Abstract
Objective
In order to define the predictors of prolonged survival available at the time of first examination we performed a historical cohort study of amyotrophis sclerosis (ALS) patients referred to our ALS Clinic over the last 20 years.
Methods
In a group of 1034 patients with the diagnosis of definite or probable ALS the effects of individual prognostic factors on tracheostomy-free survival were assessed with the Kaplan-Meier life-table method. The prognostic value of each factor was estimated using univariate and multivariate Cox proportional hazard analyses.
Results
The median survival time was 3.45 years, (95%CI 3.27–3.74). Both the univariate and multivariate Cox models indicated that younger age, limb site of onset, longer diagnostic delay, lower Appel ALS score (AALSS) at first examination, lower AALSS-rate of change between first symptom and first exam (preslope), and higher baseline forced vital capacity (FVC) were associated with longer survival. In addition, four factors: age, diagnostic delay, baseline FVC and AALSS preslope have been identified as independent predictors of survival in our patient population.
Conclusions
The identification of younger age, limb site of onset and longer diagnostic delay as predictors of prolonged survival in ALS clinic population supports the findings of several, earlier studies that were based on smaller groups of patients. More significantly, several additional variables assessed at the first examination predict longer survival: lower baseline AALSS, lower AALSS- preslope and higher baseline FVC. All of these parameters are of value in patient management and in clinical trial development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, ALS clinical researchers have searched for new surrogate outcome measures that are objective and sensitive to change, with a particular view towards reduction of sample size and study duration [2, 25, 33]. Nevertheless, survival remains still the most commonly used outcome measure in ALS trials. Reported median lengths of survival in ALS patients vary from 2 to 4 years [8, 9, 13, 15, 25, 29]. Moreover, survival in ALS is known to vary among individuals and is considered to be difficult to predict in individual cases [24].
A variety of prognostic factors have been associated with prolonged survival in ALS in previous studies. The most consistently reported of them are younger age, limb site of symptom onset, and longer time from first symptom to diagnosis [8, 9, 12, 13, 15, 19, 20, 25, 34]. In addition, some investigators have reported male gender as a favorable prognostic factor [6, 8, 13]. Several reports have suggested that disease specific measures using different clinical scoring systems (i.e., ALSFRS, Appel Score) taken repeatedly during the early course of disease or even at the time of diagnosis may act as independent covariates of survival [9, 12, 15, 19, 25, 33]. However, given the different study designs (i.e., prospective or retrospective) and patient selection methods (i.e., referral vs. population-based series), the results of those studies sometimes conflicted and led to some uncertainty regarding potential prognostic factors in ALS [9, 13].
The evaluation of early prognostic variables and the understanding of “at first exam” factors related to survival may impact on the selection of patient cohorts for clinical trails and identify practical indicators that clinicians might use in the management of ALS patients. Thus, in order to estimate the influence of potential prognostic factors which are available at the time of the first examination on survival in ALS, we performed a historical cohort study of ALS patients, who were referred to our MDA-ALS Clinic in Houston, Texas. Moreover, we also sought to validate the Appel ALS score (AALSS), an ALS scoring system routinely used in our clinic, as an early and independent predictor of survival.
Methods
In our ALS Database we identified 1034 patients who fulfilled the diagnostic criteria for definite or probable ALS according to El Escorial/Airlie House criteria [5, 32] and who have regularly been followed at our ALS Clinic over a time period of more than 20 years. Demographic, clinical, laboratory, and EMG assessment data are collected at the first clinic visit or within a few days of that visit. Quantitative evaluations of disease progression using total Appel ALS score are performed at each follow-up clinic visit at approximately three-month intervals. During follow-up, major interventions such as percutaneous endoscopic gastrostomy (PEG), noninvasive ventilation (NIV), and tracheostomy are recorded.
