Abstract
Impairments in cognition, visual perception, motor function, and increased daytime sleepiness reduce driving performance and safety in Parkinson’s disease (PD). Although drivers with PD perform worse than controls on experimental road and driving simulation studies, there is no well-established epidemiological association with increased crashes in drivers with PD. However, drivers with PD cease driving earlier than controls.
Medical diagnosis or a clinician’s assessment alone is inadequate to determine driving competence in drivers with PD. Although testing of motor, cognitive, and visual functions help to understand the mechanisms of driving impairment in PD, there are no established guidelines on assessing driver fitness in PD. There are no evidence based methods for driver rehabilitation in PD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Road Test
- Crash Risk
- National Highway Traffic Safety Administration
- Paced Auditory Serial Addition Task
- Instrument Vehicle
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Patient Vignette
A 90-year-old man with a 5-year history of Parkinson’s disease returned to clinic for his routine follow-up visit in the company of his daughter. He displayed mild slowing of arm movements, and moderate slowing of foot tapping while seated in a chair. He was able to arise without assistance, and walked slowly but independently. During the course of the visit, his daughter brought up the issue of driving safety. She stated that she was concerned about his driving, that she had witnessed how slow he was to react to other drivers, and that she and other family members had asked him to stop driving. The patient stated that he thought that his driving had not changed, and that he wanted to continue driving. The neurologist discussed the pros and cons of continuing to drive given his age and examination, and given his refusal to stop driving, asked him to undergo a formal driving evaluation at the motor vehicle bureau. He was not keen to agree, fearing the loss of his license if he failed the test, and the neurologist then advised him and his daughter that he should stop driving, documenting this in the medical record.
At his next visit to the clinic 6 months later, his neurologic examination was unchanged. The neurologist inquired whether or not he was still driving. Somewhat sheepishly, he relayed the following story. He had continued driving while wintering in Florida, never travelling more than a couple of miles from his home. Because he never drove on the highway and never went above 30 mph, he was convinced that he was not unsafe. While making a left hand turn, he struck another car that had the right of way. The police were called to the scene, and fortunately no one was injured. On seeing him at the scene, the police officer informed him that he should not be driving, and confiscated his license on the spot. His daughter and family viewed the incident as a near-miss, and his neurologist agreed.
The Scope of the Problem
Driving is an important activity of daily living and is essential for mobility and independence for many individuals. With increased longevity the number of elderly drivers is rising, which will be accompanied by an increase of drivers with neurological diseases of aging such as dementia, stroke, and Parkinson’s disease (PD). In addition to typical motor dysfunction, PD also impairs cognition, vision, sleep, and alertness [1], and is associated with lower performance on road tests [2–13] and driving simulator performance [14–23] compared to controls.
One of the most important concerns in drivers with PD is the potential for increased risk for accidents. Motor vehicle crashes are a major public health problem with about 42,000 fatalities and a financial cost of ∼$231 billion in 2000 [24]. Indeed driving simulation studies have shown increased crash rates in PD [15, 20, 22] and retrospective surveys have suggested increased crashes in drivers with PD [25, 26]. However, increased real-life crash risk in drivers with PD has not been confirmed by community based prospective controlled studies or epidemiological research [27–29]. Another potential unfavorable driving outcome in drivers with PD is loss of vehicular mobility (driving cessation) as shown on cross-sectional or retrospective [25–27, 30–36] and prospective [28] surveys.
The goal in counseling drivers with PD is to prevent crashes while preserving mobility and independence. The methods for assessing driver safety in potentially impaired persons and requirements for reporting vary across the world [27] and among states within the USA [37], and no clear guidelines have been established for PD [38]. Medical diagnosis or a clinician’s assessment alone is inadequate to determine driving competence in those with cognitive impairment [39, 40]. While a proportion of drivers with PD use compensatory strategies such as reduction of driving exposure, avoidance of difficult driving conditions (inclement weather, darkness, rush hour, difficult maneuvers) suggesting some insight into their limitations [28], both patients [2, 3, 9] and their neurologists [2] have been shown to overestimate the patient’s driving ability.
Theoretical Framework to Study Driving
Driving performance is determined by factors related to the driver (e.g., age, medical condition, cognitive, visual, motor or behavioral dysfunction, decreased alertness, substance abuse), environment (weather, road conditions), vehicle (maintenance, presence of warning or safety devices), presence of distractions, and their interactions [41].
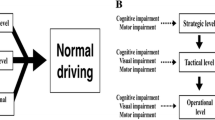
Michon proposed a hierarchical model of cognitive control of driving with concurrent activity at three levels: (a) strategic, (b) tactical/maneuvering, and (c) operational/vehicle control. The decisions to drive during inclement weather or route selection (e.g., freeways vs. urban streets) are examples of strategic behavior that affect driving performance and safety on a time scale of minutes to days. Adjusting speed and car-following distance, choice of lane, or decision to overtake according to road rules and conditions are examples of tactical behaviors, and affect driving on a time scale of 5–60 s. Maintaining lane position with ongoing steering adjustments, keeping a safe distance to the car in front from moment to moment, and reacting to hazards represent operational behaviors, which determine driving in the next 0.5–5 s [42].
