Abstract
This study examined whether symptoms (motor, cognitive, vision, sleepiness, depression) of Parkinson’s disease (PD) were associated with restricted driving practices. To quantify driving practices, electronic devices were installed in the vehicles of 27 drivers with PD (78 % men; M = 71.6, SD = 6.6; Unified Parkinson’s Disease Rating Scale (UPDRS) motor score M = 30.1, SD = 8.6; disease duration M = 3.9, SD = 2.8 years) and 20 controls (80 % men; M = 70.6, SD = 7.9) for 2 weeks. Participants completed measures of sleepiness, depression, quality of life, and assessments of motor, cognitive and visual functions. The PD group had significantly slower brake response times (p < 0.05), poorer cognitive and quality of life scores (p < 0.01) and greater depression (p < 0.05) compared to controls. Slower reaction time was significantly related to reduced driving; specifically, fewer trips (r = −0.46; p < 0.05), distance (r = −0.54, p < 0.01) and duration at night (r = −0.58, p < 0.01). Better cognitive scores were associated with driving less often in difficult situations such as bad weather and rush hour (p < 0.05), as well as reduced speed on city streets, but only for the control group. While most drivers with PD rated their overall health as good or excellent, the five PD drivers who rated their health more poorly had significantly worse clinical symptoms (UPDRS motor scores, contrast sensitivity, depression, brake response time) and more restricted driving patterns. These findings show that drivers with PD who perceive their health poorly have greater symptomatology and were more likely to restrict their driving, possibly due to noticeable declines in multiple driving-related abilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Motor, sensory and cognitive deficits associated with Parkinson’s disease (PD) can impair the ability to drive safely [1–5]. Studies show that PD drivers, compared to controls, perform worse on tests of contrast sensitivity [1, 2, 6], cognition [3, 4], sleepiness and reaction time [7–10], which may lead to difficulties driving a motor vehicle [11, 12]. To compensate for declining abilities, drivers may reduce their exposure (frequency, distance and duration) and/or modify their driving patterns (when and where they drive) to avoid more challenging situations (such as driving at night, in rush hour traffic, or in bad weather).
In a survey of over 5,000 drivers with PD, 37 % reportedly restricted their driving in terms of reduced distance (km) and trip duration due to reasons such as disease progression, sleepiness at the wheel, the effort required and potential dangers [13]. Two other studies found that compared to controls, drivers with PD drove fewer km, were less likely to drive at night, in peak traffic, long distances or alone [14, 15]. However, these studies are based on self-report, which may be inaccurate due to recall and social desirability biases [16, 17].
Our group assessed naturalistic driving practices in PD drivers objectively, using in-vehicle recording devices [16, 18]. Compared to controls, the PD group drove significantly less overall (trips, km, duration) and at night (trips, km, duration), when controlling for number of days and trips driven. The PD group also drove proportionately less in bad weather, and on highways and freeways. However, they drove significantly faster (above the posted speed limit) on highways and freeways, suggesting that they may not drive more safely [18].
The primary aim of this examination was to determine whether objectively measured restrictions in driving practices were associated with disease progression and known symptoms of PD, namely, reaction time, contrast sensitivity, cognition, excessive daytime sleepiness, depression and quality of life.
Methods
Recruitment
A sample of 27 drivers with PD was recruited from the Sun Life Financial Movement Disorders Research & Rehabilitation Centre (MDRC) at Wilfrid Laurier University (in Southwest Ontario), while 20 controls (matched for age and gender) were recruited from the general community (social and recreational centres) in the same geographical region. To be eligible for the study, PD drivers were required to have a confirmed diagnosis by a neurologist. All participants were also required: to be aged 55+, have a valid license, drive a non-hybrid vehicle (as the CarChip device is not compatible with hybrid vehicles due to the alternating power source), be the primary driver of the vehicle, and drive at least three times per week. Exclusion criteria were: stroke, glaucoma, age-related macular degeneration, schizophrenia, untreated sleep apnea, use of anti-anxiety medications, as well as any neurological condition for the control group. The study was approved by the Office of Research Ethics at the University of Waterloo and the Research Ethics Board at Wilfrid Laurier University. All participants provided written informed consent prior to participation.
Clinical measures
All PD participants were assessed on the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III (Motor scale) by the director of the MDRC. UPDRS motor scores can range from 0 to 108, with higher scores indicating worse disease severity. Levodopa Dose Equivalency (LED) was also calculated for all PD participants using the standard formula [19].