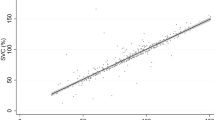
The details of the AALS score, which is routinely used in our clinic to provide an assessment of rates of progression and efficacy of therapies, are described elsewhere [1, 36]. In summary, the AALSS is based on an assessment of different categories of motor and respiratory function and includes both quantitative and functional components. It is composed of five subscores which range from 6 (normal) to 30–36 (complete loss of function). The subscores are quantified measures of (I) muscle strength, (II) bulbar function, (III) respiratory function, (IV) leg function, and (V) arm function. A total score of 30 points is normal; 164 points indicates maximal dysfunction. The AALS score assigns a weight to each region, giving the respective scores equal weight in the total score. Therefore, the total AALS score is an index of clinical severity, irrespective of the principal sites of involvement [22, 23]. The inter-observer variability (3%) and test-retest correlation (r2 = 0.99) of the total AALS score document reproducibility, and the measures are sensitive to changes in function from very early to very late disease stages [1]. In addition to the total AALS score at the time of first exam, a rate of AALSS change between first symptom and first examination (AALSS preslope) has been derived by subtracting 30 (i.e., normal function) from the total score exhibited at the first examination and dividing by the number of months reported to have passed since the first symptom [15]. First symptoms were confirmed by the family or other observers, whenever possible. Percent-predicted forced vital capacity (%FVC) was performed as recommended for ALS clinical trials using standard techniques and expressed as a percentage of the expected value [4]. FVC was examined at the time of first examination and at each follow-up visit (in general, every 3 months). FS-FE time was calculated from first symptom (FS) until the date of the first examination (FE). Survival, which was the outcome parameter in this study, was defined as the number of months from symptom onset until death from any cause or tracheostomy for institution of permanent mechanical ventilation. Patients who remained alive without tracheostomy were censored at the time of the last known follow-up. The effects of individual prognostic factors on survival were assessed with Kaplan-Meier life-table methods. Log rank test was used to assess equality of outcome functions. The prognostic value of each factor of interest was expressed interms of a hazard ratio (HR), which may be interpreted as a relative risk. The hazard ratio represents the mortality risk per time interval in the presence of a specific factor, relative to the risk in the absence of this factor. Crude hazard ratios were estimated by univariate analyses and adjusted hazard ratios by multivariate analyses using a proportional hazards regression model to correct for simultaneously effective covariables [11]. Patient characteristics subjected to univariate analyses were age, gender, site of symptom onset, clinical features at diagnosis, FS-FE time, disease stage at the time of the first clinic presentation (first AALSS and first FVC), and the rate at which the disease had progressed prior to first examination (AALSS preslope).
Given the importance of well-established prognostic factors, such as older age at onset, female gender, and bulbar site of onset HR and 95% CI for all variables significant in univariate analysis were adjusted for age, sex and site of onset (model 1). Finally, to identify the independent covariates of survival in our population we included all significant or clinically meaningful variables in the same Cox model (model 2). A p value of < 0.05 was considered significant. All statistical analyses were done using the SPSS v. 11.5.1 (SPSS, Chicago, IL) program.
Results
Demographics
The study cohort consisted of 1034 patients. Men composed 66.4% of the study population, while women were 33.6% of the group (1.9:1 ratio). The mean age at the time of disease onset was 54.1 years (SD 13.2), ranging from 19.8 to 84.8 years. On average, males were older (57.6 years) at disease onset than females (52.4 years). 171 patients (16.5%) exhibited primary bulbar symptoms, whereas the other 863 subjects described limb-onset disease. Of the 863 patients with limb onset, 443 (51%) exhibited their first symptoms in the lower limbs and 327 in the upper limbs. The remaining 93 patients reported both lower and upper limb symptoms at onset or were unable to provide this specific information. In addition, there was a strong tendency to report first symptoms in the distal portions of the affected limb (n = 623, 72%) compared with proximal portions (n = 83). The remaining 157 patients presented with both distal and proximal symptoms or this specific information could not be obtained. The average time from first symptom to first examination (FS-FE time) was 16.3 months (SD 12.3). The study patients were seen an average of 4.7 visits (SD 5.3) with a mean time between consecutive visits of 2.58 months (SD 1.7). The mean FVC at the time of the first examination was 82.9% (SD 20.9), mean baseline total AALS 63.3 points (SD 18.9) and the mean AALS preslope 2.68 points/month (SD 1.9). Riluzole (50 mg twice daily) was given to 430 (41.6%) patients. During the disease course, 275 patients (26.6%) underwent percutaneous endoscopic gastrostomy (PEG) and 128 (12.4%) were placed on noninvasive ventilation (NIV).
Survival analysis
As of November 2004, 576 (55.7%) of the 1034 analyzed patients had died (n = 477) or had tracheostomy (n = 99). Survival varied considerably between individuals and ranged from 2 months up to 11.5 years. The median tracheostomy-free survival time of the 1034 patients was 3.45 years (95% CI 3.27–3.74, mean 4.32 years). The 3–year survival rate from symptom onset was 59% (95%CI 56.4–63.3) and the 5–year survival rate was 28% (95% CI 25.3–32.7) (Figure 1).