At an operational level, driver actions can be analyzed by information processing models (Fig. 26.1): (1) Perception and attention to stimulus (e.g., visual and auditory inputs) and interpretation of the road situation; (2) Planning a reaction to the stimulus based on relevant previous experience in similar situations; (3) Execution of selected plan (e.g., by applying the accelerator, brake or steering controls); and (4) Monitoring the outcome of the behavior and subsequent self correction [43]. The driver’s response to the stimulus (e.g., a hazard such as an illegal intersection incursion by another vehicle) is either safe (able to stop) or unsafe (crash) as a result of errors at one or more of these stages [43].
Information processing model for driver error in PD. From Uc and Rizzo [43]
Neural Substrates of Driving
Driving engages parieto-occipital cortices, cerebellum and cortical regions associated with perception and motor control as shown by fMRI studies during simulation [44] or FDG or positron emission tomography (PET) scanning after a road drive [45]. Alcohol degrades driving performance and decreases activation in these areas [46]. Even a simple auditory-verbal distraction such as listening to sentences produces a significant deterioration in vehicle control and is associated with increased activation in temporal regions at the expense of decreased activation of parietal regions, suggesting that language comprehension performed concurrently with driving draws mental resources (spatial processing by the parietal lobe) away from the primary task and impairs driving performance [47]. Alcohol amplifies the negative effects of distraction on brain activation and driving performance [48].
PD pathology involves many regions in the brain, leading to multiple cognitive, visual and motor impairments that can interfere with driving performance at different levels. For example, decreased decision making ability/executive dysfunction due to frontostriatal dysfunction can lead to poor strategic and tactical choices such as driving under challenging conditions and making risky maneuvers. Impairments in attention, visual perception, memory, executive functions, motor speed, and self-monitoring can lead to driver errors at operational level with unsafe responses to sudden hazards.
Driving Research in PD
Due to the complexity of the driving task and PD, multiple complementary assessment methods in comparison to a control group need to be studied longitudinally to determine the predictors of driving safety and outcomes. Off-road batteries usually combine questionnaires on general health, mood and sleep, quality of life, driving history and habits, with performance based measures of cognition, vision and motor function. As real life crashes are rare events, driving performance in a simulator and road test in an instrumented vehicle are used as intermediate steps to uncover relationships between cognitive, visual, motor impairments and driving outcomes. While most driving experience consists of uneventful long stretches, there are interspersed segments with multitasking. Some of the secondary tasks are required as part of driving (e.g., following a new route to reach a destination, paying attention to landmarks and traffic signs, listening to radio for weather updates), others may be discretionary (e.g., speaking on a cell phone, talking to a passenger or eating). The secondary tasks can have a degrading effect on driver safety and performance, especially in drivers with cognitive dysfunction.
Off-Road Battery
Demographics
The patients in reported studies of driving in PD are usually in their 60s or 70s and predominantly male, have mild–moderate disease severity, and live in the community [11]. The male predominance among drivers in PD may reflect that men are at higher risk for PD [26] and that women in this age group have not traditionally been the main driver in the family, and might have more readily relinquished their driving privileges once they developed PD [5].
Driving History and Habits
Questionnaires (e.g., Driving Habits Questionnaire [28]) are used to collect self-report information on driving exposure (e.g., miles/week, days/week), driving history (crashes and citations), perceptions and judgments of impairment and driving ability, and use of compensatory strategies (e.g., no driving at night or in snow). The driving history can be verified by using state records. The caregiver perspective can also give valuable insights on driving ability and deficiency awareness of the patient [10].
Assessments of Cognition, Vision, Motor Function, Indices of Parkinsonism, Sleep, Psychiatric Problems
Although individual tests may differ between batteries used by various research teams, they attempt to probe different aspects of visual perception, cognition (e.g., executive functions, attention, and memory), motor function, mood and sleep. As driving is a primarily visual task, these batteries are rich in visual tests and usually cover all aspects of visual function from the retinal to the cortical level. In most studies, drivers with PD had mild–moderate parkinsonism and performed worse compared to controls on most visual and cognitive abilities, albeit usually showing mild deficits [2, 3, 5–8, 11, 13, 14, 18–20, 22, 23, 27].
Road Testing
In this set of studies (Table 26.1), drivers with PD underwent standardized road tests and various tests of cognition, vision and motor function. Most studies included control drivers with similar demographics. The main outcome measures of these road tests were pass/fail (or safe/unsafe) ratings by driving experts as categorical measures and/or at-fault error counts as continuous measures. Types and locations of errors were also reported (Table 26.2). Analyses were done within PD group to determine the cognitive, visual, and motor predictors of pass/fail ratings or error counts.
Heikkila [2] assessed the driving ability of 20 patients with idiopathic PD and 20 age- and gender-matched healthy control subjects on the road and showed that patients and their neurologists typically overestimate driving ability. All subjects also underwent a neuropsychological battery (measuring vigilance and concentration, visual perception, choice reaction times, and information processing). The driving abilities of PD patients were estimated by a neurologist and by a psychologist using tests and an interview, by a driving instructor on the basis of a driving test, and by the patients themselves using the same global scale. The patients with PD performed worse than the controls both on neuropsychological tests and on the road test. The driving instructor found 35% of PD drivers unsafe, while none of the patients were rated unsafe by themselves or the neurologist. There was a significant correlation between the driver instructor scores and the psychologist’s estimates, but not with the neurologist’s estimates. All controls were found safe, and there was agreement between all parties. Drivers with PD committed significantly more at-fault errors, violated the traffic rules more often, and had more difficulty driving in a traffic flow and turning across traffic, especially in urban conditions. In both the patient group and the control group, there was a high correlation between performances in the neuropsychology battery and driving test. Disease duration and the motor stage of the disease, and MMSE were not associated with the driving test scores in PD patients; however, slower information processing correlated with faults observed while driving on the road [2].
