Abstract
Parkinson’s disease is a movement disorder whose principal symptoms are tremor, rigidity, bradykinesia and postural instability. Initially, drugs like l-dopa or dopaminergic agonists are able to control these symptoms, but with the progress of the disease these drugs become less effective. Previous studies have reported that repetitive transcranial magnetic stimulation (rTMS) can improve these motor symptoms. The objective of this study was to investigate the neural mechanisms through which 25 Hz rTMS may improve motor symptoms in Parkinson’s disease. In a double-blind placebo-controlled study, we evaluated the effects of 25 Hz. rTMS in 10 Parkinson’s disease patients. Fifteen rTMS sessions were performed over the primary cortex on both hemispheres (one after the other) during a 12-week period. The patients were studied using functional magnetic resonance imaging during performance of a simple tapping and a complex tapping task, 1 week before the administration of the first rTMS session and just after the last session. rTMS improved bradykinesia, while functional magnetic resonance imaging showed different cortical patterns in prefrontal cortex when patients performed the complex tapping test. Furthermore, the improvement in bradykinesia is associated with caudate nucleus activity increases in simple tapping. Finally, we observed a relative change in functional connectivity between the prefrontal areas and the supplementary motor area after rTMS. These results show a potential beneficial effect of repetitive transcranial magnetic stimulation on bradykinesia in Parkinson’s disease which is substantiated by neural changes observed in functional magnetic resonance imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a movement disorder arising from the loss of the dopamine (DA) neurons in the substantia nigra that project to striatum. Its main symptoms are tremor, rigidity, bradykinesia and postural instability. These symptoms are thought to arise as a result of the complex rearrangements occurring in the neuronal circuits responsible for motor activity which rely on the striatum. These are (1) hyperactivity of the subthalamic nucleus (STN) and globus pallidus (GP) [6, 12, 17], and (2) a change in firing rate and pattern in several of the basal ganglia nuclei [2, 7, 9, 42].
Initially, drugs such as l-dopa or dopaminergic agonists can control these symptoms, but as the disease progresses, their efficacy diminishes [46]. This requires increased doses which, in turn, can lead to important adverse side effects [53]. Therefore, new treatment approaches have been developed, such as chronic deep brain electrical stimulation (DBS), particularly in the STN and GP [36]. However, the complexity of the procedure, which requires the accurate placement of the electrodes in small deep brain nuclei currently restricts the use of high-frequency deep brain stimulation to a very limited number of patients [1, 28]. Moreover, gait and postural disturbances do not respond to DBS. An alternative target for chronic brain stimulation is the motor cortex. Indeed, the akinesia and rigidity in PD have been associated with abnormal motor cortex firing patterns and synchronization [25], while some studies have shown a direct involvement of the primary motor area M1 in the pathological firing patterns of STN and GP [38]. Finally, a recent study has found that STN-DBS reduced PD-like oscillations and symptoms through antidromic cortical activation [11]. Critically, because of its relatively large size and superficial location, M1 can be stimulated by less invasive methods, such as transcranial magnetic stimulation (TMS).
The application of repetitive TMS (rTMS) in PD was first described by Pascual-Leone and colleagues [47], who reported that sub-threshold, high-frequency (5 HZ) rTMS over M1 induced a significant improvement in reaction and movement times, as well as in the performance on the grooved pegboard test, in six PD patients. The benefits of rTMS were later confirmed by others groups [22, 34, 37, 39, 41, 54, 55]. However, other studies have failed to obtain a positive effect of rTMS in PD. For example, Ghabra and coworkers [23] failed to reproduce, in 11 PD patients, the rTMS results obtained by the original group even though they employed nearly identical methods and parameters. Negative results also were obtained by Tergau and colleagues [62] who studied seven patients before and after exposure to 500 stimuli delivered at four different frequencies (1–20 Hz) in separate experimental sessions. Although some of the inconsistencies in the findings among studies could be due to the specific experimental design employed [55], these conflicting results generated some skepticism about the potential therapeutic usefulness of rTMS. Identifying the neural circuits modulated by rTMS, beyond those directly affected by the stimulation (i.e., M1), and how they relate to symptom improvement in PD could help resolve the inconsistency in the previous studies.
Functional neuroimaging, in particular fMRI, provides an ideally suited technique to investigate the neural mechanisms underlying the possible therapeutic effects of rTMS in PD. Indeed, TMS has been used in conjunction with neuroimaging techniques such a PET [20, 48, 57, 58] SPECT [13, 45] and fMRI [3–5] to explore changes in functional connectivity in various brain networks. These neuroimaging studies have shown that stimulation of a single cortical focus can lead to alterations in several different cortical and subcortical regions of a long-range, distributed network. However, to the best of our knowledge, the combination of fMRI and TMS has not been specifically employed to study PD. Thus, the objective of this study was to investigate through fMRI the possible neural mechanisms by which rTMS may improve motor symptoms in PD. To do so, we conducted a longitudinal study in which patients underwent were scanned before and after a 3-month-long rTMS treatment.