Prognostic factors
As shown by Kaplan-Meier plots (Figures 2–7) and log-rank tests, survival differed significantly across categories of many factors. Univariate analyses identified all of the analyzed covariates except for gender and some clinical features at diagnosis (first symptom proximal vs. distal and first symptom in lower vs. in upper limb) (Table 1). The evaluation of effect modification in the multivariable Cox models after adjusting for established survival factors like age, gender, and site of disease onset (model 1), indicated that younger age, limb site of onset, longer FS-FE time, lower baseline AALSS, lower AALSS preslope, and higher baseline FVC were associated with longer survival (Table 1).
The final multivariate analysis, which analyzed all relevant demographic and clinical covariates along with therapies, in the single Cox model simultaneously (model 2), eliminated site of disease onset and baseline AALS score as independent covariates of survival in our ALS clinic population. However, age at the time of symptom presentation, FS-FE time, baseline FVC value and AALSS preslope remained independently and significantly associated with survival (Table 2).
Age
Age was identified as a strong and independent predictor of survival in our group. Younger age at the time of symptom onset was a strong favorable prognostic factor. Prognosis worsened with older age groups: patients who exhibited the first symptom at an age of 40 or younger had a median survival time of 6.01 years (95% CI 4.67–7.34), compared with 3.23 years (95% CI 3.03–3.43) for patients with onset between 40–70 and 2.85 years (95% CI 2.47–3.23) for patients above 70 years (Figure 2). In the youngest group, 60% survived at least 5 years, whereas only 8% of the eldest patients reached this endpoint. In the univariate analysis, patients in the age group between 40–70 years had a 2.65-fold increased risk of death or tracheostomy compared with patients younger than 40 years (p < 0.001). This effect was even stronger for the group of eldest patients who were characterized by a 3.86-fold increased risk of death in comparison with the group of youngest patients. More importantly, age at onset remained significantly associated with survival in the multivariate model 1 (HR 2.70 and HR 3.79, p < 0.001) after adjustment for significant or clinically meaningful variables (Table 1). In addition, statistical model 2 indicated younger age at onset as independent prognostic factor in our population (Table 2).
Gender
The difference in survival between females and males was not significant. Gender was not a predictor for survival (figure not shown, Table 1).
Site of onset and clinical features at diagnosis
Patients with limb symptoms at onset survived remarkably longer than bulbar onset patients (3.74 years vs. 2.80 years, p < 0.001), (Figure 3). Furthermore, the presence of bulbar symptoms at onset increased the risk of death in both univariate and multivariate analyses (HR 1.54 and HR 1.47) (Table 1). Our final multivariate model (model 2) eliminated ,however, the site of onset as an independent covariate of survival in the studied patient population (Table 2).
There was no significant difference in survival between initial proximal and initial distal limb involvement (p = 0.6), but a trend toward longer survival in those with lower limb onset was seen (p = 0.1) (Kaplan-Meier plots not shown). The univariate analyses eliminated these additional clinical features as risk factors for survival (Table 1).
First symptom (FS)-First examination (FE) delay (disease duration at first examination)
Patients whose first examination was longer than 12 months after first symptom survived longer (4.04 years, 95% CI 3.75–4.32) compared with patients who were first examined within 12 months after the onset of symptoms (2.61 years,95% CI 2.38–2.84, log-rank p < 0.001) (Figure 4). In the univariate analysis, patients with a shorter time to first examination (< 12 months) had a 2.02-fold increased risk of death or tracheostomy compared to patients with a longer FS-FE delay (> 12 months), (Table 1). Most importantly, in all performed multivariate models FS-FE delay remained significantly and independently associated with survival (Table 1 and 2).
Disease stage at the time of the first examination
We investigated the association between total AALS score at baseline and survival by comparing patients with total AALS score below and above 60 points. A 60-point level was chosen because it is indicative of a clinically evident impairment in a patient’s clinical status and ability to perform Activities of Daily Living. The median survival time for patients with baseline total AALS score below 60 points was 3.94 years (95% CI 3.57–4.31), compared with 3.02 years (95% CI 2.80–3.23, log-rank p < 0.001) for those with baseline AALSS above 60 points (Figure 5).
