Abstract
The aim of this study is to evaluate the association between changes in routinely prescribed laboratory tests and tracheostomy-free survival in amyotrophic lateral sclerosis (ALS). Two hundred seventy-five ALS patients were retrospectively studied. BMI, forced vital capacity, hemoglobin, hematocrit, lymphocytes, cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides, proteins, albumin, creatine-phosphokinase, iron, ferritin, transferrin, glucose, urea, uric acid, and creatinine were measured every 6 months from baseline to 24 months, death or study end, together with the probability of death or tracheostomy. Missing data were handled using multiple imputation chained equations. Hemoglobin (OR = 1.71, 95%CI 1.24–2.36 for IQR increase), hematocrit (OR = 1.87, 95%CI 1.34–2.63 for IQR increase), urea (OR = 1.51, 95%CI 1.21–1.89 for IQR increase), and uric acid (OR = 1.98, 95%CI 1.23–3.20 for IQR increase) were directly associated, while triglycerides (OR = 0.69, 0.51 to 0.93 for IQR increase) were inversely associated with the odds of death or tracheostomy. In our cohort, an increase of hemoglobin, hematocrit, urea, and uric acid was directly associated, and an increase of triglycerides was inversely associated with the odds of death or tracheostomy. Should these findings be replicated in an external cohort, they might help to discriminate ALS progression and patients’ decisions about procedures and end of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) has a progressive course characterized by worsening disability and death after a period of time which is highly variable among patients. Such heterogeneity makes it difficult to predict how ALS will progress in a given patient and to evaluate the efficacy of new treatments in clinical trials [1].
The uncertain prognosis of ALS is discomforting to the patients and their families, who have to cope with an increasing number of difficulties in an unpredictable time. Being able to better discriminate the progression of ALS might allow patients and physicians to make better decisions about ventilation, nutritional support, and end of life [1].
Known prognostic factors for ALS include age at onset, phenotype, diagnostic delay, degree of diagnostic certainty according to El Escorial-Revised Criteria (EEC-R), concurrent dementia, and body mass index (BMI) [2, 3]. Many potential prognostic markers have been studied in ALS patients including uric acid [4, 5], albumin, creatinine [6], blood lipids [7, 8], ferritin, transferrin [9, 10], creatine-phosphokinase (CPK) [11], regulatory T cells [12, 13], and neurofilaments [14, 15]. The study of such prognostic markers has generally led to conflicting results. A recent crowd-sourced analysis of data from multiple clinical trials has suggested a prognostic role for uric acid and creatinine [16]. However, only one study so far has tested the association between repeated measures of prognostic markers and ALS prognosis [17].
An ideal prognostic marker for ALS should be obtained with minimum discomfort to the patient and should be rapidly available. For this reason, we retrospectively evaluated the association between the changes in routinely prescribed laboratory tests and tracheostomy-free survival in the cohort of ALS patients followed at our Center.
Patients and methods
Study design
This was a retrospective cohort study performed on ALS patients diagnosed between 1 January 2000 and 31 December 2013 in Modena (Italy). Starting from 1 January 2000, an ALS multidisciplinary Center is working in Modena and collecting all cases of incident ALS on a registry [18]. The data of the ALS patients diagnosed from 1 January 2009 are also available in the web-based Regional (Emilia Romagna) ALS Registry [19]. ALS was diagnosed in all cases using the EEC-R [20]. ALS patients were followed up from diagnosis until death or last observation date, which was set at 31 December 2014 for the present analysis. The study was approved by the local Ethical Committee.
Clinical assessment
Each ALS patient underwent a standardized clinical assessment including the evaluation of the variables of interest for the present analysis: (1) ALS diagnosis according to EEC-R; (2) sex; (3) age at diagnosis; (4) age at onset; (5) site of onset; (6) clinical phenotype [21]; (7) presence of percutaneous endoscopic gastrostomy (PEG); (8) treatment with riluzole; and (9) ventilation. Forced vital capacity (FVC) was measured using whole body pletismography. Weight and height were measured following international guidelines, and BMI was calculated as weight (kg) × height (m)−2. A functional assessment was performed using the ALS functional rating scale [22, 23]. The clinical information was updated at each follow-up visit. At our ALS Center, we perform follow-up visits every 3 months. Such visits include support from pulmonologists, dietitians, speech pathologist, rehabilitation physicians, psychologists, and other specialists when needed. For the purpose of the present study, we used the data obtained at follow-up visits performed every 6 months (see below).
