Abstract
Hereditary peripheral neuropathies present a group of clinically and genetically heterogeneous entities. All known forms, including the various forms of Charcot-Marie-Tooth disease (CMT) are characterized as Mendelian traits and over 35 genes have been identified thus far. The mutational mechanism of the most common CMT type, CMT1A, is a 1.5 Mb chromosomal duplication at 17p12 that contains the gene PMP22. Only recently it has been realized that such copy number variants (CNV) are a widespread phenomenon and important for disease. However, it is not known whether CNVs play a wider role in hereditary peripheral neuropathies outside of CMT1A. In a phenotypically heterogeneous sample of 97 patients, we performed the first high-density CNV study of 34 genomic regions harboring known genes for hereditary peripheral neuropathies including the 17p12 duplication region, with comparative genomic hybridization (CGH) microarrays. We identified three CNVs that affected coding exons. A novel shorter form of a PMP22 duplication was detected in a CMT1A family previously tested negative in a commercial test. Two other CNVs in MTMR2 and ARHGEF10 are likely not disease associated. Our results indicate that CNVs are a rare cause for non-CMT1A CMT. Their potential relevance as disease modifiers remains to be evaluated. The present study design cannot rule out that specific CMT forms exist where CNVs play a larger role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hereditary peripheral neuropathies comprise a clinically and genetically heterogeneous group of diseases with a prevalence of 1/2500 [1]. All subtypes with motor and sensory deficits are known as Charcot-Marie-Tooth (CMT) diseases and make up the majority of peripheral neuropathies. A clinical spectrum can be drawn from pure motor neuropathies, over motor and sensory, to pure sensory forms of peripheral neuropathies. Genetically more than 35 genes have been identified, though there is often not a strict genotype–phenotype correlation (Inherited Peripheral Neuropathies Mutation Database: http://molgen-www.uia.ac.be). With the identification of the underlying genes, the screening for mutations has become a mainstay in the diagnosis of peripheral neuropathies. Although current testing batteries are still limited to a few more common CMT forms it is generally expected that the scope of these tests will greatly increase in the near future. The state of the art approach for genetic testing in CMT is based on direct sequencing. This technique is suited to detect point mutations and small insertions/deletions with a high sensitivity and specificity. However, it is not possible to directly detect chromosomal gains or losses that extend beyond the reach of polymerase chain reaction (PCR) primers, usually a genetic distance of less than 1,000 bp. The majority of exons fall into this range, but copy number variations that include several exons or a large portion of an intron would be missed by conventional methods. Importantly, the major subtype of demyelinating CMT, CMT1A, is caused by a duplication of a 1.5 Mbp fragment of chromosome 17p12 that contains the causative gene PMP22. The opposite event, a loss of PMP22 is associated with a different peripheral neuropathy, hereditary neuropathy with liability to pressure palsies (HNPP) [2, 3]. No other CMT form is known to be caused by copy number variations (CNV). With the recent availability of high-density custom microarrays, the opportunity arises to screen the complete set of CMT genes for CNVs. In this study we performed the first high density CNV screen on a clinically heterogeneous sample of 97 CMT cases.
Materials and methods
CMT sample description
We studied 97 unrelated index patients with inherited peripheral neuropathies. Seventy patients were collected at the CMT clinic at Wayne State University and thirty patients came from the Miami Institute for Human Genomics. The majority (65) of these patients had an axonal phenotype, in accordance with the fact that the genetics of axonal neuropathies is least well understood (Table 1). We also included 17 demyelinating neuropathies, two dominant intermediate CMT patients, five sensory neuropathies, and three predominantly motor neuropathies. In five patients the neuropathy was not further categorized. The majority of these patients had been screened for the most frequent CMT genes. All participating individuals gave informed consent prior to initiating this study in agreement with the institutional review boards at Wayne State University and the University of Miami.