Grace [4] compared road safety (error counts and ratings of “safe,” “marginal,” “unsafe”) of drivers with PD (n = 21), mild Alzheimer’s disease (n = 20, Clinical Dementia Rating scale range 0–1), and controls (n = 21). Drivers with AD were more impaired on the road than PD. Compared to other groups, drivers with PD had difficulty in maneuvers requiring head turning. Driving performance in PD was related to disease severity (Hoehn-Yahr stage), cognitive measures (Rey Osterreith Complex Figure, Trails B, Hopkins Verbal List Learning Test-delay), and specific motor symptoms (axial rigidity, postural instability), but not to the UPDRS motor total score [4].
Wood [3] assessed driving performance (safety error counts and types, overall pass/fail judgement) of 25 patients with idiopathic PD and 21 age-matched controls on a standardized open road route. The drivers with PD were rated as significantly less safe than controls, and more than half of the drivers with PD would not have passed a state-based driving test. The driver safety ratings were significantly correlated with disease duration but not severity, as indexed by the “on” time UPDRS score. Drivers with PD made significantly more errors than the control group during maneuvers that involved changing lanes and lane keeping, monitoring their blind spot, reversing, car parking, and traffic light controlled intersections. The driving instructor had to intervene to avoid an incident significantly more often for drivers with PD than for controls [3]. Tests of motor performance (Purdue Pegboard test), contrast sensitivity (Pelli-Robson test), and cognitive function (verbal version of Symbol Digit Modalities test) predicted passing the driving test with relatively high sensitivity and moderate specificity [7].
Devos studied 40 patients with PD and 40 healthy age- and sex-matched control subjects in the simulator and administered an off-road test battery [9] to predict the results of driving fitness on a road test administered by an official agency. A “pass” (fit to drive without restrictions) rating was given to 72.5% of PD drivers, and the rest (27.5%) received a “fail” rating, defined as being judged as “fit to drive with restrictions” (25%) or “unfit to drive” (2.5%, n = 1). A screening battery assessing four clinical variables (disease duration, contrast sensitivity, Clinical Dementia Rating, and motor part of the Unified Parkinson’s Disease Rating Scale) provided the best model to predict the pass/fail ratings, correctly classifying 90% of the patients with PD as pass or fail. The Test Ride for Investigating Practical fitness to drive (TRIP) driving simulator score discriminated significantly between drivers with PD and controls [9]. However, only drivers with “minor cognitive deterioration” [9] were enrolled in this study, limiting the generalizability of these results.
Cordell [10] assessed 53 PD subjects and 129 controls in the participant’s car along a 15 km route chosen by the participant in his/her neighborhood. Drivers with PD were significantly less competent drivers than controls. The driving performance of the participants declined with age. UPDRS-ADL score and Timed Get Up and Go test correlated with the driving performance. IQ Code (Informant Questionnaire on cognitive decline) was used to assess cognitive status. No other performance based tests to assess cognition or visual perception were reported. In models adjusted for age, gender and disease duration, information provided by caregivers explained 56% of variability in road test scores, whereas UPDRS-ADL and the timed walking test only explained ∼30% of variability [10].
Classen [12] compared 19 drivers with PD and 104 controls on a road test and found that 42.1% of PD and 21.2% of controls failed (p < 0.05). Among several variables that significantly correlated with failing the road test and number of driving errors in PD, The Useful Field of View (UFOV) test was found to have the strongest correlation [12].
Uc [11] compared at-fault safety errors of 84 licensed, active drivers with PD with mild–moderate disease severity (median Hoehn Yahr stage II) and 182 controls on a standardized route across urban and rural settings using an instrumented vehicle (IV) [11]. Overall, drivers with PD had poorer road safety compared to controls, but there was considerable variability among the PD drivers, and some performed normally. Drivers with PD committed significantly more total safety errors compared to controls (41.6 ± 14.6 vs. 32.9 ± 12.3) and 77.4% of PD drivers committed more errors than the median total error count of the controls (medians: PD = 39.5, controls = 31.0). Lane violations were the most common error category, and group differences in some error categories became insignificant after results were adjusted for demographics and familiarity with the local driving environment. Within the PD group, older age and worse performances on tests of visual acuity, contrast sensitivity, attention, visuospatial abilities, visual memory, and general cognition predicted error counts. Measures of visual processing speed and attention (UFOV test) and far visual acuity were jointly predictive of error counts in a multivariate model [11]. An alternative model using CFT-COPY (another strong univariate predictor) resulted in slightly smaller but still significant R-squared value. The advantage of CFT-COPY is that it is a paper-pencil test, which is in public domain and is quick to administer [11]. The follow-up of this cohort [11] showed that 38% of PD drivers and 68% of control drivers returned about 2 years later for follow-up road test [13]. Drivers with PD who returned had fewer safety errors at baseline compared to those who didn’t return, whereas no such difference was observed among controls. Compared to controls, the PD group showed a significantly greater increase in total error counts longitudinally (median 13.5 vs. 3.0). Measures of visual processing speed/attention (UFOV) and global cognition predicted decline in driving safety within PD [13].