Materials and methods
Subjects
Seventeen patients, predominantly with the akinetic rigid form of idiopathic PD (Hoen and Yahr 2–3 while off) according to the diagnostic criteria of the UK Parkinson’s Disease Society Brain Bank [24], participated in the study. Clinical details of the patients, including type and dose of medication are shown in Table 1. Ten patients were assigned to the experimental patient (EP) group and the other seven (patients 11–17 in Table 1) to the control patient (CP) group (see below). Patients were not aware of the specifics of the experimental design. In addition, ten healthy volunteers, matched in sex and age to the EP group, were included as a healthy control (HC) group in the fMRI study. The study obtained the approval of the ethics committee of the Hospital General de Mexico. Written informed consent was obtained from all participants.
Procedure
The overall experimental procedure consisted of two fMRI sessions, before and after a 3-month rTMS treatment. A schematic of the various stages and their timing is shown in Fig. 1, with their details described below.
Experimental design (day1) baseline evaluation was performed 1 week before rTMS session (scan and UPDRS). (Day 8–12, 39–43 and 70–74) The patients received a rTMS session for 5 day continued, 15 min after each session the participants were evaluated with tapping and random sequence, the rest periods inter-rTMS session were 3 weeks. (Day 74) the post-TMS assessment was performed 30 min after the last rTMS session (scan and UPDRS). During scan acquisition the subjects performed two motor tasks in a blocked design, evaluated with UPDRS
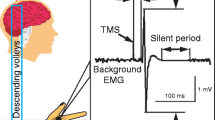
Transcranial magnetic stimulation
The ten patients of the EP group received ten trains of 100 pulses of rTMS at 25 Hz over the motor cortex (M1) at 80% of the resting motor threshold (RMT), determined as the lowest intensity capable of producing motor evoked potentials (MEPs) in the right APB (abductor pollicis brevis muscle). Patients in the CP group received 1,000 pulses (10 Hz) of rTMS over the occipital lobe of both hemispheres [34] at 50% of RMT. In all cases, rTMS was administered to both hemispheres (first right and then left), using the Rapid2 Magstim magnetic stimulator (Magstim Co., Whitland, Carmathenshire, Wales) equipped with an eight-shape coil. A total of 15 such sessions were conducted, five times on the first week of each month for 3 months at the same hour of the day every 24 h. The protocol was based on previous studies showing that bilateral high intensity and frequency rTMS for at least 5 days produces long lasting and potent effect on motor performance [37]. Patients received the stimulation 60 min after they had taken their usual medication. Participants from the HC group did not receive any rTMS treatment.
Motor evaluations
Motor evaluations were performed in sequential order (tapping first) 15 min after each rTMS session:
Tapping
Patients were seated in front of a panel containing three buttons. The central button was yellow and the left and right buttons were green. They were instructed to press first the central yellow button as soon as they heard a beep and immediately afterwards to press the right green button with the right hand until a second beep was presented. They repeated the task using their left hand (and left button). The interval between beeps was 1 min [43]. The number of alternative taps within this minute was measured for each hand for each subject.
Random sequence
The apparatus and initial procedure were similar to the tapping task but this time the movement to the right or left button depended on the auditory stimulus. Specifically, patients were asked to press the central yellow button upon hearing a beep, but to only release it and press either the left or right button depending on whether they heard one or two beeps. One beep indicated that they had to press the right button with the right hand and two beeps indicated that they had to press the left button with the same hand. Thirty trials were administered for each hand. The presentation of the one- and two-beep signals was random.
We measured reaction time (the elapsed time between hearing the second auditory signal and the release the central button), and movement time (the elapsed time from the releasing the central button and pressing the corresponding lateral button). The number of successful attempts and errors was also measured.
Analysis of reaction and movement times for both tasks was conducted through an ANOVA with treatment (EP vs. CP) as the between-group factor and session as the within-subject repeated-measures variable.
Clinical evaluation
A neurologist blind to the procedure evaluated the patients using the Unified Parkinson’s disease rating scale (UPDRS) [16] twice, at the beginning and the end of the study.
fMRI acquisition and analysis
fMRI acquisition was performed on 1.5 Tesla General Electric HDx system equipped with standard head coil, using gradient EPI sequences. A vacuum cushion was used to stabilize the participants’ head. During data acquisition the subjects performed two motor tasks in a blocked design: a paced index finger test which involved pressing a button at fixed time intervals of 1,000 ms following an auditory signal (100-ms, 440 Hz pure tone), referred here as the simple task, and a second, more demanding test (the complex task) which involved pressing one button upon hearing a given cue (1 tone) and pressing another button upon hearing a different cue (2 successive tones separated by 100 ms). In this task, the inter-stimulus interval varied randomly between 850 and 1,500 ms. Reaction times for both tapping tasks and correct responses in the complex tapping tasks were measured. In addition, two types of rest blocks were interleaved with the motor tasks. These rest blocks were identical to the simple or complex tapping ones, but subjects were instructed to only listen to the sounds without responding (simple rest, SR and complex rest, CR, respectively). Preceding each block an auditory instruction was given to indicate the type of task (movement/rest). In total, there were eight blocks in the following fixed order: CR, ST, SR, CT, SR, ST, CR, CT. Patients were trained prior to scanning until they reached an accuracy level of 75–80%. Patients in the CP and EP groups were scanned 1 week before the first rTMS session and again 1 h after the last rTMS session. Participants from the HC group were scanned once.