Custom CGH microarray
CNVs were detected using NimbleGen custom 385 k 4-plex comparative genomic hybridization (CGH) microarrays. We selected 34 genomic regions harboring known genes for hereditary peripheral neuropathies, including the 17p12 duplication region (Table 2). Microarrays consisting of 72,000 probes per array were manufactured by Roche/NimbleGen. Probes had an average length of 54 bp and were designed to achieve isothermal hybridization conditions. The average distance between probes within each region is 64 bp. Hybridizations were performed by Roche NimbleGen as a standard service. A pool of eight anonymous DNA samples, four males, four females (Promega), served as reference DNA for the CGH reaction. CGH data were normalized with NimbleScan 2.4 (Roche/NimbleGen) and segmented with Nexus 3.1 (BioDiscovery) using the rank segmentation algorithm. The significance threshold for segmentation was set at 10−6 and the minimal number of probes required per segment was 100. Copy number gains and losses were defined with a log2 Cy3/Cy5 ratio of 0.3 and −0.3, respectively; high gains and homozygous losses were defined with a ratio of 0.5 and −0.7. The X-chromosome encoded gene GJB1 (CMTX1) was excluded from the analysis as the reference DNA consisted of a pool of both genders. Data were further inspected manually by direct visualization using SignalMap (Roche NimbleGen).
Quantitative PCR assays
To confirm detected copy number variations we designed qPCR assays. Quantitative PCR was performed with Taqman assays and SYBR green-based quantification. A custom Taqman assay was designed for exon 15 of MTMR2. Sequences of the primers and probe are: MTMR2-ex15-PF: 5′-CCAGCATGCGCCACCTA-3′; PR: 5′-GTGGTTTCATCCGTGGATTCCA-3′; Probe: 5′-CTGGGTGGGATATTAC-3′. qPCR was performed using the Taqman Universal PCR Mastermix (Applied Biosystems) with the RNase P assay kit as endogenous control on a 7900HT Fast Real-Time PCR System (Applied Biosystems) with the manufacturer-recommended PCR conditions. For SYBR green-based detection, primers were designed for exon 2 of ARHGEF10 and exon 8 of IPO8 (endogenous control). qPCR was performed using the DyNAmo HS SYBR Green qPCR Kit (New England BioLabs) with the following conditions: 50°C 2 min; 95°C 15 min; 40 cycles of 94°C 10 s, 60°C 30 s and 72°C 30 s. Reactions were performed in triplicate with 5 ng/ul DNA. Data were analyzed using the ΔΔCt method. Sequences of the primers are: ARHGEF10-ex2-PF: 5′-TCCACCTGAACGGTGACAAG-3′; PR: 5′-TCTCAGCTCTGTTAAGGGAAGGA-3′; IPO8-ex8-PF: 5′-GGTTGCAATTGCTGCCTTGT-3′; PR: 5′-GGCAACTGAATTCGTTCTAAAGTATG-3′. Primers used to determine the breakpoints of the small duplication on chr17 are listed in Supplementary Table 1. We confirmed the chr17 duplication by qPCR using a custom Taqman assay designed for exon 2 of PMP22 with the RNase P assay kit as endogenous control (Applied Biosystems). Sequences of the primers and probe are: PMP22-ex2 PF: 5′-CTCCTCCTGTTGCTGAGTATCATC-3′; PR: 5′-GACGATCGTGGAGACGAACA-3′; Probe: 5′-CCAGCACCGCGACGTG-3′. PCR reactions were performed in quadruplicates with 5 ng/ul DNA on the 7900HT Fast Real-Time PCR System (Applied Biosystems).
Sequencing analysis
All exons of MTMR2 were sequenced with BigDye V3.1 chemistry on an ABI 3730 capillary instrument. PCR was performed on genomic DNA from the appropriate subjects using Platinum Taq (Invitrogen). Primer sequences are listed in Supplementary Table 2. Sequence reads were analyzed with the Sequencher software package (Genecodes).
Results
In the present study we screened for copy number variations (CNV) in 34 genomic regions that are known to harbor genes for hereditary peripheral neuropathies in 97 patients. We utilized high-density custom CGH microarrays for CNV detection. In each experiment, DNA isolated from patient blood samples was labeled with Cy3 and hybridized to high-density microarrays. As a control, a pool of DNA from eight anonymous individuals was labeled with Cy5, and hybridized simultaneously to the same microarray. The log ratio of the signal intensity from the patient relative to the control pool sample represents the DNA copy number ratio between the patient and the control sample. As an initial validation of this platform, we tested a CMT1A patient with a known chr17p12 duplication and were able to confirm the duplication with the CGH microarray. In 97 patients we detected three CNVs that affected coding exons (Table 3). All unique and potentially disease-causing CNVs were confirmed by qPCR analysis. In addition, we excluded additional compound heterozygous variants in samples that carried a CNV in the recessive MTMR2 gene.