As part of the road drive in an IV, Uc compared multitasking abilities of drivers with PD and controls by administering tasks (Table 26.1) on navigation (route following) [8], visual search [6], and mental arithmetic (to simulate audioverbal distraction) [5]. Drivers with PD took longer to finish the route following task [8]. A higher proportion of PD drivers made incorrect turns, got lost, or committed at-fault safety errors [8]. Within the PD group, the navigational and safety errors were predicted by poor performance on cognitive and visual tests, but not by the severity of motor dysfunction [8]. During the same IV drive, drivers were asked to report sightings of specific landmarks and traffic signs along a four-lane commercial strip to assess the ability for visual search and recognition of roadside targets [6]. The drivers with PD identified significantly fewer landmarks and traffic signs, and they committed more at-fault safety errors during the task than control subjects, even after adjusting for baseline errors. Within the PD group, the most important predictors of landmark and traffic sign identification rate were performances on visual speed of processing and attention and visuospatial abilities. Trail Making Test (B-A), a measure of cognitive flexibility independent of motor function, was the only independent predictor of at-fault safety errors in drivers with PD [6]. In another IV experiment in this cohort of PD patients and controls, the effects of auditory-verbal distraction on driving performance in PD were assessed using the Paced Auditory Serial Addition Task (PASAT) [5]. Despite driving slower, drivers with PD were more affected by the distracter task with increased safety errors and higher speed. Decreased performance on tests of cognitive flexibility, verbal memory, postural control, and increased daytime sleepiness predicted worsening of driving performance due to distraction within the PD group [5].
Driving Simulation
Although actual road testing provides richer and more balanced visual, tactile, vibratory, and vestibular cues to the driver [43], road conditions vary between subjects and some maneuvers may be unsafe to test. Driving simulators replicate the experimental conditions for each subject and enable administration of challenging tasks in a safe environment with complete experimental control [49]. Driving simulators may vary widely in their technical characteristics (e.g., motion base vs. fixed base, interactivity, resolution, and field of view). Validation of individual simulators and driving scenarios is needed to derive meaningful conclusions from their administration. Another important concern about simulators is “simulator sickness” (similar to motion sickness), also known as simulator adaptation syndrome, which occurs in a proportion of drivers due to visual vestibular mismatch and can reduce performance or preclude simulation all together [50]. Most studies in the following section (Table 26.3) were performed on medium-high fidelity simulators with a fixed motion base.
Drivers with PD are able to tolerate simulated driving similarly to elderly healthy drivers [20]. Simulator studies in drivers with PD showed impaired steering accuracy, slower driving reaction times, missing red lights [21], impaired land keeping, increased crashes [15] especially rear end collisions [22] and crashes at intersections [20] under low visibility conditions. In these studies, PD driver performance was associated with cognitive and visual dysfunction as well as severity of parkinsonism, especially for reaction times in tasks where speed of response was critical (e.g., reaction to sudden hazard such as an illegal intersection incursion by another vehicle [20]) (Fig. 26.2).
Diagrams of vehicle kinematics and the vehicle path after the intersection incursion was triggered (4.0 s before the intersection as determined by driver speed) in three participants. The common ordinate scale shows the driver’s vehicle speed, percentage of pedal application for accelerator and brake, and steering wheel rotations in degrees (upward deflections are counterclockwise rotations). The x-axis ends at the expected position of the incurring vehicle. The upper panel shows vehicle path inside the lane. (a) A control participant able to stop timely before colliding with the incurring vehicle. At 1.83 s after the trigger, he releases the accelerator and starts braking with a smooth deceleration. The brake is applied 82% at the time of stopping. (b) The driver with Parkinson disease (PD) reacts late (2.73 s) and collides with the incurring vehicle at 34 mph. (c) This driver with PD does not perceive the incurring vehicle, does not react at all, and crashes at 58 mph. Modified from Uc et al. [20]
Drivers with PD have difficulty generating internal cues from memory, and rely on external cues such as warnings and signs for better driving performance due to attentional and executive dysfunction [14], akin to the usefulness of visual cues to overcome freezing. Concurrent distracting auditory-verbal [19] or motor tasks [23] take a larger toll on vehicle control and reaction to hazards in drivers with PD compared to controls, although they tend to drive slower and perform worse on the secondary tasks. The impact of these secondary tasks on drivers with PD is associated with an increased severity of their executive and attentional dysfunction.
Real-Life Driving Outcomes
There are no well established epidemiologic data on crash risk in PD [29]. However, a retrospective, cross-sectional questionnaire study from a movement disorders center found that 20% of PD patients had stopped driving due to increased accidents [25]. The frequency of crashes in subjects with more severe PD (Hoehn and Yahr [HY] stage III) was fivefold higher than controls, whereas patients with mild PD (HY I) reported almost twice as many crashes as the controls. An MMSE score of 23 or less was associated with a threefold increased crash rate.
A large mail and phone survey from Germany revealed that 82% of PD patients held a driving license, and 60% of them still actively drove. Of the patients holding a driving license, 15% had been involved in and 11% had caused at least one accident during the past 5 years [26]. The risk of crashes significantly increased for patients who felt moderately impaired by PD, had an increased ESS score, or had reported “sleep attacks” while driving. Female gender, more severe parkinsonism, sleepiness, older age and longer disease duration were associated with driving cessation [26].