The baseline FVC also predicted survival in our ALS patient cohort, when divided into three arbitrary FVC subgroups. The median survival of ALS patients with baseline FVC > 85% was 4.12 years (95% CI 3.80–4.44), 3.34 years (95% CI 2.94–3.74) in those with FVC 65–85% and 2.72 years (95% CI 2.46–2.98, log-rank p < 0.001) in those with FVC < 65%, (Figure 6).
Overall, both baseline AALS score and baseline FVC were identified as predictors of survival in univariate and in multivariate Cox model 1 (Table 1). Of note, in contrast to baseline AALSS, baseline FVC was also identified as an independent prognostic factor in our final statistical model (Table 2).
Rate of disease progression prior to the first examination
We also analyzed the correlation of the rate of change in total AALS score prior to diagnosis (preslope) with death or tracheostomy for four arbitrary subsets of patients with preslope value of < 3, 3–6, 6–9 and > 9 points/month. Patients with slower disease progression between first symptom and first examination (i.e.,, lower preslopes) survived remarkably longer than patients characterized by higher AALSS preslopes (log-rank p < 0.001), (Figure 7). All patients in the lowest preslope group ( < 3 AALSS points/month) survived at least 1 year after first symptom, compared with only 40% of patients in the group with highest preslopes. Moreover, 35% of patients in the lowest preslope group survived at least 5 years, whereas none of the patients in the highest preslope group reached this endpoint. In addition, higher AALS score preslope was shown to act as a significant and independent predictor of survival in our population and to increase risk of death or tracheostomy in both univariate and multivariate models (Table 1 and 2).
Discussion
We have used our database to estimate survival in one of the largest ALS cohorts ever investigated and have identified several predictors of prolonged survival which are available at the time of the first examination. We validated the following factors: younger age, limb onset of the disease, longer delay before first examination, lower initial AALS score, higher initial percent-predicted FVC, and lower AALSS preslope. All of these factors remained significantly associated with survival after controlling for confounding variables such as age, gender and site of onset. In addition, age at symptom onset, FS-FE delay, baseline FVC and AALSS preslope have been shown to be independent predictors of survival in our database population.
The significantly better survival in younger patients in our study is in accordance with previous results [8, 9, 12, 13, 15, 19, 20, 23, 24, 25, 30, 31, 33, 34]. The mechanism underlying this phenomenon is unknown. Younger patients may compensate better for declining motor function and older patients may have fewer motor neurons to compensate. But such explanations provide little insights as to the mechanisms involved.
In the present series, no association between gender and prognosis was found. This finding agrees with the vast majority of previous studies [10, 19, 24, 25, 28, 31, 35]. However, some investigators reported significantly shorter survival for women than men, even after adjustment for previously established outcome covariates [6, 8, 13].
Most previous studies have reported that disease onset in the limbs rather than in the bulbar muscles was predictive of longer survival time [8, 13, 19, 20, 23, 24, 25, 31]. Bulbar-onset patients may have shortened survival from earlier involvement of respiratory muscles, a higher rate of respiratory complications, malnutrition, and dehydration [24]. However, some investigators failed to confirm this or found no prognostic value after correcting for well established prognostic factors like age [14, 15, 16]. In our study, an association between site of onset and survival has been shown. Even after adjustment for several well-established prognostic factors (e.g., age), survival was shorter for patients presenting with bulbar symptoms than patients exhibiting limb symptoms first. However, we failed to confirm an independent effect of the site of onset on the survival when analyzing this factor in the same statistical model with all others variables. This finding is consistent with our previous results [15] with one important exception: in the present series based on the multivariate model 1 bulbar onset is associated with shorter survival even after controlling for age at onset as a potentially confounding factor. We attempted to investigate limb onset more extensively by creating several subcategories for the extremity related sites: proximal versus distal, first symptom in upper extremity versus lower extremity. However, there was no statistically significant correlation between those factors and survival.
The delay between symptom onset and first examination was a robust predictor of survival in our study, as in others [12, 13, 15, 31]. This delay was negatively related to hazard, i.e., positively related to length of survival—in other words, the longer the delay, the longer the survival. Of note, in our enlarged database the previously reported relationship between FS-FE delay and the AALSS preslope supports the hypothesis that the time between first symptom and first clinical examination may be a measure of the rate of disease progression [15]. The more rapidly a patient initially deteriorates (higher AALSS preslope), the shorter the delay before the first symptom and first examination. These results suggest that fast progressing patients tend to seek medical care earlier, whereas those with slower disease progression are referred later or adapt to first symptoms for a longer time before they visit a tertiary care facility [15, 23, 24].