Copy number variations and validation
Overall we identified six CNVs in the vicinity of CMT genes (Table 3). Three of them are novel CNVs and have not been reported previously according to the Database of Genomic Variants (DGV, http://projects.tcag.ca/variation/):
-
(1)
A 6.1 kb duplication was identified in one patient at the ARHGEF10 locus affecting exon 2. This occurred in a CMT patient with a demyelinating phenotype. The CNV was found to be common as it was present in six out of 57 controls (Fig. 1).
Fig. 1 Two CNVs affecting coding exons. Two plots generated with the Nexus software are shown illustrating two novel CNVs affecting coding exons. The exon–intron structure for each gene is shown on the top. Each open blue circle represents a probe on the array. The y-axis represents the log2 test-over-reference ratios of hybridization signals and the x-axis represents the location of probes corresponding to the gene above the plots. In the plot, the thresholds for calling single and higher copy number “loss” and “gain” are shown as red and green horizontal lines, respectively. The yellow line depicts a moving average value and the thick black lines are the output of the Nexus algorithm, defining segments. (a) A heterozygous deletion in MTMR2 affecting exons 13–15; (b) A duplication in ARHGEF10 affecting exon 2
-
(2)
A heterozygous 6.7 kb deletion that included exons 13–15 of the MTMR2 gene was identified in four patients, which all had an axonal phenotype. This deletion was confirmed to be a common CNV occurring in four out of 51 control samples. Sequencing of all coding exons of MTMR2 in the four patients carrying the CNV did not reveal any point mutations (Fig. 1).
-
(3)
One patient showed a 5.3 kb heterozygous deletion in intron 5 in gene SPTLC1 at 9q22.31. This individual also had an axonal dominant form of CMT. As this is a relatively small intronic deletion and is unlikely to be causative it was not further tested in controls.
The other three CNVs overlapped with known common CNVs reported in the Database of Genomic Variants (DGV: http://projects.tcag.ca/variation/):
-
(1)
A region of 5.4 kb in size in intron 11 of ARHGEF10 at 8p23.3 showed copy number gains in 13 patients and loss in one patient. This region overlaps with previously reported CNVs in the DGV database, but is larger in size.
-
(2)
One patient with a CMT1 phenotype showed a 14.7 kb heterozygous deletion in an intergenic region at 17p12, which was found in the DGV database in multiple reports. This genetic variant did neither affect PMP22 nor any other coding gene and is thus not likely a disease-causing CNV.
-
(3)
Three patients showed copy number gains with the size of 0.8 or 1.5 Mb at the 17p12 locus, which is discussed in the following section (Fig. 2).
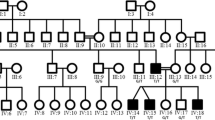
Chromosome 17 multiplications
Several changes were identified at the CMT1A locus at chromosome 17p12. First, we identified a classic 1.5 Mb duplication in a patient that was previously shown to carry this CNV. This individual served as a control sample and the investigator was blinded for its identity. Further, we identified 17p12 multiplications in two additional samples. Interestingly both samples were previously excluded for CMT1A in a commercial test. Both patients had a characteristic demyelinating clinical phenotype. Possibly explaining the divergent results, one of these patients showed a shorter duplication of only ~800 kb containing the PMP22 locus (Fig. 2a), with a distal breakpoint between 14,497 and 14,499 kb and proximal breakpoint between 15,292 and 15,295 kb as defined by qPCR (Supplementary Fig. 1), which correlated well with the CGH data. Moreover, the significantly higher ratio in qPCR with primers targeting the PMP22 gene suggested a triplication of this region (Fig. 2b). Despite this patient having potentially four copies of PMP22 instead of two, the phenotype appeared typical for CMT1A. The other patient showed the classic 1.5 Mb duplication. The 1.5 Mb variant was also reported in controls based on data from DGV (http://projects.tcag.ca/cgi-bin/variation/xview?source=hg18&view=variation&id=Variation_49816); however based on the high phenotypic penetrance of this mutation, it is highly likely the controls that carry the duplication have CMT1A. On the other hand, the 0.8 Mb variant was not found in the database.