In a cross-sectional study among PD patients, Cubo [36] found that compared to current drivers, ex-drivers were significantly older, had longer disease duration, had more overall cognitive dysfunction and greater motor impairment as measured by the CISI (Clinical Impression of Severity Index), HY stage, and the SCOPA (Scales for Outcomes in Parkinson’s disease) motor scale and difficulty in activities of daily life. Aging and ADL impairment were the principal clinical predictors that differentiated drivers from ex-drivers [36].
Review of the records of drivers with PD referred to the Scottish Driving Assessment Service over a 15-year period revealed that 66% were able to continue driving, with about half of them receiving recommendations for vehicle modifications. The ability to drive was predicted by the severity of parkinsonism, reaction time, presence of significant comorbidities and poor score on road testing [34].
Our longitudinal, prospective cohort study of 106 drivers with PD and 130 elderly control drivers [28] showed that 40.6% of PD drivers ceased driving compared to 16.9% of control drivers with an estimated HR (95% CI) of 7.09 (3.66, 13.75) for PD, adjusted for age, gender, education and driving exposure at baseline. This was consistent with prior retrospective reports and also consistent with other studies in which PD was found to play a major role in driving cessation but not a significant factor in crashes [35, 51–53]. The Kaplan–Meier plot (Fig. 26.3) shows the probability of still driving (or inversely, the risk of driving cessation) at any particular time point during follow-up, and allows visual comparison between groups for between-group comparisons over time [28]. For example, the cumulative incidence (95% CI) of driving cessation at 2 years after baseline was 17.6% (11.5%, 26.5%) for PD and 3.1% (1.2%, 8.1%) for controls [28]. Significant individual risk factors for driving cessation within PD included older age, decreased driving exposure, poorer ratings of driving ability by self and others, higher number of road errors and past crashes, increased use of compensation strategies, poorer performances in most measures of vision, and higher severity of parkinsonism. A multivariate analysis of risk factors in PD showed a preference to be driven by others, higher UFOV total score, higher UPDRS-ADL scores, and higher daily levodopa equivalent as the most important risk factors for driving cessation [28]. There was no statistically significant difference between groups on crashes; however, the study had limited power to detect differences in crashes due to small number of crashes that occurred. Of note, our results in PD are similar to observations in Alzheimer’s disease (AD) by other researchers where driving cessation was the main outcome without showing increased crashes [40]. The likely reasons for these findings may include attrition of potentially unsafe drivers with AD or PD before a potential crash, or restricted driving and strategic compensation [28].
Kaplan–Meier Curves for Driving Cessation (Logrank test χ 2 = 37.53, p-value <0.0001) between subjects with Parkinson’s Disease and elderly control subjects. From Uc et al. [28]
Special Issues Requiring Further Study
Effect of Sleep Related Impairments
Ever since Frucht’s [54] observation that PD patients taking the dopamine agonists ropinirole and pramipexole may experience “sleep attacks” leading to car crashes, excessive daytime sleepiness (EDS), or “sleep attacks” have been reported with all dopaminergic medications used to treat PD [55]. About 33% (range 16–74%) of patients with PD suffer from EDS; the estimates for “sleep attacks” are 1–14%, with 1–4% experiencing them during driving [56]. The mechanisms of sleepiness and sleep attacks in PD might include a complex drug–disease interaction with degeneration in sleep centers in the brain and side effects of dopaminergic medications, particularly direct dopamine agonists [56].
Several studies using self-report measures such as the Epworth Sleepiness Scale (ESS, cut-off score 7–10) [11, 20, 26, 33, 57, 58] found a relationship of EDS with driving performance in PD; real sleep attacks without any prior sleepiness were rare. However, the ESS does not correlate well with a more objective measure of sleepiness [55]. Empirical studies using experimental performance measures for driving and physiological measures of sleep while driving are needed to describe the characteristics of sleep related driving problems and predictors of poor outcomes due to wakefulness disorders in PD [17].
Effect of PD Treatment
Road testing in drivers with PD has usually been performed when patients are in the “on” state due to ethical (subject protection) and practical (normally subjects would not start driving without treatment effect) concerns. Thus there are no data on driving performance comparing “on” and “off” states of PD patients on the road. However, this can be potentially tested in the safe environment of a driving simulator. No significant correlations of dopaminergic medication dosage (levodopa equivalent per day) could be found with empirical driving performance [3, 5–8, 10, 11, 18, 20]. We found that higher levodopa equivalent at baseline predicted earlier driving cessation [28], probably as a surrogate measure of disease severity.
There are limited data comparing the effect of dopaminergic medication class (levodopa vs. direct agonists) on driving. Uc [8] classified PD drivers as being on levodopa, dopamine agonist, on levodopa and dopamine agonist, or other/no treatment, and made formal comparisons among these groups. There was no effect of medication group status on safety errors or performance on the route following task [8].
Guidelines on Driver Fitness Assessment and Reporting to Licensing Authorities
There are no evidence-based practice parameters for driving in PD to date. However, recent National Highway Traffic Safety Administration (NHTSA) [59] and Federal Motor Carrier Safety Administration (FMCSA) [60] guidelines suggest a case by case, multidisciplinary evaluation of the patient due to the highly individualized nature of the disease and variable progression. Assessment of visual and cognitive abilities and severity of parkinsonism can inform about the potential risk for undesirable driving outcomes. Additional information can be obtained from recent driving record and insights provided by the patient and family into driving safety concerns or changes in driver habits (e.g., compensation strategies to lower risk). A recent evidence based review [61] discusses the role of various cognitive, visual, and motor tests in predicting driver safety in PD.
