Abstract
The objectives of this study were to describe the characteristics of RBD in a group of PD patients and verify the accuracy of the clinical interview in this group, determine the causes of failure of the interview, as well as to verify the clinical and polysomnographic differences between the groups of PD patients with and without RBD. So, a cross-sectional study was conducted in 88 consecutive PD patients from the outpatient clinic, during a period of 21 months. Participants underwent a clinical interview, assessment based on standardized scales (Epworth Sleepiness Scale, Parkinson’s disease Questionnaire, Pittsburgh Sleep Quality Index), and video polysomnography. Out of the 88 participants, 55 underwent vPSG which confirmed a diagnosis of RBD. The clinical interview had a high sensitivity (87.5%) but a low specificity (42.1%) for RBD diagnosis and thus the clinical interview alone may miss those without episodes of dream-enacting behavior. We note in this group a higher proportion of men (54.5%) and an average age of 60.4 years ± 10.6. In 54% of patients, RBD preceded motor symptoms of PD. In addition, patients with PD and RBD had lower Apnea–Hypopnea Index in REM sleep and a higher equivalent dose of levodopa than PD patients without RBD. RBD is a prevalent condition in patients with PD, requiring polysomnography for diagnostic confirmation, and is associated with certain particularities in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
REM sleep behavior disorder (RBD) is characterized by loss of skeletal muscle atonia during REM sleep associated with nightmares and dreams’ enactment [1,2,3,4]. There is an association of RBD with diseases that are generated by the deposition of alpha-synuclein in neurons, such as Parkinson’s disease (PD), multiple system atrophy (MSA), and Lewy body dementia (LBD) [5, 6]. There is already evidence from experimental studies demonstrating that neurons located in the upper brainstem structures particularly the bulbar–pontine transition (sublaterodorsal nucleus-SLD and pre-coeruleus region) are active during REM sleep (called REM “on cells”) and important for the regulation of REM sleep and atonia [7, 8]. These neurons participate via a direct or indirect inhibitory descending pathway through the reticular magnocellular tract and glycinergic neurons on the spinal motor neurons [9]. The neurodegenerative process that occurs in PD with abnormal deposition of this phosphorylated alpha-synuclein leads to the formation of intraneuronal inclusion bodies, the so-called Lewy bodies, which may induce a dysfunction of this nucleus and its afferent or efferent pathways or both, resulting in loss of the normal inhibition of the motor neuron [10] and the clinical manifestation of the RBD [11, 12].
A prevalence of presumptive RBD in 15–40% of PD patients was observed in studies using RBD screening scales and frequency of confirmed RBD in up to 62.5% in studies using video polysomnography [13,14,15,16]. There is a difference in accuracy when a clinical evaluation is considered alone or in association with polysomnography [4], and a need for better identification of possible failures of clinical interview and/or scales in the diagnosis of this condition.
The presence of RBD in individuals with PD is associated with a severe clinical form of the disease [15], meaning a risk factor for a disease with greater severity of motor symptoms [13], higher incidence of freezing [17], higher prevalence of autonomic symptoms, such as orthostatic hypotension [18], and the occurrence of early onset dementia [17]. In addition, a study showed a higher prevalence of men and older individuals in the RBD group [19]. Additional studies are needed to confirm the presence of those characteristics in that group of patients.
We, therefore, aim to describe the characteristics of RBD in a group of patients with PD, to find out the accuracy of the clinical interview for diagnosis of this parasomnia in those patients, as well as to verify the clinical and polysomnographic differences between the groups of PD patients with and without RBD.
Patients and methods
Study design and population
A cross-sectional study was performed in patients with PD from the tertiary outpatient clinic of Movement Disorders of the Hospital das Clínicas, Faculty of Medicine of Ribeirão Preto—University of São Paulo (HC-FMRP-USP), São Paulo, Brazil, during a 21-month period between February of 2010 and March of 2012.