Can survival be accurately predicted by clinical measures at the first examination? AALSS preslope reflects the rate at which the disease had progressed prior to first examination, whereas the initial total AALS score, and the initial FVC may serve as indices of disease stage at the time of first exam. Based on our data, all three of these factors were shown to be significant predictors of survival even after adjustment for several potentially confounding variables and may constitute prognostic signposts in the early stages of the disease course. The slopes of the total AALS score, derived for each patient with three or more exams (post-diagnosis slopes) have previously been identified as significant covariates of survival [15]. Of note, our present study, performed with a larger number of patients, validates the AALSS preslope as significant and independent covariate of survival. The relationship between the preslope and the post-diagnosis slopes is not a good one, however [15]. Thus, predicting survival based on the preslope is probably not as accurate as utilizing the post-diagnosis slopes. However, the preslope based on a single measurement, is readily obtained at the time of the first examination, and provides a clinically meaningful measurement.
A higher initial FVC was also associated with longer survival both in univariate and multivariate statistical models; and was a significant and independent predictor of survival. The percent-predicted FVC has been previously shown to be a predictor of survival in ALS in several clinical trials [3, 12, 20, 27, 31, 33]. However, unlike previous referral cohort -based studies that reported a correlation between the rate of decline in pulmonary function, either defined as the slope of a pulmonary score [15, 30] or the slope of FVC decline [9, 25], we show that even a single FVC measurement value obtained at an initial visit may serve as a good predictor of survival in the ALS clinic population.
There are clearly potential limitations of the widespread applicability of our study. First, during the 20-year observation period, different diagnostic criteria have been used. In our experience, however, the diagnostic and clinical features of patients diagnosed as “typical ALS” (this term was in use in our database prior to the publication of El Escorial criteria in 1994) correspond very well with the features of patients diagnosed as definite or probable ALS after 1994). Second, since our database did not allow the inclusion of patients with possible or suspected ALS into the analysis, we focused on the group of patients with definite or probable ALS. It is well known, that some patients often did not satisfy the diagnosis of definite or probable ALS at the first visit but they might have fulfilled the criteria afterwards. Thus, this selectivity in patients may be a limitation of our study. In addition, nearly all of the patients in our database cohort have been referred by primary care physicians or neurologists, and the interpretation of our data should be made in light of this nonrandom enrollment. Moreover, it is possible that clinic-based series may present a somewhat distorted picture of the ALS population because of the special characteristics of patients that seek care at tertiary centers. A referral cohort tends to have younger patients and may also be weighted toward specific clinical features. Another potential limitation of our study is the inclusion of patients who were being evaluated for possible entry into therapeutic trials, resulting in a bias against participation in the clinic by patients with atypical disease presentations. Those factors, along with the access to optimal medical treatment in an academic institution, may result in a relatively better prognosis in patients seen in a referral center [17, 23].
In addition, we did not find a significant and independent effect of riluzole therapy in our patient population. PEG and NIV-use (analyzed as categorical variable ever vs. never) during the disease course was associated with increased risk of death or tracheostomy, which may suggest that these interventions may be view as markers of advanced disease and were probably performed late in disease course in severely impaired patients. These findings are consistent with several previous reports [7, 18, 26]. However, our database was not sufficient to analyze the timing of the intervention and to perform survival analyses from the point of PEG or NIV initiation. We were also not able to address the compliance issue for those therapies (i.e., comparing the NIV effect in NIV users who tolerated this intervention well with those who cannot tolerate it and discontinued treatment).
The identification of younger age, limb site of onset and longer FS-FE delay as predictors of prolonged survival in an ALS clinic population supports the findings of several, earlier studies that were based on smaller groups of patients. In addition, we describe the favorable prognostic value of several, “at first examination” clinical parameters—lower baseline AALSS, lower AALSS preslope, and higher baseline FVC, all which may have significant utility in patient management. Moreover, our findings may be helpful in designing new treatment trials, ones which use survival as the primary endpoint. The appropriate stratification of eligible patients based on the described predictors of survival could result in reduction of sample size and study duration.