Laboratory tests
The following laboratory tests were retrieved for each ALS patient at baseline and every 6 months thereafter until death or last observation date, tracheostomy, or study termination: (1) hemoglobin; (2) hematocrit; (3) lymphocytes; (4) cholesterol; (5) LDL-cholesterol; (6) HDL-cholesterol; (7) triglycerides; (8) proteins; (9) albumin; (10) CPK; (11) iron; (12) ferritin; (13) transferrin; (14) glucose; (15) urea; (16) uric acid; and (17) creatinine. All laboratory tests were performed by the same centralized clinical laboratory using standardized methods.
Statistical analysis
Most continuous variables were not Gaussian-distributed, and all are reported as 50th (median), 25th, and 75th percentiles. Discrete variables are reported as the number and proportion of subjects with the characteristic of interest.
The probability of death or tracheostomy at 6, 12, 18, and 24 months of follow-up was estimated from a discrete-time logistic regression model having death or tracheostomy as response variable (0 = no; 1 = yes) and discrete-time as predictor (0 = baseline; 1 = 6 months; 2 = 12 months; 3 = 18 months; 4 = 24 months) [24, 25].
The choice of such modeling strategy was due to the fact that traditional modeling strategies such as Cox regression are unsuitable for use with discrete-time intervals [24, 25].
To test whether the time-varying continuous variables of interest (BMI, FVC, hemoglobin, hematocrit, lymphocytes, cholesterol, LDL-cholesterol, HDL-cholesterol, triglycerides, proteins, albumin, CPK, iron, ferritin, transferrin, glucose, urea, uric acid, and creatinine) were associated with death or tracheostomy, we added each of them as predictor to the discrete-time logistic regression model together with ALS type (discrete; 0 = spinal; 1 = bulbar) and age at onset (continuous, years/10). Each continuous predictor was divided by its interquartile range (IQR) to allow the comparison of predictors with different units of measurements [26]. ALS type and age at onset were added to the model, because they are known prognostic indexes in ALS, and we aimed at assessing the independent contribution of the variables of interest to death or tracheostomy. Because the discrete-time logistic regression model has the response variable and the predictors specified at each time-point [25], the values of the predictors after death were put equal to those at death when these were available. Missing data were otherwise handled by using multiple imputation chained equations (MICE) [27]. Among the MICE predictors, the outcome (death or tracheostomy), the (discrete) time of the outcome, sex, ALS phenotype, and age at onset were known for all patients, while the time-varying variables of interest were not available at all times for all patients and were estimated by MICE using linear regression in 100 imputation datasets. Statistical analysis was performed using Stata 14.2 (Stata Corporation, College Station, TX, USA).
Results
Of 312 patients diagnosed with ALS at our Center from 1 January 2000 to 31 December 2013, 13 were excluded because of unconfirmed diagnosis and 24 because of complete lack of laboratory tests at diagnosis.
Table 1 gives the clinical characteristics of the 275 studied ALS patients stratified by sex.
Table 2 gives the values of BMI, FVC and laboratory tests at baseline and at 6,12,18 and 24 months.
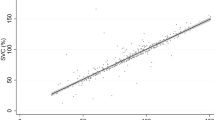
Figure 1 plots the cumulative incidence of death or tracheostomy from diagnosis as estimated by the discrete-time logistic regression model.
The cumulative incidence of death or tracheostomy was 0.08 (95%CI 0.05–0.11) at 6 months, 0.15 (95%CI 0.11–0.19) at 12 months, 0.24 (95%CI 0.19–0.29) at 18 months, and 0.36 (95%CI 0.30–0.41) at 24 months.
Figure 2 plots the odds ratio (OR) of death or tracheostomy associated with an increase of an IQR of each of the continuous predictors of interest.
Point estimates and 95% confidence intervals of the odds ratio of death or tracheostomy associated with an increase of an interquartile range of the continuous predictor of interest. The values are obtained from 19 multivariable logistic regression models controlling for ALS type (discrete, bulbar vs. spinal) and age at onset (continuous) and taking missing data into using multiple imputation chained equations (see statistical analysis for details)
These OR were obtained from multivariable logistic regression models controlling for ALS type and age at onset and taking missing data into account via MICE (models not shown; see statistical analysis for details).