In total, 124 consecutive individuals with PD were approached on the day of their usual consultation. Ninety of these individuals provided informed consent. Subsequently, the patients who agreed to participate underwent a clinical assessment with neurologists specialized in sleep medicine and movement disorders and with a psychiatrist. Two individuals did not attend the polysomnography (PSG). Patients underwent polysomnography with a maximum interval of 2 weeks after the initial assessment. During this time, there was no change in drug treatment.
This study was approved by the Ethics Committee of HC-FMRP-USP, under the protocol number 13410, in accordance with the ethical principles of the Declaration of Helsinki.
Clinical evaluation
Clinical evaluation was performed using standardized scales, and assessment of sleep disorders, cognitive framework, motor and psychiatric symptoms of PD.
The scales related to quality of life and sleep used were Epworth Sleepiness Scale (ESS), Parkinson’s Disease Questionnaire (PDQ-39), and Pittsburgh Sleep Quality Index (PSQI).
To detect and diagnose sleep disorders, including chronic insomnia, according to the International Classification of Sleep Disorders-third edition (ICSD-3), a clinical evaluation was performed by a neurologist specialized in sleep medicine [1, 4].
The assessment of functional impairment was performed by a neurologist specialized in movement disorders. The following scales were used: Unified Parkinson’s Disease Rating Scale (UPDRS)—part III, Hoehn & Yahr (H&Y) parkinsonian staging, and Schwab & England (S&E) activities of daily living score. For cognitive assessment, Mini-Mental State Examination (MMSE) and Global Deterioration Score (GDS) were used. For motor and cognitive assessment, patients were evaluated during the best “on” period as possible.
To achieve psychiatric diagnosis, such as anxiety, depressive and psychotic disorders, in accordance to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, of the American Psychiatric Association (DSM-IV), a structured clinical interview for Axis I mental disorders of the DSM-IV was used, in translated form and adapted to Portuguese (SCID-I) [20].
Polysomnography
Time-synchronized video-PSG (v-PSG) was performed with a digital polygraph (computerized sleep system; Biologic Sleepscan VISION PSG, Natus Bio-logic Systems Inc., San Carlos, CA). Data were collected using an electroencephalogram (EEG) (according to the International 10–20 System) (Fp1-M1, Fp2-M2, F3-M1, F4-M2, C3-M1, C4-M2, P3-M1, P4-M2, F7-M1, F8-M2, T3-M1, T4-M2, T5-M1, T6-M2, O1-M1, O2-M2, Fz-Cz, Cz-Pz), bilateral electrooculogram (E1-M2, E2-M1), electrocardiogram (modified V2 lead), and surface electromyography (EMG) of the mental and submental muscles. Surface electrodes were placed on both anterior tibialis, masseters, and extensors of fingers muscles. Digital video was recorded by an infrared camera (Sony Ipela., CA) synchronized with the PSG data. Respiration was monitored as follows: airflow was measured by a nasal pressure transducer system (AcSleep 119, Biolink Medical, São Paulo, Brazil) and nasal and mouth thermocouple airflow sensor (Pro-Tech Services Inc., Mukilteo, WA); chest and abdominal efforts were measured by respiratory inductive plethysmographic belts (Pro-Tech zRIP module, Pro-Tech Services Inc.); arterial SaO2 was measured by pulse oximetry (Netlink Headbox, Natus Bio-logic Systems Inc.); snoring sounds were measured using a snoring microphone; body position was determined using a sensor (Netlink Body Sensor Position, Natus Bio-logic Systems Inc.). All of the technical parameters used were performed in accordance with the AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specification [21]. According to these parameters, REM sleep without atonia was characterized defined by sustained muscle activity in REM sleep in the chin EMG and/or excessive transient muscle activity during REM sleep in the chin or limb EMG [21].