Stimuli were generated by a PC laptop computer running E-PRIME (Psychology Software Tools, Pittsburg, PA, USA) and were delivered to the subject binaurally via headphones using an MR-compatible pneumatic system. An optical mouse connected to the computer collected the participant’s responses.
Functional T2* weighted images were collected with blood oxygen level dependent (bold) contrast (120 volumes, TR = 3,000 ms, TE = 40 ms, flip angle = 90°, FOV = 256 mm2, Matrix 64 × 64), covering the entire brain (34 interleaved slices, 4 mm thickness, parallel to the anterior–posterior commissural plane; voxel size 4 × 4 × 4 mm3). Prior to the functional scan a T1-weighted anatomical volume was acquired using a gradient echo pulse sequence (TR = 10.2 ms, TE = 4.2 ms, flip angle = 90°, voxel size 1 × 1 × 1 mm3).
Functional data was pre-processed using SPM2 (Wellcome Department of Cognitive Neurology, London, UK; see http://www.fil.ion.ucl.ac.uk/spm), following standard procedure. Briefly, images were realigned to the first volume, spatially normalized (final voxel size 2 × 2 × 2 mm3) to the stereotaxic space of Talairach and Tournoux [63] using the MNI template [15] and smoothed using an isotropic 8 mm FWHM Gaussian kernel. A high-pass filter (cutoff 128 s) was applied to remove low frequency temporal drifts in fMRI signal. Data were analyzed with SPM2 using general linear model with a synthetic hemodynamic response function. Four conditions were defined based on the task: simple and complex tapping, and simple and complex rest. The movement parameters obtained during preprocessing were also included in the model (realignment procedure). For each participant, two linear contrasts of interest were calculated, corresponding to the effects of simple and complex tapping minus their corresponding controls (i.e., simple tapping–simple rest and complex tapping–complex rest). Each of these linear contrasts was taken to second level random-effects model using whole brain analysis, namely, a two-sample t test contrasting all patients before rTMS treatment versus the HC group and a paired t test for the EP groups comparing activity before and after treatment. A threshold of p < 0.001, uncorrected for multiple comparisons, together with a cluster threshold of p < 0.05 was used to determine statistical significance.
In addition, to assess the specificity of any changes in brain activity in the EP to rTMS over M1, a mixed two-factor ANOVA (Pre- vs. Post-rTMS and EP vs. CP groups) for the CP group (rTMS over occipital cortex) was conducted. For this analysis, statistical significance was determined using a threshold of p < 0.05 corrected for multiple comparisons (FWER [64]) within the volume defined by the activations obtained in the same analysis for the EP group.
Finally, a psychophysiological interaction (PPI) analysis [21] was conducted to explore functional connectivity changes with SMA during the complex tapping task as a function of treatment. The time series for SMA was extracted from the first eigentime series of all voxels within 5 mm radius sphere centered on the regional maxima in the SMA that showed significant activation in the complex tapping minus complex rest contrast (see “Results”).
Results
Motor performance
Results from the tapping test in Fig. 2 showed that, after treatment, the number of button presses for the EP group was significantly greater than for the CP group for both right and left hands [F(3,87) = 11.1, p < 0.001 and F(3,87) = 7.58, p = 0.005, respectively]. Similarly, in the random sequence test, movement time diminished in the EP group when compared to the CP group for right and left hands [F(3,87) = 59.5, p < 0.001 and F(3,87) = 82.5, p < 0.001, respectively). Figure 3 shows movement time in the random sequence test (right hand) in both groups as a function of rTMS session. As can be seen, improvement in the EP group occurred after a few sessions and it was maintained throughout the treatment. We also observed a trend for a reduction in reaction times for the EP group when using the right hand (p = 0.07), but no differences for the left hand (p = 0.6).
Movement time after each of the repetitive transcranial magnetic stimulation (rTMS) sessions (mean and SE) for the experimental (square) and control (triangle) patients groups. The x axis indicates the time, in days, after the start of treatment. Measurements for left and right hands were pooled. a right hand b left hand
Number of tappings each of the repetitive transcranial magnetic stimulation (rTMS) sessions (mean and SE) for the experimental (square) and control (triangle) patients groups. The x axis indicates the time, in days, after the start of treatment. Measurements for left and right hands were pooled. a right hand b left hand
Symptom changes
Prior to treatment, no significant differences existed between the EP and CP groups in the clinical evaluation of symptoms, measured with the UPDRS (p = 0.7). Following rTMS, the EP showed significant improvement (pre-rTMS: 40.2, post-rTMS: 32.7, p = 0.03), whereas no significant changes were observed in the CP group (pre-rTMS: 41.8, post-rTMS: 41.0, p = 0.19).