Hemoglobin (OR = 1.71, 95%CI 1.24–2.36 for IQR increase), hematocrit (OR = 1.87, 95%CI 1.34–2.63 for IQR increase), urea (OR = 1.51, 95%CI 1.21–1.89 for IQR increase), and uric acid (OR = 1.98, 95%CI 1.23–3.20 for IQR increase) were directly associated, while triglycerides (OR = 0.69, 0.51 to 0.93 for IQR increase) were inversely associated with the odds of death or tracheostomy.
Discussion
In this retrospective repeated-measure cohort study, we tested whether changes in routinely performed laboratory tests could serve as prognostic markers in ALS. We found that an increase of hemoglobin, hematocrit, urea, and uric acid was directly associated and that an increase of triglycerides was inversely associated with the odds of death or tracheostomy. Also, using such repeated-measure design, we were not able to confirm some previously reported associations between laboratory tests, e.g., albumin, and the odds of death or tracheostomy.
A great strength of this study is the availability of repeated measures. We evaluated the association between laboratory tests and death or tracheostomy using five repeated measures (0, 6, 12, 18, and 24 months). Although we had to take into account the presence of missing data, the availability of repeated measures within the same patient allows to control patient-level heterogeneity much better than the standard approach of associating a single baseline value with a later outcome [25]. The major drawback of the present study is the presence of missing data, which is nonetheless quite common with both retrospective and prospective cohort studies, especially in diseases characterized by rapidly increasing disability such as ALS. There is a general consensus among statisticians that is much better to handle missing data via multiple imputation (or other techniques) than simply discarding them [27]. We used MICE for handling missing data in the present study, which is presently regarded as the most efficient multiple imputation technique [27]. We did not, however, test the effect of time on the outcome-predictors association. This would require (at least) the addition of a timeXpredictor interaction term to the logistic regression model, something which was not possible here, because the missing data and the intrinsically discrete nature of time did not allow to have enough points to estimate a time-related effect with acceptable precision [25]. We plan to perform such analysis on a future version of our ALS database offering with the availability of more time-points.
Another limitation of the present study is its observational nature. Whether a modifiable risk factor can increase survival in ALS can only be tested by performing a randomized controlled trial aiming at modifying that factor. Confounding is the main problem of all observational epidemiology, and its effect may be even greater than usual in a disease such as ALS which requires different treatments and is characterized by substantial patient-level heterogeneity.
This is the first study showing that change during time of hemoglobin and hematocrit could serve as prognostic markers in ALS. A rising hematocrit in ALS patients may be a surrogate measure of the dehydration associated with drink dysphagia and/or respiratory insufficiency [28]. In the present repeated-measure study, however, we found no association between the changes of FVC and those of hemoglobin and hematocrit (data not shown). Also, we found no association between the changes of BMI and those of hemoglobin and hematocrit (data not shown), but this was not unexpected because of the nutritional support received by our patients. On the other hand, a rising hemoglobin level may signal an increased risk of vascular access thrombosis and adverse cardiovascular events.
The association between a rising urea and the odds of death or tracheostomy has never been reported before, to the best of our knowledge. Instead, in a large Italian cohort, creatinine was found to be a prognostic marker of ALS [6], but blood urea was not measured in that study. It should nonetheless be noted that, contrarily to that study [6], we found no association between the changes in creatinine and the odds of death or tracheostomy in our patients. Both urea and creatinine can increase because of dehydration so that, as hypothesized above for hemoglobin and hematocrit, the increase of urea may signal dehydration. Another explanation of the urea-survival association may come from the fact that urea is the product of the catabolism of ammonia and oxidation of amino acids. The ubiquitous enzyme glutamine synthetase (GS) catalyzes the conversion of ammonia and glutamate into glutamine. GS is present in the brain, mostly in astrocytes, and plays a central role in brain detoxification and glutamate metabolism regulation [29, 30]. Whether the association between a rising urea and the odds of death or tracheostomy found in our ALS patients signals a dysregulated brain metabolism is highly speculative but warrants further exploration.
Uric acid, the product of purine metabolism, has immunological and pro-inflammatory functions and has been extensively studied in ALS [31]. Low levels of uric acid have been reported not only in ALS but also in neurodegenerative disorders such as Alzheimer’s disease, Huntington’s disease, Parkinson’s disease, and multiple system atrophy [31]. A meta-analysis of ALS studies [4, 5, 31, 32] has reported an inverse association between baseline uric acid levels and mortality. Our finding of a direct association between an increase of uric acid and death or tracheostomy is not necessarily at odds with these findings, because our study focused on changes and not on static values of laboratory tests. This interpretation is supported by the finding of a recent study [33], which measured uric acid at two time-points and showed that the association of uric acid with survival was present at one but not at the other time-point. As for urea, if and how the association between uric acid and ALS survival reflect changes occurring inside astrocytes is highly speculative but warrants further exploration [31].