Statistical analysis
Kolmogorov–Smirnov test was used to determine the type of distribution of the variables. For variables with a normal distribution, parametric tests such as Student’s t test or analysis of variance (ANOVA) were used. Variables without a normal distribution were evaluated using nonparametric Mann–Whitney or Kruskal–Wallis test. Pearson’s coefficient was used in the correlation analysis of numeric variables with a normal distribution, and Spearman’s correlation coefficient, for the analysis of numerical variables without a normal distribution. The hypothesis tests were conducted to verify the nullity of the correlation coefficients. In the analysis of categorical variables into two or more groups, Chi square test or Fisher’s exact test was used, according to the expected frequency in cells. Linear regression analysis was used to calculate the predictive coefficients, for dependent quantitative variables. For the multiple correlation analysis, logistic regression analysis was used for binary categorical dependent variables. The software packages Microsoft Office Excel, IBM SPSS Statistics 19, and R 3.1.0 were used to construct and analyze the database.
Results
Diagnosis of RBD
A total of 55 participants presented RBD defined by clinical and polysomnographic evaluation, according to ICSD-3 criteria [4]. In 11 patients (12.5% of the total), the RBD diagnostic was not confirmed. There were also 6 individuals with REM sleep without atonia (6.8% of the total) without any report of dream enactment, and 16 patients (18.1%) who could not be categorized since they did not have any REM sleep or had just a very short REM sleep period during the polysomnography, although 13 of them had reported clinical complaints compatible with RBD. A total of 30 patients were using antidepressive medications at the moment of the polysomnography.
As a diagnostic tool, the clinical interview had sensitivity of 87.5%, specificity of 42.1%, positive predictive value of 81%, and negative predictive value of 53%. Among 55 individuals with RBD, 14 were defined by clinical symptoms associated with loss of atonia during REM sleep, 7 diagnosed exclusively by behavior and/or vocalization seen during the vPSG, therefore they did not present a clinical complaint, and 34 due to a clinical complaint of behavior and/or vocalization associated with loss of atonia and movement and/or vocalization during video polysomnography (Table 1).
Out of seven individuals who were diagnosed exclusively by polysomnography, two were used to sleeping alone, and four among the five subjects who referred to sleeping accompanied, attended the clinical interview with a companion who had not slept in their same room.
A total of five individuals presented symptoms suggestive of RBD but did not have polysomnographic confirmation, and their probable etiologies for dream enactment during sleep were a moderate or severe obstructive sleep apnea in four, whereas one individual had a diagnosis of sleep-related eating disorder.
Clinical characterization of RBD in the group of patients with Parkinson’s disease
Regarding the frequency of the behaviors, it was observed that in 28 individuals (50.9% of the patients with RBD) the symptoms occurred more than once a week. We also found that, in 14 subjects, the episodes occurred from once a week to once a month, while in 6 subjects, symptoms happened less than once a month. Seven subjects did not report any symptoms related to RBD and their diagnosis was made only by PSG.
Patients with RBD showed a mean symptom onset time of 9.58 years, with a standard deviation of 12.47 years. Out of the 55 subjects with RBD, 37 individuals (67.2%) had symptoms for 5 years or more, while 18 patients (32.5%) had symptoms for less than 5 years. Thirty patients reported an onset of symptoms related to RBD prior to the onset of PD (54.5% of subjects with RBD), while 18 (32.5%) reported the presence of symptoms related to RBD after onset of PD. Seven individuals reported no symptom of RBD.
Regarding the period of the night when symptoms occurred, 24 subjects pointed out the end of the sleep period, while 16 presented symptoms in the middle of the night, and 8 patients, in the begin of the sleep period (Table 2).
Fifty-one individuals reported that they had recalled dreams and/or nightmares (92.7% of this group). These dreams recalled was not restricted to enacted dreams. Twenty-seven patients (49% of this group) had experienced dreams and/or nightmares more than once a week, seventeen had have dreams frequently, between once a month and once a week, and seven had dreamed less than once a month.
Regarding the dream content, we observed a considerable proportion of the individuals reporting dreams in which they were being persecuted or attacked by animals (50.9%), 21 subjects (38.1%) reported being persecuted by another person, 27 (49%) claimed that they had dreamed about situations that made them feel sad, like death or illness of family members. Eleven individuals reported funny dreams and six reported dreaming that they were falling from a cliff.