Both groups completed the following measures. The Epworth Sleepiness Scale (ESS) was used to assess the likelihood of dozing off across a range of eight situations [20]. Items were scored from 0 (never doze off) to 3 (high chance of dozing); total scores can range from 0 to 24. The Geriatric Depression Scale (GDS) was used to assess depression; scores can range from 0 to 15, with higher scores indicating greater depression [21]. The eight-item Parkinson’s disease Questionnaire (PDQ-8), wording adapted for the controls, was used to assess perceived health related quality of life. Items were scored from 0 (never) to 4 (always), summed and divided by the total possible score (32) to produce a value from 0 to 100 %; higher scores indicate worse quality of life [22].
The Pelli-Robson chart was used to assess contrast sensitivity (CS); scores less than 1.25 denote impairment [23]. The Montreal Cognitive Assessment (MoCA) was used as a screening tool for cognitive impairment [24, 25]; scores range from 0 to 30, with scores of < 26 indicative of mild cognitive impairment (MCI) [26]. Additionally, reaction time (interval between stimulus onset and initiation of movement), movement time (interval between initiation and completion) and response time (summing reaction and movement times) were assessed using a brake test apparatus (gas and brake pedals). A total of 30 trials were conducted, with ten trials at intervals of 2, 5 and 10 s, respectively. PD participants were all tested during their optimal medication state.
Driving data
Naturalistic driving data were collected using the CarChip Pro® (Model 8226; Davis Instruments, Hayward, CA) and the Otto Driving Companion® (Model PM2626; Persen Technologies Inc., Winnipeg, MB). Both devices, which record date and time-stamped data on driving exposure (e.g., distance, duration, stops, and speed), were installed in each participant’s vehicle for 2 weeks. The GPS feature of the Otto device permits examination of driving patterns (routes). Detailed description of these devices is provided elsewhere [17, 18].
Protocol
Data collection consisted of four consecutive, seasonal (fall, winter, spring, summer) waves of recruitment, each containing at least five PD and control subjects with a similar age/gender mix. At the first assessment, participants provided study consent, completed a questionnaire to collect basic demographic and health information, as well as the ESS, GDS, PDQ-8. Cognition and contrast sensitivity were also assessed. The two electronic devices were then installed in each person’s vehicle and a set of trip logs were left in the vehicle. Trip logs were used to identify other drivers of the vehicle, presence of passengers and trip purposes. Participants were asked to drive as usual over the subsequent two weeks. Participants then returned to the MDRC, at which time the devices were removed and the brake reaction test was administered.
Analysis
Data from the CarChip and Otto were downloaded and cleaned (i.e., trips with 0.0 km or by drivers not in the study were removed). To determine complete trips (to and from home), segments were linked by cross-referencing CarChip data with the trip logs and/or Otto data. Driving data for one PD participant could not be obtained, as this person lost his license during the study. Details concerning the analysis of driving patterns (i.e., day vs. night, bad weather, roadways, radius or distance from home, speed, braking force) are provided elsewhere [17, 18].
The use of parametric versus non-parametric analysis was determined via visual examination (normal probability plots, histograms, stem and leaf plots) and statistical tests (Fisher skewness and kurtosis, Kolmogrov–Smirnov and Shapiro–Wilks tests). Group comparisons were either independent t tests or Mann–Whitney U, and correlations were either Pearson’s or Spearman Rank.
Results
Participants
The PD group of 27 drivers (78 % men) ranged in age from 57 to 82 years (M = 71.6, SD = 6.6), while the control group of 20 drivers (80 % men) ranged in age from 57 to 84 years (M = 70.6, SD = 7.9). In the PD group, disease duration ranged from 1 to 11 years (M = 3.9, SD = 2.8); the majority taking levodopa (85 %), followed by Azilect (7 %), Requip (4 %) and a combination of Azilect and Requip (4 %). UPDRS motor, LED and other clinical scores are presented in Table 1.
Both the PD and control groups were primarily college educated (70 % vs. 75 %), married and living with their spouse (74 % vs. 80 %); ten people (21 % of the sample, five in each group) were still working. Most of the PD group (81 %) and all of the controls rated their health as good or excellent (as opposed to fair or poor). Apart from PD, diagnosed health conditions that may influence driving reported by the PD and control groups, respectively, were: arthritis, rheumatism and/or osteoporosis (44 % vs. 35 %), sleep disorders (11 % vs. 15 %) and cataracts (7 % vs. 20 %).