Motor tasks in the scanner
No significant changes in accuracy during the complex tapping task in the scanner were observed between sessions for either the EP (pre-rTMS: 78%; post-rTMS: 84%; p = 0.34) or the CP group (pre-rTMS: 78%; post-rTMS: 71%; p = 0.7). Likewise, reaction times in both tasks were similar before (EP: 520 ± 72 ms; CP: 523 ± 68 ms; p = 0.82) and after rTMS (EP: 520 ± 68 ms; CP: 516 ± 86 ms; p = 0.9). As expected, participants in the HC group were more accurate than the patients (95%; p = 0.001), but there were no differences in RTs (495 ± 67 ms; p > 0.4) (see Table 2).
fMRI data
Patients versus HCs
Tables 3, 4 and Fig. 4 show the significant activations for the comparison between all 17 patients before rTMS and HCs during the simple and complex tapping task, respectively. Overall, patients exhibited reduced activation in the thalamus, caudate and putamen, as well as parietal cortex. In addition, controls showed stronger activation in the midbrain for the simple task and premotor cortex in the complex task. Patients only exhibited stronger activation in the right DLPFC during the simple tapping task.
Activation for simple and complex tapping. a Statistical parametric map (color scale represents t values), for the contrast simple tapping minus simple rest, showing areas with stronger signal in HCs and b for contrast in complex tapping-complex rest showing areas with stronger signal in HCs (p < 0.001)
Pre- versus post-rTMS
In the EP group, rTMS treatment led to an increase in activation in several regions, mostly in the left hemisphere, including the caudate nucleus (CN), superior parietal gyrus, M1 and dorsal premotor cortex, for the simple task, cerebellum and DLPFC for the complex task. In contrast, activity in left S1 decreased following rTMS treatment in the case of the simple task. Critically, there was a reduction in SMA activity during the complex task. The complete list of activations for both tasks as a result of treatment is shown in Tables 5, 6 and Fig. 5.
To assess whether the observed fMRI results were specific to rTMS over M1, we conducted an ANOVA comparing the EP (rTMS over M1) with the CP group (rTMS over occipital cortex) for the two tasks before and after treatment. Results from the interaction analysis (group-by-session) for the simple tapping task revealed a significant activation in the CN (xyz = [−22, −18, 26], z = 4.07, p unc < 0.0001, p FWE < 0.05 SVC) and, for the complex task, in the SMA (xyz = [−10, −2, 50], z = 2.6, p unc = 0.005, p FWE < 0.05 SVC). As seen in the graphs of the parameter estimates in Figs. 6 and 7, these analyses confirmed that the observed increase in the CN and decrease in SMA after treatment was specific to the experimental group, as no significant differences were observed in the CP patients (CN: p = 0.12, SMA: p = 0.48).
a Statistical parametric map (color scale represents t values) of the group-by-time interaction for the simple-tapping minus simple-rest contrast showing that the change in activation following rTMS differed between the experimental (EP) and control (CP) patients groups in the CN. b Parameter estimates of this contrast in the peak voxel of the CN activation (xyz = [−22, −18, 26], z = 4.07, p < 0.05 FWE) for the b EP group and c CP group before and after rTMS. (bold responses are reported in arbitrary units)
a Statistical parametric map (color scale represents t values) of the group-by-time interaction for the complex–tapping – complex–rest contrast showing that the change in activation following rTMS differed between the experimental (EP) and control (CP) patients groups in SMA. b Parameter estimates of this contrast in the peak voxel of SMA (xyz = [−10, −2, 50], z = 2.6, p < 0.05 FWE) for the b EP group and c CP group before and after rTMS. (bold responses are reported in arbitrary units)
To further explore the changes in SMA activity following rTMS treatment in the EP group, we conducted a functional PPI analysis using the peak activation of SMA as the seed voxel (see “Materials and methods”). Functional connectivity between SMA and prefrontal cortex during complex tapping significantly increased after rTMS shown in Fig. 8 and Table 7.
Discussion
In this study, we investigated the clinical, behavioral and neural effects of long-term application of rTMS over primary motor cortex on PD. We observed that fifteen sessions of rTMS, over the course of a 3-month period, significantly improved bradykinesia, in agreement with previous studies, [22, 34, 37, 47, 56]. Before treatment, patients exhibited the typical pattern of reduced activation in the basal ganglia during motor tasks [30, 32], as well as in other cortical regions, particularly the parietal cortex [26, 51]. After the 3-month treatment, patients who had rTMS over M1 showed a significant increase in activation in the CN, as well as a reduction in activity in SMA when performing a complex motor task. Interestingly, this decreased activation was associated with a stronger effective connectivity of this region with the medial prefrontal cortex. Critically, these effects, both at the behavioral and neural level, were specific to M1 rTMS, as a group of patients undergoing the same treatment but with the TMS coil placed over the occipital cortex did not show any of the changes in behavior or brain activity mentioned above. Below, we discuss these findings in more detail.