In our study, there was an inverse association between the changes of triglycerides and the odds of death and tracheostomy in ALS. On the other hand, we observed no association between the changes in total, HDL and LDL cholesterol, and the odds of death and tracheostomy. Blood lipids have been studied more than other laboratory tests in ALS with contradictory findings [7, 8, 34]. The precision of the effect size attributable to an increase of an IQR (i.e., 65 mg × dl-1) of triglycerides is wide enough (OR = 0.69, 0.51 to 0.93) to suggest that larger studies are needed before one can reliably infer the existence of a clinically relevant relationship between triglycerides and survival in ALS.
In conclusion, in the present retrospective cohort study of ALS patients, an increase of hemoglobin, hematocrit, urea, and uric acid was positively associated, and an increase of triglycerides was inversely associated with the odds of death or tracheostomy. These findings need to be replicated in external cohorts before they can be translated into clinical practice.
References
Hardiman O, van den Berg LH, Kiernan MC (2011) Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat Rev Neurol 7:639–649
Creemers H, Grupstra H, Nollet F et al (2014) Prognostic factors for the course of functional status of patients with ALS: a systematic review. J Neurol:1407–1423. https://doi.org/10.1007/s00415-014-7564-8
Calvo A, Moglia C, Lunetta C et al (2016) Factors predicting survival in ALS: a multicenter Italian study. J Neurol. https://doi.org/10.1007/s00415-016-8313-y
Keizman D, Ish-shalom M, Berliner S et al (2009) Low uric acid levels in serum of patients with ALS: further evidence for oxidative stress? J Neurol Sci 285:95–99. https://doi.org/10.1016/j.jns.2009.06.002
Ikeda K, Kawabe K, Iwasaki Y (2009) Do serum uric acid levels reflect oxidative stress in the progression of ALS? J Neurol Sci 287:294. https://doi.org/10.1016/j.jns.2009.08.008
Chiò A, Calvo A, Bovio G et al (2014) Amyotrophic lateral sclerosis outcome measures and the role of albumin and creatinine: a population-based study. JAMA Neurol 71:1–9. https://doi.org/10.1001/jamaneurol.2014.1129
Dorst J, Kühnlein P, Hendrich C et al (2011) Patients with elevated triglyceride and cholesterol serum levels have a prolonged survival in amyotrophic lateral sclerosis. J Neurol 258:613–617. https://doi.org/10.1007/s00415-010-5805-z
Dupuis L, Corcia P, Fergani A et al (2008) Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology 70:1004–1009. https://doi.org/10.1212/01.wnl.0000285080.70324.27
Veyrat-Durebex C, Corcia P, Mucha A et al (2014) Iron metabolism disturbance in a French cohort of ALS patients. Biomed Res Int. https://doi.org/10.1155/2014/485723
Nadjar Y, Gordon P, Corcia P et al (2012) Elevated serum ferritin is associated with reduced survival in amyotrophic lateral sclerosis. PLoS One 7:2–7. https://doi.org/10.1371/journal.pone.0045034
Rafiq MK, Lee E, Bradburn M et al (2016) Creatine kinase enzyme level correlates positively with serum creatinine and lean body mass, and is a prognostic factor for survival in amyotrophic lateral sclerosis. Eur J Neurol 23:1071–1078. https://doi.org/10.1111/ene.12995
Beers DR, Henkel JS, Zhao W et al (2011) Endogenous regulatory T lymphocytes ameliorate amyotrophic lateral sclerosis in mice and correlate with disease progression in patients with amyotrophic lateral sclerosis. Brain 134:1293–1314. https://doi.org/10.1093/brain/awr074
Henkel JS, Beers DR, Wen S et al (2013) Regulatory T-lymphocytes mediate amyotrophic lateral sclerosis progression and survival. EMBO Mol Med 5:64–79. https://doi.org/10.1002/emmm.201201544
Steinacker P, Huss A, Mayer B, et al. (2016) Diagnostic and prognostic significance of neurofilament light chain NF-L, but not progranulin and S100B, in the course of amyotrophic lateral sclerosis: Data from the German MND-net. Amyotroph Lateral Scler Frontotemporal Degener:1–8. https://doi.org/10.1080/21678421.2016.1241279