Clinical battery
As shown in Table 1, the PD group had greater daytime sleepiness (ESS scores), approaching significance. Compared to controls, they had significantly worse GDS scores; however, most fell within the non-depressed category. On individual GDS items, the PD group reported more problems with memory than controls (χ 2 = 7.72, p < 0.01). The PD group also had worse quality of life (PDQ) scores than controls. On the individual items, the PD group reported more problems in five of the eight areas: getting around in public (t = 2.80, p < 0.01); dressing (t = 3.76, p < 0.01); concentration (t = 3.25, p < 0.01), communication (t = 2.63, p < 0.01) and painful muscle cramps/spasms (t = 2.80, p < 0.01).
Compared to controls, the PD group had worse cognitive (MoCA) scores, with a greater proportion of PD drivers considered to have mild cognitive impairment/dementia. Additionally, the PD group had significantly slower brake response times; slower reaction time and poorer contrast sensitivity approached significance.
Associations between clinical scores and driving indicators
As shown in Table 2, for the PD group, slower brake reaction time was significantly associated with reduced night driving: fewer trips, less distance and duration. Although not significant, MoCA scores were negatively associated with multiple indicators of night driving (number of nights driven, trips, distance and duration). On the other hand, slower movement and response times were significantly associated with a greater amount of highway driving overall and during rush hour traffic.
As shown in Table 3, for the control group, higher PDQ or worse quality of life scores were related to a greater number of trips, while ESS (sleepiness scores) were inversely related to speed of freeway driving. Contrast sensitivity was negatively associated with freeway speed and driving on highways during rush hour. Cognitive (MoCA) scores were significantly and inversely related to driving in bad weather and during rush hour in town. Reaction time, meanwhile, was negatively associated with driving during rush hour in town and driving speed on freeways. Driving speed on city streets was significantly related to better cognitive scores, movement and response times.
The sample was also asked how many days per week they engaged in at least 30 min of moderate physical activity. Although the PD group reported exercising less often compared to controls (M = 3.2, SD = 1.9 vs. M = 4.1, SD = 1.9, t = −1.71, p = 0.10), physical activity was significantly correlated with UPDRS motor scores (r = −0.39, p < 0.05) and reaction time (r = −0.52, p < 0.01); i.e., more physical activity was related to fewer motor symptoms and faster reaction time. No associations emerged between physical activity and clinical scores for the controls.
Perceived health status
The five drivers with PD who rated their health as fair (average age M = 72.2, SD = 6.2; range 64–80; four men and one women; disease duration M = 3.4, SD = 2.5; range 1–7 years) were examined further. Compared to PD drivers who rated their health as good or excellent (n = 22), these drivers with PD had significantly worse scores on the UPDRS motor section (M = 36.9, SD = 6.0 vs. M = 28.6, SD = 8.4, t = 2.08, p < 0.05), GDS (M = 3.4, SD = .90 vs. M = 1.7, SD = 1.9, z = −2.50, p < 0.05), PDQ (M = 27.5, SD = 13.5 vs. M = 13.6, SD = 15.1, z = −2.05, p < 0.05), binocular CS (M = 31.71, SD = 0.13 vs. M = 1.88, SD = 0.14, z = −2.37, p < 0.05) and brake response time (M = 0.695, SD = 0.12 vs. M = 0.585, SD = 0.09 s, t = 2.27, p < 0.05). Additionally, they drove fewer kilometres (M = 135.3, SD = 57.8 km vs. M = 201.5, SD = 107.3 km), for a shorter duration (M = 3 h: 54 min vs. M = 5 h: 15 min) and closer to home (M = 14.6, SD = 12.0 km vs. M = 19.6, SD = 26.4 km), although group differences were not statistically significant. Cognitive scores (M = 23.0, SD = 2.0 vs. M = 22.7, SD = 3.4) were not significantly different from the rest of the PD drivers.
Discussion
Overall, the PD group scored significantly poorer on the GDS, PDQ and MoCA, as well as brake response time compared to controls. They also had higher scores on the ESS (excessive daytime sleepiness), poorer contrast sensitivity and brake reaction time, approaching significance. However, none of these clinical measures was associated with overall driving exposure (trips, km, and duration).
The PD group had significantly worse response, reaction and movement times on the brake test compared to controls, consistent with prior studies [7, 9]. Slower brake reaction time was significantly associated with reduced night driving (trips, distance and duration). Difficulty reacting to stimuli may be more noticeable than other symptoms of PD (i.e., depression, contrast sensitivity), particularly at night. On the other hand, slower movement and response times were significantly associated with greater frequency of highway driving (overall and during rush hour). This is concerning, as PD drivers with slower movement and response times may be placing themselves at higher risk on highways for adverse events (i.e., crashes), particularly as we previously showed that PD drivers drove significantly faster than controls on highways and freeways [18].