Motor behavior
We showed that rTMS over M1 improved motor performance. However, unlike some of the previous studies [34, 37], we did not see a cumulative effect over time. Instead, performance in the motor tasks was already significantly better after the first rTMS session but did not improve further with more sessions. Nonetheless, we did observe that after a month without treatment, performance decreased, albeit not to the pre-treatment levels (see Fig. 2), suggesting that periodic boost sessions of rTMS may be necessary for long-term maintenance of its effects of motor behavior. We observed a delayed effect of rTMS on the right hand’s movement, similar to what has been previously reported in PD and post-stroke patients [40].
Caudate nucleus
Most neuroimaging studies, including ours, in PD that employed simple motor tasks to investigate bradykinesia-related neural activity found significantly decreased activation in the CN, among other regions [26, 30, 31, 51]. It has been suggested that this CN hypoactivity contributes to the observed motor deficits in PD patients, particularly those requiring an external cue for initiation [49], by interfering with the normal functioning of the striato-frontal motor loop. Consistent with this model, we observed that rTMS over M1 significantly improved motor behavior and resulted in increased motor-related activity in the CN.
The mechanism linking rTMS over M1 and activity in CN remain be determined. However, we can speculate about possible ways in which this could be affected. Recent studies have shown direct evidence, using PET, of DA release in the striatum in healthy subjects, PD patients and monkeys after rTMS over dorsolateral prefrontal cortex and motor cortex [59–61], which, in turn, could lead to increases in blood oxygen-level dependent (BOLD) signal [35]. Another possibility is that rTMS causes changes in CN activity indirectly, through its action on other brain regions, such as SMA (see below). Indeed, functional MRI and computational modeling studies [29] suggest that the striatum and pre-SMA are functionally linked, particularly during tasks that required speeded, cue-based, simple decision-making [19]. Furthermore, a recent study has shown that structural connectivity between pre-SMA and the striatum can account for some of the observed individual differences in behavioral performance during simple cognitive tasks [18]. It is therefore possible that improvement in motor performance in our patients was also associated with structural, rather than functional, changes in this network. Future analyses using structural data could potentially test this hypothesis.
Supplementary motor area
SMA has been consistently implicated in PD and many neuroimaging studies have shown underactivity of the SMA in PD during movement [8, 26, 31, 52]. However, several other studies have shown the opposite, namely stronger SMA activity in PD patients compared to controls [10, 14, 30, 50, 51]. In our study, we did not observe differences in SMA activity between controls and patients before rTMS treatment. Nonetheless, we found a reduction in SMA activity after rTMS application over motor cortex. This finding is in agreement with previous studies showing that deep brain stimulation of the STN in PD patients resulted in an improvement in symptoms and a decrease in cerebral blood flow in SMA [27, 33]. Interestingly, in our study, this reduction in SMA activity after rTMS was associated with an enhanced effective connectivity of this area with prefrontal cortex during the complex motor task. Taken together, these findings could be interpreted as rTMS improving the efficiency of SMA during the performance of complex motor tasks by reducing its activity and increasing its connectivity to other regions involved in the “attention-to-action” circuit [44]. Consistent with this hypothesis, Rowe and colleagues [50] observed that, although SMA activity during a simple motor task was higher in PD patients than controls, increasing the attentional load of the task failed to modulate SMA activity or increase its effective connectivity with prefrontal cortex, as it was the case with control subjects.
Specificity of the effects
Our results show that repeated sessions of rTMS over primary motor cortex resulted in significant changes in behavior and brain activity in PD patients. However, it could be theoretically possible that at least some of these changes were due to a placebo or other non-specific effect of TMS. Indeed, Strafella et al. [59] showed that sham rTMS increased DA neurotransmission in dorsal and ventral striatum. To rule out this possible placebo effect in our study, we included a group of CPs, matched to the experimental group in terms of symptom severity, who underwent actual (non-sham) rTMS treatment but with the coil placed over the occipital cortex. Critically, these patients did not exhibit any clinical symptom or motor behavior improvement nor did they show the changes in brain activity, particularly in CN and SMA, observed in the experimental group. Nonetheless, we cannot rule out that rTMS over another location, more related to the motor or attention network (e.g., parietal cortex or SMA) could have similar effects to those we observed. Furthermore, our rTMS protocol was chosen so as to maximize the probability of having positive effects on motor performance; future studies varying some of the parameters, such as frequency, duration, number of sessions, will be necessary to fully characterize the influence of rTMS on symptom improvement in PD.
Limitations
One limitation of our study is the relatively small number of patients tested. However, our sample size is similar to most previous PD studies [26, 30, 50, 51]. Furthermore, the within-subject design employed here has substantially higher statistical power than a cross-sectional one using the same number of patients. Because we only scanned patients after 3 months of rTMS, we were not able to determine the time course of neural changes or the minimum number of sessions necessary to effect these changes. Similarly, repeated follow-up behavioral and fMRI tests would be needed to assess the long-term effects of rTMS treatment and the role of medication on symptom and motor performance improvement which will be the focus of future studies.
