ruled out completely, since the current study lacks a control condition with a cognitive single task. To elucate this aspect, future studies should include comprehensive single and dual task conditions in order to further investigate attentional demands of gait control in PPV patients.
Decrements of cognitive rather than postural tasks yield information on the prioritization of tasks in DTc situations. Although the PPV patients were instructed to give priority to the cognitive task, the patients rather focused on good postural control instead of a good performance of the cognitive task. Thus, the main focus of PPV patients lies on the maintenance of postural stability, which might explain why they do not actually fall despite their high scores for fear of falling.
Walking with eyes closed revealed a more pronounced reduction of walking speed and higher individual VR in PPV patients compared to HS. This indicates that PPV patients rely more on visual inputs during walking than do HS, a fact that agrees with the concept of visual vertigo [9]. This phenomenon was independent from the duration of symptoms and did not show any correlations to the subjective fear of falling. The weighting of sensory inputs of PPV patients seems to be shifted toward the visual system. The sensory shift towards the visual system also explains the common observation that PPV patients experience exacerbation of their complaints in situations requiring complex visual information processing (moving visual scenes, supermarkets, open spaces).
Conclusion
PPV patients show characteristic gait alterations: a reduced gait speed and consequent impairments of the pace, rhythm and gait cycle variables. These changes correlate with the patients’ subjective fear of falling. Moreover, dual-task and eyes closed walking paradigms suggest that walking in PPV patients is characterized by an increased attentional control and a higher reliance on visual input.
References
Aizen E (2001) Cautious gait and fear of falling in the elderly. Harefuah 140(1091–1094):1115
Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL (1992) Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil 73:1073–1080
Bessot N, Denise P, Toupet M, Van Nechel C, Chavoix C (2012) Interference between walking and a cognitive task is increased in patients with bilateral vestibular loss. Gait posture 36:319–321
Best C, Eckhardt-Henn A, Diener G, Bense S, Breuer P, Dieterich M (2006) Interaction of somatoform and vestibular disorders. J Neurol Neurosurg Psychiatry 77:658–664
Brandt T (1996) Phobic postural vertigo. Neurology 46:1515–1519
Brandt T, Huppert D, Dieterich M (1994) Phobic postural vertigo: a first follow-up. J Neurol 241:191–195
Brandt T, Strupp M, Benson J (1999) You are better off running than walking with acute vestibulopathy. Lancet 354:746
Brandt T, Strupp M, Novozhilov S, Krafczyk S (2012) Artificial neural network posturography detects the transition of vestibular neuritis to phobic postural vertigo. J Neurol 259:182–184
Bronstein AM (1995) Visual vertigo syndrome: clinical and posturography findings. J Neurol Neurosurg Psychiatry 59:472–476
Cohen HS, Mulavara AP, Peters BT, Sangi-Haghpeykar H, Bloomberg JJ (2012) Tests of walking balance for screening vestibular disorders. J Vestib Res 22:95–104
Dieterich M, Krafczyk S, Querner V, Brandt T (2001) Somatoform phobic postural vertigo and psychogenic disorders of stance and gait. Adv Neurol 87:225–233
Dimitrijevic MR, Gerasimenko Y, Pinter MM (1998) Evidence for a spinal central pattern generator in humans. Ann NY Acad Sci 860:360–376
Duysens J, Tax AA, van der Doelen B, Trippel M, Dietz V (1991) Selective activation of human soleus or gastrocnemius in reflex responses during walking and running. Exp Brain Res 87:193–204
Ebersbach G, Dimitrijevic MR, Poewe W (1995) Influence of concurrent tasks on gait: a dual-task approach. Percept Mot Skills 81:107–113
Eckhardt-Henn A, Breuer P, Thomalske C, Hoffmann SO, Hopf HC (2003) Anxiety disorders and other psychiatric subgroups in patients complaining of dizziness. J Anxiety Disord 17:369–388
Furman JM, Jacob RG (1997) Psychiatric dizziness. Neurology 48:1161–1166
Gagey PM, Weber B (2005) “Stabilométrie,” In: Masson E (ed) Posturologic: régulation et dérèglements de la station debout. Elsevier Masson, Issy-les-Moulineaux, pp 45–59
Giladi N, Herman T, Reider G II, Gurevich T, Hausdorff JM (2005) Clinical characteristics of elderly patients with a cautious gait of unknown origin. J Neurol 252:300–306
Greenberg SA (2012) Analysis of measurement tools of fear of falling for high-risk, community-dwelling older adults. Clin Nurs Res 21:113–130
Halmagyi GM, Curthoys IS (1988) A clinical sign of canal paresis. Arch Neurol 45:737–739
Hausdorff JM (2005) Gait variability: methods, modeling and meaning. J Neuroeng Rehabil 2:19