Reporting requirements for medically impaired drivers are not uniform across the USA and across the world. The healthcare providers should familiarize themselves with local rules and regulations on reporting of medically impaired drivers. The American Academy of Neurology (AAN) “supports optional reporting of individuals with medical conditions that may impact one’s ability to drive safety, especially in cases where public safety has already been compromised, or it is clear that the person no longer has the skills needed to drive safely” and advocates immunity for physicians “both for reporting and not reporting a patient’s condition when such action is taken in good faith, when the patient is reasonably informed of his or her driving risks, and when such actions are documented by the physician in good faith” [62].
Interventions to Improve Driving in PD
The literature on driving rehabilitation of elderly or neurologically impaired drivers is limited. Physical retraining and visual perception retraining may improve driving related skills in older drivers [63–66]. Speed of processing or reasoning training may delay driving cessation in the elderly [67]. There was moderate evidence that educational interventions improve driving awareness and driving behavior, but do not reduce crashes in older drivers [63, 68–70]. Short-term trials using physical conditioning [71] or classroom and road retraining [72] showed improvements in post-training road test performances, but impact on future real life outcomes has not been reported. An intense simulator training program led to significant improvements within the simulator and was associated with passing an official driving assessment in stroke survivors [73]. However, there was no difference in driving cessation in these stroke patients between the simulator training and control groups at 5 years [74].
To our knowledge, there are no published reports on driver rehabilitation in PD except our pilot studies showing feasibility of simulator training [75, 76]. The challenge is to identify the drivers who would benefit from such intervention, to determine the remediable components of driving impairment, and to design intervention methods that are feasible and useful.
References
Uc EY, Rizzo M, Anderson SW, et al. Visual dysfunction in Parkinson disease without dementia. Neurology. 2005;65:1907–13.
Heikkila VM, Turkka J, Korpelainen J, et al. Decreased driving ability in people with Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1998;64:325–30.
Wood JM, Worringham C, Kerr G, et al. Quantitative assessment of driving performance in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2005;76:176–80.
Grace J, Amick MM, D’Abreu A, et al. Neuropsychological deficits associated with driving performance in Parkinson’s and Alzheimer’s disease. J Int Neuropsychol Soc. 2005;11:766–75.
Uc EY, Rizzo M, Anderson SW, et al. Driving with distraction in Parkinson disease. Neurology. 2006;67:1774–80.
Uc EY, Rizzo M, Anderson SW, et al. Impaired visual search in drivers with Parkinson’s disease. Ann Neurol. 2006;60:407–13.
Worringham CJ, Wood JM, Kerr GK, et al. Predictors of driving assessment outcome in Parkinson’s disease. Mov Disord. 2006;21:230–5.
Uc EY, Rizzo M, Anderson SW, et al. Impaired navigation in drivers with Parkinson’s disease. Brain. 2007;130:2433–40.
Devos H, Vandenberghe W, Nieuwboer A, et al. Predictors of fitness to drive in people with Parkinson disease. Neurology. 2007;69:1434–41.
Cordell R, Lee HC, Granger A, et al. Driving assessment in Parkinson’s disease-A novel predictor of performance? Mov Disord. 2008;23:1217–22.
Uc EY, Rizzo M, Johnson AM, et al. Road safety in drivers with Parkinson disease. Neurology. 2009;73:2112–9.
Classen S, McCarthy DP, Shechtman O, et al. Useful field of view as a reliable screening measure of driving performance in people with Parkinson’s disease: results of a pilot study. Traffic Inj Prev. 2009;10:593–8.
Uc, EY, Rizzo, M, Johnson, AM, et al. Longitudinal Decline of Driving Safey in Parkinson’s Disease. Annals of Neurology 66[S13], 52. 2009.
Stolwyk RJ, Triggs TJ, Charlton JL, et al. Impact of internal versus external cueing on driving performance in people with Parkinson’s disease. Mov Disord. 2005;20:846–57.
Zesiewicz TA, Cimino CR, Malek AR, et al. Driving safety in Parkinson’s disease. Neurology. 2002;59:1787–8.
Madeley P, Hulley JL, Wildgust H, et al. Parkinson’s disease and driving ability. J Neurol Neurosurg Psychiatry. 1990;53:580–2.
Moller JC, Stiasny K, Hargutt V, et al. Evaluation of sleep and driving performance in six patients with Parkinson’s disease reporting sudden onset of sleep under dopaminergic medication: a pilot study. Mov Disord. 2002;17:474–81.
Stolwyk RJ, Charlton JL, Triggs TJ, et al. Neuropsychological function and driving ability in people with Parkinson’s disease. J Clin Exp Neuropsychol. 2006;28:898–913.
Stolwyk RJ, Triggs TJ, Charlton JL, et al. Effect of a concurrent task on driving performance in people with Parkinson’s disease. Mov Disord. 2006;21:2096–100.
Uc EY, Rizzo M, Anderson SW, et al. Driving under low-contrast visibility conditions in Parkinson disease. Neurology. 2009;73:1103–10.
Lings S, Dupont E. Driving with Parkinson’s disease. A controlled laboratory investigation. Acta Neurol Scand. 1992;86:33–9.