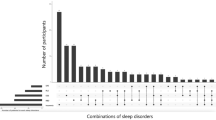
The main behaviors observed by roommates in the group of patients with RBD (n = 55) were: talking (71.4%), shouting (60.7%), laughing (42.9%), kicking (41.1%), punching (37.5%) and crying (32.1%) (Fig. 1). Most of individuals presented five different behaviors (Fig. 2).
We also observed among the individuals with a diagnosis of RBD (n = 55) that 25.4% informed having already injured their bedmates, and 20% reported having injured themselves during sleep episodes since the disease began. Among those individuals with a diagnosis of RBD, only six sought medical assistance for diagnosis and treatment.
Comparison between clinical and polysomnographic characteristics from individuals with RBD and PD and those with PD without RBD
We compared characteristics between PD patients who had a diagnosis of RBD established by ICSD-3 (n = 55) and PD patients that RBD diagnosis was definitively ruled out by vPSG (n = 11).
We observed a higher equivalent dose of levodopa in patients with PD and RBD, with a mean ± SD of 889.2 ± 426.8 mg as compared to non-RBD parkinsonians, whose mean ± SD dose was 490.9 ± 260.3 mg (p = 0.00). Patients with PD and RBD, however, did not present significant differences in mean age, schooling, time of onset of PD and BMI, in relation to the PD group without RBD (Table 3). Also, we did not find a difference in the proportion of males between the two groups evaluated (Table 3).
Mean scores on ESS, IQSP, PDQ-39, UDPRS part III, GDS, Hoehn and Yahr scale, and Schawb and England functional score scale were equivalent in the groups with and without RBD (Table 3).
Likewise, there were no differences in proportions in the subgroups evaluated with and without RBD in relation to the presence of chronic insomnia, OSAS, RLS, excessive fragmentary myoclonus, bruxism, ALMA/HFT, depression, psychotic disorder, anxiety disorder, dementia, hypersalivation, dysphagia, dyskinesia, nocturia, anosmia, excessive sweating and constipation (Table 3).
Regarding the polysomnographic variables, it was observed a tendency to lower arousal index in the subgroup of patients with RBD as compared to the group without RBD with average values ± SD of 21.7 ± 8.6 and 27.9 ± 14.8, respectively (p = 0.06). The other polysomnographic variables evaluated showed no significant differences in groups with and without RBD (Table 4).
Multivariate analysis of RBD
Multivariate analysis was used to evaluate the association between presence of RBD and the multiple variables involved in the study. For logistic regression analysis, we considered variables with p value < 0.1 in univariate analysis (equivalent dose of levodopa, arousal index, and Apnea-Hypopnea Index (AHI) in REM sleep). After an initial review of the independent variables cited above, those with higher p values were withdrawn gradually until the maintenance of only those with p < 0.05. Thus, the following independent variables were significant in the final model: equivalent dose of levodopa (estimated coefficient = 0.004; p = 0.01) e AHI in REM sleep (estimated coefficient = − 0.04; p = 0.01).
Discussion
In this paper we describe the clinical and polysomnographic characteristics of Parkinson’s disease patients with and without REM sleep behavior disorder. We have shown that patients with RBD have a higher equivalent dose of levodopa and a lower rate of respiratory disturb index during REM sleep. It is known that there is a greater tendency to respiratory events (apnea and hypopnea) in REM sleep due to a physiological and significant reduction in muscle tone, leading to a higher collapsibility of the upper airways, at this sleep phase [22]. Beside this, PD patients with RBD presented a lower AHI in REM sleep than PD patients without RBD. A possible explanation for lower AHI in REM sleep in PD individuals with RBD could be the maintenance of tonic and phasic activity during in REM sleep in RBD group, reducing the susceptibility to obstructive respiratory events.
In partial agreement with our findings, Huang et al. evaluated differences in polysomnographic variables during REM sleep in the groups of PD with and without RBD. They observed a decrease in oxygen saturation and duration of apnea in REM sleep in RBD group as compared to those without this disorder. This suggests that excessive muscle activity during REM sleep could protect patients from more intense respiratory events. Despite these findings, this study did not document a significant difference between AHI in REM sleep in the groups of individuals with and without RBD [23].