Conclusion
In conclusion, the present study extends previous findings on the beneficial effects of rTMS on motor behavior in PD and sheds light on the possible neural mechanisms underlying this improvement. Specifically, we showed that rTMS induced increases in activity in the CN during a simple motor task and decreased SMA activity, coupled with enhanced functional connectivity with prefrontal areas. Taken together, these results further highlight the potential therapeutic effects of rTMS, especially in combination with other treatment approaches in PD.
References
Bejjani BP, Damier P, Arnulf I, Thivard L, Bonnet AM, Dormont D, Cornu P, Pidoux B, Samson Y, Agid Y (1999) Transient acute depression induced by high-frequency deep-brain stimulation. N Engl J Med 340:1476–1480
Bergman H, Feingold A, Nini A, Raz A, Slovin H, Abeles M, Vaadia E (1998) Physiological aspects of information processing in the basal ganglia of normal and parkinsonian primates. Trends Neurosci 21:32–38
Bestmann S, Baudewig J, Siebner HR, Rothwell JC, Frahm J (2003) Subthreshold high-frequency TMS of human primary motor cortex modulates interconnected frontal motor areas as detected by interleaved fMRI-TMS. Neuroimage 20:1685–1696
Bohning DE, Shastri A, McConnell KA, Nahas Z, Lorberbaum JP, Roberts DR, Teneback C, Vincent DJ, George MS (1999) A combined TMS/fMRI study of intensity-dependent TMS over motor cortex. Biol Psychiatry 45:385–394
Bohning DE, Shastri A, Nahas Z, Lorberbaum JP, Andersen SW, Dannels WR, Haxthausen EU, Vincent DJ, George MS (1998) Echoplanar BOLD fMRI of brain activation induced by concurrent transcranial magnetic stimulation. Invest Radiol 33:336–340
Boraud T, Bezard E, Guehl D, Bioulac B, Gross C (1998) Effects of L-DOPA on neuronal activity of the globus pallidus externalis (GPe) and globus pallidus internalis (GPi) in the MPTP-treated monkey. Brain Res 787:157–160
Brown P (2003) Oscillatory nature of human basal ganglia activity: relationship to the pathophysiology of Parkinson’s disease. Mov Disord 18:357–363
Buhmann C, Glauche V, Sturenburg HJ, Oechsner M, Weiller C, Buchel C (2003) Pharmacologically modulated Fmri-cortical responsiveness to levodopa in drug-naive hemiparkinsonian patients. Brain 126:451–461
Carrillo-Reid L, Tecuapetla F, Tapia D, Hernandez-Cruz A, Galarraga E, Drucker-Colin R, Bargas J (2008) Encoding network states by striatal cell assemblies. J Neurophysiol 99:1435–1450
Catalan MJ, Ishii K, Honda M, Samii A, Hallett M (1999) A PET study of sequential finger movements of varying length in patients with Parkinson’s disease. Brain 122(Pt 3):483–495
Dejean C, Hyland B, Arbuthnott G (2009) Cortical effects of subthalamic stimulation correlate with behavioral recovery from dopamine antagonist induced akinesia. Cereb Cortex 19:1055–1063
DeLong MR (1990) Primate models of movement disorders of basal ganglia origin. Trends Neurosci 13:281–285
Dressler D, Voth E, Feldmann M, Benecke R (1990) Safety aspects of transcranial brain stimulation in man tested by single photon emission-computed tomography. Neurosci Lett 119:153–155
Eckert T, Peschel T, Heinze HJ, Rotte M (2006) Increased pre-SMA activation in early PD patients during simple self-initiated hand movements. J Neurol 253:199–207
Evans MK, Collins D, McDonald D (1994) Magnetic resonance scanning and epilepsy Plenum, New York
Fahn S, Elton R, Members of the UPDRS Development Committee. The Unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M (eds) (1987) Recent Developments in Parkinson’s Disease
Filion M, Tremblay L (1991) Abnormal spontaneous activity of globus pallidus neurons in monkeys with MPTP-induced parkinsonism. Brain Res 547:142–151
Forstmann BU, Anwander A, Schafer A, Neumann J, Brown S, Wagenmakers EJ, Bogacz R, Turner R (2010) Cortico-striatal connections predict control over speed and accuracy in perceptual decision making. Proc Natl Acad Sci USA 107:15916–15920
Forstmann BU, Dutilh G, Brown S, Neumann J, von Cramon DY, Ridderinkhof KR, Wagenmakers EJ (2008) Striatum and pre-SMA facilitate decision-making under time pressure. Proc Natl Acad Sci USA 105:17538–17542
Fox P, Ingham R, George MS, Mayberg H, Ingham J, Roby J, Martin C, Jerabek P (1997) Imaging human intra-cerebral connectivity by PET during TMS. Neuroreport 8:2787–2791
Friston KJ, Buechel C, Fink GR, Morris J, Rolls E, Dolan RJ (1997) Psychophysiological and modulatory interactions in neuroimaging. Neuroimage 6:218–229