Uc EY, Rizzo M, Liu D, et al. Increased rear-end collisions in drivers with Parkinson’s disease. Mov Disord. 2009;24:S315.
Uc EY, Rizzo M, Sparks J, et al. Effect of concomitant motor task on driving in Parkinson disease. Mov Disord. 2006;21:S580.
Shafi S, Parks J, Gentilello L. Cost benefits of reduction in motor vehicle injuries with a nationwide speed limit of 65 miles per hour (mph). J Trauma. 2008;65:1122–5.
Dubinsky RM, Gray C, Husted D, et al. Driving in Parkinson’s disease. Neurology. 1991;41:517–20.
Meindorfner C, Korner Y, Moller JC, et al. Driving in Parkinson’s disease: mobility, accidents, and sudden onset of sleep at the wheel. Mov Disord. 2005;20:832–42.
Klimkeit EI, Bradshaw JL, Charlton J, et al. Driving ability in Parkinson’s disease: current status of research. Neurosci Biobehav Rev. 2009;33:223–31.
Uc EY, Rizzo M, Johnson AM, et al. Real-life driving outcomes in Parkinson disease. Neurology. 2011;76:1894–902.
Homann CN, Suppan K, Homann B, et al. Driving in Parkinson’s disease—a health hazard? J Neurol. 2003;250:1439–46.
McLay P. The parkinsonian and driving. Int Disabil Stud. 1989;11:50–1.
Borromei A, Caramelli R, Chieregatti G, et al. Ability and fitness to drive of Parkinson’s disease patients. Funct Neurol. 1999;14:227–34.
Adler G, Rottunda S, Bauer M, et al. The older driver with Parkinson’s disease. J Gerontol Soc Work. 2000;34:39–49.
Hobson DE, Lang AE, Martin WR, et al. Excessive daytime sleepiness and sudden-onset sleep in Parkinson disease: a survey by the Canadian Movement Disorders Group. JAMA. 2002;287:455–63.
Singh R, Pentland B, Hunter J, et al. Parkinson’s disease and driving ability. J Neurol Neurosurg Psychiatry. 2007;78:363–6.
Lafont S, Laumon B, Helmer C, et al. Driving cessation and self-reported car crashes in older drivers: the impact of cognitive impairment and dementia in a population-based study. J Geriatr Psychiatry Neurol. 2008;21:171–82.
Cubo E, Martinez MP, Gonzalez M, et al. What contributes to driving ability in Parkinson’s disease. Disabil Rehabil. 2010;32:374–8.
Wang CC, Carr DB. Older driver safety: a report from the older drivers project. J Am Geriatr Soc. 2004;52:143–9.
Driver Fitness Medical Guidelines. DOT HS 811 210. 2009. National Highway Traffic Safety Administration. US Department of Transportation.
Ott BR, Anthony D, Papandonatos GD, et al. Clinician assessment of the driving competence of patients with dementia. J Am Geriatr Soc. 2005;53:829–33.
Ott BR, Heindel WC, Papandonatos GD, et al. A longitudinal study of drivers with Alzheimer disease. Neurology. 2008;70:1171–8.
Galski T, Bruno RL, Ehle HT. Driving after cerebral damage: a model with implications for evaluation. Am J Occup Ther. 1992;46:324–32.
Lee JD, Strayer DL. Preface to the special section on driver distraction. Hum Factors. 2004;46:583–6.
Uc EY, Rizzo M. Driving and neurodegenerative diseases. Curr Neurol Neurosci Rep. 2008;8:377–83.
Spiers HJ, Maguire EA. Neural substrates of driving behaviour. Neuroimage. 2007;36:245–55.
Jeong M, Tashiro M, Singh LN, et al. Functional brain mapping of actual car-driving using [18 F]FDG-PET. Ann Nucl Med. 2006;20:623–8.
Meda SA, Calhoun VD, Astur RS, et al. Alcohol dose effects on brain circuits during simulated driving: an fMRI study. Hum Brain Mapp. 2009;30:1257–70.
Just MA, Keller TA, Cynkar J. A decrease in brain activation associated with driving when listening to someone speak. Brain Res. 2008;1205:70–80.
Allen AJ, Meda SA, Skudlarski P, et al. Effects of alcohol on performance on a distraction task during simulated driving. Alcohol Clin Exp Res. 2009;33:617–25.
Uc EY, Rizzo M, Anderson SW, et al. Unsafe rear-end collision avoidance in Alzheimer’s disease. J Neurol Sci. 2006;251:35–43.
Uc EY, Rizzo M. Driving in Alzheimer’s Disease, Parkinson’s Disease, and Stroke. In: Fisher D, Lee JD, Caird J, et al., editors. Handbook of driving simulation in engineering, medicine and psychology. Boca Raton: CRC Press; 2011.
Campbell MK, Bush TL, Hale WE. Medical conditions associated with driving cessation in community-dwelling, ambulatory elders. J Gerontol. 1993;48:S230–4.
Hu PS, Trumble DA, Foley DJ, et al. Crash risks of older drivers: a panel data analysis. Accid Anal Prev. 1998;30:569–81.
Sims RV, Owsley C, Allman RM, et al. A preliminary assessment of the medical and functional factors associated with vehicle crashes by older adults. J Am Geriatr Soc. 1998;46:556–61.
Frucht S, Rogers JD, Greene PE, et al. Falling asleep at the wheel: motor vehicle mishaps in persons taking pramipexole and ropinirole. Neurology. 1999;52:1908–10.