On the other hand, De Cock et al. observed that subjects without REM sleep atonia had higher AHI values in REM sleep than subjects with preservation of atonia [24]. The possible explanations for the divergence between those studies are different methods adopted in each works. De Cock et al. did not diagnose RBD, and the groups were divided into the presence or absence of atonia in REM sleep. In addition, no multivariate analysis was performed in this study.
Another important association is the higher equivalent dose of levodopa with the presence of RBD in PD patients. Since 2008, several studies have evaluated the relationship of RBD with various characteristics of PD [13, 17,18,19, 25,26,27,28,29,30]. Ferri et al., Sixel-Doring et al. and Nomura et al. had already demonstrated a difference in the equivalent dose of levodopa between the subgroups of PD patients with and without RBD [13, 17, 30], as in the present study. However, we cannot establish a causal relationship between equivalent dose of levodopa and RBD. Possible explanations for that association could be: (1) the presence of RBD may be associated with advanced PD, which requires a higher equivalent dose of levodopa, as demonstrated in Sixel-Doring et al. and Romenets et al. [13, 19]; or (2) individuals with RBD show reduced response to dopaminergic medications, requiring higher doses. We must consider the possibility that higher doses of dopaminergic medications are associated with the appearance of RBD symptoms.
We observed that 30 out of the 55 individuals (54.5%) reported symptoms compatible with RBD before the onset of motor symptoms, while 18 patients reported symptoms of RBD starting after the motor symptoms of PD. Ferri et al. showed the occurrence of RBD symptoms before the motor symptoms of PD in 37.5% of those diagnosed with RBD [30]. However, in that study, only 16 individuals with RBD were included. In another paper, De Cock et al. reported onset of RBD symptoms before PD symptoms in 22% of subjects, simultaneous onset in 23% and onset after PD symptoms in 55% of the individuals studied [31]. These data differ from our work and can be explained by the different methods employed. The study by De Cock et al. used PSG in only 51% of the individuals evaluated, while it was used in all patients in our study. These two studies cited above were cross-sectional and evaluated patients from a tertiary hospital, likewise ours. Therefore, it is important to consider that the determination of the onset of symptoms depends on the memory of the subjects assessed and the bed partners, which could vary from study to study.
This study also reinforces the need for the use of video-polysomnography, as described in ICSD-3, for the diagnostic confirmation of RBD. It is possible that the use of antidepressants could be the main reason for the high prevalence of insufficient proportion of REM sleep. Despite this, we observed that 7 individuals among the 55 included denied RBD symptoms during the clinical evaluation and were diagnosed exclusively by visualization of movement and/or vocalization during polysomnography. This could be justified by the fact that these subjects did not attend the interviews accompanied by the roommate, or that part of them used to sleep alone. In other words, polysomnography continues playing an essential role in the diagnosis of RBD, especially in patients who do not have companions sleeping in the same room. These data are in agreement with the study by Fraucher et al., in which the majority of individuals with RBD were diagnosed after a specific questionnaire and polysomnography [32].
In addition, five subjects who had presented RBD symptoms in clinical interview were diagnosed, after polysomnography, as having OSAS or Sleep-related eating disorder, which may explain the presence of complex movements during sleep. The relationship of OSAS with symptoms of dream-enactment had already been reported by Iranzo et al., whose work had demonstrated that clinical evaluation was not able to accurately differentiate OSAS from RBD, based only in clinical interview [33].
Most individuals reported a frequency of symptoms of more than once a week (50.9%), demonstrating the high variability of these symptoms in this group of patients. De Cock et al. documented that 33% of PD subjects had symptoms of acting more than once a week. On the other hand, Mahale et al. reported that 56.7% of the PD subjects had RBD symptoms of more than 6 times a month [34]. These data corroborate a high frequency of the symptoms of behaviors in subjects with PD.