(a) Two CMT1A patients with chr17p12 copy number gains. SignalMap software plots for two CMT1A patients with copy number gains at 17p12 are shown here. Each black dot represents a probe. The y-axis represents the log2 test-over-reference ratios of hybridization signals and the x-axis represents the genomic location of probes. The upper panel shows a patient with the classic 1.5 Mb duplication (depicted by the green arrow) and the lower panel shows a patient with a shorter region of copy number gain of about 0.8 Mb. Note both CNVs involve the PMP22 gene. (b) qPCR analysis of copy number at the PMP22 locus for the above two samples. The y-axis represents the copy number of each sample calculated from the qPCR ratios. For each sample qPCR was performed five times in quadruplicates and the average copy numbers are shown here
Our sample of 97 patients also contained a patient clinically diagnosed as HNPP, but we did not identify a loss at 17p12, neither with CGH nor with qPCR.
Discussion
Only recently has it been realized that CNVs play a much broader role in the human genome [4–6]. In fact, more base pairs vary between any two individuals as a consequence of CNVs than due to single nucleotide polymorphisms (SNP) [5]. Thus, CNVs are increasingly studied in the context of disease [7–14]. The first, and now classic, example of a disease causing CNV was the identification of a duplication of chr17p12 containing the gene PMP22 and leading to CMT1A [3]. In CMT1A only a minority of patients show a point mutation in PMP22. In contrast all other CMT genes appear to be caused exclusively by point mutations or small indels. To date it had not been comprehensively established whether additional CMT genes contain CNVs in CMT patients. Although it is desirable to perform whole-genome analysis of CNVs in CMT patients, the costs of such studies remain prohibitively high. The availability of custom microarrays allowed us to design an array that covers all known genes for hereditary peripheral neuropathies with a high density of probes. However, it is important to note that extra caution is needed when array CGH data are analyzed to detect smaller CNVs (<5 kb). As array CGH data are based on hybridization between probes and labeled DNA, sequence characteristics of probes, such as GC content, will have a significant impact on the hybridization. The smaller the region of interest, the greater the impact of local sequence content on hybridization dynamics, which could generate misleading results. In a high density array where probes are relatively close to each other, it is important to include a large number of probes when defining a CNV region, in order to reduce the influence of local sequence content characteristics. After intensive validation, we decided on a minimal CNV size of 100 probes (approximately 5 kb) to minimize false-positives in our results.
By studying a set of 97 CMT samples we identified a number of CNVs in different CMT genes. However, with the exception of PMP22, none of these changes appear to present a causative mutation. Three novel CNVs were found in our study. A heterozygous CNV in the recessive MTMR2 gene included the loss of exons. The identification of such alleles is likely not disease causing, but could nevertheless be important in two ways [1]. A compound heterozygous inheritance in combination with a causative point mutation on the other chromosome is conceivable. In other words, the identification of a heterozygous point mutation in a genetic test does not rule out the co-occurrence with a CNV, which would result in a phenotype. Thus, we excluded additional mutations by direct sequencing of MTMR2 in the four patients identified with this CNV. Importantly, CNV screens are not yet part of the general genetic testing in CMT. The CNV in MTMR2 might act as a modifying variant with consequences for age of onset, severity or other clinical characteristics. This possibility could not be proved in the current study, because the involved families were too small and the overall number of individuals carrying this change was limited. We also identified a novel duplication in ARHGEF10 affecting a coding exon. A mutation in this gene has been shown to be responsible for autosomal dominant slowed nerve conduction velocity [15]; however, since the duplication was common in controls, it is unlikely to be causative for the disease. Finally, we detected an intronic heterozygous deletion in gene SPTLC1. Because this deletion affected neither the coding sequence nor the splicing sites, it is unlikely to cause altered gene expression and a disease phenotype, though aberrations in intronic sequences can be disease-causing when they interfere with gene expression through altering DNA structure and stability, such as the GAA triplet repeats in the first intron of the gene FXN in Friedreich’s ataxia [16].
We also identified a gain of PMP22 that was suggestive of a triplication of the gene resulting in four gene copies in this individual. Gene dosage has been shown to be crucial for PMP22 function. A loss of PMP22 leads to HNPP; two copies represent the normal phenotype, while a duplication leads to CMT1A. The phenotype of the identified subject; however, was consistent with CMT1A. No especially severe clinical course was present. In addition, this individual had a shorter duplication of approximately 800 kb. Initial testing of this individual by a commercial laboratory came back with a negative result. This exemplifies that high density CGH could provide a more reliable technique for identification of small CNV or atypical CNV. The constant length of the chr17p12 CNV of 1.5Mbp has been attributed to two identical low copy number repeat (CMT1A-REP) sites that are flanking this chromosomal segment [17]. The occurrence of this shorter CNV would suggest an alternative mechanism not involving the REP sites, such as non-homologous end-joining (NHEJ) or Fork Stalling and Template Switching (FosTeS) [18].