Fukudome T, Goto H, Izumoto H, Matsuo H, Shibuya N (2002) The effects of repetitive transcranial magnetic stimulation (rTMS) in the patients with Parkinson’s disease. Rinsho Shinkeigaku 42:35–37
Ghabra MB, Hallett M, Wassermann EM (1999) Simultaneous repetitive transcranial magnetic stimulation does not speed fine movement in PD. Neurology 52:768–770
Gibb WR, Lees AJ (1988) The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J Neurol Neurosurg Psychiatry 51:745–752
Goldberg JA, Boraud T, Maraton S, Haber SN, Vaadia E, Bergman H (2002) Enhanced synchrony among primary motor cortex neurons in the 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine primate model of Parkinson’s disease. J Neurosci 22:4639–4653
Haslinger B, Erhard P, Kampfe N, Boecker H, Rummeny E, Schwaiger M, Conrad B, Ceballos-Baumann AO (2001) Event-related functional magnetic resonance imaging in Parkinson’s disease before and after levodopa. Brain 124:558–570
Hershey T, Revilla FJ, Wernle AR, McGee-Minnich L, Antenor JV, Videen TO, Dowling JL, Mink JW, Perlmutter JS (2003) Cortical and subcortical blood flow effects of subthalamic nucleus stimulation in PD. Neurology 61:816–821
Houeto JL, Mesnage V, Mallet L, Pillon B, Gargiulo M, du Moncel ST, Bonnet AM, Pidoux B, Dormont D, Cornu P, Agid Y (2002) Behavioural disorders, Parkinson’s disease and subthalamic stimulation. J Neurol Neurosurg Psychiatry 72:701–707
Ivanoff J, Branning P, Marois R (2008) fMRI evidence for a dual process account of the speed-accuracy tradeoff in decision-making. PLoS One 3:e2635
Jahanshahi M, Jones CR, Zijlmans J, Katzenschlager R, Lee L, Quinn N, Frith CD, Lees AJ (2010) Dopaminergic modulation of striato-frontal connectivity during motor timing in Parkinson’s disease. Brain 133:727–745
Jenkins IH, Fernandez W, Playford ED, Lees AJ, Frackowiak RS, Passingham RE, Brooks DJ (1992) Impaired activation of the supplementary motor area in Parkinson’s disease is reversed when akinesia is treated with apomorphine. Ann Neurol 32:749–757
Jenkins IH, Jahanshahi M, Jueptner M, Passingham RE, Brooks DJ (2000) Self-initiated versus externally triggered movements. II. The effect of movement predictability on regional cerebral blood flow. Brain 123(Pt 6):1216–1228
Karimi M, Golchin N, Tabbal SD, Hershey T, Videen TO, Wu J, Usche JW, Revilla FJ, Hartlein JM, Wernle AR, Mink JW, Perlmutter JS (2008) Subthalamic nucleus stimulation-induced regional blood flow responses correlate with improvement of motor signs in Parkinson disease. Brain 131:2710–2719
Khedr EM, Rothwell JC, Shawky OA, Ahmed MA, Hamdy A (2006) Effect of daily repetitive transcranial magnetic stimulation on motor performance in Parkinson’s disease. Mov Disord 21:2201–2205
Knutson B, Gibbs SE (2007) Linking nucleus accumbens dopamine and blood oxygenation. Psychopharmacology (Berl) 191:813–822
Limousin P, Pollak P, Benazzouz A, Hoffmann D, Le Bas JF, Broussolle E, Perret JE, Benabid AL (1995) Effect of parkinsonian signs and symptoms of bilateral subthalamic nucleus stimulation. Lancet 345:91–95
Lomarev MP, Kanchana S, Bara-Jimenez W, Iyer M, Wassermann EM, Hallett M (2006) Placebo-controlled study of rTMS for the treatment of Parkinson’s disease. Mov Disord 21:325–331
Magill PJ, Bolam JP, Bevan MD (2001) Dopamine regulates the impact of the cerebral cortex on the subthalamic nucleus-globus pallidus network. Neuroscience 106:313–330
Mally J, Farkas R, Tothfalusi L, Stone TW (2004) Long-term follow-up study with repetitive transcranial magnetic stimulation (rTMS) in Parkinson’s disease. Brain Res Bull 64:259–263
Mally J, Stone TW (2007) New advances in the rehabilitation of CNS diseases applying rTMS. Expert Rev Neurother 7:165–177
Mally J, Stone TW (1999) Therapeutic and “dose-dependent” effect of repetitive microelectroshock induced by transcranial magnetic stimulation in Parkinson’s disease. J Neurosci Res 57:935–940
Marsden JF, Limousin-Dowsey P, Ashby P, Pollak P, Brown P (2001) Subthalamic nucleus, sensorimotor cortex and muscle interrelationships in Parkinson’s disease. Brain 124:378–388
Martilla UKRaRJ (1977) Disability and progression in Parkinson’s disease. Acta Neurol Scand 56:159–169
Miller EK (1999) The prefrontal cortex: complex neural properties for complex behavior. Neuron 22:15–17