A significant part of the individuals evaluated reported symptoms in the middle and final third of sleep (72.7%). This data, already reported by De Cock et al. and by Mahale et al., stems from the higher proportion of REM sleep in the middle and late thirds of the night [31, 34]. This may help, in the clinical evaluation, to differentiate from other conditions, such as NREM parasomnias, which more usually occur in the first third of the night [4].
The content of dreams presented by the patients was mainly related to persecution and/or attack by animals (50.9%), persecution by people (38.1%), and situations that caused sadness such as death or illness of relatives (49%). Bugalho et al. reported a higher frequency of dreams with aggressive and animal content in the PD group, comparing individuals with PD with those without this pathology, demonstrating a change in the content of dreams [35]. Among the pathophysiological mechanisms that could explain this change in PD, we could relate the treatment with dopaminergic medications as well as frontal dysfunction with less regulation of the limbic system during sleep [35, 36].
Regarding RBD manifestations, most individuals described vocalizations during sleep, such as talking, shouting and laughing [37]. A considerable proportion of the subjects presented aggressive behaviors with kicks (41.1%) and punches (37.5%), while 28.6% PD patients had fallen from bed. Mahale et al. documented talking in all subjects with RBD, while screaming was observed in 76.7% [34]. In turn, Oudiette et al. demonstrated that only 18% of subjects with PD presented nonviolent behaviors, such as laughing, singing, speaking, or whistling [38]. We believe that the observed variations between papers result from the difficulty in remembering and describing all the episodes, as well as from the fact that patients do not always have a witness to the behavior that occurred during sleep.
In the current study, 25.4% of patients reported having injured their roommate, and 20% had some injury due to sleep behavior. The high frequency of lesions to patients and their partners had already been described by Olson et al. in a series of RBD cases. In this study, it was observed a prevalence of 16% of injuries to the bed partner, and, 32% of self-injuries [39]. This paper however included in large part individuals with idiopathic RBD, differently from ours, that is exclusively composed by PD patients. In a study that included only individuals with PD, De Cock et al. reported injury to roommates in 34% of cases and 46% injury to the subject himself [31].
It would be expected that PD patients would have difficulty moving during both wakefulness and sleep. However, De Cock et al. reported individuals with PD presenting movements with better velocity and amplitude during an episode of RBD than the usual movements in wakefulness [31]. A possible explanation for this fact was that generation of the movements during sleep do not pass through the basal ganglia. They are probably commanded directly by motor area without the regulation of the sublaterodorsal nuclei and the magnocellular reticular formation [31, 40].
Despite the high rate of lesions reported in this study, it was observed that only 10.9% of the individuals with RBD sought medical assistance due to this complaint. This seems to have happened because many patients and caregivers believed that symptoms of dream enactment were a normal behavior during sleep, or because the individuals or companions fell embarrassed in reporting to others the aggressions suffered by the partner during sleep.
The present study had some limitations, such as the following: (1) it was carried out in a high-complexity outpatient hospital, therefore involving patients with greater disease severity and duration, which restricts the possibility of generalization of our data; (2) a moderate rate of participation, thus including those with greater interest in participating and who possibly presented problems during sleep; (3) the low number of patients included given the large number of variables considered in the analyzes; (4) the absence of a control group without PD, reducing the possibility of comparisons; (5) and the cross-sectional design of the study, making it difficult to establish cause and effect associations.
Finally, we wish to emphasize that, in PD patients, RBD have a great diversity of clinical manifestations and that this parasomnia are associated with low respiratory events during REM sleep. Beside this, in this group of patients RBD is related directly or indirectly with higher levodopa equivalent dose. So, we hope that in the near future, new controlled studies with larger numbers of PD patients to evaluate the RBD. Furthermore, in clinical care of patients with PD, we emphasize the importance of a systematic and comprehensive assessment of this parasomnia.
References
American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. American Academy of Sleep Medicine; 2005.
Iranzo A, Santamaria J, Tolosa E. The clinical and pathophysiological relevance of REM sleep behavior disorder in neurodegenerative diseases. Sleep Med Rev. 2009;13(6):385–401
Mahowald MW, Schenck CH. REM sleep parasomnias. In: Kryger M, Roth T, Dement W, editors. Principles and practice of sleep medicine. Philadelphia, PA: WB Saunders; 2005. p. 897–916.