Surprisingly, it appears that copy number detection in single cases can still pose challenges in quality-controlled commercial laboratories. The discrepancy between our data and the commercial analysis could result from different technologies used, i.e. CGH array vs. PCR-based MLPA. High density CGH arrays likely perform more consistently when detecting extended CNVs due to the large number of probes involved, as compared to PCR-based methods where typically only a few exons are being tested. However, the relatively high cost of CGH arrays remained (until recently) a major impediment for clinical diagnostic applications.
We conclude that CNVs play a rare role in CMT, with the important exception of PMP22. Nevertheless our study design does not exclude the possibility that a specific, relatively rare gene for CMT is characterized by CNV. The possibility of CNVs adds a considerable level of complexity to genetic testing, especially for recessive CMT genes. Further studies will be necessary to fully understand the contribution of CNV in the pathogenesis of hereditary peripheral neuropathies including CMT.
References
Skre H (1974) Genetic and clinical aspects of Charcot-Marie-Tooth’s disease. Clin Genet 6:98–118
Chance PF, Alderson MK, Leppig KA et al (1993) DNA deletion associated with hereditary neuropathy with liability to pressure palsies. Cell 72:143–151
Lupski JR, de Oca-Luna RM, Slaugenhaupt S et al (1991) DNA duplication associated with Charcot-Marie-Tooth disease type 1A. Cell 66:219–232
Iafrate AJ, Feuk L, Rivera MN et al (2004) Detection of large-scale variation in the human genome. Nat Genet 36:949–951
Redon R, Ishikawa S, Fitch KR et al (2006) Global variation in copy number in the human genome. Nature 444:444–454
Sebat J, Lakshmi B, Troge J et al (2004) Large-scale copy number polymorphism in the human genome. Science 305:525–528
Sebat J (2007) Strong association of de novo copy number mutations with autism. Science 316:445–449
Marshall CR (2008) Structural variation of chromosomes in autism spectrum disorder. Am J Hum Genet 82:477–488
Morrow EM (2008) Identifying autism loci and genes by tracing recent shared ancestry. Science 321:218–223
Stefansson H (2008) Large recurrent microdeletions associated with schizophrenia. Nature 455:232–236
Walsh T (2008) Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science 320:539–543
Xu B (2008) Strong association of de novo copy number mutations with sporadic schizophrenia. Nat Genet 40:880–885
The International Schizophrenia Consortium (2008) Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature 455:237–241
Beetz C Fau-Nygren AOH, Nygren Ao Fau-Schickel J, Schickel J Fau-Auer-Grumbach M et al (2006) High frequency of partial SPAST deletions in autosomal dominant hereditary spastic paraplegia. Neurology 66(3):421–423
Verhoeven K, De Jonghe P, Van de Putte T et al (2003) Slowed conduction and thin myelination of peripheral nerves associated with mutant rho Guanine-nucleotide exchange factor 10. Am J Hum Genet 73:926–932
Patel PI, Isaya G (2001) Friedreich ataxia: from GAA triplet-repeat expansion to frataxin deficiency. Am J Hum Genet 69:15–24
Pentao L, Wise CA, Chinault AC, Patel PI, Lupski JR (1992) Charcot-Marie-Tooth type 1A duplication appears to arise from recombination at repeat sequences flanking the 1.5 Mb monomer unit. Nat Genet 2:292–300
Gu W, Zhang F, Lupski JR (2008) Mechanisms for human genomic rearrangements. Pathogenetics 1:4
Acknowledgment
This study was supported by the National Institute of Neurological Disorders and Stroke (5R01NS052767-04, to S.Z.) and the Charcot-Marie-Tooth Association (to S.Z.).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Huang, J., Wu, X., Montenegro, G. et al. Copy number variations are a rare cause of non-CMT1A Charcot-Marie-Tooth disease. J Neurol 257, 735–741 (2010). https://doi.org/10.1007/s00415-009-5401-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5401-2