In controls, a different pattern of associations emerged between clinical scores (quality of life and sleepiness) and driving variables. The only association in the unexpected direction was that poorer quality of life was related to greater trip frequency. Further examination showed that those who rated their quality of life more poorly were still working, which likely explains their higher trip frequency. Otherwise, all associations were in the expected direction. Sleepiness was inversely related to speed of freeway driving. Poorer contrast sensitivity was associated with driving slower on freeways and less often in rush hour on the highway. Those with slower reaction times drove less in traffic in town and slower on freeways. Slower movement and response times were also related to driving slower on city streets, where accidents occur more frequently (i.e., at intersections and making left turns) [27, 28].
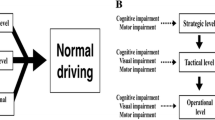
One’s ability to make strategic driving decisions (such as when and under what conditions to drive) depends on higher-order executive functions. Cognitive scores in controls were associated with driving less in risky situations (i.e., in bad weather and during rush hour), while the PD group did not show such restrictions. As the PD group overall had worse MoCA scores, not all may recognize potentially dangerous driving situations.
Although our prior study showed that PD drivers restricted their driving exposure (i.e., driving overall and at night) and patterns (i.e., bad weather, highways/freeways, rush hour) to a greater extent than controls [18], this examination showed that restrictions were not strongly associated with many of the clinical indicators or that any one symptom alone may greatly affect driving practices. Clinical symptoms in the PD group were likely not severe enough to impact driving practices, with the exception of five PD drivers. These five drivers (19 % of the sample), who had been diagnosed anywhere from 1 to 7 years ago, rated their health as fair. Compared to the rest of the sample with PD, these drivers had significantly worse UPDRS motor scores, slower reaction time, poorer contrast sensitivity and higher depression scores. Moreover, these individuals restricted their driving practices (drove fewer km and close to home) to a greater extent, possibly due to worsening symptoms and more noticeable declines in multiple driving related abilities. However, these results did not reach significance, likely due to the small sample size.
Our sample of PD drivers was recruited from a Movement Disorders Center; however, only 21 % (27 of 128) of those screened for participation enrolled in the study [29]. Many of those who were eligible chose not to participate, primarily due to fear of being reported to licensing authorities. Thus, we may have missed drivers with PD with more severe symptoms, as well as those who drive less frequently (due to the criteria of driving at least 3× per week). In general, drivers with PD who participate in research studies may be more healthy, active and confident in their abilities [12, 29]. Additionally, all participants were tested during the “on” medication state whereby PD participants may have performed better on various clinical tests. This is supported by a prior study that found that UPDRS “off” motor scores were probably predictive of driving performance where “on” scores were not [11]. Another limitation was that our sample was primarily male. Women drivers with PD, who often present with less motor dysfunction, are often under-represented in research studies [30]. Larger samples including a better gender balance are required to replicate and extend these preliminary findings. Longitudinal studies using objective measures of driving are also needed to examine how PD symptoms progress and impact on driving practices.
In conclusion, these preliminary findings suggest that at least some drivers with PD may recognize difficulties (particularly due to more severe motor problems) and restrict their driving accordingly. However, as many drivers with PD may not recognize or acknowledge their deficits, clinicians should be encouraged to refer all PD patients for periodic comprehensive driving evaluations (including both clinical and on-road assessments).
References
Devos H, Vandenberghe W, Nieuwboer A et al (2007) Predictors of fitness to drive in people with Parkinson disease. Neurology 69(14):1434–1441
Devos H, Vandenberghe W, Nieuwboer A, et al (2013) Validation of a screening battery to predict driving fitness in people with Parkinson’s disease. Mov Disord 28(5):671–674
Uc EY, Rizzo M, Anderson SW et al (2009) Driving under low-contrast visibility conditions in Parkinson’s disease. Neurology 73:1103–1110
Uc EY, Rizzo M, Anderson SW et al (2007) Impaired navigation in drivers with Parkinson’s disease. Brain 130(9):2433–2440