American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Westchester: American Academy of Sleep Medicine; 2013.
Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14(8):744–8.
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M, et al. Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behavior disorder: an observational cohort study. Lancet Neurol. 2013;12(5):443–53.
Rye DB. Contributions of the pedunculopontine region to normal and altered REM sleep. Sleep. 1997;20(9):757–88.
Hendricks JC, Morrison AR, Mann GL. Different behaviors during paradoxical sleep without atonia depend on pontine lesion site. Brain Res. 1982;6(1):81–105. 239(.
Greene RW, Gerber U, McCarley RW. Cholinergic activation of medial pontine reticular formation neurons in vitro. Brain Res. 1989;476(1):154–9.
Boeve BF, Silber MH, Saper CB, Ferman TJ, Dickson DW, Parisi JE, et al. Pathophysiology of REM sleep behavior disorder and relevance to neurodegenerative disease. Brain. 2007;130(Pt 11):2770–88.
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197–211.
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K. Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res. 2004;318(1):121–34.
Sixel-Doring F, Trautmann E, Mollenhauer B, Trenkwalder C. Associated factors for REM sleep behavior disorder in Parkinson disease. Neurology. 2011;77(11):1048–54.
Nomura T, Inoue Y, Kagimura T, Uemura Y, Nakashima K. Utility of the REM sleep behavior disorder screening questionnaire (RBDSQ) in Parkinson’s disease patients. Sleep Med. 2011;12(7):711–3.
Comella CL, Nardine TM, Diederich NJ, Stebbins GT. Sleep-related violence, injury, and REM sleep behavior disorder in Parkinson’s disease. Neurology. 1998;51(2):526–9.
Sobreira-Neto MA, Pena-Pereira MA, Sobreira EST, Chagas MHN, Fernandes RMF, Tumas V, et al. High frequency of sleep disorders in Parkinson’s disease and its relationship with quality of life. Eur Neurol. 2017;78(5–6):330–7.
Nomura T, Inoue Y, Kagimura T, Nakashima K. Clinical significance of REM sleep behavior disorder in Parkinson’s disease. Sleep Med. 2013;14(2):131–5.
Postuma RB, Gagnon JF, Vendette M, Charland K, Montplaisir J. Manifestations of Parkinson disease differ in association with REM sleep behavior disorder. Mov Disord. 2008;23(12):1665–72.
Romenets SR, Gagnon JF, Latreille V, Panniset M, Chouinard S, Montplaisir J, et al. Rapid eye movement sleep behavior disorder and subtypes of Parkinson’s disease. Mov Disord. 2012;27(8):996–1003.
Del-Ben C, Vilela J, Crippa J, Hallak J, Labate C, Zuardi A. Test-retest reliability of the structured clinical interview for DSM-IV—clinical version (SCID-CV) translated into portuguese. Revista Brasileira de Psiquiatria. 2001;23:156–9.
Iber C, Ancoli-Israel S, Chesson AL, Quan SF. The AASM manual for scoring of sleep and associated events. 1st ed. Westchester: American Academy of Sleep Medicine; 2007.
Peregrim I, Gresova S, Pallayova M, Fulton BL, Stimmelova J, Bacova I, et al. Does obstructive sleep apnea worsen during REM sleep? Physiol Res (Academia Scientiarum Bohemoslovaca). 2013;62(5):569–75.
Huang J, Zhang J, Lam SP, Li SX, Ho CK, Lam V, et al. Amelioration of obstructive sleep apnea in REM sleep behavior disorder: implications for the neuromuscular control of OSA. Sleep. 2011;34(7):909–15.
Cochen De Cock V, Abouda M, Leu S, Oudiette D, Roze E, Vidailhet M, et al. Is obstructive sleep apnea a problem in Parkinson’s disease? Sleep Med. 2010;11(3):247–52.