References
Appel V, Stewart SS, Smith G, Appel SH (1987) A rating scale for amyotrophic lateral sclerosis: Description and preliminary experience. Ann Neurol 22:328–333
Armon C, Graves MC, Moses D, Forte DK, Sepulveda L, Darby SM, Smith RA (2000) Linear estimates of disease progression predict survival in patients with amyotrophic lateral sclerosis. Muscle Nerve 23:874–882
Bensimon G, Lacomblez L, Meininger V (1994) A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med 330:585–591
Brinkmann JR, Andres P, Mendoza M, Sanjak M (1997) Guidelines for the use and performance of quantitative outcome measures in ALS clinical trials. J Neurol Sci 147:97–111
Brooks BR (1994) El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. J Neurol Sci 124:96–107
Caroscio JT, Mulvihill MN, Sterling R, Abrams B (1987) Amyotrophic lateral sclerosis: its natural history. Neurol Clin 5:1–8
Cedarbaum JM, Stambler N (2001) Disease status and use of ventilatory support by ALS patients BDNF Study Group. Amyotroph Lateral Scler Other Motor Neuron Disord 2:19–22
Chancellor AM, Slattery JM, Fraser H, Swingler RJ, Holloway SM, Warlow CP (1993) The prognosis of adult-onset motor neuron disease: a prospective study based on the Scottish Motor Neuron Disease Register. J Neurol 240:339–346
Chio A, Mora G, Leone M, Mazzini L, Cocito D, Giordana MT, Bottacchi E, Mutani R (2002) Piemonte and Valle d’Aosta Register for ALS (PARALS) Early symptom progression rate is related to ALS outcome: a prospective population-based study. Neurology 59:99–103
Christensen PB, Hojer-Pedersen E, Jensen NB (1990) Survival of patients with amyotrophic lateral sclerosis. Neurology 40:600–604
Cox DR (1972) Regression models and life tables. J R Stat Soc B 34:187–220
Cudkowicz ME, Shefner JM, Schoenfeld DA, Brown RH Jr, Johnson H, Qureshi M, Jacobs M, Rothstein JD, Appel SH, Pascuzzi RM, Heiman-Patterson TD, Donofrio PD, David WS, Russell JA, Tandan R, Pioro EP, Felice KJ, Rosenfeld J, Mandler RN, Sachs GM, Bradley WG, Raynor EM, Baquis GD, Belsh JM, Novella S, Goldstein J, Hulihan J (2003) Northeast ALS Consortium A randomized, placebo-controlled trial of topiramate in amyotrophic lateral sclerosis. Neurology 61:456–464
del Aguila MA, Longstreth WT Jr, McGuire V, Koepsell TD, van Belle G (2003) Prognosis in amyotrophic lateral sclerosis: a population-based study. Neurology 60:813–819
Eisen A, Schulzer M, MacNeil M, Pant B, Mak E (1993) Duration of amyotrophic lateral sclerosis is age dependent. Muscle Nerve 116:27–32
Haverkamp LJ, Appel V, Appel SH (1995) Natural history of amyotrophic lateral sclerosis in a database population. Validation of a scoring system and a model for survival prediction. Brain 118:707–719
Jablecki C, Berry C, Leach J (1989) Survival prediction in amyotrophic lateral sclerosis. Muscle Nerve 12:833–841
Juergens SM, Kurland LT, Okazaki H, Mulder DW (1980) ALS in Rochester, Minnesota, 1925–1977. Neurology 30:463–470
Kasarskis EJ, Scarlata D, Hill R, Fuller C, Stambler N, Cedarbaum JM (1999) A retrospective study of percutaneous endoscopic gastrostomy in ALS patients during the BDNF and CNTF trials. J Neurol Sci 169:118–125
Kaufmann P, Levy G, Thompson JL, Delbene ML, Battista V, Gordon PH, Rowland LP, Levin B, Mitsumoto H (2005) The ALSFRSr predicts survival time in an ALS clinic population. Neurology 64:38–43
Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V (1996) Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet 347:1425–1431
Lange DJ, Felice KJ, Festoff BW, Gawel MJ, Gelinas DF, Kratz R, Lai EC, Murphy MF, Natter HM, Norris FH, Rudnicki S (1996) Recombinant human insulin-like growth factor-I in ALS: description of a double-blind, placebo-controlled study. North American ALS/IGF-I Study Group. Neurology 47(Suppl 2):S93–94
Lange DJ, Murphy PL, Diamond B, Appel V, Lai EC, Younger DS, Appel SH (1998) Selegiline is ineffective in a collaborative double-blind, placebo-controlled trial for treatment of amyotrophic lateral sclerosis. Arch Neurol 55:93–96