Okabe S, Hanajima R, Ohnishi T, Nishikawa M, Imabayashi E, Takano H, Kawachi T, Matsuda H, Shiio Y, Iwata NK, Furubayashi T, Terao Y, Ugawa Y (2003) Functional connectivity revealed by single-photon emission computed tomography (SPECT) during repetitive transcranial magnetic stimulation (rTMS) of the motor cortex. Clin Neurophysiol 114:450–457
Olanow CW, Watts RL, Koller WC (2001) An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology 56:S1–S88
Pascual-Leone A, Valls-Sole J, Brasil-Neto JP, Cammarota A, Grafman J, Hallett M (1994) Akinesia in Parkinson’s disease. II. Effects of subthreshold repetitive transcranial motor cortex stimulation. Neurology 44:892–898
Paus T, Jech R, Thompson CJ, Comeau R, Peters T, Evans AC (1997) Transcranial magnetic stimulation during positron emission tomography: a new method for studying connectivity of the human cerebral cortex. J Neurosci 17:3178–3184
Rolls ET, Thorpe SJ, Maddison SP (1983) Responses of striatal neurons in the behaving monkey. 1. Head of the caudate nucleus. Behav Brain Res 7:179–210
Rowe J, Stephan KE, Friston K, Frackowiak R, Lees A, Passingham R (2002) Attention to action in Parkinson’s disease: impaired effective connectivity among frontal cortical regions. Brain 125:276–289
Sabatini U, Boulanouar K, Fabre N, Martin F, Carel C, Colonnese C, Bozzao L, Berry I, Montastruc JL, Chollet F, Rascol O (2000) Cortical motor reorganization in akinetic patients with Parkinson’s disease: a functional MRI study. Brain 123(Pt 2):394–403
Samuel M, Ceballos-Baumann AO, Blin J, Uema T, Boecker H, Passingham RE, Brooks DJ (1997) Evidence for lateral premotor and parietal overactivity in Parkinson’s disease during sequential and bimanual movements. A PET study. Brain 120(6):963–976
Schrag A, Ben-Shlomo Y, Brown R, Marsden CD, Quinn N (1998) Young-onset Parkinson’s disease revisited–clinical features, natural history, and mortality. Mov Disord 13:885–894
Shimamoto H, Morimitsu H, Sugita S, Nakahara K, Shigemori M (1999) Therapeutic effect of repetitive transcranial magnetic stimulation in Parkinson’s disease. Rinsho Shinkeigaku 39:1264–1267
Siebner HR (2000) Simultaneous repetitive transcranial magnetic stimulation does not speed fine movement in PD. Neurology 54:272; author reply 273
Siebner HR, Rossmeier C, Mentschel C, Peinemann A, Conrad B (2000) Short-term motor improvement after sub-threshold 5-Hz repetitive transcranial magnetic stimulation of the primary motor hand area in Parkinson’s disease. J Neurol Sci 178:91–94
Siebner HR, Willoch F, Peller M, Auer C, Boecker H, Conrad B, Bartenstein P (1998) Imaging brain activation induced by long trains of repetitive transcranial magnetic stimulation. Neuroreport 9:943–948
Speer AM, Kimbrell TA, DR J, Wassermann EM, Willis MW, Herscovitch P, Post RM (2000) Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 48:1133–1141
Strafella AP, Ko JH, Monchi O (2006) Therapeutic application of transcranial magnetic stimulation in Parkinson’s disease: the contribution of expectation. Neuroimage 31:1666–1672
Strafella AP, Paus T, Barrett J, Dagher A (2001) Repetitive transcranial magnetic stimulation of the human prefrontal cortex induces dopamine release in the caudate nucleus. J Neurosci 21:RC157
Strafella AP, Paus T, Fraraccio M, Dagher A (2003) Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain 126:2609–2615
Tergau F, Wanschura V, Canelo M, Wischer S, Wassermann EM, Ziemann U, Paulus W (1999) Complete suppression of voluntary motor drive during the silent period after transcranial magnetic stimulation. Exp Brain Res 124:447–454
Tournoux Ta (1988) Stereotactic coplanar atlas of the human brain. Stuttgart, Germany
Worsley KJ, Marrett S, Neelin P, Evans AC (1996) Searching scale space for activation in PET images. Hum Brain Mapp 4:74–90
Acknowledgments
We thank Diana Millan-Aldaco, Marcela Palomero-Rivero and Francisco Pérez-Eugenio for their technical support and advice. This work was supported by a grant from IMPULSA 02-UNAM. Nadia González-García had a CONACYT (México) fellowship and additional support from the PhD Program of Biomedical Sciences, UNAM.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
González-García, N., Armony, J.L., Soto, J. et al. Effects of rTMS on Parkinson’s disease: a longitudinal fMRI study. J Neurol 258, 1268–1280 (2011). https://doi.org/10.1007/s00415-011-5923-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-5923-2