Classen S, Witter DP, Lanford DN et al (2011) Usefulness of screening tools for predicting driving performance in people with Parkinson’s disease. Am J Occup Ther 65(5):579–588
Uc EY, Rizzo M, Anderson SW et al (2006) Impaired visual search in drivers with Parkinson’s disease. Ann Neurol 60(4):407–413
Singh R, Pentland B, Hunter J et al (2007) Parkinson’s disease and driving ability. J Neurol Neurosurg Psychiatry 78(4):363–366
Heikkila VM, Turkka J, Korpelainen J et al (1998) Decreased driving ability in people with Parkinson’s disease. J Neurol Neurosurg Psychiatry 64(3):325–330
Madeley P, Hulley JL, Wildgust H et al (1990) Parkinson’s disease and driving ability. J Neurol Neurosurg Psychiatry 53:580–582
Worringham CJ, Wood JM, Kerr GK et al (2006) Predictors of driving assessment outcome in Parkinson’s disease. Mov Disord 21(2):230–235
Crizzle AM, Classen S, Uc E (2012) Parkinson’s disease and driving: an evidence based review. Neurology 79:2067–2074
Klimkeit EI, Bradshaw JL, Charlton J et al (2009) Driving ability in Parkinson’s disease: current status of research. Neurosci Biobehav Rev 33(3):223–231
Meindorfner C, Korner Y, Moller JC et al (2005) Driving in Parkinson’s disease: mobility, accidents, and sudden onset of sleep at the wheel. Mov Disord 20:79–84
Adler G, Rottunda S, Bauer M et al (2000) The Older driver with Parkinson’s disease. J Gerontol Soc Work 34:39–49
Wood JM, Worringham C, Kerr G et al (2005) Quantitative assessment of driving performance in Parkinson’s disease. J Neurol Neurosurg Psychiatry 76:176–180
Crizzle AM, Myers AM, Almeida QJ (2013) Self-regulatory practices of drivers with Parkinson’s disease: accuracy of patient reports. Parkinsonism Relat Disord 19:176–180
Blanchard RA, Myers AM, Porter MM (2010) Correspondence between self-reported and objective measures of driving exposure and patterns in older drivers. Accid Anal Prev 42:523–529
Crizzle AM, Myers AM (2013) Examination of naturalistic driving practices in drivers with Parkinson’s disease compared to age and gender-matched controls. Accid Anal Prev 50:724–731
Tomlinson CL, Stowe R, Patel S et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14:540–545
Weintraub D, Oehlberg KA, Katz IR et al (2006) Test characteristics of the 15-item Geriatric Depression Scale and Hamilton Depression Rating Scale in Parkinson’s disease. Am J Geriatr Psychiatry 14(2):169–175
Jenkinson C, Fitzpatrick R, Peto V et al (1997) The Parkinson’s disease questionnaire (PDQ- 39): development and validation of a Parkinson’s disease summary index score. Age Ageing 28:253–257
Owsley C, Stalvey BT, Wells J et al (2001) Visual risk factors for crash involvement in older drivers with cataract. Arch Ophthalmol 19(6):881–887
Gill DJ, Freshamn A, Blender JA et al (2008) The montreal cognitive assessment as a screening tool for cognitive impairment in Parkinson’s disease. Mov Disord 23(7):1043–1046
Nazem S, Siderowf AD, Duda JE et al (2009) Montreal cognitive assessment performance n patients with Parkinson’s disease with normal global cognition according to the mini-mental state examination score. J Am Gerontol Soc 57:304–308
Nasreddine ZS, Phillips NA, Bedirian V et al (2005) The montreal cognitive assessment: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4):695–699
Janke M (1991) Accidents, mileage and the exaggeration of risk. Accid Anal Prev 23(2–3):183–188
Langford J, Koppel S (2005) A tale of two surveys: explaining older drivers’ low mileage bias. Paper presented to the Australasian Road Safety Research, Policing and Education Conference, Wellington, New Zealand, 13–16 Nov 2005
Crizzle AM, Myers AM, Almeida QJ (2012) Drivers with Parkinson’s disease: who participates in research studies? Parkinsonism Relat Disord 18:833–836
Haaxma CA, Bloem BB, Borm GF et al (2007) Gender differences in Parkinson’s disease. J Neurol Neurosurg Psychiatry 78:819–824
Acknowledgments
Both Drs Alexander Crizzle and Anita Myers are members of the Canadian Driving Research Initiative for Vehicular Safety in the Elderly (Candrive), an interdisciplinary health related research program dedicated to improving the safety of older drivers. We would like to acknowledge the support of Candrive, the Schlegel University of Waterloo Research Institute of Aging, and the Sun Life Financial Movement Disorders Research and Rehabilitation Centre at Wilfrid Laurier University.
Conflicts of interest
This study was supported by Canadian Driving Research Initiative for Vehicular Safety in the Elderly (Candrive), Schlegel U-W Research Institute of Aging and the Sun Life Financial Movement Disorders Research & Rehabilitation Centre. No other support was provided. No authors report conflicts of interest pertaining to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Crizzle, A.M., Myers, A.M., Roy, E.A. et al. Drivers with Parkinson’s disease: are the symptoms of PD associated with restricted driving practices?. J Neurol 260, 2562–2568 (2013). https://doi.org/10.1007/s00415-013-7017-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-013-7017-9