Lee JR, Annegers JF, Appel SH (1995) Prognosis of amyotrophic lateral sclerosis and the effect of referral selection. J Neurol Sci 132:207–215
Louwerse ES, Visser CE, Bossuyt PM, Weverling GJ (1997) Amyotrophic lateral sclerosis: mortality risk during the course of the disease and prognostic factors. The Netherlands ALS Consortium. J Neurol Sci 152(Suppl 1):S10–17
Magnus T, Beck M, Giess R, Puls I, Naumann M, Toyka KV (2002) Disease progression in amyotrophic lateral sclerosis: predictors of survival. Muscle Nerve 25:709–714
Mitsumoto H, Davidson M, Moore D, Gad N, Brandis M, Ringel S, Rosenfeld J, Shefner JM, Strong MJ, Sufit R, Anderson FA (2003) ALS CARE Study Group Percutaneous endoscopic gastrostomy (PEG) in patients with ALS and bulbar dysfunction. Amyotroph Lateral Scler Other Motor Neuron Disord 4:177–185
Moore DH, Miller RG (2003) WALS Study Group ALS CARE Study Group ALSRFS as a measure of disease progression and survival. Amyotroph Lateral Scler Other Motor Neuron Disord 4(Suppl 1):C51
Norris F, Shepherd R, Denys E, U K, Mukai E, Elias L, Holden D, Norris H (1993) Onset, natural history and outcome in idiopathic motor neuron disease. J Neurol Sci 118:48–55
Preux PM, Couratier P, Boutros-Toni F, Salle JY, Tabaraud F, Bernet-Bernady P, Vallat JM, Dumas M (1996) Survival prediction in sporadic amyotrophic lateral sclerosis : age and clinical form at onset are independent risk factors. Neuroepidemiology 15:153–160
Ringel SP, Murphy JR, Alderson MK, Bryan W, England JD, Miller RG, Petajan JH, Smith SA, Roelofs RI, Ziter F (1993) The natural history of amyotrophic lateral sclerosis. Neurology 43:1316–1322
Stambler N, Charatan M, Cedarbaum JM (1998) Prognostic indicators of survival in ALS. Neurology 50:66–72
Traynor BJ, Codd MB, Corr B, Forde C, Frost E, Hardiman OM (2000) Clinical features of amyotrophic lateral sclerosis according to the El Escorial and Airlie House diagnostic criteria: A population-based study. Arch Neurol 57:1171–1176
Traynor BJ, Zhang H, Shefner JM, Schoenfeld D, Cudkowicz ME; NEALS Consortium (2004) Functional outcome measures as clinical trial endpoints in ALS. Neurology 63:1933–1935
Turner MR, Parton MJ, Shaw CE, Leigh PN, Al-Chalabi A (2003) Prolonged survival in motor neuron disease a descriptive study of the King’s database 1990–2002. J Neurol Neurosurg Psychiatry 74:995–997
Tysens OB, Vollset SE, Aarli JA (1991) Epidemiology of amyotrophic lateral sclerosis in Hordaland county, western Norway. Acta Neurol Scand 83:280–285
Yen AA, Simpson E, Haverkamp LJ, Appel SH (2004) AALS. ALS and Other Motor Neuron Disorders 5(Suppl1):S1–S5
Acknowledgements
We thank the patients and the members of the Muscular Dystrophy Association ALS Clinic team at Methodist Neurological Institute and Baylor College of Medicine in Houston, Texas for their contributions to gathering the database information. This work was supported by the MDA and the Houston Endowment. Adam Czaplinski was the recipient of the Sheila Essey ALS Fellowship Award and was also supported by Swiss National Science Foundation and Fonds zur Foerderung des Akademischen Nachwuchses University of Basel, Switzerland. We thank Dipl.-Math. Andreas Schoetzau for his thoughtful statistical advice and comments. We are grateful to Joan Appel for her assistance in coordinating the data-base investigation and manuscript review.
Author information
Authors and Affiliations
Corresponding author
Additional information
Received in revised form: 02 March 2006
Rights and permissions
About this article
Cite this article
Czaplinski, A., Yen, A.A. & Appel, S.H. Amyotrophic lateral sclerosis: early predictors of prolonged survival. J Neurol 253, 1428–1436 (2006). https://doi.org/10.1007/s00415-006-0226-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-006-0226-8