Oeckl P, Jardel C, Salachas F et al (2016) Multicenter validation of CSF neurofilaments as diagnostic biomarkers for ALS. Amyotroph Lateral Scler Frontotemporal Degener 17:404–413. https://doi.org/10.3109/21678421.2016.1167913
Küffner R, Zach N, Norel R et al (2015) Crowdsourced analysis of clinical trial data to predict amyotrophic lateral sclerosis progression. Nat Biotechnol 33:51–57. https://doi.org/10.1038/nbt.3051
Patin F, Corcia P, Madji Hounoum B et al (2015) Biological follow-up in amyotrophic lateral sclerosis: decrease in creatinine levels and increase in ferritin levels predict poor prognosis. Eur J Neurol 22:1385–1390. https://doi.org/10.1111/ene.12754
Fini N, Georgoulopoulou E, Vinceti M et al (2014) Noninvasive and invasive ventilation and enteral nutrition for ALS in Italy. Muscle Nerve 50:508–516. https://doi.org/10.1002/mus.24187
Mandrioli J, Biguzzi S, Guidi C et al (2014) Epidemiology of amyotrophic lateral sclerosis in Emilia Romagna Region ( Italy ): a population based study. Amyotroph Lateral Scler Frontotemporal Degener 15:262–268. https://doi.org/10.3109/21678421.2013.865752
Brooks BR, Miller RG, Swash M, Munsat TL (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1:293–299. https://doi.org/10.1080/146608200300079536
Chiò A, Calvo A, Moglia C, Mazzini L, Mora G, PARALS Study Group (2011) Phenotypic heterogeneity of amyotrophic lateral sclerosis: a population based study. J Neurol Neurosurg Psychiatry 82:740–746
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169:13–21
Mandrioli J, Biguzzi S, Guidi C et al (2015) Heterogeneity in ALSFRS-R decline and survival: a population-based study in Italy. Neurol Sci 36:2243–2252. https://doi.org/10.1007/s10072-015-2343-6
Allison PD (1982) Discrete-time methods for the analysis of event histories. Sociol Methodol 13:61–98
Allison P (2014) Event history and survival analysis. SAGE, Thousand Oaks. https://doi.org/10.4135/9781452270029
Harrell F (2015) Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer International Publishing AG, Switzerland
White IR, Royston PWA (2011) Multiple imputation using chained equations: Issues and guidance for practice. Stat Med 30:377–399
Solmaz S, Duksal FGS (2015) Is obstructive sleep apnoea syndrome really one of the causes of secondary polycythaemia? Hematology 20:108–111
Suarez I, Bodega G, Fernandez B (2002) Glutamine synthetase in brain: Effect of ammonia. Neurochem Int 41:123–142. https://doi.org/10.1016/S0197-0186(02)00033-5
Hertz L, Schousboe A, Boechler N, Mukerji S, Fedoroff S (1978) Kinetic characteristics of the glutamate uptake into normal astrocytes in cultures. Neurochem Res 3:1–14
Abraham A, Drory VE (2014) Influence of serum uric acid levels on prognosis and survival in amyotrophic lateral sclerosis: a meta-analysis. J Neurol 261:1133–1138. https://doi.org/10.1007/s00415-014-7331-x
Zoccolella S, Simone IL, Capozzo R et al (2011) An exploratory study of serum urate levels in patients with amyotrophic lateral sclerosis. J Neurol 258:238–243. https://doi.org/10.1007/s00415-010-5735-9
S Il O, Baek S, Park JS et al (2015) Prognostic role of serum levels of uric acid in amyotrophic lateral sclerosis. J Clin Neurol (Seoul, Korea) 11:376–382. https://doi.org/10.3988/jcn.2015.11.4.376
Chiò A, Calvo A, Ilardi A et al (2009) Lower serum lipid levels are related to respiratory impairment in patients with ALS. Neurology 73:1681–1685. https://doi.org/10.1212/WNL.0b013e3181c1df1e
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mandrioli, J., Rosi, E., Fini, N. et al. Changes in routine laboratory tests and survival in amyotrophic lateral sclerosis. Neurol Sci 38, 2177–2182 (2017). https://doi.org/10.1007/s10072-017-3138-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3138-8