Yoritaka A, Ohizumi H, Tanaka S, Hattori N. Parkinson’s disease with and without REM sleep behaviour disorder: are there any clinical differences? Eur Neurol. 2009;61(3):164–70.
Plomhause L, Dujardin K, Duhamel A, Delliaux M, Derambure P, Defebvre L, et al. Rapid eye movement sleep behavior disorder in treatment-naive Parkinson disease patients. Sleep Med. 2013;14(10):1035–7.
Suzuki K, Miyamoto T, Miyamoto M, Watanabe Y, Suzuki S, Tatsumoto M, et al. Probable rapid eye movement sleep behavior disorder, nocturnal disturbances and quality of life in patients with Parkinson’s disease: a case–controlled study using the rapid eye movement sleep behavior disorder screening questionnaire. BMC Neurol. 2013;13:18.
Rolinski M, Szewczyk-Krolikowski K, Tomlinson PR, Nithi K, Talbot K, Ben-Shlomo Y, et al. REM sleep behaviour disorder is associated with worse quality of life and other non-motor features in early Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2014;85(5):560–6.
Benninger DH, Michel J, Waldvogel D, Candia V, Poryazova R, van Hedel HJ, et al. REM sleep behavior disorder is not linked to postural instability and gait dysfunction in Parkinson. Mov Disord. 2010;25(11):1597–604.
Ferri R, Cosentino FI, Pizza F, Arico D, Plazzi G. The timing between REM sleep behavior disorder and Parkinson’s disease. Sleep Breath (Schlaf & Atmung). 2014;18(2):319–23.
De Cock VC, Vidailhet M, Leu S, Texeira A, Apartis E, Elbaz A, et al. Restoration of normal motor control in Parkinson’s disease during REM sleep. Brain. 2007;130(Pt 2):450–6.
Frauscher B, Gschliesser V, Brandauer E, Marti I, Furtner MT, Ulmer H, et al. REM sleep behavior disorder in 703 sleep-disorder patients: the importance of eliciting a comprehensive sleep history. Sleep Med. 2010;11(2):167–71.
Iranzo A, Santamaria J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005;28(2):203–6.
Mahale R, Yadav R, Pal PK. Rapid eye movement sleep behaviour disorder in young- and older-onset Parkinson disease: a questionnaire-based study. Sleep Med. 2014;15(6):642–6.
Bugalho P, Paiva T. Dream features in the early stages of Parkinson’s disease. J Neural Transm. 2011;118(11):1613–9.
Nausieda PA, Weiner WJ, Kaplan LR, Weber S, Klawans HL. Sleep disruption in the course of chronic levodopa therapy: an early feature of the levodopa psychosis. Clin Neuropharmacol. 1982;5(2):183–94.
Fernandez-Arcos A, Iranzo A, Serradell M, Gaig C, Santamaria J. The clinical phenotype of idiopathic rapid eye movement sleep behavior disorder at presentation: a study in 203 consecutive patients. Sleep. 2016;39(1):121–32.
Oudiette D, De Cock VC, Lavault S, Leu S, Vidailhet M, Arnulf I. Nonviolent elaborate behaviors may also occur in REM sleep behavior disorder. Neurology. 2009;72(6):551–7.
Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–9.
Dauvilliers Y, Boudousq V, Lopez R, Gabelle A, De Cock VC, Bayard S, et al. Increased perfusion in supplementary motor area during a REM sleep behaviour episode. Sleep Med. 2014;12(5):531–2.
Acknowledgements
We are grateful to the patients with PD whose collaboration was essential to the success of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Committee Permission
This study was approved by the Ethics Committee of Clinical Hospital of Faculty of Medicine of Ribeirão Preto—University of São Paulo, under the protocol number 13410.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Sobreira-Neto, M.A., Pena-Pereira, M.A., Sobreira, E.S.T. et al. REM sleep behavior disorder in patients with Parkinson’s disease: clinical and polysomnographic characteristics. Sleep Biol. Rhythms 17, 113–122 (2019). https://doi.org/10.1007/s41105-018-0189-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-018-0189-z