Herman T, Giladi N, Gurevich T, Hausdorff JM (2005) Gait instability and fractal dynamics of older adults with a “cautious” gait: why do certain older adults walk fearfully? Gait Posture 21:178–185
Holmberg J, Tjernstrom F, Karlberg M, Fransson PA, Magnusson M (2009) Reduced postural differences between phobic postural vertigo patients and healthy subjects during a postural threat. J Neurol 256:1258–1262
Jahn K, Deutschlander A, Stephan T, Kalla R, Hufner K, Wagner J, Strupp M, Brandt T (2008) Supraspinal locomotor control in quadrupeds and humans. Prog Brain Res 171:353–362
Jahn K, Deutschlander A, Stephan T, Strupp M, Wiesmann M, Brandt T (2004) Brain activation patterns during imagined stance and locomotion in functional magnetic resonance imaging. Neuroimage 22:1722–1731
Jahn K, Strupp M, Schneider E, Dieterich M, Brandt T (2000) Differential effects of vestibular stimulation on walking and running. NeuroReport 11:1745–1748
Jahn K, Strupp M, Schneider E, Dieterich M, Brandt T (2001) Visually induced gait deviations during different locomotion speeds. Exp Brain Res 141:370–374
Jahn K, Zwergal A (2010) Imaging supraspinal locomotor control in balance disorders. Restor Neurol Neurosci 28:105–114
Kerr B, Condon SM, McDonald LA (1985) Cognitive spatial processing and the regulation of posture. J Exp Psychol Hum Percept Perform 11:617–622
Krafczyk S, Schlamp V, Dieterich M, Haberhauer P, Brandt T (1999) Increased body sway at 3.5–8 Hz in patients with phobic postural vertigo. Neurosci Lett 259:149–152
Lord S, Galna B, Verghese J, Coleman S, Burn D, Rochester L (2013) Independent domains of gait in older adults and associated motor and nonmotor attributes: validation of a factor analysis approach. J Gerontol A Biol Sci Med Sci 68:820–827
Nelson AJ (1974) Functional ambulation profile. Phys Ther 54:1059–1065
Nutt JG, Marsden CD, Thompson PD (1993) Human walking and higher-level gait disorders, particularly in the elderly. Neurology 43:268–279
Perring S, Summers T (2007) Laboratory-free measurement of gait rhythmicity in the assessment of the degree of impairment and the effectiveness of rehabilitation in patients with vertigo resulting from vestibular hypofunction. Physiol Meas 28:697–705
Porciuncula F, Johnson CC, Glickman LB (2012) The effect of vestibular rehabilitation on adults with bilateral vestibular hypofunction: a systematic review. J Vestib Res 22:283–298
Powell LE, Myers AM (1995) The activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci 50:M28–M34
Querner V, Krafczyk S, Dieterich M, Brandt T (2002) Phobic postural vertigo. Body sway during visually induced roll vection. Exp Brain Res 143:269–275
Schniepp R, Wuehr M, Neuhaeusser M, Kamenova M, Dimitriadis K, Klopstock T, Strupp M, Brandt T, Jahn K (2012) Locomotion speed determines gait variability in cerebellar ataxia and vestibular failure. Mov Disord 27:125–131
Schniepp R, Wuehr M, Pradhan C, Novozhilov S, Krafczyk S, Brandt T, Jahn K (2013) Nonlinear variability of body sway in patients with phobic postural vertigo. Front Neurol 4:115
Staab JP, Ruckenstein MJ (2007) Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg 133:170–176
Tjernstrom F, Fransson PA, Holmberg J, Karlberg M, Magnusson M (2009) Decreased postural adaptation in patients with phobic postural vertigo––an effect of an “anxious” control of posture? Neurosci Lett 454:198–202
Woollacott M, Shumway-Cook A (2002) Attention and the control of posture and gait: a review of an emerging area of research. Gait Posture 16:1–14
Wrisley DM, Marchetti GF, Kuharsky DK, Whitney SL (2004) Reliability, internal consistency, and validity of data obtained with the functional gait assessment. Phys Ther 84:906–918
Wuehr M, Pradhan C, Novozhilov S, Krafczyk S, Brandt T, Jahn K, Schniepp R (2012) Inadequate interaction between open- and closed-loop postural control in phobic postural vertigo. J Neurol 260(5):1314–1323
Wuehr M, Schniepp R, Ilmberger J, Brandt T, Jahn K (2013) Speed-dependent temporospatial gait variability and long-range correlations in cerebellar ataxia. Gait Posture 37:214–218
Wuehr M, Schniepp R, Pradhan C, Ilmberger J, Strupp M, Brandt T, Jahn K (2013) Differential effects of absent visual feedback control on gait variability during different locomotion speeds. Exp Brain Res 224:287–294
Acknowledgments
The authors thank Judy Benson for copy-editing the manuscript. The work was supported by the German research foundation (Deutsche Forschungsgemeinschaft, DFG JA 1087/1-1), the German Hertie Foundation and the German Federal Ministry for Education and Science (BMBF, Nr. 01EO0901).
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schniepp, R., Wuehr, M., Huth, S. et al. Gait characteristics of patients with phobic postural vertigo: effects of fear of falling, attention, and visual input. J Neurol 261, 738–746 (2014). https://doi.org/10.1007/s00415-014-7259-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7259-1