Comella CL. Daytime sleepiness, agonist therapy, and driving in Parkinson disease. JAMA. 2002;287:509–11.
De Cock VC, Vidailhet M, Arnulf I. Sleep disturbances in patients with parkinsonism. Nat Clin Pract Neurol. 2008;4:254–66.
Korner Y, Meindorfner C, Moller JC, et al. Predictors of sudden onset of sleep in Parkinson’s disease. Mov Disord. 2004;19(11):1298–305.
Ghorayeb I, Loundou A, Auquier P, et al. A nationwide survey of excessive daytime sleepiness in Parkinson’s disease in France. Mov Disord. 2007;22(11):1567–72.
Driver Fitness Working Group of the American Association of Motor Vehicle Administrators (AAMVA). Driver Fitness Medical Guidelines. Pages. 24-28. 2009. National Highway Traffic Safety Administration (NHTSA).
Caruso, G, Dawson, J, Deluca, J, et al. Opinions of Expert Panel: Parkinson’s Disease, Multiple Sclerosis, and Commercial Motor Vehicle Driver Safety, presented to Federal Motor Carrier Safety Administration. 2009.
Crizzle AM, Classen S, Uc EY. Parkinson’s disease and driving: An evidence based review. Neurology. 2012 (in press).
Bacon D, Fisher RS, Morris JC, et al. American Academy of Neurology position statement on physician reporting of medical conditions that may affect driving competence. Neurology. 2007;68:1174–7.
Kua A, Korner-Bitensky N, Desrosiers J, et al. Older driver retraining: a systematic review of evidence of effectiveness. J Safety Res. 2007;38:81–90.
Mazer BL, Sofer S, Korner-Bitensky N, et al. Use of the UFOV to evaluate and retrain visual attention skills in clients with stroke: a pilot study. Am J Occup Ther. 2001;55:552–7.
Mazer BL, Sofer S, Korner-Bitensky N, et al. Effectiveness of a visual attention retraining program on the driving performance of clients with stroke. Arch Phys Med Rehabil. 2003;84:541–50.
Roenker DL, Cissell GM, Ball KK, et al. Speed-of-processing and driving simulator training result in improved driving performance. Hum Factors. 2003;45:218–33.
Ball K, Edwards JD, Ross LA, et al. Cognitive training decreases motor vehicle collision involvement of older drivers. J Am Geriatr Soc. 2010;58:2107–13.
Bedard M, Isherwood I, Moore E, et al. Evaluation of a re-training program for older drivers. Can J Public Health. 2004;95:295–8.
Owsley C, Stalvey BT, Phillips JM. The efficacy of an educational intervention in promoting self-regulation among high-risk older drivers. Accid Anal Prev. 2003;35:393–400.
Owsley C, McGwin Jr G, Phillips JM, et al. Impact of an educational program on the safety of high-risk, visually impaired, older drivers. Am J Prev Med. 2004;26:222–9.
Marottoli RA, Allore H, Araujo KL, et al. A randomized trial of a physical conditioning program to enhance the driving performance of older persons. J Gen Intern Med. 2007;22: 590–7.
Marottoli RA, Ness PH, Araujo KL, et al. A randomized trial of an education program to enhance older driver performance. J Gerontol A Biol Sci Med Sci. 2007;62:1113–9.
Akinwuntan AE, De Weerdt W, Feys H, et al. Effect of simulator training on driving after stroke: a randomized controlled trial. Neurology. 2005;65:843–50.
Devos H, Akinwuntan AE, Nieuwboer A, et al. Comparison of the effect of two driving retraining programs on on-road performance after stroke. Neurorehabil Neural Repair. 2009; 23:699–705.
Dawson JD, Rizzo M, Anderson SW, et al. Collision avoidance training using a driving simulator in drivers with Parkinson’s disease: a pilot study. In: Boyle LN, Lee JD, McGehee DV, et al., editors. Proceedings of Driving Assessment 2009: The Fifth International Driving Symposium on Human Factors in Driver Assessment, Training and Vehicle Design. Iowa City, Iowa: The University of Iowa; 2009. p. 154–60.
Uc EY, Rizzo M, Anderson SW, et al. Driver rehabilitation in Parkinson’s disease using a driving simulator: a pilot study. In: Boyle LN, Lee JD, McGehee DV, editors. Proceedings of Driving Assessment 2011: The Sixth International Driving Symposium on Human Factors in Driver Assessment, Training and Vehicle Design. Iowa City: University of Iowa; 2011. p. 248–54.
Radford K, Lincoln N, Lennox G. The effects of cognitive abilities on driving in people with Parkinson’s disease. Disabil Rehabil. 2004;26:65–70.
Amick MM, Grace J, Ott BR. Visual and cognitive predictors of driving safety in Parkinson’s disease patients. Arch Clin Neuropsychol. 2007;22:957–67.
Acknowledgments
Supported by NIH R01 grant NS044930.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Uc, E.Y. (2013). Driving Risk in Patients with Movement Disorders. In: Frucht, S. (eds) Movement Disorder Emergencies. Current Clinical Neurology. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-60761-835-5_26
Download citation
DOI: https://doi.org/10.1007/978-1-60761-835-5_26
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-60761-834-8
Online ISBN: 978-1-60761-835-5
eBook Packages: MedicineMedicine (R0)